Perceived Vaccine Availability and the Uptake of Measles Vaccine in Sudan: The Mediating Role of Vaccination Hesitancy
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Population and Sampling
2.2.1. Population
2.2.2. Sampling
2.3. Data Collection
2.4. Measurements
2.4.1. Dependent Variable
2.4.2. Independent Variables
2.5. Statistical Analysis
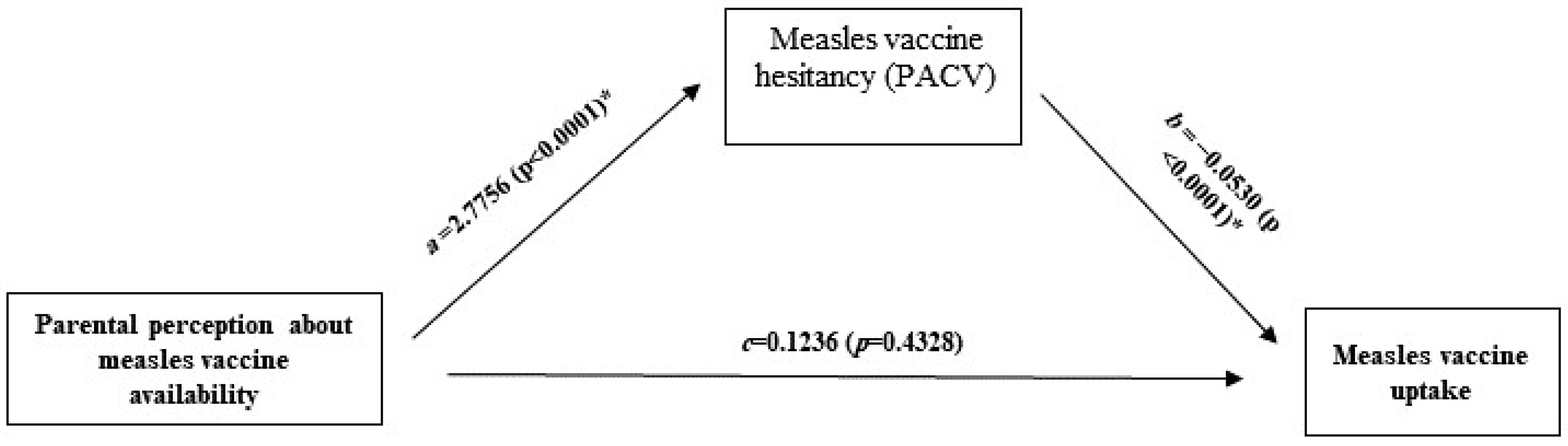
2.5.1. The Mediation Analysis
2.5.2. Ethical Consideration
3. Results
3.1. Descriptive Statistics and Associations between the Sociodemographic and Parental Perceptions of the Measles Vaccine with the Uptake of the Measles Vaccine
3.2. PACV Survey Analysis
3.3. Mediation Analysis
4. Discussion
4.1. Perceived Availability of the Measles Vaccine—Measles Vaccine Hesitancy (PACV)
4.2. PACV—Uptake of the Measles Vaccine
4.3. Perceived Accessibility to the Measles Vaccine—Uptake of the Measles Vaccine
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| No. | PACV’s Items | N (%) | |
|---|---|---|---|
| 1 | Have you ever delayed having your child get the measles vaccine for reasons other than illness or allergy? | Yes | 89 (17.8) |
| No | 406 (81.2) | ||
| I don’t know | 5 (1.0) | ||
| 2 | Have you ever decided not to have your child get the measles vaccine for reasons other than illness or allergy? | Yes | 11 (2.2) |
| No | 485 (97.0) | ||
| I don’t know | 4 (0.8) | ||
| 3 | How sure are you that following the recommended measles vaccine schedule is a good idea for your child? | 0–5 | 19 (3.8) |
| 6–7 | 42 (8.4) | ||
| 8–10 | 439 (87.8) | ||
| 4 | Children get more shots of the measles vaccine than are good for them. | Strongly agree | 16 (3.2) |
| Agree | 21 (4.2) | ||
| Not sure | 18 (3.6) | ||
| Disagree | 294 (58.8) | ||
| Strongly disagree | 150 (30.0) | ||
| Missing | 1 (0.2) | ||
| 5 | I believe that measles that shots prevent is severe. | Strongly agree | 306 (61.2) |
| Agree | 174 (34.8) | ||
| Not sure | 6 (1.2) | ||
| Disagree | 14 (2.8) | ||
| 6 | It is better for my child to develop immunity by getting sick than to get a shot. | Strongly agree | 26 (5.2) |
| Agree | 12 (2.4) | ||
| Not sure | 2 (0.4) | ||
| Disagree | 225 (45.0) | ||
| Strongly disagree | 235 (47.0) | ||
| 7 | It is better for children to get fewer vaccines at the same time. | Strongly agree | 56 (11.2) |
| Agree | 58 (11.6) | ||
| Not sure | 14 (2.8) | ||
| Disagree | 254 (50.8) | ||
| Strongly disagree | 118 (23.6) | ||
| 8 | How concerned are you that your child might have a serious side effect from a shot of the measles vaccine? | Not at all concerned | 208 (41.6) |
| Not concerned | 191 (38.2) | ||
| Not sure | 6 (1.2) | ||
| Concerned | 60 (12.0) | ||
| Very concerned | 35 (7.0) | ||
