Elevated Bile Acid 3β,5α,6β-Trihydroxycholanoyl Glycine in a Subset of Adult Ataxias Including Niemann–Pick Type C
Abstract
:1. Introduction
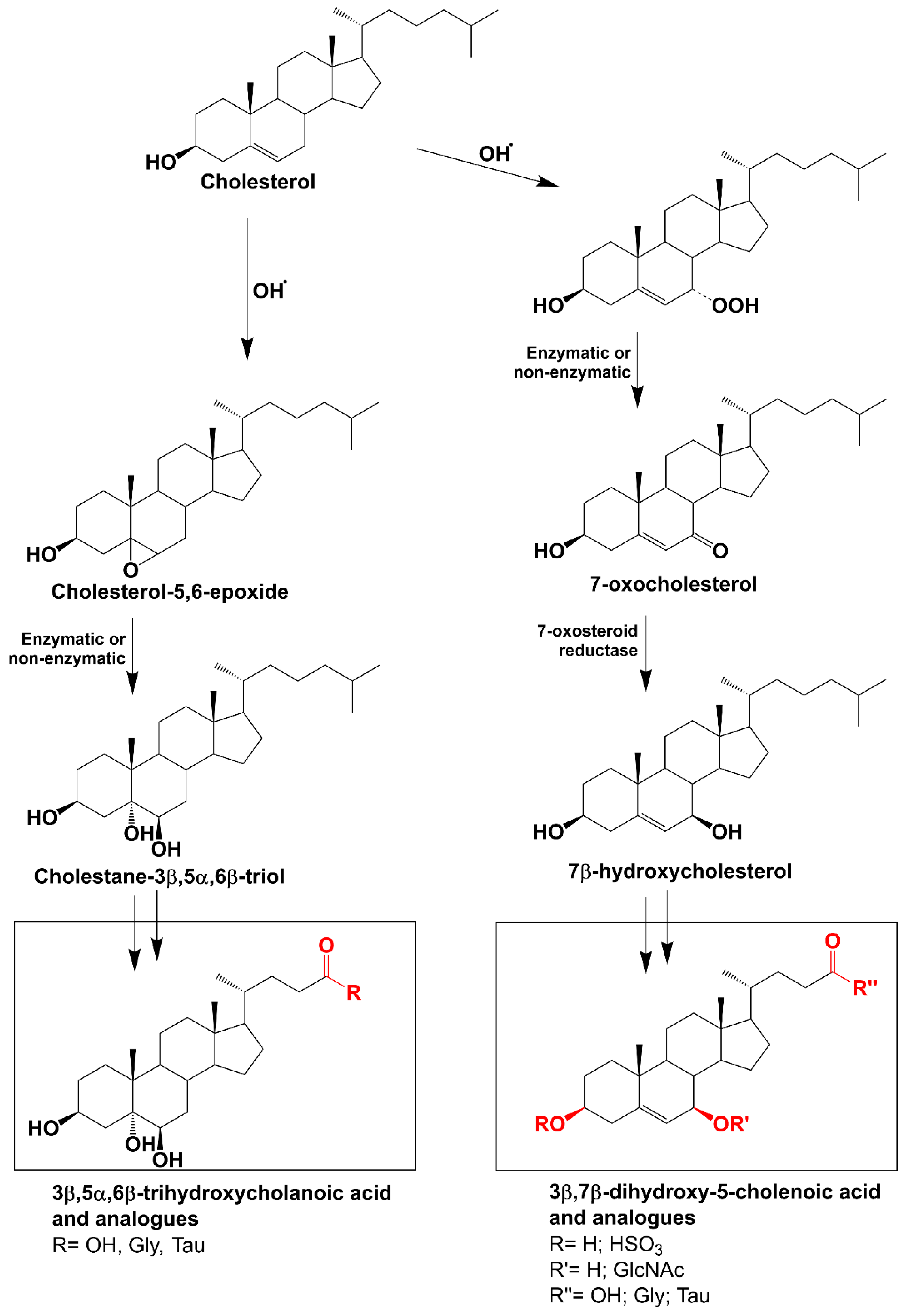
- (i)
- Those derived from 7-oxo cholesterol. These include 3β,7β-dihydroxy-5-cholenoic acid, which may be sulphated on the 3β hydroxyl group, conjugated with N-acetylglucosamine on the 7β hydroxyl group and conjugated with glycine (3β,7β-diOH-Δ5-Gly) or taurine at the C24 carboxyl group.
