Urinary Carnosinase-1 Excretion is Associated with Urinary Carnosine Depletion and Risk of Graft Failure in Kidney Transplant Recipients: Results of the TransplantLines Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Data Collection, Clinical and Laboratory Measurements
2.3. Assessment of Urinary CN1 and Urinary Carnosine
2.4. Clinical Endpoints
2.5. Statistical Analyses
Prospective Analyses
3. Results
3.1. Urinary Carnosine is Reduced in KTRs Compared to Healthy Donors
3.2. Urinary CN1 is Inversely Associated with Urinary Carnosine in KTRs
3.3. Urinary CN1 Excretion Is Associated with Urinary Oxidative Stress Markers
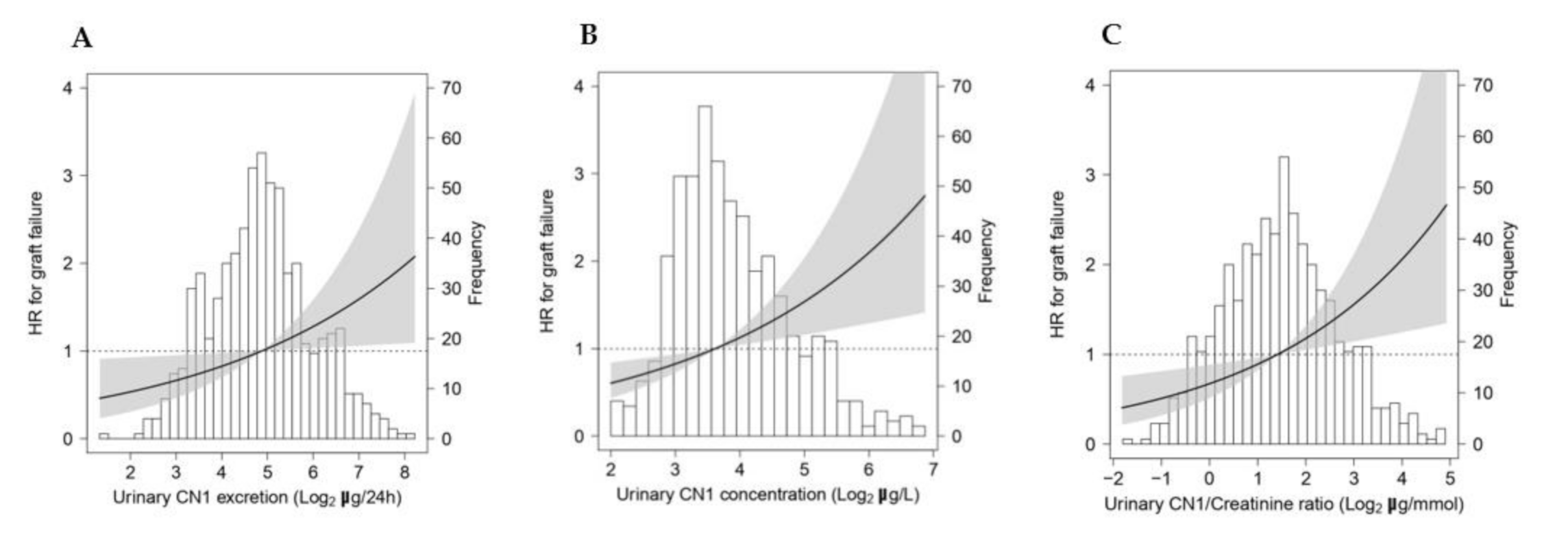
3.4. Urinary CN1 Is Associated with High Risk of Graft Failure in KTRs
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
Appendix A.1. Carnosinase-1 Determination in Urine by ELISA
Appendix A.2. Amino Acid Profiling with Liquid Chromatography Isotope Dilution Mass Spectrometry
References
- Wolfe, R.A.; Ashby, V.B.; Milford, E.L.; Ojo, A.O.; Ettenger, R.E.; Agodoa, L.Y.C.; Held, P.J.; Port, F.K. Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. N. Engl. J. Med. 1999, 341, 1725–1730. [Google Scholar] [CrossRef] [Green Version]
- Tonelli, M.; Wiebe, N.; Knoll, G.; Bello, A.; Browne, S.; Jadhav, D.; Klarenbach, S.; Gill, J. Systematic review: Kidney transplantation compared with dialysis in clinically relevant outcomes. Am. J. Transplant. 2011, 11, 2093–2109. [Google Scholar] [CrossRef]
- Howard, K.; Salkeld, G.; White, S.; McDonald, S.; Chadban, S.; Craig, J.C.; Cass, A. The cost-effectiveness of increasing kidney transplantation and home-based dialysis. Nephrology 2009, 14, 123–132. [Google Scholar] [CrossRef] [PubMed]
- Haller, M.; Gutjahr, G.; Kramar, R.; Harnoncourt, F.; Oberbauer, R. Cost-effectiveness analysis of renal replacement therapy in Austria. Nephrol. Dial. Transplant. 2011, 26, 2988–2995. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matas, A.J.; Gillingham, K.J.; Humar, A.; Kandaswamy, R.; Sutherland, D.E.R.; Payne, W.D.; Dunn, T.B.; Najarian, J.S. 2202 Kidney transplant recipients with 10 years of graft function: What happens next? Am. J. Transplant. 2008, 8, 2410–2419. [Google Scholar] [CrossRef] [Green Version]
- Janssen, B.; Hohenadel, D.; Brinkkoetter, P.; Peters, V.; Rind, N.; Fischer, C.; Rychlik, I.; Cerna, M.; Romzova, M.; de Heer, E.; et al. Carnosine as a protective factor in diabetic nephropathy: Association with a leucine repeat of the carnosinase gene CNDP1. Diabetes 2005, 54, 2320–2327. [Google Scholar] [CrossRef] [Green Version]
- Freedman, B.I.; Hicks, P.J.; Sale, M.M.; Pierson, E.D.; Langefeld, C.D.; Rich, S.S.; Xu, J.; McDonough, C.; Janssen, B.; Yard, B.A.; et al. A leucine repeat in the carnosinase gene CNDP1 is associated with diabetic end-stage renal disease in European Americans. Nephrol. Dial. Transplant. 2007, 22, 1131–1135. [Google Scholar] [CrossRef] [PubMed]
- Mooyaart, A.L.; van Valkengoed, I.G.M.; Shaw, P.K.C.; Peters, V.; Baelde, H.J.; Rabelink, T.J.; Bruijn, J.A.; Stronks, K.; de Heer, E. Lower frequency of the 5/5 homozygous CNDP1 genotype in South Asian Surinamese. Diabetes Res. Clin. Pract. 2009, 85, 272–278. [Google Scholar] [CrossRef] [PubMed]
- Ahluwalia, T.S.; Lindholm, E.; Groop, L.C. Common variants in CNDP1 and CNDP2, and risk of nephropathy in type 2 diabetes. Diabetologia 2011, 54, 2295–2302. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yadav, A.K.; Sinha, N.; Kumar, V.; Bhansali, A.; Dutta, P.; Jha, V. Association of CTG repeat polymorphism in carnosine dipeptidase 1 (CNDP1) gene with diabetic nephropathy in north Indians. Indian J. Med. Res. 2016, 144, 32–37. [Google Scholar] [CrossRef] [PubMed]