| 9 | How concerned are you that any one of the measles vaccine shots might not be safe? | Not at all concerned | 253 (50.6) |
| Not concerned | 163 (32.6) | ||
| Not sure | 19 (3.8) | ||
| Concerned | 48 (9.6) | ||
| Very concerned | 17 (3.4) | ||
| 10 | How concerned are you that a shot of the measles vaccine might not prevent measles? | Not at all concerned | 211 (42.2) |
| Not concerned | 188 (37.6) | ||
| Not sure | 17 (3.4) | ||
| Concerned | 62 (12.4) | ||
| Very concerned | 21 (4.2) | ||
| Missing | 1 (0.2) | ||
| 11 | If you had another infant today, would you want him/her to get all the recommended (measles) shots? | Yes | 487 (97.4) |
| No | 9 (1.8) | ||
| I don’t know | 4 (0.8) | ||
| 12 | Overall, how hesitant about measles vaccine shots would you consider yourself to be? | Not at all hesitant | 284 (56.8) |
| Not hesitant | 195 (39.0) | ||
| Not sure | 3 (0.6) | ||
| Hesitant | 12 (2.4) | ||
| Very hesitant | 6 (1.2) | ||
| 13 | I trust the information I receive about measles vaccine shots. | Strongly agree | 242 (48.4) |
| Agree | 239 (47.8) | ||
| Not sure | 8 (1.6) | ||
| Disagree | 8 (1.6) | ||
| Strongly disagree | 2 (0.4) | ||
| Missing | 1 (0.2) | ||
| 14 | I am able to openly discuss my concerns about shots with my child’s doctor. | Strongly agree | 272 (54.4) |
| Agree | 203 (40.6) | ||
| Not sure | 11 (2.2) | ||
| Disagree | 12 (2.4) | ||
| Strongly disagree | 2 (0.4) | ||
| 15 | All things considered, how much do you trust your child’s doctor? | 0–5 | 25 (5.0) |
| 6–7 | 35 (7.0) | ||
| 8–10 | 440 (88.0) | ||
References
- Kumar, S.; Quinn, S.C.; Kim, K.H.; Musa, D.; Hilyard, K.M.; Freimuth, V.S. The social ecological model as a framework for determinants of 2009 H1N1 influenza vaccine uptake in the United States. Health Educ. Behav. 2012, 39, 229–243. [Google Scholar] [CrossRef] [PubMed]
- Kolff, C.A.; Scott, V.P.; Stockwell, M.S. The use of technology to promote vaccination: A social ecological model based framework. Hum. Vaccines Immunother. 2018, 14, 1636–1646. [Google Scholar] [CrossRef]
- Olaniyan, A.; Isiguzo, C.; Hawk, M. The Socioecological Model as a framework for exploring factors influencing childhood immunization uptake in Lagos state, Nigeria. BMC Public Health 2021, 21, 867. [Google Scholar] [CrossRef] [PubMed]
- Bedford, H.; Attwell, K.; Danchin, M.; Marshall, H.; Corben, P.; Leask, J. Vaccine hesitancy, refusal and access barriers: The need for clarity in terminology. Vaccine 2018, 36, 6556–6558. [Google Scholar] [CrossRef] [PubMed]
- Cooper, S.; Okeibunor, J.C.; Wiyeh, A.; Wiysonge, C.S. Knowledge advances and gaps on the demand side of vaccination. Lancet Infect. Dis. 2019, 19, 13–15. [Google Scholar] [CrossRef]