- (ii)
- Those derived from cholestane-3β,5α,6β-triol. These include 3β,5α,6β-trihydroxycholanoic acid, which may be conjugated with glycine (3β,5α,6β-triOH-Gly) and taurine [15].
2. Methods
2.1. Study Population
2.2. Bile Acid Analysis and Genetic Testing
2.3. Statistical Analysis
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vanier, M.T. Niemann-Pick diseases. Handb. Clin. Neurol. 2013, 113, 1717–1721. [Google Scholar] [CrossRef]
- Patterson, M.C.; Clayton, P.; Gissen, P.; Anheim, M.; Bauer, P.; Bonnot, O.; Dardis, A.; Dionisi-Vici, C.; Klünemann, H.H.; Latour, P.; et al. Recommendations for the detection and diagnosis of Niemann-Pick disease type C: An update. Neurol. Clin. Pract. 2017, 7, 499–511. [Google Scholar] [CrossRef]
- Torres, S.; Balboa, E.; Zanlungo, S.; Enrich, C.; Garcia-Ruiz, C.; Fernandez-Checa, J.C. Lysosomal and Mitochondrial Liaisons in Niemann-Pick Disease. Front. Physiol. 2017, 8, 982. [Google Scholar] [CrossRef]
- Vanier, M.T.; Latour, P. Laboratory diagnosis of Niemann-Pick disease type C: The filipin staining test. Methods Cell Biol. 2015, 126, 357–375. [Google Scholar] [CrossRef]
- Porter, F.D.; Scherrer, D.E.; Lanier, M.H.; Langmade, S.J.; Molugu, V.; Gale, S.E.; Olzeski, D.; Sidhu, R.; Dietzen, D.J.; Fu, R.; et al. Cholesterol oxidation products are sensitive and specific blood-based biomarkers for Niemann-Pick C1 disease. Sci. Transl. Med. 2010, 2, 56ra81. [Google Scholar] [CrossRef]
- Mouritsen, O.G.; Zuckermann, M.J. What’s so special about cholesterol? Lipids 2004, 39, 1101–1113. [Google Scholar] [CrossRef]
- Zhang, X.; Barraza, K.M.; Beauchamp, J.L. Cholesterol provides nonsacrificial protection of membrane lipids from chemical damage at air-water interface. Proc. Natl. Acad. Sci. USA 2018, 115, 3255–3260. [Google Scholar] [CrossRef]
- Alvelius, G.; Hjalmarson, O.; Griffiths, W.J.; Björkhem, I.; Sjövall, J. Identification of unusual 7-oxygenated bile acid sulfates in a patient with Niemann-Pick disease, type C. J. Lipid Res. 2001, 42, 1571–1577. [Google Scholar] [CrossRef]
- Boenzi, S.; Deodato, F.; Taurisano, R.; Goffredo, B.M.; Rizzo, C.; Dionisi-Vici, C. Evaluation of plasma cholestane-3β,5α,6β-triol and 7-ketocholesterol in inherited disorders related to cholesterol metabolism. J. Lipid Res. 2016, 57, 361–367. [Google Scholar] [CrossRef]
- Reunert, J.; Fobker, M.; Kannenberg, F.; Du Chesne, I.; Plate, M.; Wellhausen, J.; Rust, S.; Marquardt, T. Rapid Diagnosis of 83 Patients with Niemann Pick Type C Disease and Related Cholesterol Transport Disorders by Cholestantriol Screening. EBioMedicine 2016, 4, 170–175. [Google Scholar] [CrossRef]
- Griffiths, W.J.; Yutuc, E.; Abdel-Khalik, J.; Crick, P.J.; Hearn, T.; Dickson, A.; Bigger, B.W.; Hoi-Yee Wu, T.; Goenka, A.; Ghosh, A.; et al. Metabolism of Non-Enzymatically Derived Oxysterols: Clues from sterol metabolic disorders. Free Radic. Biol. Med. 2019, 144, 124–133. [Google Scholar] [CrossRef] [PubMed]