- Peters, V.; Kebbewar, M.; Janssen, B.; Hoffmann, G.F.; Möller, K.; Wygoda, S.; Charbit, M.; Fernandes-Teixeira, A.; Jeck, N.; Zschocke, J.; et al. CNDP1 genotype and renal survival in pediatric nephropathies. J. Pediatr. Endocrinol. Metab. 2016, 29, 827–833. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Abboud, H.E.; Pahl, M.V.; Tayek, J.; Snyder, S.; Tamkin, J.; Alcorn, H.; Ipp, E.; Nast, C.C.; Elston, R.C.; et al. Examination of Association with Candidate Genes for Diabetic Nephropathy in a Mexican American Population. Clin. J. Am. Soc. Nephrol. 2010, 5, 1072–1078. [Google Scholar] [CrossRef] [Green Version]
- Mcdonough, C.W.; Hicks, P.J.; Lu, L.; Langefeld, C.D.; Freedman, B.I.; Bowden, D.W. The Influence of Carnosinase Gene Polymorphisms on Diabetic Nephropathy Risk in African Americans NIH Public Access. Hum. Genet. 2009, 126, 265–275. [Google Scholar] [CrossRef] [Green Version]
- Boldyrev, A.A.; Aldini, G.; Derave, W. Physiology and Pathophysiology of Carnosine. Physiol. Rev. 2013, 93, 1803–1845. [Google Scholar] [CrossRef] [PubMed]
- Sauerhöfer, S.; Yuan, G.; Braun, G.S.; Deinzer, M.; Neumaier, M.; Gretz, N.; Floege, J.; Kriz, W.; van der Woude, F.; Moeller, M.J. L-carnosine, a substrate of carnosinase-1, influences glucose metabolism. Diabetes 2007, 56, 2425–2432. [Google Scholar] [CrossRef] [Green Version]
- Everaert, I.; He, J.; Hanssens, M.; Stautemas, J.; Bakker, K.; Albrecht, T.; Zhang, S.; Van der Stede, T.; Vanhove, K.; Hoetker, D.; et al. Carnosinase-1 overexpression, but not aerobic exercise training, affects the development of diabetic nephropathy in BTBR ob/ob mice. Am. J. Physiol. Ren. Physiol. 2020, 318, F1030–F1040. [Google Scholar] [CrossRef] [PubMed]
- Qiu, J.; Albrecht, T.; Zhang, S.; Hauske, S.J.; Rodriguez-Niño, A.; Zhang, X.; Nosan, D.; Pastene, D.O.; Sticht, C.; Delatorre, C.; et al. Human carnosinase 1 overexpression aggravates diabetes and renal impairment in BTBROb/Ob mice. J. Mol. Med. 2020, 98, 1333–1346. [Google Scholar] [CrossRef]
- Albrecht, T.; Schilperoort, M.; Zhang, S.; Braun, J.D.; Qiu, J.; Rodriguez, A.; Pastene, D.O.; Krämer, B.K.; Köppel, H.; Baelde, H.; et al. Carnosine Attenuates the Development of both Type 2 Diabetes and Diabetic Nephropathy in BTBR ob/ob Mice. Sci. Rep. 2017, 7, 44492. [Google Scholar] [CrossRef] [PubMed]
- Peters, V.; Riedl, E.; Braunagel, M.; Höger, S.; Hauske, S.; Pfister, F.; Zschocke, J.; Lanthaler, B.; Benck, U.; Hammes, H.P.; et al. Carnosine treatment in combination with ACE inhibition in diabetic rats. Regul. Pept. 2014, 194, 36–40. [Google Scholar] [CrossRef] [PubMed]
- Aldini, G.; Orioli, M.; Rossoni, G.; Savi, F.; Braidotti, P.; Vistoli, G.; Yeum, K.J.; Negrisoli, G.; Carini, M. The carbonyl scavenger carnosine ameliorates dyslipidaemia and renal function in Zucker obese rats. J. Cell. Mol. Med. 2011, 15, 1339–1354. [Google Scholar] [CrossRef] [PubMed]
- Gardner, M.L.; Illingworth, K.M.; Kelleher, J.; Wood, D. Intestinal absorption of the intact peptide carnosine in man, and comparison with intestinal permeability to lactulose. J. Physiol. 1991, 439, 411–422. [Google Scholar] [CrossRef]
- Everaert, I.; Taes, Y.; De Heer, E.; Baelde, H.; Zutinic, A.; Yard, B.; Sauerhöfer, S.; Vanhee, L.; Delanghe, J.; Aldini, G.; et al. Low plasma carnosinase activity promotes carnosinemia after carnosine ingestion in humans. Am. J. Physiol. Ren. Physiol. 2012, 302, F1537–F1544. [Google Scholar] [CrossRef]
- Rodriguez-Niño, A.; Gant, C.M.; Braun, J.D.; Li, X.; Zhang, S.; Albrecht, T.; Qiu, J.; Bakker, S.J.L.; Laverman, G.D.; Krämer, B.K.; et al. Detection of carnosinase-1 in urine of healthy individuals and patients with type 2 diabetes: Correlation with albuminuria and renal function. Amino Acids 2019, 51, 17–25. [Google Scholar] [CrossRef]
