SiONx Coating Regulates Mesenchymal Stem Cell Antioxidant Capacity via Nuclear Erythroid Factor 2 Activity under Toxic Oxidative Stress Conditions
Abstract
1. Introduction
2. Materials and Methods
2.1. Fabrication of the Coatings
2.2. In Vitro Studies
2.3. Statistical Methods
3. Results
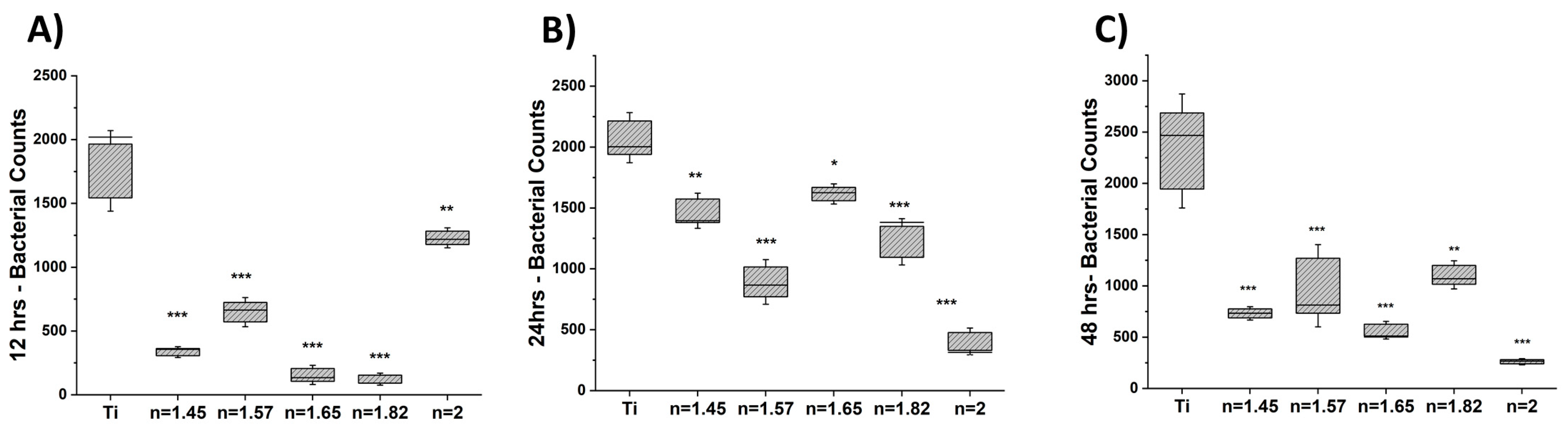
3.1. Bacteriostatic Effect
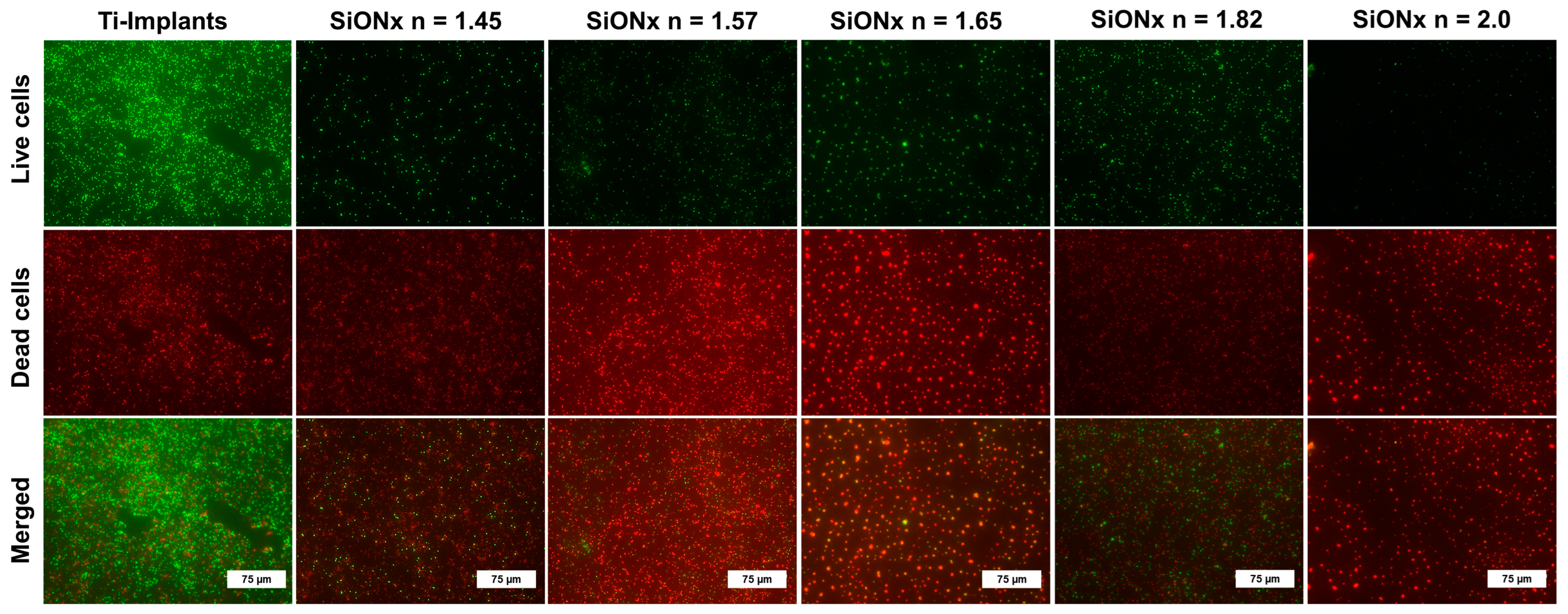
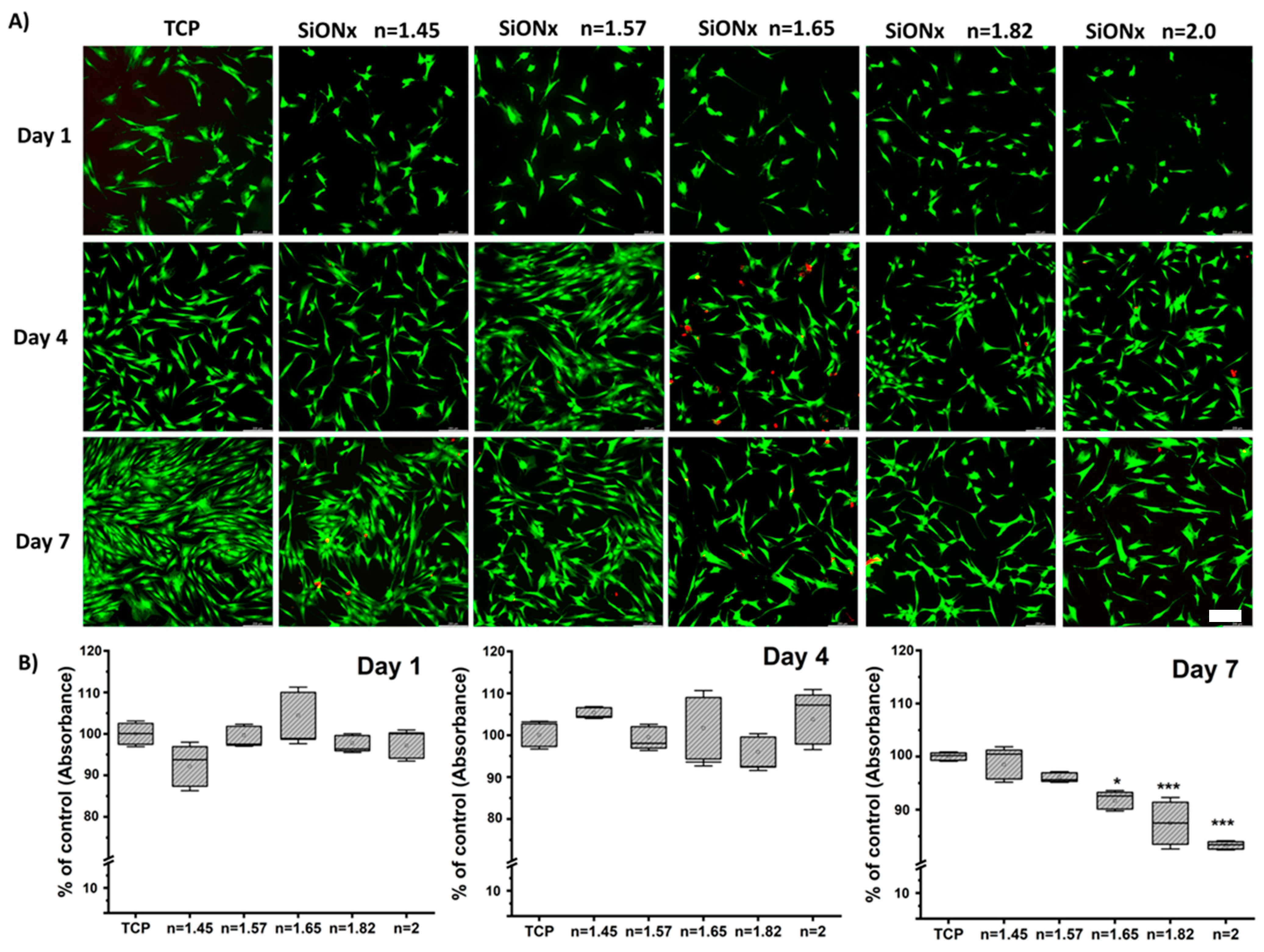
3.2. Cell Viability and Proliferation under Normal Conditions
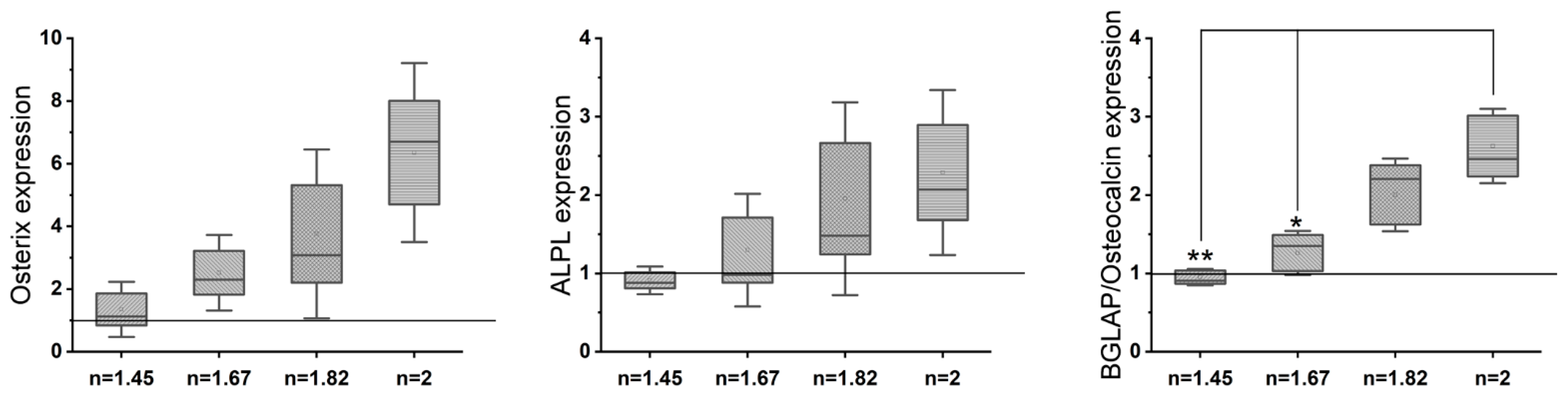
3.3. Osteogenic Differentiation with Increasing N/O Ratio in SiONx Surfaces
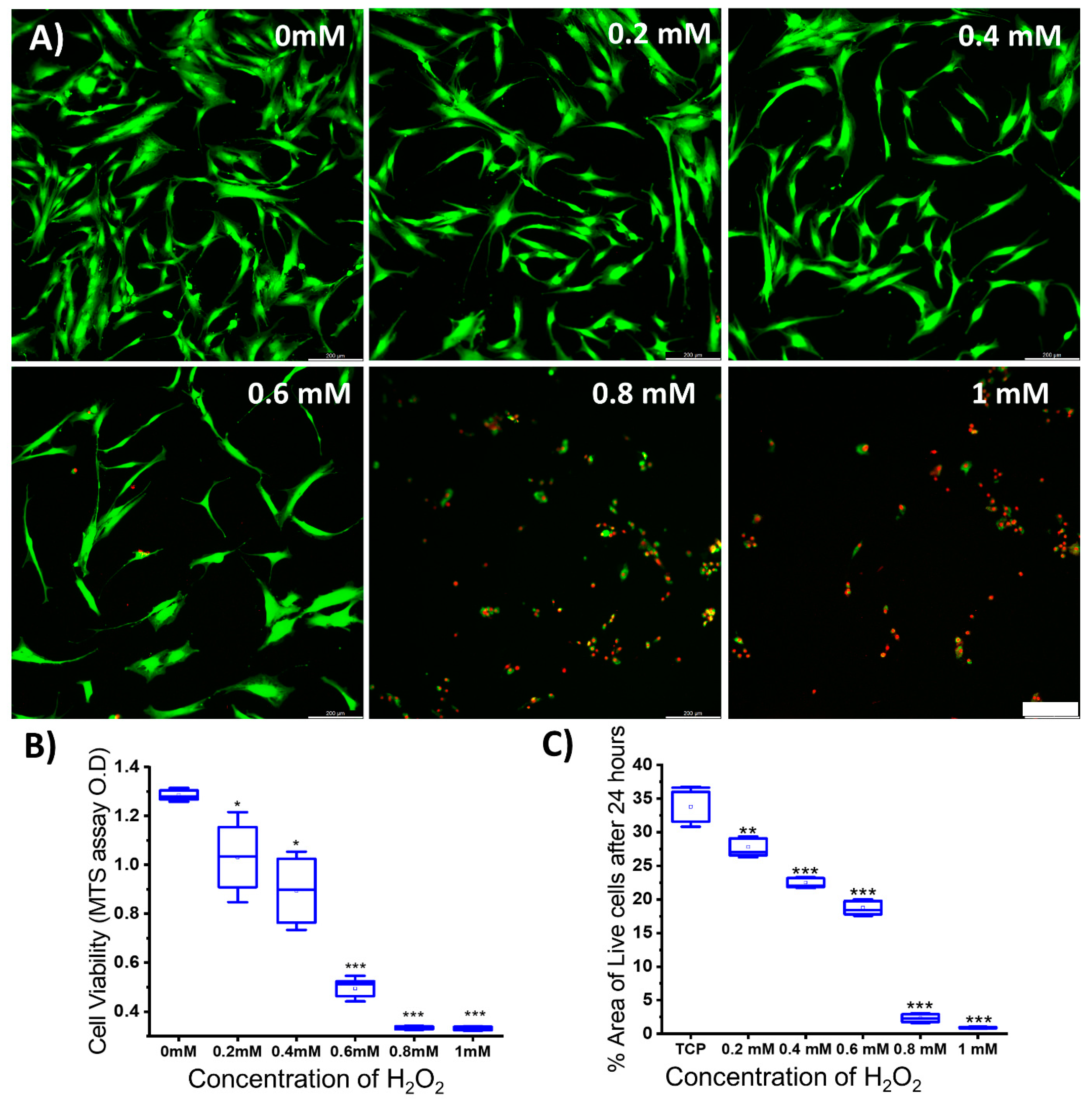
3.4. Determining Minimal H2O2 Concentration for Inducing Oxidative Stress in MSCs
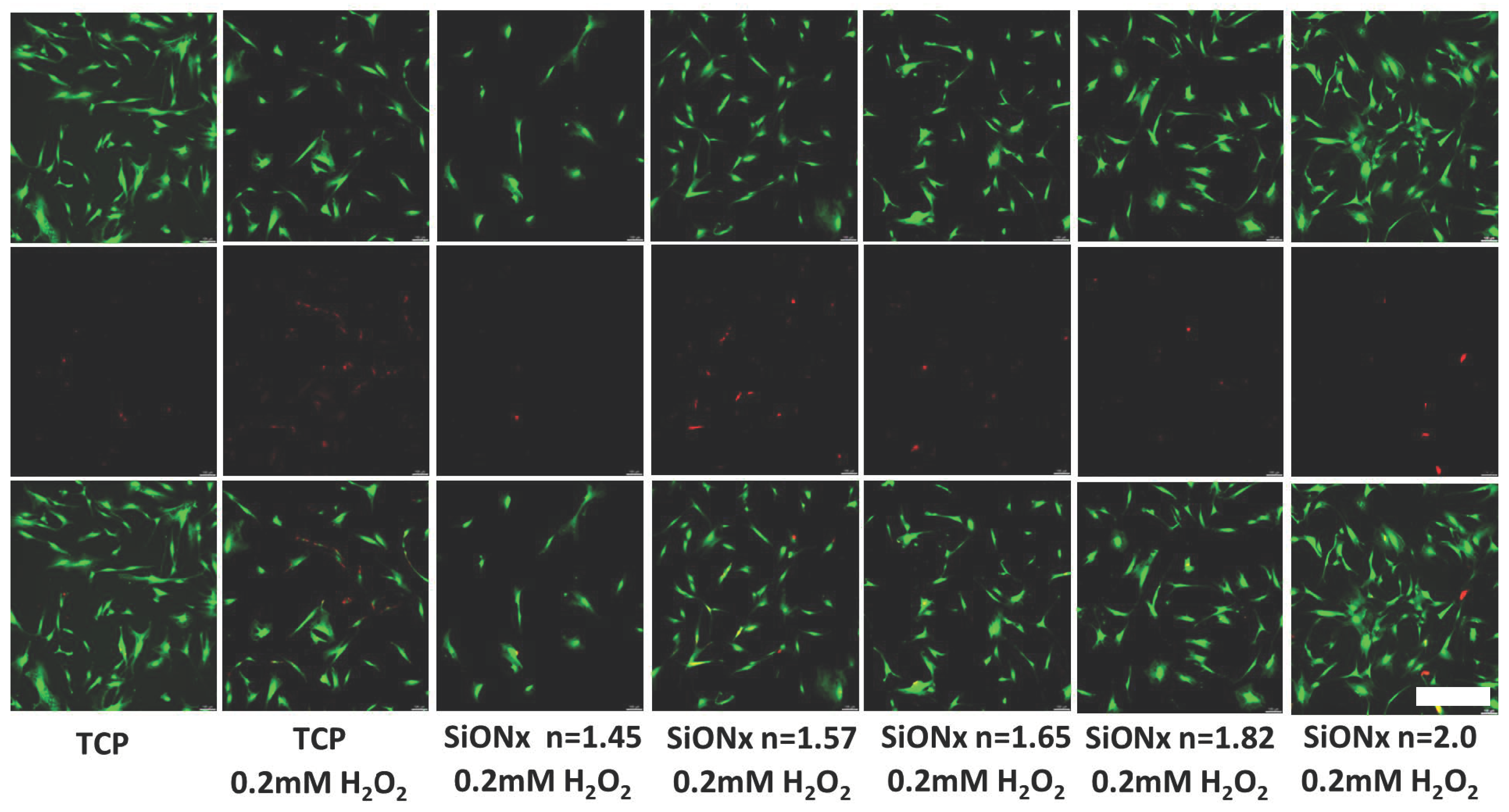
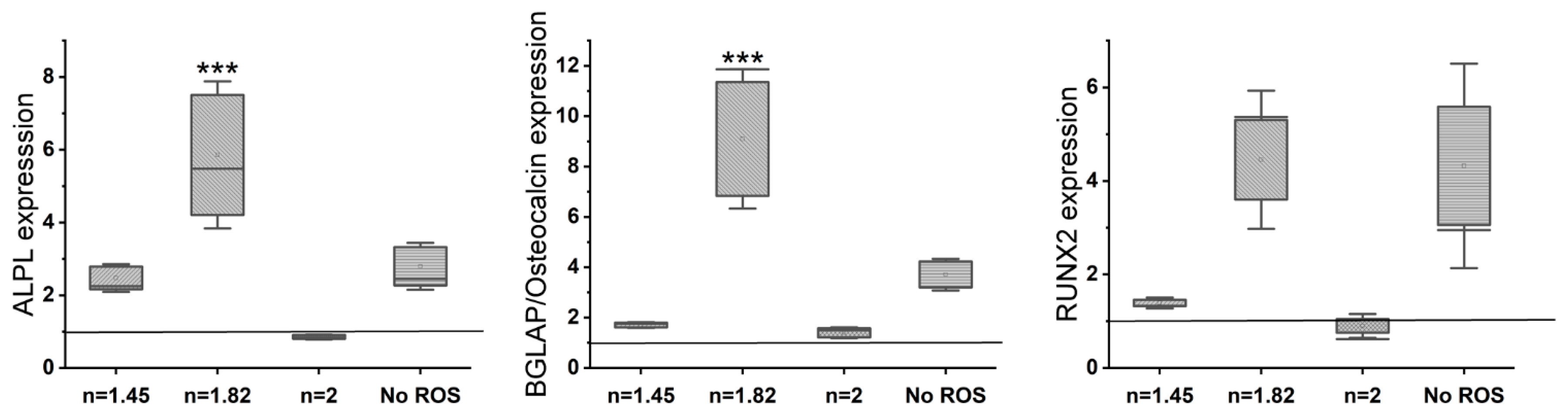
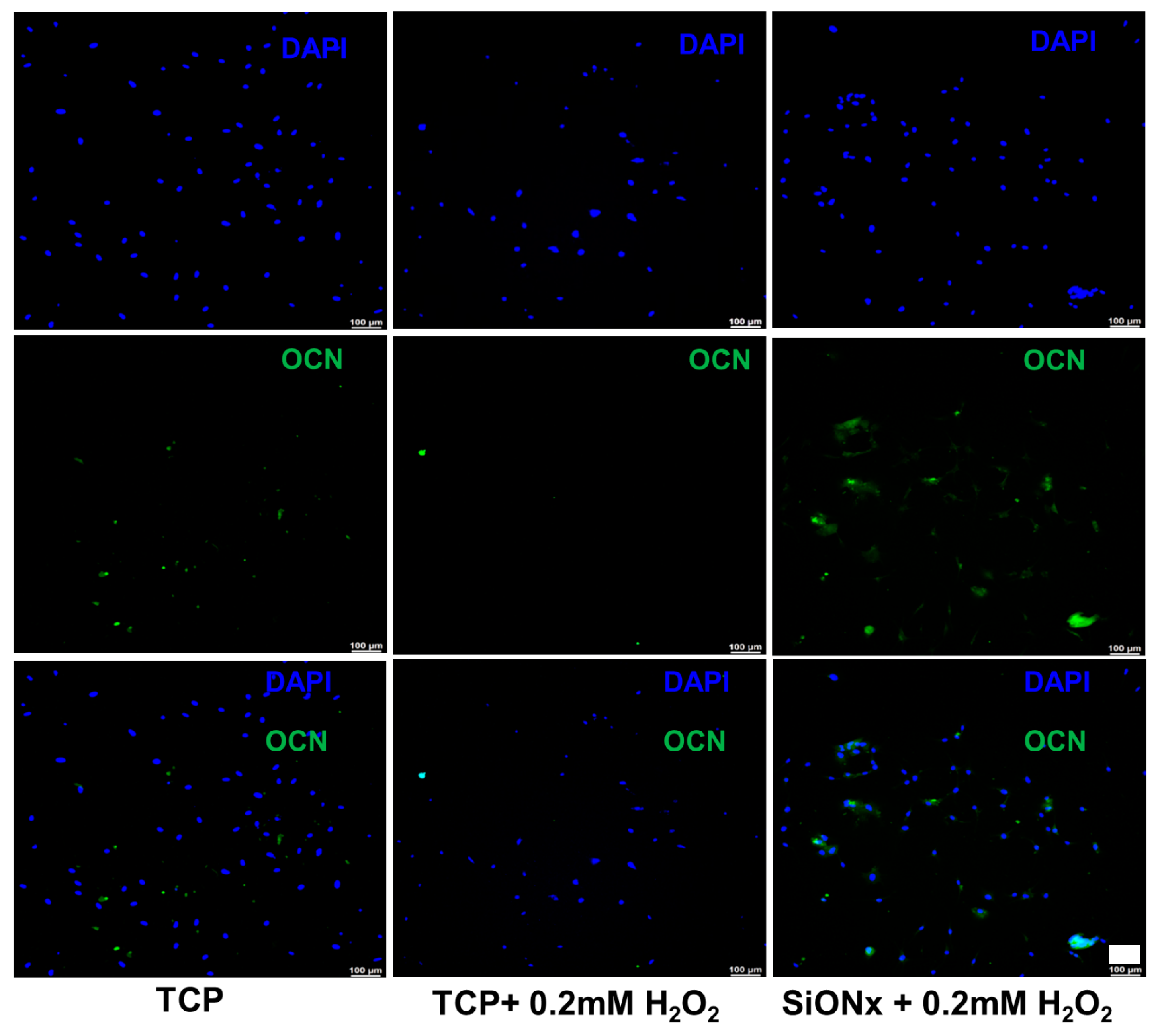
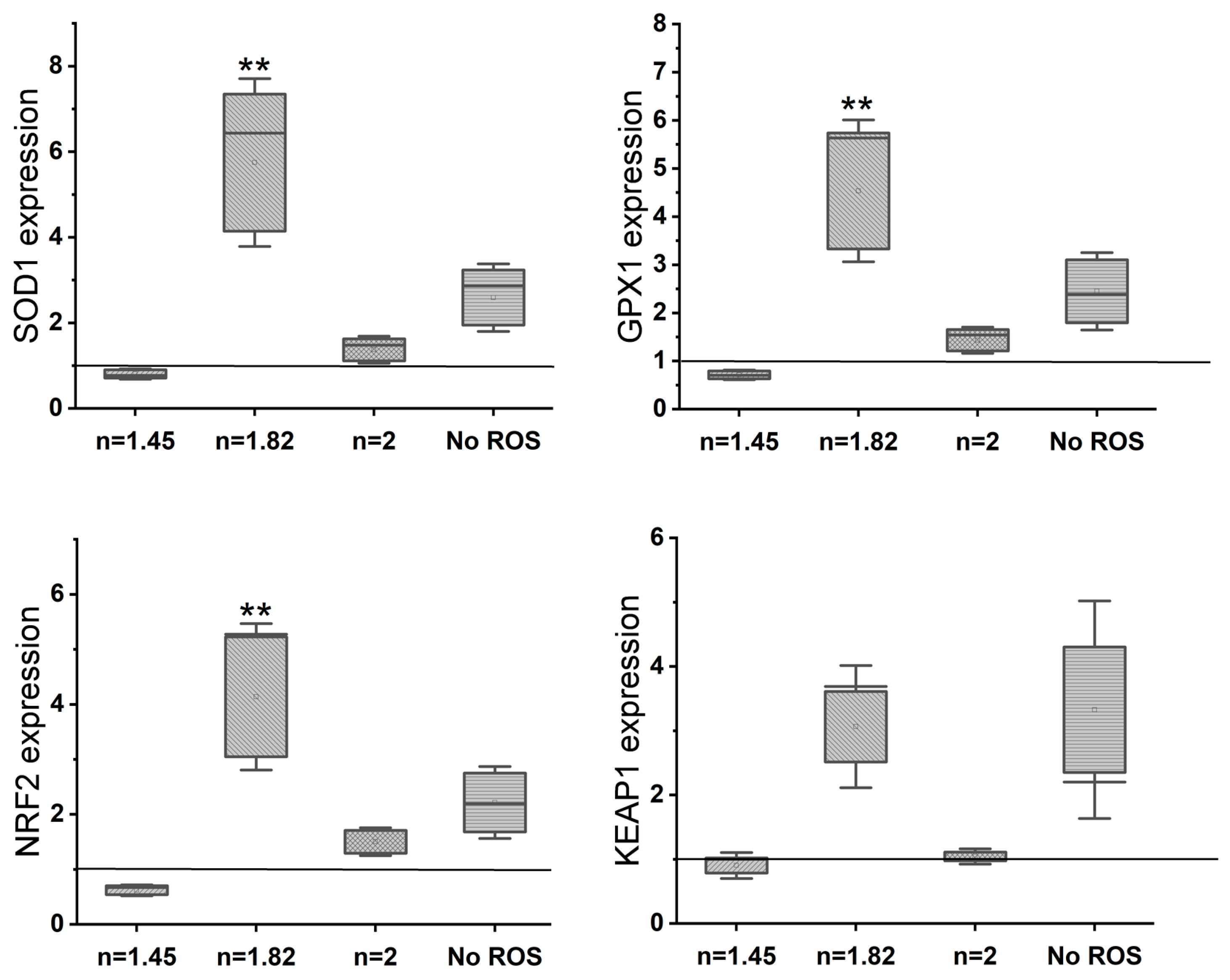
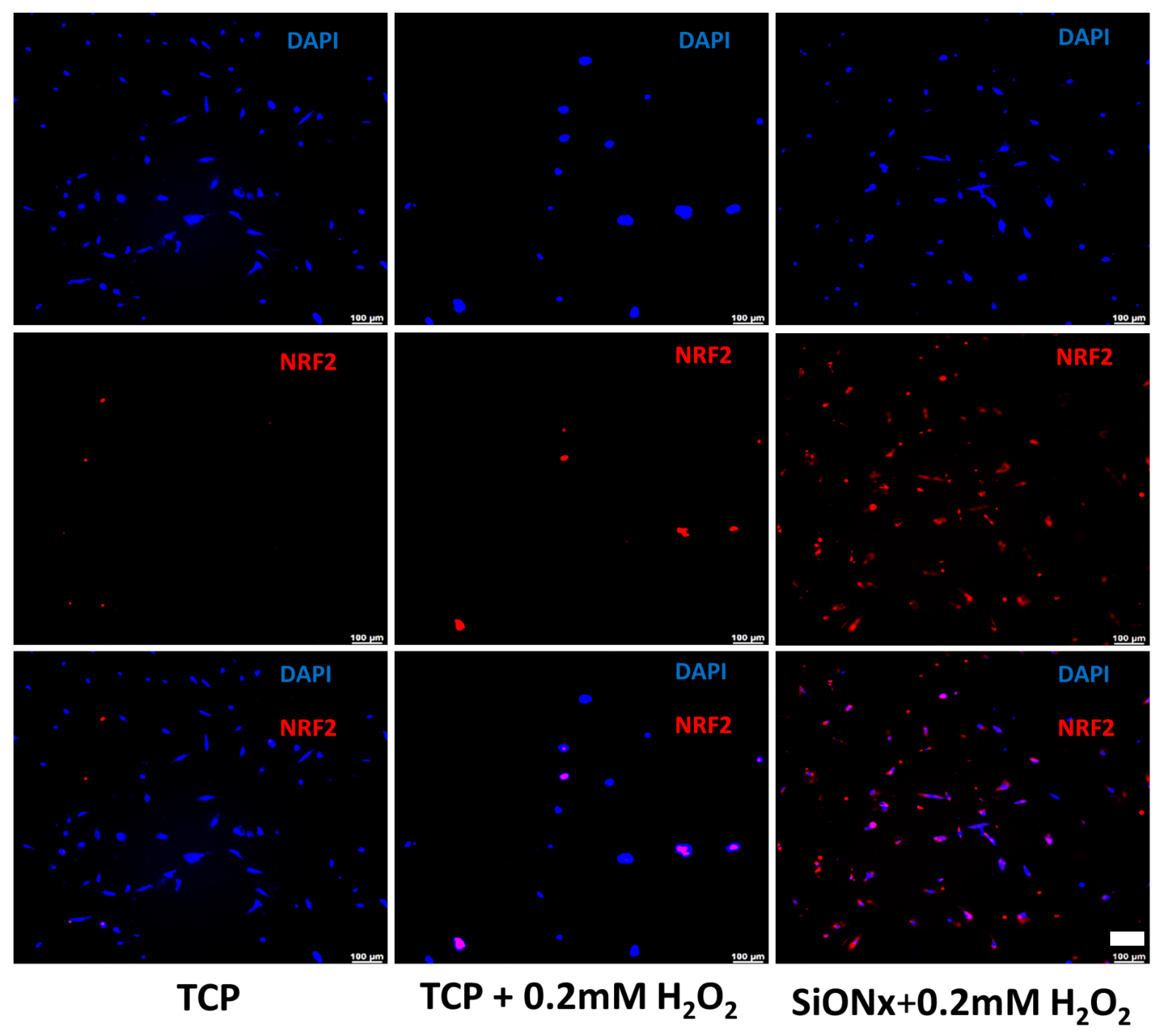
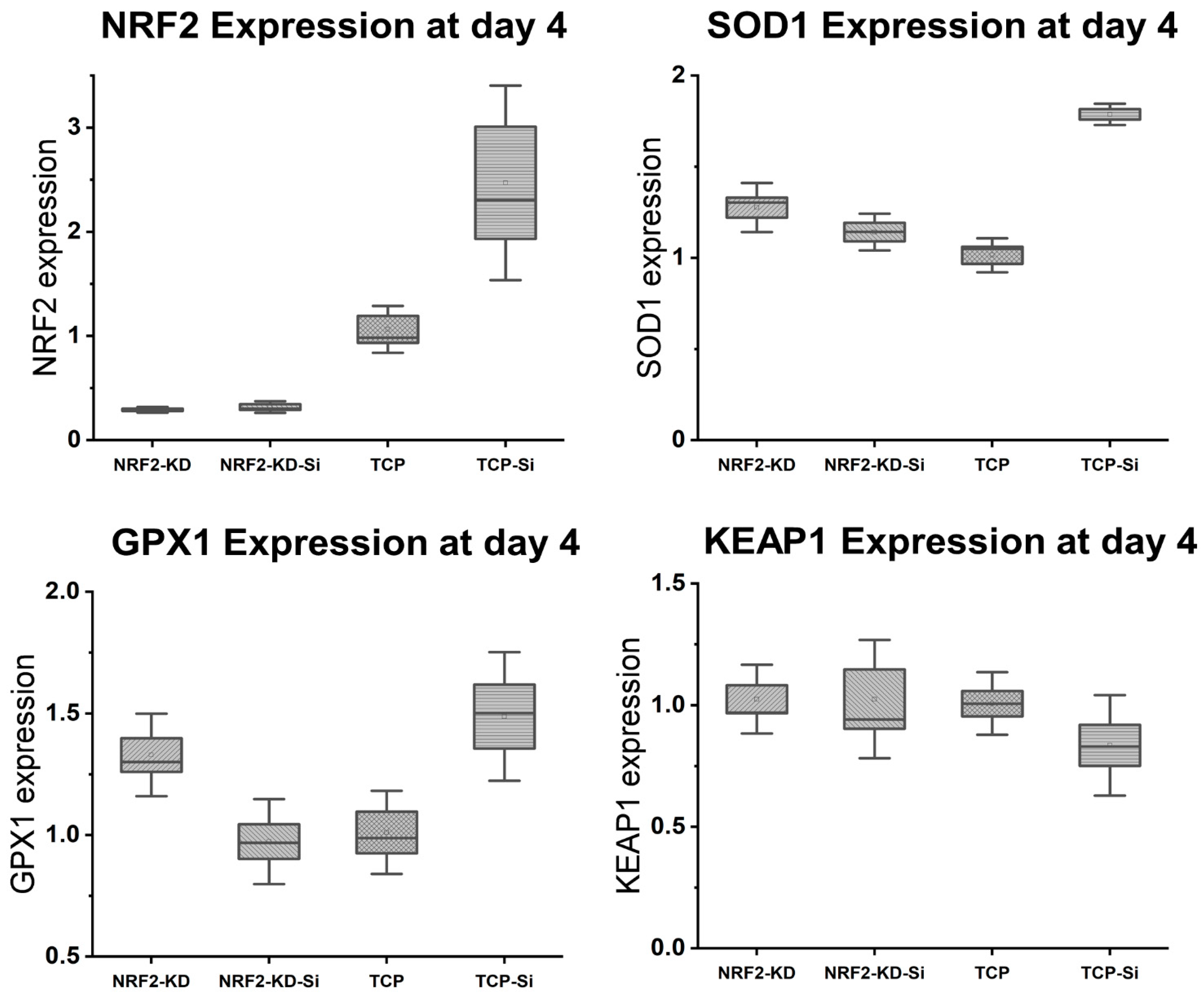
3.5. Effect of Increasing the Nitrogen Concentration in SiONx Chemistry on the Cell Proliferation and Differentiation under Oxidative Stress Conditions
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dimitriou, R.; Jones, E.; McGonagle, D.; Giannoudis, P.V. Bone regeneration: Current concepts and future directions. BMC Med. 2011, 9, 66. [Google Scholar] [CrossRef]
- Nauth, A.; Schemitsch, E.; Norris, B.; Nollin, Z.; Watson, J.T. Critical-Size Bone Defects: Is There a Consensus for Diagnosis and Treatment? J. Orthop. Trauma 2018, 32, S7–S11. [Google Scholar] [CrossRef]
- Sandukji, A.; Al-Sawaf, H.; Mohamadin, A.; Alrashidi, Y.; Sheweita, S.A. Oxidative stress and bone markers in plasma of patients with long-bone fixative surgery: Role of antioxidants. Hum. Exp. Toxicol. 2010, 30, 435–442. [Google Scholar] [CrossRef]
- Banfi, G.; Iorio, E.L.; Corsi, M.M. Oxidative stress, free radicals and bone remodeling. Clin. Chem. Lab. Med. 2008, 46, 1550–1555. [Google Scholar] [CrossRef]
- Sheweita, S.A.; Khoshhal, K.I. Calcium Metabolism and Oxidative Stress in Bone Fractures: Role of Antioxidants. Curr. Drug Metab. 2007, 8, 519–525. [Google Scholar] [CrossRef]