- Jiang, X.; Sidhu, R.; Mydock-McGrane, L.; Hsu, F.F.; Covey, D.F.; Scherrer, D.E.; Earley, B.; Gale, S.E.; Farhat, N.Y.; Porter, F.D.; et al. Development of a bile acid-based newborn screen for Niemann-Pick disease type C. Sci. Transl. Med. 2016, 8, 337ra363. [Google Scholar] [CrossRef] [PubMed]
- Maekawa, M.; Jinnoh, I.; Narita, A.; Iida, T.; Saigusa, D.; Iwahori, A.; Nittono, H.; Okuyama, T.; Eto, Y.; Ohno, K.; et al. Investigation of diagnostic performance of five urinary cholesterol metabolites for Niemann-Pick disease type C. J. Lipid Res. 2019, 60, 2074–2081. [Google Scholar] [CrossRef] [PubMed]
- Maekawa, M.; Narita, A.; Jinnoh, I.; Iida, T.; Marquardt, T.; Mengel, E.; Eto, Y.; Clayton, P.T.; Yamaguchi, H.; Mano, N. Diagnostic performance evaluation of sulfate-conjugated cholesterol metabolites as urinary biomarkers of Niemann-Pick disease type C. Clin. Chim. Acta Int. J. Clin. Chem. 2019, 494, 58–63. [Google Scholar] [CrossRef]
- Mazzacuva, F.; Mills, P.; Mills, K.; Camuzeaux, S.; Gissen, P.; Nicoli, E.R.; Wassif, C.; Te Vruchte, D.; Porter, F.D.; Maekawa, M.; et al. Identification of novel bile acids as biomarkers for the early diagnosis of Niemann-Pick C disease. FEBS Lett. 2016, 590, 1651–1662. [Google Scholar] [CrossRef] [PubMed]
- Jiang, X.; Sidhu, R.; Orsini, J.J.; Farhat, N.Y.; Porter, F.D.; Berry-Kravis, E.; Schaffer, J.E.; Ory, D.S. Diagnosis of niemann-pick C1 by measurement of bile acid biomarkers in archived newborn dried blood spots. Mol. Genet. Metab. 2019, 126, 183–187. [Google Scholar] [CrossRef]
- Patterson, M. Niemann-Pick Disease Type C. In GeneReviews(®); Adam, M.P., Mirzaa, G.M., Pagon, R.A., Wallace, S.E., Bean, L.J.H., Gripp, K.W., Amemiya, A., Eds.; University of Washington: Seattle, WA, USA, 2020; Updated 10 December 2020. [Google Scholar]
- Synofzik, M.; Harmuth, F.; Stampfer, M.; Müller Vom Hagen, J.; Schöls, L.; Bauer, P. NPC1 is enriched in unexplained early onset ataxia: A targeted high-throughput screening. J. Neurol. 2015, 262, 2557–2563. [Google Scholar] [CrossRef]
- Papandreou, A.; Doykov, I.; Spiewak, J.; Komarov, N.; Habermann, S.; Kurian, M.A.; Mills, P.B.; Mills, K.; Gissen, P.; Heywood, W.E. Niemann-Pick type C disease as proof-of-concept for intelligent biomarker panel selection in neurometabolic disorders. Dev. Med. Child. Neurol. 2022, 64, 1539–1546. [Google Scholar] [CrossRef]
- Ibañez, K.; Polke, J.; Hagelstrom, R.T.; Dolzhenko, E.; Pasko, D.; Thomas, E.R.A.; Daugherty, L.C.; Kasperaviciute, D.; Smith, K.R.; Deans, Z.C.; et al. Whole genome sequencing for the diagnosis of neurological repeat expansion disorders in the UK: A retrospective diagnostic accuracy and prospective clinical validation study. Lancet Neurol. 2022, 21, 234–245. [Google Scholar] [CrossRef]
- Sidhu, R.; Mondjinou, Y.; Qian, M.; Song, H.; Kumar, A.B.; Hong, X.; Hsu, F.F.; Dietzen, D.J.; Yanjanin, N.M.; Porter, F.D.; et al. N-acyl-O-phosphocholineserines: Structures of a novel class of lipids that are biomarkers for Niemann-Pick C1 disease. J. Lipid Res. 2019, 60, 1410–1424. [Google Scholar] [CrossRef]