- Rodriguez-Niño, A.; Hauske, S.J.; Herold, A.; Qiu, J.; van den Born, J.; Bakker, S.J.L.; Krämer, B.K.; Yard, B.A. Serum Carnosinase-1 and Albuminuria Rather than the CNDP1 Genotype Correlate with Urinary Carnosinase-1 in Diabetic and Nondiabetic Patients with Chronic Kidney Disease. J. Diabetes Res. 2019, 2019, 6850628. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pascual, M.; Theruvath, T.; Kawai, T.; Tolkoff-Rubin, N.; Cosimi, A.B. Strategies to Improve Long-Term Outcomes after Renal Transplantation. N. Engl. J. Med. 2002, 346, 580–590. [Google Scholar] [CrossRef]
- Nankivell, B.J.; Borrows, R.J.; Fung, C.L.S.; O’Connell, P.J.; Allen, R.D.M.; Chapman, J.R. The Natural History of Chronic Allograft Nephropathy. N. Engl. J. Med. 2003, 349, 2326–2333. [Google Scholar] [CrossRef] [Green Version]
- Halloran, P.F.; Melk, A.; Barth, C. Rethinking chronic allograft nephropathy: The concept of accelerated senescence. J. Am. Soc. Nephrol. 1999, 10, 167–181. [Google Scholar] [CrossRef]
- Djamali, A. Oxidative stress as a common pathway to chronic tubulointerstitial injury in kidney allografts. Am. J. Physiol. Ren. Physiol. 2007, 293, F445–F455. [Google Scholar] [CrossRef] [PubMed]
- Zahmatkesh, M.; Kadkhodaee, M.; Mahdavi-Mazdeh, M.; Ghaznavi, R.; Hemati, M.; Seifi, B.; Golab, F.; Hasani, K.; Lessan-Pezeshki, M.; Einollahi, B. Oxidative stress status in renal transplant recipients. Exp. Clin. Transplant. 2010, 8, 38–44. [Google Scholar]
- van den Berg, E.; Pasch, A.; Westendorp, W.H.; Navis, G.; Brink, E.J.; Gans, R.O.B.; van Goor, H.; Bakker, S.J.L. Urinary sulfur metabolites associate with a favorable cardiovascular risk profile and survival benefit in renal transplant recipients. J. Am. Soc. Nephrol. 2014, 25, 1303–1312. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- van den Berg, E.; Engberink, M.F.; Brink, E.J.; van Baak, M.A.; Joosten, M.M.; Gans, R.O.B.; Navis, G.; Bakker, S.J.L. Dietary acid load and metabolic acidosis in renal transplant recipients. Clin. J. Am. Soc. Nephrol. 2012, 7, 1811–1818. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Faizan, M.; Esatbeyoglu, T.; Bayram, B.; Rimbach, G. A Fast and Validated Method for the Determination of Malondialdehyde in Fish Liver Using High-Performance Liquid Chromatography with a Photodiode Array Detector. J. Food Sci. 2014, 79. [Google Scholar] [CrossRef]
- Yepes-Calderón, M.; Sotomayor, C.G.; Pena, M.; Eisenga, M.F.; Gans, R.O.B.; Berger, S.P.; Moers, C.; Sugaya, T.; Doekharan, D.; Navis, G.J.; et al. Urinary liver-type fatty acid-binding protein is independently associated with graft failure in outpatient kidney transplant recipients. Am. J. Transplant. 2020. [Google Scholar] [CrossRef]
- American Diabetes Association. 2. Classification and Diagnosis of Diabetes. Diabetes Care 2017, 40, S11–S24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Inker, L.A.; Schmid, C.H.; Tighiouart, H.; Eckfeldt, J.H.; Feldman, H.I.; Greene, T.; Kusek, J.W.; Manzi, J.; Van Lente, F.; Zhang, Y.L.; et al. Estimating Glomerular Filtration Rate from Serum Creatinine and Cystatin C. N. Engl. J. Med. 2012, 367, 20–29. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Den Berg, E.; Engberink, M.F.; Brink, E.J.; Van Baak, M.A.; Gans, R.O.B.; Navis, G.; Bakker, S.J.L. Dietary protein, blood pressure and renal function in renal transplant recipients. Br. J. Nutr. 2013, 109, 1463–1470. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Voedingscentrum Den Haag. Stichting Nederlands Voedingsstoffenbestand Zeist NEVO-Tabel: Nederlands Voedingsstoffenbestand; Voedingscentrum: Den Haag, The Netherlands, 2006. [Google Scholar]
- Willett, W.C.; Howe, G.R.; Kushi, L.H. Adjustment for total energy intake in epidemiologic studies. Am. J. Clin. Nutr. 1997, 65, 1220S–1228S. [Google Scholar] [CrossRef]
- Maroni, B.J.; Steinman, T.I.; Mitch, W.E. A method for estimating nitrogen intake of patients with chronic renal failure. Kidney Int. 1985, 27, 58–65. [Google Scholar] [CrossRef] [Green Version]