- Wang, Z.; Ehnert, S.; Ihle, C.; Schyschka, L.; Pscherer, S.; Nussler, N.C.; Braun, K.F.; Van Griensven, M.; Wang, G.; Burgkart, R. Increased Oxidative Stress Response in Granulocytes from Older Patients with a Hip Fracture May Account for Slow Regeneration. Oxidative Med. Cell. Longev. 2014, 2014, 819847. [Google Scholar] [CrossRef]
- Lean, J.M.; Davies, J.T.; Fuller, K.; Jagger, C.J.; Kirstein, B.; Partington, G.A.; Urry, Z.L.; Chambers, T.J. A crucial role for thiol antioxidants in estrogen-deficiency bone loss. J. Clin. Investig. 2003, 112, 915–923. [Google Scholar] [CrossRef]
- Zhou, Q.; Zhu, L.; Zhang, D.; Li, N.; Li, Q.; Dai, P.; Mao, Y.; Li, X.; Ma, J.; Huang, S. Oxidative Stress-Related Biomarkers in Postmenopausal Osteoporosis: A Systematic Review and Meta-Analyses. Dis. Markers 2016, 2016, 7067984. [Google Scholar] [CrossRef]
- Mathy-Hartert, M.; Hogge, L.; Sanchez, C.; Deby-Dupont, G.; Crielaard, J.M.; Henrotin, Y. Interleukin-1β and interleukin-6 disturb the antioxidant enzyme system in bovine chondrocytes: A possible explanation for oxidative stress generation. Osteoarthr. Cartil. 2008, 16, 756–763. [Google Scholar] [CrossRef]
- Simunovic, N.; Devereaux, P.J.; Bhandari, M. Surgery for hip fractures: Does surgical delay affect outcomes? Indian J. Orthop. 2011, 45, 27–32. [Google Scholar] [CrossRef]
- Kubo, Y.; Wruck, C.J.; Fragoulis, A.; Drescher, W.; Pape, H.C.; Lichte, P.; Fischer, H.; Tohidnezhad, M.; Hildebrand, F.; Pufe, T.; et al. Role of Nrf2 in Fracture Healing: Clinical Aspects of Oxidative Stress. Calcif. Tissue Int. 2019, 105, 341–352. [Google Scholar] [CrossRef]
- Sun, Y.-X.; Li, L.; Corry, K.A.; Zhang, P.; Yang, Y.; Himes, E.; Mihuti, C.L.; Nelson, C.; Dai, G.; Li, J. Deletion of Nrf2 reduces skeletal mechanical properties and decreases load-driven bone formation. Bone 2015, 74, 1–9. [Google Scholar] [CrossRef]
- Jiang, T.; He, Y. Recent Advances in the Role of Nuclear Factor Erythroid-2-Related Factor 2 in Spinal Cord Injury: Regulatory Mechanisms and Therapeutic Options. Front. Aging Neurosci. 2022, 14, 851257. [Google Scholar] [CrossRef]
- Silvestro, S.; Mazzon, E. Nrf2 Activation: Involvement in Central Nervous System Traumatic Injuries. A Promising Therapeutic Target of Natural Compounds. Int. J. Mol. Sci. 2023, 24, 199. [Google Scholar] [CrossRef]