- Maekawa, M.; Jinnoh, I.; Matsumoto, Y.; Narita, A.; Mashima, R.; Takahashi, H.; Iwahori, A.; Saigusa, D.; Fujii, K.; Abe, A.; et al. Structural Determination of Lysosphingomyelin-509 and Discovery of Novel Class Lipids from Patients with Niemann-Pick Disease Type C. Int. J. Mol. Sci. 2019, 20, 5018. [Google Scholar] [CrossRef] [PubMed]
- Clayton, P.T. Disorders of Bile Acid Synthesis. In Inborn Metabolic Diseases: Diagnosis and Treatment; Saudubray, J.-M., Baumgartner, M.R., García-Cazorla, Á., Walter, J., Eds.; Springer: Berlin/Heidelberg, Germany, 2022; pp. 705–718. [Google Scholar]
- Stieger, B.; Zhang, J.; O’Neill, B.; Sjövall, J.; Meier, P.J. Differential interaction of bile acids from patients with inborn errors of bile acid synthesis with hepatocellular bile acid transporters. Eur. J. Biochem. 1997, 244, 39–44. [Google Scholar] [CrossRef]
- al-Arfaj, H.F.; Naddaf, H.O. Cerebellar atrophy in systemic lupus erythematosus. Lupus 1995, 4, 412–414. [Google Scholar] [CrossRef] [PubMed]
- Yazawa, S.; Kawasaki, S.; Ohi, T.; Shiomi, K.; Sugimoto, S.; Kawagoe, J.; Matsukura, S. Development of severe longitudinal atrophy of thoracic spinal cord following lupus-related myelitis. Intern. Med. 2001, 40, 353–357. [Google Scholar] [CrossRef] [PubMed]
- Kurien, B.T.; Scofield, R.H. Lipid peroxidation in systemic lupus erythematosus. Indian J. Exp. Biol. 2006, 44, 349–356. [Google Scholar] [PubMed]
- Joshi, R.; Heinz, A.; Fan, Q.; Guo, S.; Monia, B.; Schmelzer, C.E.H.; Weiss, A.S.; Batie, M.; Parameshwaran, H.; Varisco, B.M. Role for Cela1 in Postnatal Lung Remodeling and Alpha-1 Antitrypsin-Deficient Emphysema. Am. J. Respir. Cell Mol. Biol. 2018, 59, 167–178. [Google Scholar] [CrossRef] [PubMed]
- Johar, A.S.; Mastronardi, C.; Rojas-Villarraga, A.; Patel, H.R.; Chuah, A.; Peng, K.; Higgins, A.; Milburn, P.; Palmer, S.; Silva-Lara, M.F.; et al. Novel and rare functional genomic variants in multiple autoimmune syndrome and Sjögren’s syndrome. J. Transl. Med. 2015, 13, 173. [Google Scholar] [CrossRef]
- Branda, S.S.; Yang, Z.Y.; Chew, A.; Isaya, G. Mitochondrial intermediate peptidase and the yeast frataxin homolog together maintain mitochondrial iron homeostasis in Saccharomyces cerevisiae. Hum. Mol. Genet. 1999, 8, 1099–1110. [Google Scholar] [CrossRef] [PubMed]
- Cook, A.; Giunti, P. Friedreich’s ataxia: Clinical features, pathogenesis and management. Br. Med. Bull. 2017, 124, 19–30. [Google Scholar] [CrossRef]
- Elustondo, P.; Martin, L.A.; Karten, B. Mitochondrial cholesterol import. Biochim. Biophys. Acta Mol. Cell Biol. Lipids 2017, 1862, 90–101. [Google Scholar] [CrossRef]
- Puccio, H.; Simon, D.; Cossée, M.; Criqui-Filipe, P.; Tiziano, F.; Melki, J.; Hindelang, C.; Matyas, R.; Rustin, P.; Koenig, M. Mouse models for Friedreich ataxia exhibit cardiomyopathy, sensory nerve defect and Fe-S enzyme deficiency followed by intramitochondrial iron deposits. Nat. Genet. 2001, 27, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Abeti, R.; Parkinson, M.H.; Hargreaves, I.P.; Angelova, P.R.; Sandi, C.; Pook, M.A.; Giunti, P.; Abramov, A.Y. Mitochondrial energy imbalance and lipid peroxidation cause cell death in Friedreich’s ataxia. Cell Death Dis. 2016, 7, e2237. [Google Scholar] [CrossRef] [PubMed]