- Eisenga, M.F.; Kieneker, L.M.; Soedamah-Muthu, S.S.; van den Berg, E.; Deetman, P.E.; Navis, G.J.; Gans, R.O.; Gaillard, C.A.; Bakker, S.J.; Joosten, M.M. Urinary potassium excretion, renal ammoniagenesis, and risk of graft failure and mortality in renal transplant recipients. Am. J. Clin. Nutr. 2016, 104, 1703–1711. [Google Scholar] [CrossRef]
- Peters, V.; Klessens, C.Q.F.; Baelde, H.J.; Singler, B.; Veraar, K.A.M.; Zutinic, A.; Drozak, J.; Zschocke, J.; Schmitt, C.P.; de Heer, E. Intrinsic carnosine metabolism in the human kidney. Amino Acids 2015, 47, 2541–2550. [Google Scholar] [CrossRef] [Green Version]
- Teufel, M.; Saudek, V.; Ledig, J.-P.; Bernhardt, A.; Boularand, S.; Carreau, A.; Cairns, N.J.; Carter, C.; Cowley, D.J.; Duverger, D.; et al. Sequence identification and characterization of human carnosinase and a closely related non-specific dipeptidase. J. Biol. Chem. 2003, 278, 6521–6531. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ruggiero, A.; Villa, C.H.; Bander, E.; Rey, D.A.; Bergkvist, M.; Batt, C.A.; Manova-Todorova, K.; Deen, W.M.; Scheinberg, D.A.; McDevitt, M.R. Paradoxical glomerular filtration of carbon nanotubes. Proc. Natl. Acad. Sci. USA 2010, 107, 12369–12374. [Google Scholar] [CrossRef] [Green Version]
- Dantzler, W.H.; Layton, A.T.; Layton, H.E.; Pannabecker, T.L. Urine-concentrating mechanism in the inner medulla: Function of the thin limbs of the loops of henle. Clin. J. Am. Soc. Nephrol. 2014, 9, 1781–1789. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dar, M.A.; Wahiduzzaman; Islam, A.; Hassan, M.I.; Ahmad, F. Counteraction of the deleterious effects of urea on structure and stability of mammalian kidney proteins by osmolytes. Int. J. Biol. Macromol. 2018, 107, 1659–1667. [Google Scholar] [CrossRef] [PubMed]
- Yang, B.; Bankir, L. Urea and urine concentrating ability: New insights from studies in mice. Am. J. Physiol. Ren. Physiol. 2005, 288. [Google Scholar] [CrossRef]
- Peters, V.; Lanthaler, B.; Amberger, A.; Fleming, T.; Forsberg, E.; Hecker, M.; Wagner, A.H.; Yue, W.W.; Hoffmann, G.F.; Nawroth, P.; et al. Carnosine metabolism in diabetes is altered by reactive metabolites. Amino Acids 2015, 47, 2367–2376. [Google Scholar] [CrossRef]
- Bellia, F.; Calabrese, V.; Guarino, F.; Cavallaro, M.; Cornelius, C.; De Pinto, V.; Rizzarelli, E. Carnosinase levels in aging brain: Redox state induction and cellular stress response. Antioxid. Redox Signal. 2009, 11, 2759–2775. [Google Scholar] [CrossRef] [PubMed]
- Peters, V.; Schmitt, C.P.; Zschocke, J.; Gross, M.-L.; Brismar, K.; Forsberg, E. Carnosine treatment largely prevents alterations of renal carnosine metabolism in diabetic mice. Amino Acids 2012, 42, 2411–2416. [Google Scholar] [CrossRef]
- Minz, M.; Heer, M.; Arora, S.; Sharma, A.; Khullar, M. Oxidative Status in Stable Renal Transplantation. In Transplantation proceedings; Elsevier: Amsterdam, The Netherlands, 2006; Volume 38, pp. 2020–2021. [Google Scholar]
- Zhou, Z.; Liu, X.Q.; Zhang, S.Q.; Qi, X.M.; Zhang, Q.; Yard, B.; Wu, Y.G. Correlation between serum carnosinase concentration and renal damage in diabetic nephropathy patients. Amino Acids 2021, 53, 687–700. [Google Scholar] [CrossRef] [PubMed]
- Xing, L.; Chee, M.E.; Zhang, H.; Zhang, W.; Mine, Y. Carnosine—A natural bioactive dipeptide: Bioaccessibility, bioavailability and health benefits. J. Food Bioact. 2019, 5, 8–17. [Google Scholar] [CrossRef] [Green Version]
- Kamal, M.A.; Jiang, H.; Hu, Y.; Keep, R.F.; Smith, D.E. Influence of genetic knockout of Pept2 on the in vivo disposition of endogenous and exogenous carnosine in wild-type and Pept2 null mice. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2009, 296, R986–R991. [Google Scholar] [CrossRef] [Green Version]