- Awad, K.; Ahuja, N.; Yacoub, A.S.; Brotto, L.; Young, S.; Mikos, A.; Aswath, P.; Varanasi, V. Revolutionizing bone regeneration: Advanced biomaterials for healing compromised bone defects. Front. Aging 2023, 4, 1217054. [Google Scholar] [CrossRef]
- Sun, Y.-X.; Xu, A.-H.; Yang, Y.; Li, J. Role of Nrf2 in bone metabolism. J. Biomed. Sci. 2015, 22, 101. [Google Scholar] [CrossRef]
- McMahon, M.; Swift, S.R.; Hayes, J.D. Zinc-binding triggers a conformational-switch in the cullin-3 substrate adaptor protein KEAP1 that controls transcription factor NRF2. Toxicol. Appl. Pharmacol. 2018, 360, 45–57. [Google Scholar] [CrossRef]
- Iwai-Yoshida, M.; Shibata, Y.; Wurihan; Suzuki, D.; Fujisawa, N.; Tanimoto, Y.; Kamijo, R.; Maki, K.; Miyazaki, T. Antioxidant and osteogenic properties of anodically oxidized titanium. J. Mech. Behav. Biomed. Mater. 2012, 13, 230–236. [Google Scholar] [CrossRef]
- Xue, T.; Attarilar, S.; Liu, S.; Liu, J.; Song, X.; Li, L.; Zhao, B.; Tang, Y. Surface Modification Techniques of Titanium and its Alloys to Functionally Optimize Their Biomedical Properties: Thematic Review. Front. Bioeng. Biotechnol. 2020, 8, 603072. [Google Scholar] [CrossRef]
- Schmidt, A.H.; Swiontkowski, M.F. Pathophysiology of Infections After Internal Fixation of Fractures. JAAOS-J. Am. Acad. Orthop. Surg. 2000, 8, 285–291. [Google Scholar] [CrossRef]
- Flemming, H.-C.; Wingender, J. The biofilm matrix. Nat. Rev. Microbiol. 2010, 8, 623–633. [Google Scholar] [CrossRef]
- Arciola, C.R.; Campoccia, D.; Montanaro, L. Implant infections: Adhesion, biofilm formation and immune evasion. Nat. Rev. Microbiol. 2018, 16, 397–409. [Google Scholar] [CrossRef]
- Farag, A.; Abdal-hay, A.; Han, P.; Ivanovski, S. Fabrication of 3D melt electrowritting multiphasic scaffold with bioactive and osteoconductivite functionalities for periodontal regeneration. Ceram. Int. 2023, 49, 8015–8021. [Google Scholar] [CrossRef]
- Abdal-hay, A.; Sheikh, F.A.; Shmroukh, A.N.; Mousa, H.M.; Kim, Y.-K.; Ivanovski, S. Immobilization of bioactive glass ceramics @ 2D and 3D polyamide polymer substrates for bone tissue regeneration. Mater. Des. 2021, 210, 110094. [Google Scholar] [CrossRef]
- Abdal-hay, A.; Gulati, K.; Fernandez-Medina, T.; Qian, M.; Ivanovski, S. In situ hydrothermal transformation of titanium surface into lithium-doped continuous nanowire network towards augmented bioactivity. Appl. Surf. Sci. 2020, 505, 144604. [Google Scholar] [CrossRef]
