Impact of Heavy Metals on Human Male Fertility—An Overview
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy and Information Processing
2.2. Selection of Relevant Studies and Data Analysis
3. Results and Discussion
3.1. Compilation of Relevant Bibliographic Sources
3.2. Bibliometric Analysis
3.3. Bibliographical Analysis
3.4. Analysis of the Clinical Trials
3.5. Analysis of the Reviews
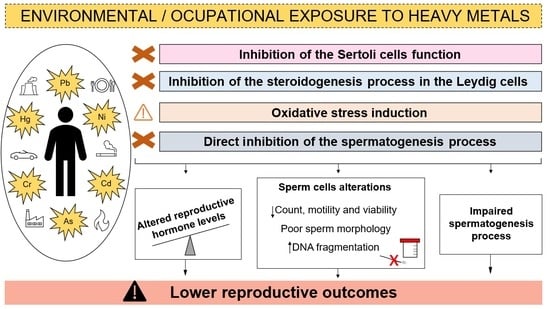
3.5.1. Heavy Metals Effects in the Reproductive Processes
3.5.2. Sources of Heavy Metals Exposure
Food Exposure
Environmental Exposure
Occupational Exposure
3.6. Analysis of the Articles
3.6.1. In Vitro Studies Exposing Sperm to Heavy Metals
3.6.2. Men from General Population as Study Subjects
3.6.3. Occupationally and Environmentally Exposed Men as Study Subjects
3.6.4. Men from Assisted-Reproduction Centers as Study Subjects
4. Conclusions
Supplementary Materials
Funding
Conflicts of Interest
References
- Agarwal, A.; Mulgund, A.; Hamada, A.; Chyatte, M.R. A unique view on male infertility around the globe. Reprod. Biol. Endocrinol. 2015, 13, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Brugo-Olmedo, S.; Chillik, C.; Kopelman, S. Definición y causas de la infertilidad. Rev. Colomb. Obstet. Ginecol. 2003, 54, 227–248. [Google Scholar] [CrossRef]
- Levine, H.; Jørgensen, N.; Martino-Andrade, A.; Mendiola, J.; Weksler-Derri, D.; Mindlis, I.; Pinotti, R.; Swan, S.H. Temporal trends in sperm count: A systematic review and meta-regression analysis. Hum. Reprod. Update 2017, 23, 646–659. [Google Scholar] [CrossRef]
- Mann, U.; Shiff, B.; Patel, P. Reasons for worldwide decline in male fertility. Curr. Opin. Urol. 2020, 30, 296–301. [Google Scholar] [CrossRef] [PubMed]
- Lindgren, M. Male Infertility. J. Physician Assis. 2018, 3, 139–147. [Google Scholar] [CrossRef]
- Guzick, D.S.; Overstreet, J.W.; Factor-Litvak, P.; Brazil, C.K.; Nakajima, S.T.; Coutifaris, C.; Carson, S.A.; Cisneros, P.; Steinkampf, M.P.; Hill, J.A.; et al. Sperm Morphology, Motility, and Concentration in Fertile and Infertile Men. N. Engl. J. Med. 2001, 345, 1388–1393. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Laboratory Manual for the Examination and Processing of Human Semen; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Kenkel, S.; Rolf, C.; Nieschlag, E. Occupational risks for male fertility: An analysis of patients attending a tertiary referral centre. Int. J. Androl. 2001, 24, 318–326. [Google Scholar] [CrossRef] [PubMed]
- Wald, M. Male infertility: Causes and cures. Sex. Reprod. Menopause 2005, 3, 83–87. [Google Scholar] [CrossRef]
- Bracke, A.; Peeters, K.; Punjabi, U.; Hoogewijs, D.; Dewilde, S. A search for molecular mechanisms underlying male idiopathic infertility. Reprod. Biomed. Online 2018, 36, 327–339. [Google Scholar] [CrossRef]
- Wang, C.; Swerdloff, R.S. Limitations of semen analysis as a test of male fertility and anticipated needs from newer tests. Fertil. Steril. 2014, 102, 1502–1507. [Google Scholar] [CrossRef]
- Khatun, A.; Rahman, S.; Pang, M.-G. Clinical assessment of the male fertility. Obstet. Gynecol. Sci. 2018, 61, 179–191. [Google Scholar] [CrossRef]
- Muratori, M.; Marchiani, S.; Maggi, M.; Forti, G.; Baldi, E. Origin and biological significance of DNA fragmentation in human spermatozoa. Front. Biosci. 2006, 11, 1491–1499. [Google Scholar] [CrossRef]
- Uppangalaa, S.; Pudakalakattib, S.; D’souzaa, F.; Salian, S.R.; Kalthur, G.; Kumar, P.; Atreya, H.; Adiga, S.K. Influence of sperm DNA damage on human preimplantation embryo metabolism. Reprod. Biol. 2016, 16, 234–241. [Google Scholar] [CrossRef]
- Aitken, R.J.; Baker, M.A. The Role of Genetics and Oxidative Stress in the Etiology of Male Infertility—A Unifying Hypothesis? Front. Endocrinol. 2020, 11, 581838. [Google Scholar] [CrossRef]
- Ma, Y.; He, X.; Qi, K.; Wang, T.; Qi, Y.; Cui, L.; Wang, F.; Song, M. Effects of environmental contaminants on fertility and reproductive health. J. Environ. Sci. 2019, 77, 210–217. [Google Scholar] [CrossRef]
- Figa-Talamanca, I.; Traina, M.E.; Urbani, E. Occupational exposures to metals, solvents and pesticides: Recent evidence on male reproductive effects and biological markers. Occup. Med. 2001, 51, 174–188. [Google Scholar] [CrossRef]
- Kopp, R.; Martínez, I.O.; Legradi, J.; Legler, J. Exposure to endocrine disrupting chemicals perturbs lipid metabolism and circadian rhythms. J. Environ. Sci. 2017, 62, 133–137. [Google Scholar] [CrossRef]
- Duffus, J.H. “Heavy metals” a meaningless term? (IUPAC Technical Report). Pure Appl. Chem. 2002, 74, 793–807. [Google Scholar] [CrossRef]