- Jappar, D.; Hu, Y.; Keep, R.F.; Smith, D.E. Transport mechanisms of carnosine in SKPT cells: Contribution of apical and basolateral membrane transporters. Pharm. Res. 2009, 26, 172–181. [Google Scholar] [CrossRef] [Green Version]
- KaborÉ, R.; Haller, M.C.; Harambat, J.; Heinze, G.; LeffondrÉ, K. Risk prediction models for graft failure in kidney transplantation: A systematic review. Nephrol. Dial. Transplant. 2017, 32, ii68–ii76. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meier-Kriesche, H.U.; Schold, J.D.; Kaplan, B. Long-term renal allograft survival: Have we made significant progress or is it time to rethink our analytic and therapeutic strategies? Am. J. Transplant. 2004, 4, 1289–1295. [Google Scholar] [CrossRef]
- Cristol, J.P.; Vela, C.; Maggi, M.F.; Descomps, B.; Mourad, G. Oxidative stress and lipid abnormalities in renal transplant recipients with or without chronic rejection. Transplantation 1998, 65, 1322–1328. [Google Scholar] [CrossRef]
- Fonseca, I.; Reguengo, H.; Almeida, M.; Dias, L.; Martins, L.S.; Pedroso, S.; Santos, J.; Lobato, L.; Henriques, A.C.; Mendonça, D. Oxidative stress in kidney transplantation: Malondialdehyde is an early predictive marker of graft dysfunction. Transplantation 2014, 97, 1058–1065. [Google Scholar] [CrossRef] [Green Version]
- Aldini, G.; Carini, M.; Beretta, G.; Bradamante, S.; Facino, R.M. Carnosine is a quencher of 4-hydroxy-nonenal: Through what mechanism of reaction? Biochem. Biophys. Res. Commun. 2002, 298, 699–706. [Google Scholar] [CrossRef]
- Vistoli, G.; Colzani, M.; Mazzolari, A.; Gilardoni, E.; Rivaletto, C.; Carini, M.; Aldini, G. Quenching activity of carnosine derivatives towards reactive carbonyl species: Focus on α−(methylglyoxal) and β−(malondialdehyde) dicarbonyls. Biochem. Biophys. Res. Commun. 2017, 492, 487–492. [Google Scholar] [CrossRef] [PubMed]
- Aldini, G.; Facino, R.M.; Beretta, G.; Carini, M. Carnosine and related dipeptides as quenchers of reactive carbonyl species: From structural studies to therapeutic perspectives. Biofactors 2005, 24, 77–87. [Google Scholar] [CrossRef] [PubMed]
- Ansurudeen, I.; Sunkari, V.G.; Grünler, J.; Peters, V.; Schmitt, C.P.; Catrina, S.-B.; Brismar, K.; Forsberg, E.A. Carnosine enhances diabetic wound healing in the db/db mouse model of type 2 diabetes. Amino Acids 2012, 43, 127–134. [Google Scholar] [CrossRef]
- Kurata, H.; Fujii, T.; Tsutsui, H.; Katayama, T.; Ohkita, M.; Takaoka, M.; Tsuruoka, N.; Kiso, Y.; Ohno, Y.; Fujisawa, Y.; et al. Renoprotective effects of l-carnosine on ischemia/reperfusion-induced renal injury in rats. J. Pharmacol. Exp. Ther. 2006, 319, 640–647. [Google Scholar] [PubMed] [Green Version]
- Fujii, T.; Takaoka, M.; Muraoka, T.; Kurata, H.; Tsuruoka, N.; Ono, H.; Kiso, Y.; Tanaka, T.; Matsumura, Y. Preventive effect of L-carnosine on ischemia/reperfusion-induced acute renal failure in rats. Eur. J. Pharmacol. 2003, 474, 261–267. [Google Scholar] [CrossRef]
- Elbarbary, N.S.; Ismail, E.A.R.; El-Naggar, A.R.; Hamouda, M.H.; El-Hamamsy, M. The effect of 12 weeks carnosine supplementation on renal functional integrity and oxidative stress in pediatric patients with diabetic nephropathy: A randomized placebo-controlled trial. Pediatr. Diabetes 2018, 19, 470–477. [Google Scholar] [CrossRef] [PubMed]
- Qiu, J.; Hauske, S.J.; Zhang, S.; Rodriguez-Niño, A.; Albrecht, T.; Pastene, D.O.; van den Born, J.; van Goor, H.; Ruf, S.; Kohlmann, M.; et al. Identification and characterisation of carnostatine (SAN9812), a potent and selective carnosinase (CN1) inhibitor with in vivo activity. Amino Acids 2019, 51, 7–16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Anderson, E.J.; Vistoli, G.; Katunga, L.A.; Funai, K.; Regazzoni, L.; Blake Monroe, T.; Gilardoni, E.; Cannizzaro, L.; Colzani, M.; De Maddis, D.; et al. A carnosine analog mitigates metabolic disorders of obesity by reducing carbonyl stress. J. Clin. Investig. 2018, 128, 5280–5293. [Google Scholar] [CrossRef] [PubMed]