- Xiang, E.; Gómez-Cerezo, M.N.; Ali, Y.; Ramachandra, S.S.; Yang, N.; Dargusch, M.; Moran, C.S.; Ivanovski, S.; Abdal-hay, A. Surface Modification of Pure Zinc by Acid Etching: Accelerating the Corrosion Rate and Enhancing Biocompatibility and Antibacterial Characteristics. ACS Appl. Mater. Interfaces 2022, 14, 22554–22569. [Google Scholar] [CrossRef]
- Xia, L.; Xie, Y.; Fang, B.; Wang, X.; Lin, K. In situ modulation of crystallinity and nano-structures to enhance the stability and osseointegration of hydroxyapatite coatings on Ti-6Al-4V implants. Chem. Eng. J. 2018, 347, 711–720. [Google Scholar] [CrossRef]
- Goller, G. The effect of bond coat on mechanical properties of plasma sprayed bioglass-titanium coatings. Ceram. Int. 2004, 30, 351–355. [Google Scholar] [CrossRef]
- Montazerian, M.; Hosseinzadeh, F.; Migneco, C.; Fook, M.V.L.; Baino, F. Bioceramic coatings on metallic implants: An overview. Ceram. Int. 2022, 48, 8987–9005. [Google Scholar] [CrossRef]
- Narayanan, R.; Seshadri, S.K.; Kwon, T.Y.; Kim, K.H. Calcium phosphate-based coatings on titanium and its alloys. J. Biomed. Mater. Res. Part B Appl. Biomater. 2008, 85, 279–299. [Google Scholar] [CrossRef]
- Sadowski, T.; Golewski, P. (Eds.) Protective Thermal Barrier Coatings. In Loadings in Thermal Barrier Coatings of Jet Engine Turbine Blades: An Experimental Research and Numerical Modeling; Springer: Singapore, 2016; pp. 5–11. [Google Scholar]
- Oku, T.; Suganuma, K.; Wallenberg, L.R.; Tomsia, A.P.; Gomez-Vega, J.M.; Saiz, E. Structural characterization of the metal/glass interface in bioactive glass coatings on Ti-6Al-4V. J. Mater. Sci. Mater. Med. 2001, 12, 413–417. [Google Scholar] [CrossRef]
- Gomez-Vega, J.M.; Saiz, E.; Tomsia, A.P.; Marshall, G.W.; Marshall, S.J. Bioactive glass coatings with hydroxyapatite and Bioglass® particles on Ti-based implants. 1. Processing. Biomaterials 2000, 21, 105–111. [Google Scholar] [CrossRef]
- Saffarian Tousi, N.; Velten, M.F.; Bishop, T.J.; Leong, K.K.; Barkhordar, N.S.; Marshall, G.W.; Loomer, P.M.; Aswath, P.B.; Varanasi, V.G. Combinatorial effect of Si4+, Ca2+, and Mg2+ released from bioactive glasses on osteoblast osteocalcin expression and biomineralization. Mater. Sci. Eng. C 2013, 33, 2757–2765. [Google Scholar] [CrossRef]