- Cooper, S.; Betsch, C.; Sambala, E.Z.; Mchiza, N.; Wiysonge, C.S. Vaccine hesitancy—A potential threat to the achievements of vaccination programmes in Africa. Hum. Vaccines Immunother. 2018, 14, 2355–2357. [Google Scholar] [CrossRef]
- Sabahelzain, M.M.; Moukhyer, M.; Dubé, E.; Hardan, A.; van den Borne, B.; Bosma, H. Towards a further understanding of measles vaccine hesitancy in Khartoum state, Sudan: A qualitative study. PLoS ONE 2019, 14, e0213882. [Google Scholar] [CrossRef]
- Adetokunboh, O.; Iwu-Jaja, C.J.; Nnaji, C.A.; Ndwandwe, D. Missed opportunities for vaccination in Africa. Curr. Opin. Immunol. 2021, 71, 55–61. [Google Scholar] [CrossRef]
- Quinn, S.; Jamison, A.; Musa, D.; Hilyard, K.; Freimuth, V. Exploring the Continuum of Vaccine Hesitancy Between African American and White Adults: Results of a Qualitative Study. PLoS Curr. 2016, 8. [Google Scholar] [CrossRef]
- Magodi, R.; Mmbaga, E.J.; Massaga, J.; Lyimo, D.; Mphuru, A.; Abade, A. Factors associated with non-uptake of measles-rubella vaccine second dose among children under five years in Mtwara district council, Tanzania, 2017. Pan Afr. Med. J. 2019, 33, 67. [Google Scholar] [CrossRef]
- Bangura, J.B.; Xiao, S.; Qiu, D.; Ouyang, F.; Chen, L. Barriers to childhood immunization in sub-Saharan Africa: A systematic review. BMC Public Health 2020, 20, 1108. [Google Scholar] [CrossRef] [PubMed]
- Adamu, A.A.; Essoh, T.A.; Adeyanju, G.C.; Jalo, R.I.; Saleh, Y.; Aplogan, A.; Wiysonge, C.S. Drivers of hesitancy towards recommended childhood vaccines in African settings: A scoping review of literature from Kenya, Malawi and Ethiopia. Expert Rev. Vaccines 2021, 20, 611–621. [Google Scholar] [CrossRef] [PubMed]
- Krudwig, K.; Knittel, B.; Karim, A.; Kanagat, N.; Prosser, W.; Phiri, G.; Mwansa, F.; Steinglass, R. The effects of switching from 10 to 5-dose vials of MR vaccine on vaccination coverage and wastage: A mixed-method study in Zambia. Vaccine 2020, 38, 5905–5913. [Google Scholar] [CrossRef] [PubMed]
- UNICEF; WHO. Introducing the Measles and Measles-Rubella (MR) Vaccine Five-Dose Vial Presentations Fact Sheet. Available online: https://www.technet-21.org/fr/library/main/5167-introducing-the-measles-and-measles-rubella-mr-vaccine-five-dose-vial-presentations-facts-sheet (accessed on 7 December 2021).
- World Health Organization. Ten Threats to Global Health in 2019. Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 25 January 2021).
- MacDonald, N.E. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef]
- World Health Organization. Report of the SAGE Working Group on Vaccine Hesitancy; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Ministry of Health in Sudan. Annual Statistical Report 2018. Available online: https://ghdx.healthdata.org/record/sudan-annual-health-statistical-report-2018 (accessed on 2 January 2022).