- Ali, H.; Khan, E. What are heavy metals? Long-standing controversy over the scientific use of the term ‘heavy metals’—Proposal of a comprehensive definition. Toxicol. Environ. Chem. 2018, 100, 6–19. [Google Scholar] [CrossRef]
- Balabanic, D.; Klemencic, A.K. Diet containing endocrine-disruptors and reproductive health. Handbook of Diet and Nutrition in the Menstrual Cycle. J. Reprod. Fertil. 2014, 2014, 359–372. [Google Scholar] [CrossRef]
- Balabanič, D.; Rupnik, M.S.; Klemenčič, A.K. Negative impact of endocrine-disrupting compounds on human reproductive health. Reprod. Fertil. Dev. 2011, 23, 403–416. [Google Scholar] [CrossRef] [PubMed]
- Lettieri, G.; Marra, F.; Moriello, C.; Prisco, M.; Notari, T.; Trifuoggi, M.; Giarra, A.; Bosco, L.; Montano, L.; Piscopo, M. Molecular Alterations in Spermatozoa of a Family Case Living in the Land of Fires. A First Look at Possible Transgenerational Effects of Pollutants. Int. J. Mol. Sci. 2020, 21, 6710. [Google Scholar] [CrossRef] [PubMed]
- Bergamo, P.; Volpe, M.G.; Lorenzetti, S.; Mantovani, A.; Notari, T.; Cocca, E.; Cerullo, S.; Di Stasio, M.; Cerino, P.; Montano, L. Human semen as an early, sensitive biomarker of highly polluted living environment in healthy men: A pilot biomonitoring study on trace elements in blood and semen and their relationship with sperm quality and RedOx status. Reprod. Toxicol. 2016, 66, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Alexander, B.H.; Checkoway, H.; Costa-Mallen, P.; Faustman, E.M.; Woods, J.S.; Kelsey, K.T.; Van Netten, C.; Costa, L.G. Interaction of blood lead and delta-aminolevulinic acid dehydratase genotype on markers of heme synthesis and sperm production in lead smelter workers. Environ. Health Perspect. 1998, 106, 213–216. [Google Scholar] [CrossRef]
- Ali, S.; Chaspoul, F.; Anderson, L.; Bergé-Lefranc, D.; Achard, V.; Perrin, J.; Gallice, P.; Guichaoua, M. Mapping Fifteen Trace Elements in Human Seminal Plasma and Sperm DNA. Biol. Trace Element Res. 2017, 175, 244–253. [Google Scholar] [CrossRef]
- Droller, M. Environment and the genitourinary tract. Otolaryngol. Neck Surg. 1996, 114, 248–252. [Google Scholar] [CrossRef]
- Jenardhanan, P.; Panneerselvam, M.; Mathur, P.P. Effect of environmental contaminants on spermatogenesis. Semin. Cell Dev. Biol. 2016, 59, 126–140. [Google Scholar] [CrossRef]
- Ilieva, I.; Sainova, I.; Yosifcheva, K. Toxic Effects of Heavy Metals (Lead and Cadmium) on Sperm Quality and Male Fertility. Acta Morphol. Anthropol. 2020, 27, 63–75. [Google Scholar]
- Kumar, S. Occupational Exposure Associated with Reproductive Dysfunction. J. Occup. Health 2004, 46, 1–19. [Google Scholar] [CrossRef]
- Bosco, L.; Notari, T.; Ruvolo, G.; Roccheri, M.C.; Martino, C.; Chiappetta, R.; Carone, D.; Bosco, G.L.; Carrillo, L.; Raimondo, S.; et al. Sperm DNA fragmentation: An early and reliable marker of air pollution. Environ. Toxicol. Pharmacol. 2018, 58, 243–249. [Google Scholar] [CrossRef]
- Yang, T.; Deng, L.; Sun, B.; Zhang, S.; Xian, Y.; Xiao, X.; Zhan, Y.; Xu, K.; Buonocore, J.J.; Tang, Y.; et al. Semen quality and windows of susceptibility: A case study during COVID-19 outbreak in China. Environ. Res. 2021, 197, 111085. [Google Scholar] [CrossRef]
- Li, H.; Xiao, X.; Zhang, J.; Zafar, M.I.; Wu, C.; Long, Y.; Lu, W.; Pan, F.; Meng, T.; Zhao, K.; et al. Impaired spermatogenesis in COVID-19 patients. EClinicalMedicine 2020, 28, 100604. [Google Scholar] [CrossRef]
- Wan, H.T.; Mruk, D.D.; Wong, C.K.C.; Cheng, C.Y. Targeting testis-specific proteins to inhibit spermatogenesis: Lesson from endocrine disrupting chemicals. Expert Opin. Ther. Targets 2013, 17, 839–855. [Google Scholar] [CrossRef]
- Reis, M.M.S.; Moreira, A.C.; Sousa, M.; Mathur, P.; Oliveira, P.F.; Alves, M.G. Sertoli cell as a model in male reproductive toxicology: Advantages and disadvantages. J. Appl. Toxicol. 2015, 35, 870–883. [Google Scholar] [CrossRef]
- Lovaković, B.T. Cadmium, arsenic, and lead: Elements affecting male reproductive health. Curr. Opin. Toxicol. 2020, 19, 7–14. [Google Scholar] [CrossRef]
- De Angelis, C.; Galdiero, M.; Pivonello, C.; Salzano, C.; Gianfrilli, D.; Piscitelli, P.; Lenzi, A.; Colao, A.; Pivonello, R. The environment and male reproduction: The effect of cadmium exposure on reproductive function and its implication in fertility. Reprod. Toxicol. 2017, 73, 105–127. [Google Scholar] [CrossRef]
- Pavlova, E.; Atanassova, N. Impact of Cadmium on Male Fertility. Acta Morphol. Anthropol. 2018, 25, 108–116. [Google Scholar]
- Manfo, F.P.T.; Nantia, E.A.; Mathur, P.P. Effect of Environmental Contaminants on Mammalian Testis. Curr. Mol. Pharmacol. 2015, 7, 119–135. [Google Scholar] [CrossRef]