- van Oirschot, B.A.J.A.; Alghamdi, H.S.; Närhi, T.O.; Anil, S.; Al Farraj Aldosari, A.; van den Beucken, J.J.J.P.; Jansen, J.A. In vivo evaluation of bioactive glass-based coatings on dental implants in a dog implantation model. Clin. Oral Implant. Res. 2014, 25, 21–28. [Google Scholar] [CrossRef]
- Roy, M.; Bandyopadhyay, A.; Bose, S. Induction plasma sprayed nano hydroxyapatite coatings on titanium for orthopaedic and dental implants. Surf. Coat. Technol. 2011, 205, 2785–2792. [Google Scholar] [CrossRef]
- do Monte, F.A.; Ahuja, N.; Awad, K.R.; Pan, Z.; Young, S.; Kim, H.K.W.; Aswath, P.; Brotto, M.; Varanasi, V.G. Silicon Oxynitrophosphide Nanoscale Coating Enhances Antioxidant Marker-Induced Angiogenesis During in vivo Cranial Bone-Defect Healing. JBMR Plus 2021, 5, e10425. [Google Scholar] [CrossRef]
- Ilyas, A.; Odatsu, T.; Shah, A.; Monte, F.; Kim, H.K.W.; Kramer, P.; Aswath, P.B.; Varanasi, V.G. Amorphous Silica: A New Antioxidant Role for Rapid Critical-Sized Bone Defect Healing. Adv. Healthc. Mater. 2016, 5, 2199–2213. [Google Scholar] [CrossRef]
- Ilyas, A.; Velton, M.; Shah, A.; Monte, F.; Kim, H.K.W.; Aswath, P.B.; Varanasi, V.G. Rapid Regeneration of Vascularized Bone by Nanofabricated Amorphous Silicon Oxynitrophosphide (SiONP) Overlays. J. Biomed. Nanotechnol. 2019, 15, 1241–1255. [Google Scholar] [CrossRef]
- Monte, F.; Awad, K.R.; Ahuja, N.; Kim, H.; Aswath, P.; Brotto, M.; Varanasi, V.G. Amorphous Silicon Oxynitrophosphide Coated Implants Boost Angiogenic Activity of Endothelial Cells. Tissue Eng. Part A 2020, 26, 15–27. [Google Scholar] [CrossRef]
- Varanasi, V.G.; Ilyas, A.; Velten, M.F.; Shah, A.; Lanford, W.A.; Aswath, P.B. Role of Hydrogen and Nitrogen on the Surface Chemical Structure of Bioactive Amorphous Silicon Oxynitride Films. J. Phys. Chem. B 2017, 121, 8991–9005. [Google Scholar] [CrossRef]
- Tian, B.; Liu, Y. Antibacterial applications and safety issues of silica-based materials: A review. Int. J. Appl. Ceram. Technol. 2021, 18, 289–301. [Google Scholar] [CrossRef]
- Awad, K.; Young, S.; Aswath, P.; Varanasi, V. Interfacial adhesion and surface bioactivity of anodized titanium modified with SiON and SiONP surface coatings. Surf. Interfaces 2022, 28, 101645. [Google Scholar] [CrossRef]