- Ministry of Health in Sudan. Annual Statistical Report 2019. Available online: http://www.sho.gov.sd/controller/kn_hub_%20featured.php?sm_id=133&mid=110&lid=1# (accessed on 3 January 2022).
- Ministry of Health in Sudan. WHO and UNICEF Estimate of Immunization Coverage: 2018 Revision. Available online: www.sho.gov.sd (accessed on 15 December 2021).
- Sabahelzain, M.M.; Moukhyer, M.; Bosma, H.; van den Borne, B. Determinants of Measles Vaccine Hesitancy among Sudanese Parents in Khartoum State, Sudan: A Cross-Sectional Study. Vaccines 2021, 10, 6. [Google Scholar] [CrossRef]
- Sabahelzain, M.M.; Moukhyer, M.; van den Borne, B.; Bosma, H. Vaccine Hesitancy among Parents and Its Association with the Uptake of Measles Vaccine in Urban Settings in Khartoum State, Sudan. Vaccines 2022, 10, 205. [Google Scholar] [CrossRef] [PubMed]
- Fleiss, J.L. Statistical Methods for Rates and Proportions, 2nd ed.; John Wiley: New York, NY, USA, 1981. [Google Scholar]
- Opel, D.J.; Taylor, J.A.; Mangione-Smith, R.; Solomon, C.; Zhao, C.; Catz, S.; Martin, D. Validity and reliability of a survey to identify vaccine-hesitant parents. Vaccine 2011, 29, 6598–6605. [Google Scholar] [CrossRef]
- Opel, D.J.; Taylor, J.A.; Zhou, C.; Catz, S.; Myaing, M.; Mangione-Smith, R. The relationship between parent attitudes about childhood vaccines survey scores and future child immunization status: A validation study. JAMA Pediatr. 2013, 167, 1065–1071. [Google Scholar] [CrossRef]
- Sabahelzain, M.M.; Dubé, E.; Moukhyer, M.; Larson, H.J.; van den Borne, B.; Bosma, H. Psychometric properties of the adapted measles vaccine hesitancy scale in Sudan. PLoS ONE 2020, 15, e0237171. [Google Scholar] [CrossRef] [PubMed]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; Guilford Publications: New York, NY, USA, 2017; Available online: https://afhayes.com/public/v3docadd.pdf (accessed on 1 December 2021).
- Goodson, J.L. Recent setbacks in measles elimination: The importance of investing in innovations for immunizations. Pan Afr. Med. J. 2020, 35 (Suppl. S1), 15. [Google Scholar] [CrossRef] [PubMed]
- Williams, S.E.; Morgan, A.; Opel, D.; Edwards, K.; Weinberg, S.; Rothman, R. Screening tool predicts future underimmunization among a pediatric practice in Tennessee. Clin. Pediatr. 2016, 55, 537–542. [Google Scholar] [CrossRef] [PubMed]
- Glanz, J.M.; Wagner, N.M.; Narwaney, K.J.; Kraus, C.R.; Shoup, J.A.; Xu, S.; O’Leary, S.T.; Omer, S.B.; Gleason, K.S.; Daley, M.F. Web-based social media intervention to increase vaccine acceptance: A randomized controlled trial. Pediatrics 2017, 140, e20171117. [Google Scholar] [CrossRef] [PubMed]
- Williams, S.E.; Rothman, R.L.; Offit, P.A.; Schaffner, W.; Sullivan, M.; Edwards, K.M. A randomized trial to increase acceptance of childhood vaccines by vaccine-hesitant parents: A pilot study. Acad. Pediatr. 2013, 13, 475–480. [Google Scholar] [CrossRef] [PubMed]