- Abeti, R.; Uzun, E.; Renganathan, I.; Honda, T.; Pook, M.A.; Giunti, P. Targeting lipid peroxidation and mitochondrial imbalance in Friedreich’s ataxia. Pharmacol. Res. 2015, 99, 344–350. [Google Scholar] [CrossRef]
- Lynch, D.R.; Chin, M.P.; Delatycki, M.B.; Subramony, S.H.; Corti, M.; Hoyle, J.C.; Boesch, S.; Nachbauer, W.; Mariotti, C.; Mathews, K.D.; et al. Safety and Efficacy of Omaveloxolone in Friedreich Ataxia (MOXIe Study). Ann. Neurol. 2021, 89, 212–225. [Google Scholar] [CrossRef] [PubMed]
- Theofilopoulos, S.; Griffiths, W.J.; Crick, P.J.; Yang, S.; Meljon, A.; Ogundare, M.; Kitambi, S.S.; Lockhart, A.; Tuschl, K.; Clayton, P.T.; et al. Cholestenoic acids regulate motor neuron survival via liver X receptors. J. Clin. Investig. 2014, 124, 4829–4842. [Google Scholar] [CrossRef]

| Plasma Bile Acid Concentration nM (n = 184) | ||
|---|---|---|
| 3β,5α,6β-triOH-Gly | 3β,7β-diOH-Δ5-Gly | |
| Median | 22 | 85 |
| Range | 2–219 | 4–964 |
| 96th centile | 90 | 380 |
| Number | Age (Median; Q1, Q3) | Male/Female Number | |
|---|---|---|---|
| Total participants | 184 | 58 (43, 67) | 93/91 |
| Patients with confirmed genetic diagnosis | 28 | 50 (35, 60) | 16/12 |
| CACNA1 a—related ataxia | 5 | 40 (32, 56) | 4/1 |
| HSP b | 3 | 57 (52, 59) | 3/0 |
| CANVAS c | 2 | 71.5 (66, 77) | 0/2 |
| Leigh syndrome | 2 | 61 (60, 62) | 1/1 |
| SCA d-8 | 2 | 38 (36, 41) | 2/0 |
| ANO10 e—related ataxia | 2 | 64 (57, 71) | 0/2 |
| Niemann–Pick Disease Type C | 1 | 20 | 1/0 |
| Friedreich’s ataxia | 1 | 46 | 0/1 |
| SCA-3 | 1 | 48 | 1/0 |
| SCA-11 | 1 | 61 | 1/0 |
| SCA-13 | 1 | 50 | 1/0 |
| SCA-14 | 1 | 51 | 0/1 |
| SCA-26 | 1 | 28 | 0/1 |
| SCA-28 | 1 | 31 | 1/0 |
| Charcot–Marie–Tooth Disease | 1 | 27 | 1/0 |
| AOA2 f | 1 | 34 | 0/1 |
| Occult Macular Dystrophy | 1 | 63 | 0/1 |
| Mast syndrome | 1 | 37 | 0/1 |
| Patients without genetic diagnosis | 156 | 59 (46, 68) | 77/79 |
| Pt n°20 | Pt n°100 | Pt n°51 | Pt n°88 | Pt n°185 | Pt n°155 | Pt n°175 | Pt n°154 | |
|---|---|---|---|---|---|---|---|---|
| Sex | Male | Male | Female | Male | Female | Female | Female | Female |
| Age at sampling (yrs) | 20 | 56 | 81 | 58 | 43 | 46 | 37 | 43 |
| Bile acid 3β5α6β nM (0–90 nM) | 124 | 165 | 109 | 111 | 100 | 159 | 101 | 219 |
| Bile acid 3β7βΔ5 nM (0–380 nM) | 78 | 83 | 450 | 59 | 964 | 105 | 401 | 127 |
| Family History | - | + (Autosomal dominant: sibling affected with same variant. Mother, sister, sister’s daughter, and another brother affected with similar condition, but not tested) | - | Unknown (adopted) | - | + (Sibling also with biallelic GAA repeat expansions, 83 and 118) | - | - |
| Age of onset (yrs) | 14 | 1 delayed milestones | 10 epilepsy 64 nystagmus 68 ataxia | 43 “shakiness” when bending down 56 ataxia | Delayed speech (14 months old: Speech and Language Therapy) 39 ataxia | 33 ataxia, dysarthria | 37 epilepsy, vertigo 40 ataxia, nystagmus | 40 ataxia 46 dysarthria when tired 48 confusion, insomnia, depression |