- Yun, J.; Wang, W.; Kim, S.M.; Bae, T.-S.; Lee, S.; Kim, D.; Lee, G.-H.; Lee, H.-S.; Song, M. Light trapping in bendable organic solar cells using silica nanoparticle arrays. Energy Environ. Sci. 2015, 8, 932–940. [Google Scholar] [CrossRef]
- Awad, K.; Ahuja, N.; Fiedler, M.; Peper, S.; Wang, Z.; Aswath, P.; Brotto, M.; Varanasi, V. Ionic Silicon Protects Oxidative Damage and Promotes Skeletal Muscle Cell Regeneration. Int. J. Mol. Sci. 2021, 22, 497. [Google Scholar] [CrossRef]
- Pezzotti, G.; Bock, R.M.; McEntire, B.J.; Jones, E.; Boffelli, M.; Zhu, W.; Baggio, G.; Boschetto, F.; Puppulin, L.; Adachi, T.; et al. Silicon Nitride Bioceramics Induce Chemically Driven Lysis in Porphyromonas gingivalis. Langmuir 2016, 32, 3024–3035. [Google Scholar] [CrossRef]
- Jensen, J.; Kraft, D.C.E.; Lysdahl, H.; Foldager, C.B.; Chen, M.; Kristiansen, A.A.; Rölfing, J.H.D.; Bünger, C.E. Functionalization of Polycaprolactone Scaffolds with Hyaluronic Acid and β-TCP Facilitates Migration and Osteogenic Differentiation of Human Dental Pulp Stem Cells In Vitro. Tissue Eng. Part A 2014, 21, 729–739. [Google Scholar] [CrossRef]
- Ilyas, A.; Lavrik, N.V.; Kim, H.K.W.; Aswath, P.B.; Varanasi, V.G. Enhanced Interfacial Adhesion and Osteogenesis for Rapid “Bone-like” Biomineralization by PECVD-Based Silicon Oxynitride Overlays. ACS Appl. Mater. Interfaces 2015, 7, 15368–15379. [Google Scholar] [CrossRef]
- Sandle, T. (Ed.) 6-Dry Heat Sterilisation. In Sterility, Sterilisation and Sterility Assurance for Pharmaceuticals; Woodhead Publishing: Cambridge, UK, 2013; pp. 83–92. [Google Scholar]
- Rose, J.; Vaughan, J. In Vitro Test Methods for Antimicrobial Coatings on Medical Devices: Learnings from Industry. In Antimicrobial Combination Devices; Urish, K.L., Mihalko, W.M., Eds.; ASTM International: West Conshohocken, PA, USA, 2020; pp. 38–52. [Google Scholar]
- Tong Steven, Y.C.; Joshua, S.D.; Eichenberger, E.; Thomas, L.H.; Vance, G.F. Staphylococcus aureus Infections: Epidemiology, Pathophysiology, Clinical Manifestations, and Management. Clin. Microbiol. Rev. 2015, 28, 603–661. [Google Scholar] [CrossRef]
- Velichkova, M.; Hasson, T. Keap1 regulates the oxidation-sensitive shuttling of Nrf2 into and out of the nucleus via a Crm1-dependent nuclear export mechanism. Mol. Cell. Biol. 2005, 25, 4501–4513. [Google Scholar] [CrossRef]