- Ramos-Treviño, J.; Bassol-Mayagoitia, S.; Hernández-Ibarra, J.A.; Ruiz-Flores, P.; Nava-Hernández, M.P. Toxic effect of cadmium, lead, and arsenic on the sertoli cell: Mechanisms of damage involved. DNA Cell Biol. 2018, 37, 600–608. [Google Scholar] [CrossRef]
- Plunk, E.C.; Richards, S.M. Endocrine-Disrupting Air Pollutants and Their Effects on the Hypothalamus-Pituitary-Gonadal Axis. Int. J. Mol. Sci. 2020, 21, 9191. [Google Scholar] [CrossRef]
- Vigeh, M.; Smith, D.; Hsu, P.-C. How does lead induce male infertility? Iran. J. Reprod. Med. 2011, 9, 1–8. [Google Scholar] [PubMed]
- Sheweita, S.; Tilmisany, A.; Al-Sawaf, H. Mechanisms of Male Infertility: Role of Antioxidants. Curr. Drug Metab. 2005, 6, 495–501. [Google Scholar] [CrossRef] [PubMed]
- Ko, E.Y.; Sabanegh, E.S.; Agarwal, A. Male infertility testing: Reactive oxygen species and antioxidant capacity. Fertil. Steril. 2014, 102, 1518–1527. [Google Scholar] [CrossRef] [PubMed]
- Zareba, P.; Colaci, D.S.; Afeiche, M.; Gaskins, A.J.; Jørgensen, N.; Mendiola, J.; Swan, S.H.; Chavarro, J.E. Semen quality in relation to antioxidant intake in a healthy male population. Fertil. Steril. 2013, 100, 1572–1579. [Google Scholar] [CrossRef]
- Young, S.; Eskenazi, B.; Marchetti, F.; Block, G.; Wyrobek, A. The association of folate, zinc and antioxidant intake with sperm aneuploidy in healthy non-smoking men. Hum. Reprod. 2008, 23, 1014–1022. [Google Scholar] [CrossRef]
- Tchounwou, P.B.; Yedjou, C.G.; Patlolla, A.K.; Sutton, D.J. Heavy Metal Toxicity and the Environment. Mol. Clin. Environ. Toxicol. 2012, 101, 133–164. [Google Scholar] [CrossRef]
- Mukherjee, A.; Sengupta, M.K.; Hossain, M.A.; Ahamed, S.; Das, B.; Nayak, B.; Lodh, D.; Rahman, M.M.; Chakraborti, D. Arsenic contamination in groundwater: A global perspective with emphasis on the Asian scenario. J. Health Popul. Nutr. 2006, 24, 142–163. [Google Scholar]
- Hamurcu, M.; Özcan, M.M.; Dursun, N.; Gezgin, S. Mineral and heavy metal levels of some fruits grown at the roadsides. Food Chem. Toxicol. 2010, 48, 1767–1770. [Google Scholar] [CrossRef]
- Radwan, M.A.; Salama, A.K. Market basket survey for some heavy metals in Egyptian fruits and vegetables. Food Chem. Toxicol. 2006, 44, 1273–1278. [Google Scholar] [CrossRef]
- Muñoz, O.; Bastias, J.M.; Araya, M.; Morales, A.; Orellana, C.; Rebolledo, R.; Velez, D. Estimation of the dietary intake of cadmium, lead, mercury, and arsenic by the population of Santiago (Chile) using a Total Diet Study. Food Chem. Toxicol. 2005, 43, 1647–1655. [Google Scholar] [CrossRef]
- Almela, C.; Algora, S.; Benito, V.; Clemente, M.J.; Devesa, V.; Súñer, M.A.; Vélez, D.; Montoro, R. Heavy Metal, Total Arsenic, and Inorganic Arsenic Contents of Algae Food Products. J. Agric. Food Chem. 2002, 50, 918–923. [Google Scholar] [CrossRef]
- Almutairi, M.; Alsaleem, T.; Jeperel, H.; Alsamti, M.; Alowaifeer, A.M. Determination of inorganic arsenic, heavy metals, pesticides and mycotoxins in Indian rice (Oryza sativa) and a probabilistic dietary risk assessment for the population of Saudi Arabia. Regul. Toxicol. Pharmacol. 2021, 125, 104986. [Google Scholar] [CrossRef]
- Hruska, K.S.; Furth, P.A.; Seifer, D.B.; Sharara, F.I.; Flaws, J.A. Environmental Factors in Infertility. Clin. Obstet. Gynecol. 2000, 43, 821–829. [Google Scholar] [CrossRef]
- Wirth, J.J.; Mijal, R.S. Adverse Effects of Low Level Heavy Metal Exposure on Male Reproductive Function. Syst. Biol. Reprod. Med. 2010, 56, 147–167. [Google Scholar] [CrossRef]
- Najafi, T.F.; Roudsari, R.L.; Namvar, F.; Ghanbarabadi, V.G.; Talasaz, Z.H.; Esmaeli, M. Air Pollution and Quality of Sperm: A Meta-Analysis. Iran. Red Crescent Med. J. 2015, 17, e26930. [Google Scholar] [CrossRef]
- Abarikwu, S.O. Causes and risk factors for male-factor infertility in Nigeria: A review. Afr. J. Reprod. Health 2013, 17, 150–166. [Google Scholar]
- Sengupta, P.; Nwagha, U.; Dutta, S.; Krajewska-Kulak, E.; Izuka, E. Evidence for decreasing sperm count in African population from 1965 to 2015. Afr. Health Sci. 2017, 17, 418–427. [Google Scholar] [CrossRef]
- Thompson, J.; Bannigan, J. Cadmium: Toxic effects on the reproductive system and the embryo. Reprod. Toxicol. 2008, 25, 304–315. [Google Scholar] [CrossRef]
- Rogers, J.M. Tobacco and pregnancy: Overview of exposures and effects. Birth Defects Res. Part C Embryo Today Rev. 2008, 84, 1–15. [Google Scholar] [CrossRef]
- Ren, T.; Chen, X.; Ge, Y.; Zhao, L.; Zhong, R. Determination of heavy metals in cigarettes using high-resolution continuum source graphite furnace atomic absorption spectrometry. Anal. Methods 2017, 9, 4033–4043. [Google Scholar] [CrossRef]