| First sign | Ataxia | Ataxia | Gelastic epilepsy | “Shakiness” (tremor/imbalance) | Ataxia | Ataxia | - | Ataxia |
| Neurological Examination | Ataxia, dystonia, vertical gaze palsy | Ataxia, nystagmus, mild cognitive impairment | Ataxia, downbeat nystagmus | Functional signs (violent jerking movements of both legs) | Nystagmus, spasticity in all 4 limbs, ankle clonus, hyperreflexia, flexor plantars, ataxia? (antalgic gait, narrow-based) | Ataxia, spasticity, intention tremor, lower-limb hyperreflexia, bilateral upgoing plantars | Rotary nystagmus on left lateral gaze, downbeat nystagmus. Double vision on lateral gaze. Problems with speech, hearing and memory | Ataxia, dysarthria |
| MRI brain | Cerebellar atrophy | Cerebellar atrophy | Cerebellar atrophy | Cerebellar atrophy | Progressive (stable on last MRI) cerebellar and possible cord atrophy (none on last MRI), 2 brainstem telangiectasias | Unremarkable | - | Progressive cerebellar and possible cord atrophy |
| Additional conditions | Kartagener syndrome | Delayed milestones, learning disability, migraine | Epilepsy, diabetes, anti-GAD a but no insulin antibodies, monoclonal gammopathy | Functional neurological disorder, benign essential tremor, abdominal aortic aneurysm, adrenal adenoma, atrial fibrillation, emphysema, migraine | Spasticity, systemic lupus erythematous, depression, anxiety, lung cavity following severe pneumonia, thrombocytopenia treated with steroids at age 13, migraines, purple discolouration of her feet | No | - | Age 35 onset systemic lupus erythematosus resistant to immunosuppression. ANA and dsDNA positive ENA negative. Hypo complementaemia. Idiopathic thrombocytopenic purpura. Fibromyalgia |
| WGS b | Homozygous for primary ciliary dyskinesia (CCDC114) & homozygous for p.(Val1165Met) mutation in NPC1 gene | Heterozygous for c.2636_2652dup p.(Ala885Thrfs*14) likely pathogenic mutation in CACNA1A c) | No primary finding (panels investigated: hereditary ataxia, brain channelopathy, familial hypercholesterolaemia, early-onset dyston ia) | No primary finding (panels investigated: inherited colorectal cancer (with or without polyposis), Parkinson’s disease and complex parkinsonism, hereditary ataxia, hereditary spastic paraplegia, thoracic aortic aneurysm or dissection). Also, DNA molecular analysis for cholestasis (24 genes): negative MLPA for whole exon deletions and duplications not performed | No primary finding (panels investigated: brain channelopathy, hereditary ataxia, mitochondrial disorders, hereditary spastic paraplegia, primary ovarian insufficiency, early-onset dystonia) familial hypercholesterolaemia, early-onset dystonia). Also, DNA molecular analysis for cholestasis (24 genes): negative MLPA for whole exon deletions and duplications not performed | Friedreich’s ataxia (compound heterozygous for 2 GAA repeat expansions: 75 and 101) (panels investigated: hereditary ataxia, brain channelopathy, hearing loss, hereditary spastic paraplegia) Previous to that, suspicion was ANO10 d or SPG7 e (Irish origin) | No primary finding (panels investigated: hereditary ataxia, epileptic encephalopathy, congenital disorders of glycosylation, undiagnosed metabolic disorders, mitochondrial disorders, early-onset dystonia, rare multisystem ciliopathy disorders, familial genetic generalised epilepsies) Also, whole mitochondrial genome sequencing: negative Also, next-generation sequencing (NGS) analysis of a panel of 11 genes involved in ion channel diseases of the brain and MLPA gene dosage analysis of 3 genes: negative | No primary finding (panels investigated: brain channelopathy, hereditary ataxia, mitochondrial disorders, hereditary spastic paraplegia, primary ovarian insufficiency, early-onset dystonia) |
| Final genetic diagnosis | Niemann–Pick disease type C | Episodic ataxia type 2 | None | None | None | Friedreich’s ataxia | None | None |
| Genetic Diagnosis of NPC | |||
|---|---|---|---|
| Positive | Negative | Total | |
| Raised 3β,5α,6β-triOH-Gly (>90 nM) | |||
| Positive | 1 | 7 | 8 |
| Negative | 0 | 176 | 176 |
| Total | 1 | 183 | 184 |
| Sensitivity | 100% | ||
| Specificity | 96.2% | ||
| Positive predictive value (PPV) | 12.5% | ||
| Negative predictive value (NPV) | 100% | ||
| Raised 3β,7β-diOH-Δ5-Gly (>380 nM) | |||
| Positive | 0 | 8 | 8 |
| Negative | 1 | 175 | 176 |
| Total | 1 | 183 | 184 |
| Sensitivity | 0 | ||
| Specificity | 95% | ||
| Positive predictive value (PPV) | 0 | ||
| Negative predictive value (NPV) | 99.4% | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Motamed-Gorji, N.; Khalil, Y.; Gonzalez-Robles, C.; Khan, S.; Mills, P.; Garcia-Moreno, H.; Ging, H.; Tariq, A.; Clayton, P.T.; Giunti, P. Elevated Bile Acid 3β,5α,6β-Trihydroxycholanoyl Glycine in a Subset of Adult Ataxias Including Niemann–Pick Type C. Antioxidants 2024, 13, 561. https://doi.org/10.3390/antiox13050561
Motamed-Gorji N, Khalil Y, Gonzalez-Robles C, Khan S, Mills P, Garcia-Moreno H, Ging H, Tariq A, Clayton PT, Giunti P. Elevated Bile Acid 3β,5α,6β-Trihydroxycholanoyl Glycine in a Subset of Adult Ataxias Including Niemann–Pick Type C. Antioxidants. 2024; 13(5):561. https://doi.org/10.3390/antiox13050561
Chicago/Turabian StyleMotamed-Gorji, Nazgol, Youssef Khalil, Cristina Gonzalez-Robles, Shamsher Khan, Philippa Mills, Hector Garcia-Moreno, Heather Ging, Ambreen Tariq, Peter T. Clayton, and Paola Giunti. 2024. "Elevated Bile Acid 3β,5α,6β-Trihydroxycholanoyl Glycine in a Subset of Adult Ataxias Including Niemann–Pick Type C" Antioxidants 13, no. 5: 561. https://doi.org/10.3390/antiox13050561
APA StyleMotamed-Gorji, N., Khalil, Y., Gonzalez-Robles, C., Khan, S., Mills, P., Garcia-Moreno, H., Ging, H., Tariq, A., Clayton, P. T., & Giunti, P. (2024). Elevated Bile Acid 3β,5α,6β-Trihydroxycholanoyl Glycine in a Subset of Adult Ataxias Including Niemann–Pick Type C. Antioxidants, 13(5), 561. https://doi.org/10.3390/antiox13050561