- Tebay, L.E.; Robertson, H.; Durant, S.T.; Vitale, S.R.; Penning, T.M.; Dinkova-Kostova, A.T.; Hayes, J.D. Mechanisms of activation of the transcription factor Nrf2 by redox stressors, nutrient cues, and energy status and the pathways through which it attenuates degenerative disease. Free Radic. Biol. Med. 2015, 88 Pt B, 108–146. [Google Scholar] [CrossRef]
- Dinkova-Kostova, A.T.; Holtzclaw, W.D.; Wakabayashi, N. Keap1, the Sensor for Electrophiles and Oxidants that Regulates the Phase 2 Response, Is a Zinc Metalloprotein. Biochemistry 2005, 44, 6889–6899. [Google Scholar] [CrossRef]
- Varanasi, V.G.; Velten, M.F.; Odatsu, T.; Ilyas, A.; Iqbal, S.M.; Aswath, P.B. Surface Modifications and Surface Characterization of Biomaterials Used in Bone Healing. In Materials and Devices for Bone Disorders; Academic Press: Cambridge, MA, USA, 2016; pp. 405–452. [Google Scholar]
- Drago, L.; Toscano, M.; Bottagisi, M. Recent Evidence on Bioactive Glass Antimicrobial and Antibiofilm Activity: A Mini-Review. Materials 2018, 11, 326. [Google Scholar] [CrossRef]
- Odatsu, T.; Azimaie, T.; Velten, M.F.; Vu, M.; Lyles, M.B.; Kim, H.K.; Aswath, P.B.; Varanasi, V.G. Human periosteum cell osteogenic differentiation enhanced by ionic silicon release from porous amorphous silica fibrous scaffolds. J. Biomed. Mater. Res. Part A 2015, 103, 2797–2806. [Google Scholar] [CrossRef] [PubMed]
- Jelic, M.D.; Mandic, A.D.; Maricic, S.M.; Srdjenovic, B.U. Oxidative stress and its role in cancer. J. Cancer Res. Ther. 2021, 17, 22–28. [Google Scholar] [CrossRef]
- Förstermann, U.; Sessa, W.C. Nitric oxide synthases: Regulation and function. Eur. Heart J. 2012, 33, 829–837. [Google Scholar] [CrossRef]
- Basu, S.; Michaëlsson, K.; Olofsson, H.; Johansson, S.; Melhus, H. Association between Oxidative Stress and Bone Mineral Density. Biochem. Biophys. Res. Commun. 2001, 288, 275–279. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Chen, D.; Jiang, G.; Li, Q.; Wang, Q.; Cheng, M.; He, G.; Zhang, X. A lithium-containing nanoporous coating on entangled titanium scaffold can enhance osseointegration through Wnt/β-catenin pathway. Nanomed. Nanotechnol. Biol. Med. 2018, 14, 153–164. [Google Scholar] [CrossRef] [PubMed]