| Variable | KTRs | Healthy Subjects | |
|---|---|---|---|
| n = 703 | n = 257 | p-Value | |
| Urinary CN1 | |||
| CN1 excretion, µg/24 h | 29.4 [17.4–49.2] | 32.7 [21.6–43.6] | 0.42 |
| CN1 concentration, µg/L | 12.3 [8.1–20.9] | 13 [10.5–16.5] | 0.72 |
| CN1/creatinine ratio, µg/mmol | 2.7 [1.5–4.6] | 2.6 [1.6–3.7] | 0.09 |
| Below detection limit (<4 µg/L), n (%) | 95 (14) | 33 (13) | 0.76 |
| Urinary carnosine | |||
| Carnosine excretion, µmol/24 h | 26.5 [21.4–33.3] | 34.8 [25.6–46.8] | <0.001 |
| Carnosine concentration, µmol/L | 9.9 [9.9–11.5] | 11.4 [9.9–19.5] | <0.001 |
| Carnosine/creatinine ratio, µmol/mmol | 2.3 [1.8–3.2] | 2.8 [2.1–3.8] | <0.001 |
| Below detection limit (<10 µmol/L), n (%) | 465 (66) | 96 (37) | <0.001 |
| Demographics | |||
| Male n, (%) | 399 (57) | 114 (44) | 0.001 |
| Age, years | 53.0 ± 13 | 53.8 ± 11 | 0.34 |
| Body composition | |||
| BMI, kg/m² | 26.7 ± 4.8 | 26.0 ± 3.5 | 0.02 |
| Waist circumference, cm | 98 ± 15 | 91.3 ± 10.4 | <0.001 |
| Cardiovascular | |||
| Systolic blood pressure, mmHg | 136 ± 17.5 | 127 ± 13.1 | <0.001 |
| Diastolic blood pressure, mmHg | 83 ± 11 | 77 ± 9 | <0.001 |
| Mean arterial pressure, mmHg | 107 ± 15 | 96 ± 16.1 | <0.001 |
| Heart rate, bpm | 69 ± 12 | 67 ± 10 | 0.02 |
| Lipids | |||
| Total cholesterol, mmol/L | 5.1 ± 1.1 | 5.4 ± 1.0 | 0.002 |
| HDL cholesterol, mmol/L | 1.4 ± 0.5 | 1.6 ± 0.5 | 0.02 |
| LDL cholesterol, mmol/L | 3.0 ± 0.9 | 3.8 ± 1.0 | <0.001 |
| Triglycerides, mmol/L | 1.7 [1.3–2.3] | 1.2 [0.9–1.6] | <0.001 |
| Glucose homeostasis | |||
| Diabetes mellitus, n (%) | 168 (24) | 13 (5) | <0.001 |
| Glucose, mmol/L | 5.3 [4.8–6.0] | 5.3 [5.0–5.7] | 0.22 |
| HbA1c, mmol/mol | 41.9 ± 8.9 | 37.6 ± 3.9 | <0.001 |
| Renal function | |||
| Serum creatinine, µmol/L | 125 [99–160] | 72 [64–81] | <0.001 |
| eGFR, ml/min/1.73 m² | 45 ± 18 | 92 ± 16 | <0.001 |
| Creatinine clearance, ml/min | 66 ± 27 | 127 ± 40 | <0.001 |
| Proteinuria, n (%) | 157 (22) | 1 (0.5) | <0.001 |
| Dietary intakes * | |||
| Energy intake, kcal/24 h | 2170 ± 639 | 2295 ± 738 | 0.03 |
| Total protein intake g/24 h | 82 ± 12 | 85±13 | 0.01 |
| Animal protein intake g/24 h | 51 ± 13 | 52 ± 13 | 0.17 |
| Total meat intake g/24 h | 96 [74–116] | 94 [72–115] | 0.71 |
| Red meat intake g/24 h | 82 [59–103] | 80 [60–106] | 0.76 |
| Serum parameters | |||
| NT-proBNP, ng/L | 255 [108–625] | 40 [23–68] | <0.001 |
| Sodium, mmol/L | 141 ± 2.8 | 142 ± 2.0 | <0.001 |
| Potassium mmol/L | 4.0 ± 0.5 | 3.9 ± 0.3 | <0.001 |
| hsCRP, mg/L | 1.6 [0.7–4.6] | 1.1 [0.6–2.3] | <0.001 |
| Urinary parameters | |||
| Urea excretion, mmol/24 h | 384 [308–456] | 392 [336–463] | 0.09 |
| Creatinine excretion, mmol/24 h | 11.6 ± 3.5 | 13.3 ± 4.4 | <0.001 |
| Medication use | |||
| Antihypertensives, n (%) | 620 (88) | 29 (11) | <0.001 |
| Variable | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|
| OR [95%CI] | p-Value | OR [95%CI] | p-Value | OR [95%CI] | p-Value | |
| Urinary CN1 concentrations, µg/L | 1.24 [1.06–1.45] | 0.007 | 1.26 [1.07–1.48] | 0.006 | 1.05 [0.88–1.25] | 0.60 |
| Sex, male | 1.60 [1.12–2.27] | 0.009 | 1.65 [1.14–2.40] | 0.008 | ||
| Age, years | 1.04 [1.02–1.05] | ˂0.001 | 1.03 [1.02–1.05] | ˂0.001 | ||
| eGFR, ml/min/1.73² | 0.96 [0.95–0.97] | ˂0.001 | ||||
| Variable | KTR | Model 1 | Model 2 | ||
|---|---|---|---|---|---|
| n = 703 | St. β | p-Value | St. β | p-Value | |
| Urinary CN1 | |||||
| CN1 excretion, µg/24h | 29.4 [17.4–49.2] | - | - | - | - |
| CN1 concentration, µg/L | 12.3 [8.1–20.9] | 0.91 | <0.001 | 0.91 | <0.001 |