- Bjørklund, G.; Chirumbolo, S.; Dadar, M.; Pivina, L.; Lindh, U.; Butnariu, M.; Aaseth, J. Mercury exposure and its effects on fertility and pregnancy outcome. Basic Clin. Pharmacol. Toxicol. 2019, 125, 317–327. [Google Scholar] [CrossRef] [PubMed]
- Lavranos, G.; Balla, M.; Tzortzopoulou, A.; Syriou, V.; Angelopoulou, R. Investigating ROS sources in male infertility: A common end for numerous pathways. Reprod. Toxicol. 2012, 34, 298–307. [Google Scholar] [CrossRef] [PubMed]
- Martynowicz, H.; Skoczyńska, A.; Karczmarek-Wdowiak, B.; Andrzejak, R. Effects of cadmium on testis function. Med. Pr. 2005, 56, 167–174. [Google Scholar] [PubMed]
- Lettieri, G.; D’Agostino, G.; Mele, E.; Cardito, C.; Esposito, R.; Cimmino, A.; Giarra, A.; Trifuoggi, M.; Raimondo, S.; Notari, T.; et al. Discovery of the Involvement in DNA Oxidative Damage of Human Sperm Nuclear Basic Proteins of Healthy Young Men Living in Polluted Areas. Int. J. Mol. Sci. 2020, 21, 4198. [Google Scholar] [CrossRef]
- De Guglielmo, V.; Puoti, R.; Notariale, R.; Maresca, V.; Ausió, J.; Troisi, J.; Verrillo, M.; Basile, A.; Febbraio, F.; Piscopo, M. Alterations in the properties of sperm protamine-like II protein after exposure of Mytilus galloprovincialis (Lamarck 1819) to sub-toxic doses of cadmium. Ecotoxicol. Environ. Saf. 2019, 169, 600–606. [Google Scholar] [CrossRef]
- Hales, B.F.; Robaire, B. Review—Paternal exposure to drugs and environmental chemicals: Effects on progeny outcome. J. Androl. 2001, 22, 927–936. [Google Scholar] [CrossRef]
- Qiao, Z.-D.; Dai, J.-B.; Wang, Z.-X. The hazardous effects of tobacco smoking on male fertility. Asian J. Androl. 2015, 17, 954–960. [Google Scholar] [CrossRef]
- Ashiru, O.; Odusanya, O.O. Fertility and occupational hazards: Review of the literature. Afr. J. Reprod. Health 2009, 13, 159–165. [Google Scholar]
- Sheiner, E.K.; Sheiner, E.; Hammel, R.D.; Potashnik, G.; Carel, R. Effect of Occupational Exposures on Male Fertility: Literature Review. Ind. Health 2003, 41, 55–62. [Google Scholar] [CrossRef]
- Bonde, J.P. Male reproductive organs are at risk from environmental hazards. Asian J. Androl. 2010, 12, 152–156. [Google Scholar] [CrossRef]
- Jensen, T.K.; Bonde, J.P.; Joffe, M. The influence of occupational exposure on male reproductive function. Occup. Med. 2006, 56, 544–553. [Google Scholar] [CrossRef]
- Benoff, S.; Cooper, G.W.; Centola, G.M.; Jacob, A.; Hershlag, A.; Hurley, I.R. Metal ions and human sperm mannose receptors. Andrologia 2000, 32, 317–329. [Google Scholar] [CrossRef]
- Ghaffari, M.A.; Motlagh, B. In vitro effect of lead, silver, tin, mercury, indium and bismuth on human sperm creatine kinase activity: A presumable mechanism for men infertility. Iran. Biomed. J. 2011, 15, 38–43. [Google Scholar]
- Hardneck, F.; Israel, G.; Pool, E.; Maree, L. Quantitative assessment of heavy metal effects on sperm function using computer-aided sperm analysis and cytotoxicity assays. Andrologia 2018, 50, e13141. [Google Scholar] [CrossRef]
- He, Y.; Zou, Q.; Chen, H.; Weng, S.; Luo, T.; Zeng, X. Lead Inhibits Human Sperm Functions by Reducing the Levels of Intracellular Calcium, cAMP, and Tyrosine Phosphorylation. Tohoku J. Exp. Med. 2016, 238, 295–303. [Google Scholar] [CrossRef]
- Huang, Y.; Tseng, W.; Lin, T. In Vitro Effects of Metal Ions (Fe2+, Mn2+, Pb2+) on Sperm Motility and Lipid Peroxidation in Human Semen. J. Toxicol. Environ. Health A 2001, 62, 259–267. [Google Scholar] [CrossRef]
- Marchiani, S.; Tamburrino, L.; Farnetani, G.; Muratori, M.; Vignozzi, L.; Baldi, E. Acute effects on human sperm exposed in vitro to cadmium chloride and diisobutyl phthalate. Reproduction 2019, 158, 281–290. [Google Scholar] [CrossRef]
- Li, Y.; Wu, J.; Yuan, W.; Zhou, W.; Gao, E. Are serum zinc and copper levels related to semen quality? Fertil. Steril. 2008, 89, 1008–1011. [Google Scholar] [CrossRef]
- Telišman, S.; Čolak, B.; Pizent, A.; Jurasović, J.; Cvitković, P. Reproductive toxicity of low-level lead exposure in men. Environ. Res. 2007, 105, 256–266. [Google Scholar] [CrossRef]
- Li, Y.; Wu, J.; Zhou, W.; Gao, E. Effects of manganese on routine semen quality parameters: Results from a population-based study in China. BMC Public Health 2012, 12, 919. [Google Scholar] [CrossRef]
- Kumar, R.; Pant, N.; Srivastava, S.P. Chlorinated pesticides and heavy metals in human semen. Int. J. Androl. 2000, 23, 145–149. [Google Scholar] [CrossRef]
- Dickman, M.; Leung, K. Mercury and organochlorine exposure from fish consumption in Hong Kong. Chemosphere 1998, 37, 991–1015. [Google Scholar] [CrossRef]
- Dickman, M.; Leung, C.; Leong, M. Hong Kong male subfertility links to mercury in human hair and fish. Sci. Total Environ. 1998, 214, 165–174. [Google Scholar] [CrossRef]