- Lippross, S.; Beckmann, R.; Streubesand, N.; Ayub, F.; Tohidnezhad, M.; Campbell, G.; Kan, Y.W.; Horst, F.; Sönmez, T.T.; Varoga, D. Nrf2 Deficiency Impairs Fracture Healing in Mice. Calcif. Tissue Int. 2014, 95, 349–361. [Google Scholar] [CrossRef]
- Sies, H. Hydrogen peroxide as a central redox signaling molecule in physiological oxidative stress: Oxidative eustress. Redox Biol. 2017, 11, 613–619. [Google Scholar] [CrossRef]



| Sample | Coating | Gas Flow Rate (sccm) | Deposition Rate (nm/min) | Refractive Index (n) | |||
|---|---|---|---|---|---|---|---|
| 15% SiH4/Ar | N2O | N2 | NH3 | ||||
| 1 | SiONx | 24 | 160 | 225 | 50 | 62.5 | 1.45 |
| 2 | 24 | 155 | 225 | 50 | 59.5 | 1.57 | |
| 3 | 24 | 16 | 225 | 50 | 44.5 | 1.65 | |
| 4 | 24 | 3 | 225 | 50 | 41.0 | 1.82 | |
| 5 | 24 | 0 | 225 | 50 | 36.5 | 2.0 | |
| 15%SiH4/2%PH3/Ar | N2O | N2 | NH3 | Deposition Rate | Refractive index (n) | ||
| 6 | SiONPx | 24 | 16 | 225 | 50 | 38.5 | 1.68 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ahuja, N.; Awad, K.; Yang, S.; Dong, H.; Mikos, A.; Aswath, P.; Young, S.; Brotto, M.; Varanasi, V. SiONx Coating Regulates Mesenchymal Stem Cell Antioxidant Capacity via Nuclear Erythroid Factor 2 Activity under Toxic Oxidative Stress Conditions. Antioxidants 2024, 13, 189. https://doi.org/10.3390/antiox13020189
Ahuja N, Awad K, Yang S, Dong H, Mikos A, Aswath P, Young S, Brotto M, Varanasi V. SiONx Coating Regulates Mesenchymal Stem Cell Antioxidant Capacity via Nuclear Erythroid Factor 2 Activity under Toxic Oxidative Stress Conditions. Antioxidants. 2024; 13(2):189. https://doi.org/10.3390/antiox13020189
Chicago/Turabian StyleAhuja, Neelam, Kamal Awad, Su Yang, He Dong, Antonios Mikos, Pranesh Aswath, Simon Young, Marco Brotto, and Venu Varanasi. 2024. "SiONx Coating Regulates Mesenchymal Stem Cell Antioxidant Capacity via Nuclear Erythroid Factor 2 Activity under Toxic Oxidative Stress Conditions" Antioxidants 13, no. 2: 189. https://doi.org/10.3390/antiox13020189
APA StyleAhuja, N., Awad, K., Yang, S., Dong, H., Mikos, A., Aswath, P., Young, S., Brotto, M., & Varanasi, V. (2024). SiONx Coating Regulates Mesenchymal Stem Cell Antioxidant Capacity via Nuclear Erythroid Factor 2 Activity under Toxic Oxidative Stress Conditions. Antioxidants, 13(2), 189. https://doi.org/10.3390/antiox13020189