| CN1/creatinine ratio, µg/mmol | 2.7 [1.5–4.6] | 0.92 | <0.001 | 0.98 | <0.001 |
| Demographics | |||||
| Male, n (%) | 399 (57) | 0.02 | 0.56 | 0.01 | 0.72 |
| Age, years | 53.0 ± 13 | 0.03 | 0.47 | 0.003 | 0.94 |
| Body composition | |||||
| Body surface area, m² | 1.94 ± 0.22 | −0.01 | 0.71 | −0.03 | 0.46 |
| BMI, kg/m² | 26.7 ± 4.8 | 0.01 | 0.89 | −0.02 | 0.65 |
| Waist circumference, cm | 98 ± 15 | 0.003 | 0.94 | −0.05 | 0.17 |
| Lifestyle | |||||
| Current smoker, n (%) | 83 (12) | 0.016 | 0.89 | −0.001 | 0.98 |
| Alcohol intake, g/24h | 2.6 [0.03–11.1] | −0.02 | 0.56 | −0.01 | 0.78 |
| Cardiovascular | |||||
| Systolic blood pressure, mmHg | 136 ± 17.5 | 0.09 | 0.02 | 0.07 | 0.09 |
| Diastolic blood pressure, mmHg | 83 ± 11 | 0.002 | 0.96 | −0.01 | 0.91 |
| Heart rate, bpm | 69 ± 12 | 0.03 | 0.49 | 0.03 | 0.47 |
| NT-proBNP, ng/L | 255 [108–625] | 0.21 | <0.001 | 0.13 | 0.01 |
| Hypertension, n (%) | 620 (88) | 0.06 | 0.13 | 0.04 | 0.22 |
| Cardiovascular history | |||||
| CVA and/or TIA, n (%) | 41 (6) | −0.01 | 0.77 | −0.02 | 0.60 |
| Myocardial infarction, n (%) | 35 (5) | −0.004 | 0.91 | −0.01 | 0.66 |
| Cardiovascular intervention, n (%) | 68 (10) | 0.07 | 0.05 | 0.05 | 0.16 |
| Lipids | |||||
| Total cholesterol, mmol/L | 5.1 ± 1.1 | 0.07 | 0.06 | 0.05 | 0.18 |
| HDL cholesterol, mmol/L | 1.4 ± 0.5 | 0.06 | 0.13 | 0.11 | 0.006 |
| LDL cholesterol, mmol/L | 3.0 ± 0.9 | 0.05 | 0.16 | 0.04 | 0.33 |
| Triglycerides, mmol/L | 1.7 [1.3–2.3] | 0.08 | 0.04 | 0.02 | 0.63 |
| Glucose homeostasis | |||||
| Diabetes mellitus, n (%) | 168 (24) | 0.06 | 0.11 | 0.05 | 0.18 |
| Glucose mmol/L | 5.3 [4.8–6.0] | 0.0001 | 0.99 | 0.01 | 0.84 |
| HbA1c, mmol/mol | 41.9 ± 8.9 | 0.03 | 0.48 | 0.03 | 0.42 |
| Renal function | |||||
| Serum creatinine, µmol/L | 125 [99–160] | 0.20 | <0.001 | −0.02 | 0.83 |
| eGFR, ml/min/1.73 m² | 45.1 ± 18.7 | −0.24 | <0.001 | −0.24 | <0.001 |
| Creatinine clearance, mL/min | 66 ± 27 | −0.12 | 0.002 | −0.19 | 0.002 |
| Proteinuria, n (%) | 157 (22) | 0.43 | <0.001 | 0.40 | <0.001 |
| Transplantation related | |||||
| Dialysis vintage, months | 27 [10–51] | 0.02 | 0.54 | 0.01 | 0.80 |
| Time since transplantation, years | 5.4 [1.9–12.0] | 0.03 | 0.44 | 0.05 | 0.23 |
| Transplantation up to baseline, n (%) | 0.05 | 0.16 | 0.04 | 0.24 | |
| First transplantation | 633 (90) | ||||
| Re-transplantation | 69 (10) | ||||
| Age donor, years | 43 ± 15.4 | 0.004 | 0.92 | −0.07 | 0.07 |
| Sex donor, n (% male) | 356 (51) | −0.04 | 0.30 | −0.07 | 0.06 |
| Donor type, living, n (%) | 239 (34) | −0.04 | 0.30 | −0.015 | 0.71 |
| Cold ischemia time, hours | 15 [3–21] | 0.03 | 0.41 | 0.010 | 0.79 |
| Warm ischemia, minutes | 40 [33–50] | −0.02 | 0.63 | −0.03 | 0.44 |
| Calcineurin inhibitors, n (%) | 381 (56) | 0.03 | 0.52 | −0.04 | 0.29 |
| Proliferator inhibitor, n (%) | 567 (84) | −0.07 | 0.09 | −0.03 | 0.40 |
| Prednisolone dosage, n (%) | 0.05 | 0.21 | 0.05 | 0.18 | |
| ≤7.5 mg/24 h | 284 (40) | ||||
| ˂7.5 mg/24 h | 419 (60) | ||||
| HLA-I n (%) | 106 (15) | 0.03 | 0.44 | 0.004 | 0.92 |
| HLA-II n (%) | 121 (17) | 0.04 | 0.28 | 0.01 | 0.76 |
| Graft rejection up to baseline, n (%) | 188 (27) | 0.08 | 0.04 | 0.05 | 0.20 |
| Post-transplant diabetes mellitus | 131 (19) | 0.04 | 0.34 | 0.03 | 0.44 |
| Delayed graft function | 52 (7) | 0.0001 | 0.99 | −0.03 | 0.44 |
| Dietary intake patterns | |||||
| Energy intake, kcal/24 h | 2170 ± 639 | −0.05 | 0.26 | −0.02 | 0.62 |
| Total protein intake, g/24 h | 82 ± 12 | 0.10 | 0.01 | 0.12 | 0.004 |
| Plant protein intake, g/24 h | 31 ± 6 | 0.04 | 0.37 | 0.07 | 0.12 |
| Animal protein intake, g/24 h | 51 ± 13 | 0.08 | 0.04 | 0.08 | 0.05 |
| Meat intake, g/24 h | 95 [74–116] | 0.01 | 0.28 | 0.01 | 0.26 |
| Serum parameters | |||||
| LDH, U/L | 198 [170–232] | 0.11 | 0.005 | 0.06 | 0.15 |