- Pant, N.; Pant, A.B.; Chaturvedi, P.K.; Shukla, M.; Mathur, N.; Gupta, Y.K.; Saxena, D.K. Semen quality of environmentally exposed human population: The toxicological consequence. Environ. Sci. Pollut. Res. 2013, 20, 8274–8281. [Google Scholar] [CrossRef]
- Wang, Y.-X.; Wang, P.; Feng, W.; Liu, C.; Yang, P.; Chen, Y.-J.; Sun, L.; Sun, Y.; Yue, J.; Gu, L.-J.; et al. Relationships between seminal plasma metals/metalloids and semen quality, sperm apoptosis and DNA integrity. Environ. Pollut. 2017, 224, 224–234. [Google Scholar] [CrossRef]
- Li, Y.; Wu, J.; Zhou, W.; Gao, E. Association between environmental exposure to cadmium and human semen quality. Int. J. Environ. Health Res. 2015, 26, 175–186. [Google Scholar] [CrossRef]
- Jeng, H.A.; Huang, Y.-L.; Pan, C.-H.; Diawara, N. Role of low exposure to metals as male reproductive toxicants. Int. J. Environ. Health Res. 2014, 25, 405–417. [Google Scholar] [CrossRef]
- Kuo, H.-W.; Wang, C.-S.; Lai, J.-S. Semen quality in workers with long-term lead exposure: A preliminary study in Taiwan. Sci. Total Environ. 1997, 204, 289–292. [Google Scholar] [CrossRef]
- Morán-Martínez, J.; Carranza-Rosales, P.; Morales-Vallarta, M.; Heredia-Rojas, J.A.; Bassol-Mayagoitia, S.; Betancourt-Martinez, N.D.; Cerda-Flores, R.M. Chronic environmental exposure to lead affects semen quality in a Mexican men population. Iran. J. Reprod. Med. 2013, 11, 267–274. [Google Scholar] [PubMed]
- Naha, N.; Chowdhury, A.R. Inorganic lead exposure in battery and paint factory: Effect on human sperm structure and functional activity. J. UOEH 2006, 28, 157–171. [Google Scholar] [CrossRef]
- Naha, N.; Bhar, R.B.; Mukherjee, A.; Chowdhury, A.R. Structural alteration of spermatozoa in the persons employed in lead acid battery factory. Indian J. Physiol. Pharmacol. 2005, 49, 153–162. [Google Scholar] [PubMed]
- Hanf, V.; Forstmann, A.; Costea, J.E.; Schieferstein, G.; Fischer, I.; Schweinsberg, F. Mercury in urine and ejaculate in husbands of barren couples. Toxicol. Lett. 1996, 88, 227–231. [Google Scholar] [CrossRef]
- Keck, C.; Bramkamp, G.; Behre, H.M.; Muller, C.; Jockenhovel, F.; Nieschlag, E. Lack of Correlation between Cadmium in Seminal Plasma and Fertility Status of Nonexposed Individuals and 2 Cadmium-Exposed Patients. Reprod. Toxicol. 1995, 9, 35–40. [Google Scholar] [CrossRef]
- Mitra, S.; Varghese, A.C.; Mandal, S.; Bhattacharyya, S.; Nandi, P.; Rahman, S.M.; Kar, K.K.; Saha, R.; Roychoudhury, S.; Murmu, N. Lead and cadmium exposure induces male reproductive dysfunction by modulating the expression profiles of apoptotic and survival signal proteins in tea-garden workers. Reprod. Toxicol. 2020, 98, 134–148. [Google Scholar] [CrossRef]
- Wijesekara, G.; Fernando, D.; Wijerathna, S.; Bandara, N. Environmental and occupational exposures as a cause of male infertility: A caveat. Ceylon Med. J. 2015, 60, 52–56. [Google Scholar] [CrossRef]
- Elsamanoudy, A.Z.; Shaalan, D.; Gaballah, M.; El-Atta, H.M.A.; Helaly, A.M. Possible Effects of Metallosis on Spermatozoal Apoptotic Genes Expression in Individuals with Intramedullary Nailing Prosthesis. Biol. Trace Elem. Res. 2014, 158, 334–341. [Google Scholar] [CrossRef]
- He, Y.; Zou, L.; Luo, W.; Yi, Z.; Yang, P.; Yu, S.; Liu, N.; Ji, J.; Guo, Y.; Liu, P.; et al. Heavy metal exposure, oxidative stress and semen quality: Exploring associations and mediation effects in reproductive-aged men. Chemosphere 2020, 244, 125498. [Google Scholar] [CrossRef]
- Inhorn, M.C.; King, L.; Nriagu, J.O.; Kobeissi, L.; Hammoud, N.; Awwad, J.; Abu-Musa, A.A.; Hannoun, A.B. Occupational and environmental exposures to heavy metals: Risk factors for male infertility in Lebanon? Reprod. Toxicol. 2008, 25, 203–212. [Google Scholar] [CrossRef]
- Li, Y.; Gao, Q.; Li, M.; Li, M.; Gao, X. Cadmium, Chromium, and Copper Concentration plus Semen-Quality in Environmental Pollution Site, China. Iran. J. Public Health 2014, 43, 35–41. [Google Scholar]
- Shi, Y.; Gaurab, P.; Wang, W.; Yan, J.; Sun, Z.; Zhang, Y.; Liu, J.; Liu, X.; Zheng, D. Interaction effect of polycyclic aromatic hydrocarbon metabolites and cadmium on semen quality in nonsmokers. Environ. Sci. Pollut. Res. 2020, 27, 33990–33997. [Google Scholar] [CrossRef]
- Telišman, S.; Cvitković, P.; Jurasović, J.; Pizent, A.; Gavella, M.; Ročić, B. Semen quality and reproductive endocrine function in relation to biomarkers of lead, cadmium, zinc, and copper in men. Environ. Health Perspect. 2000, 108, 45–53. [Google Scholar] [CrossRef]
- Danadevi, K.; Rozati, R.; Reddy, P.; Grover, P. Semen quality of Indian welders occupationally exposed to nickel and chromium. Reprod. Toxicol. 2003, 17, 451–456. [Google Scholar] [CrossRef]
- Kahraman, S.; Hassa, H.; Karataş, A.; Ilgin, H. The effect of blood and seminal plasma heavy metal and trace element levels on sperm quality. Turk. Klin. J. Med. Sci. 2012, 32, 1560–1568. [Google Scholar] [CrossRef][Green Version]
- Li, C.-J.; Yeh, C.-Y.; Chen, R.-Y.; Tzeng, C.-R.; Han, B.-C.; Chien, L.-C. Biomonitoring of blood heavy metals and reproductive hormone level related to low semen quality. J. Hazard. Mater. 2015, 300, 815–822. [Google Scholar] [CrossRef]
- Pant, N.; Upadhyay, G.; Pandey, S.; Mathur, N.; Saxena, D.; Srivastava, S. Lead and cadmium concentration in the seminal plasma of men in the general population: Correlation with sperm quality. Reprod. Toxicol. 2003, 17, 447–450. [Google Scholar] [CrossRef]
- Sukhn, C.; Awwad, J.; Ghantous, A.; Zaatari, G. Associations of semen quality with non-essential heavy metals in blood and seminal fluid: Data from the Environment and Male Infertility (EMI) study in Lebanon. J. Assist. Reprod. Genet. 2018, 35, 1691–1701. [Google Scholar] [CrossRef]
- Riaz, M.; Mahmood, Z.; Shahid, M.; Saeed, M.U.Q.; Tahir, I.M.; Shah, S.A.; Munir, N.; El-Ghorab, A. Impact of reactive oxygen species on antioxidant capacity of male reproductive system. Int. J. Immunopathol. Pharmacol. 2016, 29, 421–425. [Google Scholar] [CrossRef]
- Kim, K.; Bloom, M.S.; Kruger, P.C.; Parsons, P.J.; Arnason, J.G.; Byun, Y.; Goins, S.; Fujimoto, V.Y. Toxic metals in seminal plasma and in vitro fertilization (IVF) outcomes. Environ. Res. 2014, 133, 334–337. [Google Scholar] [CrossRef]
- Mendiola, J.; Moreno, J.M.; Roca, M.; Vergara-Juárez, N.; Martínez-García, M.J.; García-Sánchez, A.; Elvira-Rendueles, B.; Moreno-Grau, S.; López-Espín, J.J.; Ten, J.; et al. Relationships between heavy metal concentrations in three different body fluids and male reproductive parameters: A pilot study. Environ. Health 2011, 10, 6. [Google Scholar] [CrossRef]
- Mínguez-Alarcón, L.; Afeiche, M.C.; Williams, P.L.; Arvizu, M.; Tanrikut, C.; Amarasiriwardena, C.J.; Ford, J.B.; Hauser, R.; Chavarro, J.E. Hair mercury (Hg) levels, fish consumption and semen parameters among men attending a fertility center. Int. J. Hyg. Environ. Health 2018, 221, 174–182. [Google Scholar] [CrossRef]
- Slivkova, J.; Popelkova, M.; Massanyi, P.; Toporcerova, S.; Stawarz, R.; Formicki, G.; Lukáč, N.; Putała, A.; Guzik, M. Concentration of trace elements in human semen and relation to spermatozoa quality. J. Environ. Sci. Health Part A 2009, 44, 370–375. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.; Wang, M.; Deng, Y.; Qiu, J.; Zhang, X.; Tan, J. Associations of toxic and essential trace elements in serum, follicular fluid, and seminal plasma with In vitro fertilization outcomes. Ecotoxicol. Environ. Saf. 2020, 204, 110965. [Google Scholar] [CrossRef] [PubMed]
- Zafar, A.; Eqani, S.A.M.A.S.; Bostan, N.; Cincinelli, A.; Tahir, F.; Shah, S.T.A.; Hussain, A.; Alamdar, A.; Huang, Q.; Peng, S.; et al. Toxic metals signature in the human seminal plasma of Pakistani population and their potential role in male infertility. Environ. Geochem. Health 2015, 37, 515–527. [Google Scholar] [CrossRef] [PubMed]
- Zeng, Q.; Feng, W.; Zhou, B.; Wang, Y.-X.; He, X.-S.; Yang, P.; You, L.; Yue, J.; Li, Y.-F.; Lu, W.-Q. Urinary metal concentrations in relation to semen quality: A cross-sectional study in China. Environ. Sci. Technol. 2015, 49, 5052–5059. [Google Scholar] [CrossRef]
- Zhou, Y.; Fu, X.-M.; He, D.-L.; Zou, X.-M.; Wu, C.-Q.; Guo, W.-Z.; Feng, W. Evaluation of urinary metal concentrations and sperm DNA damage in infertile men from an infertility clinic. Environ. Toxicol. Pharmacol. 2016, 45, 68–73. [Google Scholar] [CrossRef]
- Zhang, Y.; Li, S.; Li, S. Relationship between cadmium content in semen and male infertility: A meta-analysis. Environ. Sci. Pollut. Res. 2018, 26, 1947–1953. [Google Scholar] [CrossRef]
- Bloom, M.S.; Louis, G.B.; Sundaram, R.; Maisog, J.M.; Steuerwald, A.J.; Parsons, P. Birth outcomes and background exposures to select elements, the Longitudinal Investigation of Fertility and the Environment (LIFE). Environ. Res. 2015, 138, 118–129. [Google Scholar] [CrossRef]
- Louis, G.M.B.; Sundaram, R.; Schisterman, E.F.; Sweeney, A.M.; Lynch, C.; Gore-Langton, R.E.; Chen, Z.; Kim, S.; Caldwell, K.L.; Barr, D.B. Heavy metals and couple fecundity, the LIFE Study. Chemosphere 2012, 87, 1201–1207. [Google Scholar] [CrossRef]
- Wu, H.-M.; Lin-Tan, D.-T.; Wang, M.-L.; Huang, H.-Y.; Lee, C.-L.; Wang, H.-S.; Soong, Y.-K.; Lin, J.-L. Lead level in seminal plasma may affect semen quality for men without occupational exposure to lead. Reprod. Biol. Endocrinol. 2012, 10, 91. [Google Scholar] [CrossRef]