| Sodium, mmol/L | 141 ± 2.8 | −0.14 | <0.001 | −0.12 | 0.001 |
| Potassium, mmol/L | 4.0 ± 0.5 | 0.037 | 0.335 | −0.040 | 0.314 |
| Urinary parameters | |||||
| Sodium excretion, mmol/24 h | 146 [114–190] | 0.10 | 0.01 | 0.14 | <0.001 |
| Potassium excretion, mmol/24 h | 70.1 [ 55.4–87.2] | 0.13 | < 0.001 | 0.19 | <0.001 |
| Urea excretion, mmol/24 h | 384 [308–456] | 0.13 | 0.001 | 0.19 | <0.001 |
| Maroni protein intake, g/kg bw/24 h | 85.3 ± 20.6 | 0.12 | 0.003 | 0.18 | <0.001 |
| Creatinine excretion, µmol/24 h | 11.6 ± 3.4 | 0.04 | 0.30 | 0.12 | 0.01 |
| Medication use, n (%) | |||||
| RAAS blockage | 341 (49) | 0.03 | 0.45 | 0.01 | 0.90 |
| Antihypertensives | 620 (88) | 0.11 | 0.003 | 0.07 | 0.08 |
| Diuretic | 285 (41) | 0.10 | 0.008 | 0.03 | 0.39 |
| Oxidative stress and inflammation | |||||
| hsCRP, mg/L | 1.6 [0.7–4.6] | 0.04 | 0.27 | 0.02 | 0.68 |
| uMDA excretion, µmol/24 h | 9.7 [5.8–15.7] | 0.11 | 0.003 | 0.11 | 0.003 |
| Plasma MDA, µmol/L | 2.5 [1.9–3.7] | −0.04 | 0.27 | −0.02 | 0.52 |
| uL-FABP excretion, µg/24 h | 2.1 [0.9–7.4] | 0.29 | <0.001 | 0.24 | <0.001 |
| Primary kidney disease | |||||
| Primary glomerular disease | 198 (28) | 0.05 | 0.20 | 0.05 | 0.18 |
| Glomerulonephritis | 54 (8) | −0.03 | 0.51 | −0.02 | 0.58 |
| Tubulointerstitial disease | 83 (12) | 0.002 | 0.97 | 0.03 | 0.43 |
| Polycystic renal disease | 146 (21) | −0.04 | 0.30 | −0.07 | 0.05 |
| Dysplasia and hypoplasia | 28 (4) | 0.04 | 0.36 | 0.05 | 0.21 |
| Renovascular disease | 40 (6) | −0.02 | 0.63 | −0.02 | 0.54 |
| Diabetic nephropathy | 36 (5) | 0.04 | 0.28 | 0.02 | 0.57 |
| Model | Urinary CN1 Excretion | Urinary CN1 Concentration | Urinary CN1/Creatinine Ratio | |||
|---|---|---|---|---|---|---|
| HR [95%CI] | p-Value | HR [95%CI] | p-Value | HR [95%CI] | p-Value | |
| Model 1 | 1.73 [1.44–2.08] | ˂0.001 | 2.05 [1.69–2.49] | ˂0.001 | 1.76 [1.48–2.09] | ˂0.001 |
| Model 2 | 1.74 [1.44–2.09] | ˂0.001 | 2.05 [1.69–2.49] | ˂0.001 | 1.85 [1.55–2.21] | ˂0.001 |
| Model 3 | 1.24 [1.03–1.51] | 0.026 | 1.36 [1.11–1.67] | 0.003 | 1.32 [1.09–1.61] | 0.005 |
| Model 4 | 1.32 [1.06–1.61] | 0.011 | 1.43 [1.15–1.78] | 0.002 | 1.39 [1.13–1.72] | 0.002 |
| Model 5 | 1.24 [1.01–1.52] | 0.042 | 1.39 [1.12–1.72] | 0.003 | 1.31 [1.06–1.60] | 0.001 |
| Model 6 | 1.23 [1.01–1.50] | 0.037 | 1.34 [1.09–1.65] | 0.005 | 1.31 [1.07–1.59] | 0.008 |
| Model 7 | 1.31 [1.08–1.60] | 0.008 | 1.37 [1.12–1.69] | 0.003 | 1.32 [1.09–1.61] | 0.005 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodriguez-Niño, A.; Pastene, D.O.; Post, A.; Said, M.Y.; Gomes-Neto, A.W.; Kieneker, L.M.; Heiner-Fokkema, M.R.; Esatbeyoglu, T.; Rimbach, G.; Schnuelle, P.; et al. Urinary Carnosinase-1 Excretion is Associated with Urinary Carnosine Depletion and Risk of Graft Failure in Kidney Transplant Recipients: Results of the TransplantLines Cohort Study. Antioxidants 2021, 10, 1102. https://doi.org/10.3390/antiox10071102
Rodriguez-Niño A, Pastene DO, Post A, Said MY, Gomes-Neto AW, Kieneker LM, Heiner-Fokkema MR, Esatbeyoglu T, Rimbach G, Schnuelle P, et al. Urinary Carnosinase-1 Excretion is Associated with Urinary Carnosine Depletion and Risk of Graft Failure in Kidney Transplant Recipients: Results of the TransplantLines Cohort Study. Antioxidants. 2021; 10(7):1102. https://doi.org/10.3390/antiox10071102
Chicago/Turabian StyleRodriguez-Niño, Angelica, Diego O. Pastene, Adrian Post, M. Yusof Said, Antonio W. Gomes-Neto, Lyanne M. Kieneker, M. Rebecca Heiner-Fokkema, Tuba Esatbeyoglu, Gerald Rimbach, Peter Schnuelle, and et al. 2021. "Urinary Carnosinase-1 Excretion is Associated with Urinary Carnosine Depletion and Risk of Graft Failure in Kidney Transplant Recipients: Results of the TransplantLines Cohort Study" Antioxidants 10, no. 7: 1102. https://doi.org/10.3390/antiox10071102