- Kumar, S.; Mishra, V.; Thaker, R.; Gor, M.; Perumal, S.; Joshi, P.; Sheth, H.; Shaikh, I.; Gautam, A.K.; Verma, Y. Role of environmental factors & oxidative stress with respect to in vitro fertilization outcome. Indian J. Med. Res. 2018, 148, S125–S133. [Google Scholar] [CrossRef]



| Keyword | Pubmed | Scopus | WOS |
|---|---|---|---|
| Male Fertility | 38,256 | 186,504 | 52,261 |
| Heavy metals | 345,873 | 513,286 | 199,667 |
| Human Spermatogenesis | 9211 | 54,300 | 199,667 |
| Human Sperm | 35,460 | 133,717 | 46,870 |
| Heavy metals and Human Spermatogenesis | 101 | 1144 | 69 |
| Heavy metals and Human Sperm | 573 | 2972 | 222 |
| Heavy metals and Male Fertility | 428 | 2722 | 290 |
| Symbol | Chemical Element | Symbol | Chemical Element |
|---|---|---|---|
| Ag | Silver | Mo | Molybdenum |
| Al | Aluminum | Ni | Nickel |
| As | Arsenic | Pb | Lead |
| Ba | Barium | Pt | Platinum |
| Be | Beryllium | Sb | Antimony |
| Bi | Bismuth | Sc | Scandium |
| Ca | Calcium | Se | Selenium |
| Cd | Cadmium | Sn | Tin |
| Co | Cobalt | Sr | Strontium |
| Cr | Chromium | Te | Tellurium |
| Cs | Cesium | Ti | Titanium |
| Cu | Copper | Tl | Thallium |
| Fe | Iron | U | Uranium |
| Hg | Mercury | V | Vanadium |
| In | Indium | W | Tungsten |
| Mg | Magnesium | Zn | Zinc |
| Mn | Manganese |
| Ref. | Study Groups | Biological Matrix | Detection Method | Metal Profile | Main Findings |
|---|---|---|---|---|---|
| [79] | Men from six cities of China (n = 1179) | SE | AAS | Zn and Cu |
|
| [80] | Croatian men with no occupational exposure (n = 240) | SP, B and SE | BPb and BCd by AAS. SECu and SEZn by F-AAS. Se by ETA-AAS. SEPZn by bichromatic analyzer. | BCd and BPb, SECu, SEZn and SESe. Zn on SP |
|
| [81] | Healthy volunteers from China (n = 1179) | SE | ICP-MS | Mn |
|
| [82] | Samples (n = 50) from the general population of Lucknow (India) | S | GFAAS | Cd and Pb |
|
| Ref. | Exposure | Study Groups | Biological Matrix | Detection Method | Metal Profile | Main Findings |
|---|---|---|---|---|---|---|
| [83] | E | Infertile men (n = 117) and fertile men as control group (n = 67) | H | ICP-MS | Hg |
|
| [84] | E | Infertile men (n = 117) and fertile men as control group (n = 49) | H | ICP-MS | Mn, Fe, Zn, Cu, Cd, Pb, Ni, Hg and Cr |
|
| [85] | E | Infertile men (n = 150) and fertile men as control group (n = 60) | S | AAS | Pb and Cd |
|
| [86] | E | Men recruited from a reproductive medicine center (n = 746) | SP | ICP-MS | Al, Cr, Mn, Fe, Co, Ni, Cu, Zn, As, Se, Mo, Cd, Sn, Sb, W, Tl, Pb and U |
|
| [87] | E | Men from the general population (n = 587) | SE | ICP-MS | Cd |
|
| [88] | E | Normozoospermic men from general population (n = 62) | SP and U | F-AAS, ETA-AAS and HG-AAS | Zn, Cu, Cd, As, Se and Pb |
|
| [89] | O | Exposed men (n = 5) and fertile and unexposed men as control group (n = 8) | B and S | AAS | Pb |
|
| [90] | E | Exposed group (n = 20) and non-exposed group (n = 27) as control group | B and S | GFAAS | Pb |
|
| [91] | O | Low occupationally exposed group (n = 30) with 7–10 years exposure for 8 hours per day and high exposed group (n = 50), with more than 10–15 years of lead exposure.; non-occupationally exposed as control group (n = 50) | B and S | AAS | Pb |
|
| [92] | O | Low exposed group with 7–10 years exposure (n = 30) and high exposed group with exposure period of more than 10–15 years (n = 50); 40 non-occupationally exposed as control group | B and S | GFAAS | Pb |
|
| [93] | O | Husbands of women going though infertility treatment (n = 80) and workers from a thermometer manufacturing plant as exposed control group (n = 7) | S and U | CV-AAS | Hg |
|
| [94] | O | Men with proven fertility (n = 12), normozoospermic patients (n = 44), unselected patients of an infertility clinic (n = 118) and industrial workers with occupational exposure to cadmium (n = 2) | SP | ETA-ASS | Cd |
|
| [95] | O | Male tea garden workers (n = 200) and samples from age-matched donors as control group (n = 200) | S | F-AAS | Pb and Cd |
|
| [96] | E and O | Male partners (n = 300) of couples investigated for infertility | SP | GFAAS | Pb and Cd |
|
| [97] | E | Infertile men with intramedullary nailing prosthesis (IMN) (n = 60) and age-matched healthy men as control group (n = 30) | SP | ICP-MS | Co, Cr and Mo |
|
| [98] | E | Male partners in couples from a reproductive medicine center (n = 1247) | U | ICP-MS | As, Cd and Pb |
|
| [99] | E and O | Infertile men (n = 74) and fertile men as control group (n = 76) | B, SP and U | ICP-MS | As, Mn, Co, Cd, Pb, Zn and Se |
|
| [100] | E | Exposed men (n = 30) and control groups: men from towns 100 km away (n = 32, control group one) and 200 km away (n = 33, control group two) | SP | GFAAS | Cd, Cr and Cu |
|
| [101] | E | Non-smoking males visiting infertility clinics (n = 333) | U | ICP-MS | Cd, Cr, Mn, Fe, Co, Ni, Cu, Zn, Sr, Mo, Sn, Sb, Ba, W, Tl, Pb and U |
|
| [102] | O | Workers from plants with a range of exposure to Pb (from no exposure to moderate Pb exposure) (n = 98) and no likely exposure (n = 51) | SP, B and SE | AAS | BCd, SZn, SfZn, Scu |
|
| [103] | O | Welders workers (n = 57) and 57 controls (n = 57) | B | ICP-MS | Ni and Cr |
|
| Ref. | Study Groups | Biological Matrix | Detection Method | Metal Profile | Main Findings |
|---|---|---|---|---|---|
| [104] | Men with a low seminal quality (n = 42) and normozoospermic cases (n = 10) | WB, SP and BP | Polarized Zeeman AAS | Zn, Cd, Pb, Cu |
|
| [105] | Low-quality semen group (n = 59) and high-quality semen group (n = 95) from a reproductive medical center. | B | ICP-MS | Pb, Cd, Cr, Se, Fe, Cu and Zn |
|
| [106] | Infertile male partners (oligospermia n = 17, oligoasthenospermia n = 12, asthenospermia n = 12, azoospermia n = 9) and 50 men with proven fertility as a control group | SP | AAS | Cd and Pb |
|
| [107] | Low (n = 61) and normal (n = 55) quality semen groups | S and B | ICP-MS | Pb, Cd, As, Ba, Hg and U |
|
| [108] | Infertile men (n = 20) and fertile male volunteers as a control group (n = 20) | SP and SE | AAS | Se, Pb and Cd |
|
| [109] | Men attending an in vitro fertilization (IVF) treatment (n = 30) | SP | ICP-MS | Hg, Cd and Pb |
|
| [110] | Case subjects (n = 30) with oligo-astheno-teratozoospermia and normozoospermic men (n = 31) as control subjects, all attending fertility clinics | SP, B and WB | Anodic stripping voltammetry and AAS | Cd, Pb and Hg |
|
| [111] | Men attending an accademic fertility center (n = 129) | H | Direct Mercury Analyzer 80 | Hg |
|
| [112] | Men (n = 47) undergoing semen analysis in an infertility center | S | Cd and Pb were determined by the voltametric method. Mg, Cu and Zn by F-AAS | Cd, Pb, Ni, Fe, Mg, Cu and Zn |
|
| [113] | Couples (n = 104) from China | SP | ICP-MS | Cr, As, Se, Ni Cd and Pb |
|
| [114] | Men with normozoospermia (n = 25) as a control group, oligozoospermia (n = 25) and azoospermia (n = 25) | SP | ICP-MS | Mg, Ca, Al, Ti, V, Cr, Mn, Fe, Co, Ni, Cu, Zn, Sr, Cd, Sn, Sb, Ba, Hg and Pb |
|
| [115] | Men from an infertility clinic (n = 349) | U | ICP-MS | As, Cd, Co, Cr, Cu, Fe, Pb, Mn, Mo, Hg, Ni, Se and Zn |
|
| [116] | Infertile men from an infertility clinic (n = 207) | U | ICP-MS | As, Cd, Co, Cr, Cu, Fe, Pb, Mn, Mo, Hg, Ni, Se and Zn |
|
| Ref. | Exposure | Study Groups | Biological Matrix | Detection Method | Metal Profile | Main Findings |
|---|---|---|---|---|---|---|
| [118] | Pre-conception parental exposures | A cohort of couples (n = 501), including 235 singletons born to 347 couples | B and U | ICP-MS | Pb, Cd and total Hg in blood. Sb, As, Ba, Be, Cd, Cs, Cr, Co, Cu, Pb, Mn, Mo, Ni, Pt, Se, Te, Tl, Sn, W, U, Zn in urine. |
|
| [119] | Effect of heavy metals at environmentally relevant concentrations on couple fecundity | Couples (n = 501) desiring pregnancy | B | ICP-MS | Cd, Pb and Hg |
|
| [120] | No | Couples (n = 103) who underwent IVF/intracytoplasmic sperm injection (ICSI) treatment in a reproduction center | S | ICP-MS | Cr, Ni, As, Se, Cd and Pb |
|
| [121] | Evaluation of the role of oxidative stress in lifestyle and environmental factors | Couples (n = 253) from an IVF center | B, SE and SP | AAS | Pb, Cd, Cu and Zn |
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
López-Botella, A.; Velasco, I.; Acién, M.; Sáez-Espinosa, P.; Todolí-Torró, J.-L.; Sánchez-Romero, R.; Gómez-Torres, M.J. Impact of Heavy Metals on Human Male Fertility—An Overview. Antioxidants 2021, 10, 1473. https://doi.org/10.3390/antiox10091473
López-Botella A, Velasco I, Acién M, Sáez-Espinosa P, Todolí-Torró J-L, Sánchez-Romero R, Gómez-Torres MJ. Impact of Heavy Metals on Human Male Fertility—An Overview. Antioxidants. 2021; 10(9):1473. https://doi.org/10.3390/antiox10091473
Chicago/Turabian StyleLópez-Botella, Andrea, Irene Velasco, Maribel Acién, Paula Sáez-Espinosa, José-Luis Todolí-Torró, Raquel Sánchez-Romero, and María José Gómez-Torres. 2021. "Impact of Heavy Metals on Human Male Fertility—An Overview" Antioxidants 10, no. 9: 1473. https://doi.org/10.3390/antiox10091473
APA StyleLópez-Botella, A., Velasco, I., Acién, M., Sáez-Espinosa, P., Todolí-Torró, J.-L., Sánchez-Romero, R., & Gómez-Torres, M. J. (2021). Impact of Heavy Metals on Human Male Fertility—An Overview. Antioxidants, 10(9), 1473. https://doi.org/10.3390/antiox10091473