- Roberts, J.R.; Thompson, D.; Rogacki, B.; Hale, J.J.; Jacobson, R.M.; Opel, D.J.; Darden, P.M. Vaccine hesitancy among parents of adolescents and its association with vaccine uptake. Vaccine 2015, 33, 1748–1755. [Google Scholar] [CrossRef]
| Variables | Measles Vaccination Uptake/Status | ||||||
|---|---|---|---|---|---|---|---|
| Total N = 495 (%) | Fully Vaccinated | Partially/Unvaccinated | p-Value | ||||
| N = 436 | % | N = 59 | % | ||||
| Area of the study | Alsharafia | 152 (30.7) | 128 | 84.2% | 24 | 15.8% | 0.077 |
| Abo Saeed | 343 (69.3) | 308 | 89.8% | 35 | 10.2% | ||
| Mother’s Education | Illiterate | 14 (2.8) | 11 | 78.6% | 3 | 21.4% | 0.162 |
| Primary completed | 63 (12.7) | 51 | 81.0% | 12 | 19.0% | ||
| Secondary completed | 170 (34.3) | 151 | 88.8% | 19 | 11.2% | ||
| University | 248 (50.1) | 223 | 89.9% | 25 | 10.1% | ||
| Mother’s Employment | Housewife | 370 (74.7) | 323 | 87.3% | 47 | 12.7% | 0.017 *,b |
| Student | 11 (2.2) | 10 | 90.9% | 1 | 9.1% | ||
| Domestic worker | 14 (2.8) | 12 | 85.7% | 2 | 14.3% | ||
| Officer | 50 (10.1) | 48 | 96.0% | 2 | 4.0% | ||
| Professional (e.g., Engineer, Doctor) | 33 (6.7) | 32 | 97.0% | 1 | 3.0% | ||
| Self-employed | 16 (3.2) | 10 | 62.5% | 6 | 37.5% | ||
| Others | 1 (0.2) | 1 | 100.0% | 0 | 0.0% | ||
| Income Level (Self-Ranking) | High | 70 (14.1) | 65 | 92.9% | 5 | 7.1% | 0.268 |
| Medium | 391 (79.0) | 343 | 87.7% | 48 | 12.3% | ||
| Low | 34 (6.9) | 28 | 82.4% | 6 | 17.6% | ||
| Number of Children | 1 | 218 (44.0) | 185 | 84.9% | 33 | 15.1% | 0.041 * |
| 2 | 227 (45.9) | 209 | 92.1% | 18 | 7.9% | ||
| 3 and more | 50 (10.1) | 42 | 84.0% | 8 | 16.0% | ||
| Perceived accessibility and availability of measles vaccine when my child needs it. | Strongly agree | 247 (49.9) | 217 | 87.9% | 30 | 12.1% | 0.045 *,b |
| Agree | 201 (40.6) | 183 | 91.0% | 18 | 9.0% | ||
| Not sure | 10 (2.0) | 8 | 80.0% | 2 | 20.0% | ||
| Disagree | 35 (7.1) | 27 | 77.1% | 8 | 22.9% | ||
| Strongly disagree | 2 (0.4) | 1 | 50.0% | 1 | 50.0% | ||
| M (Vaccine Hesitancy) | Y (Measles Vaccine Uptake) ** | |||||
|---|---|---|---|---|---|---|
| Antecedent | Coeff. | SE | p | Coeff. | SE | p |
| X (Perceived vaccine availability) | a, 2.7756 | 0.5411 | <0.0001 * | c, 0.1236 | 0.1576 | 0.4328 |
| M | - | - | - | b, 0.0530 | 0.0124 | <0.0001 * |
| Cov1 (Mothers’ age) | 0.0822 | 0.0802 | 0.306 | 0.0432 | 0.0246 | 0.0787 |
| Cov2 (N. of children) | 1.9258 | 0.6511 | 0.003 * | −0.2697 | 0.2040 | 0.1862 |
| Constant | −0.9268 | 2.9151 | 0.751 | −3.7734 | 0.9146 | <0.0001 * |
| Model Summary | R-sq = 0.0718, F = 12.551, p < 0.0001 * | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sabahelzain, M.M.; Tagelsir, A.; Elhadi, Y.A.M.; Abdalla, O. Perceived Vaccine Availability and the Uptake of Measles Vaccine in Sudan: The Mediating Role of Vaccination Hesitancy. Vaccines 2022, 10, 1674. https://doi.org/10.3390/vaccines10101674
Sabahelzain MM, Tagelsir A, Elhadi YAM, Abdalla O. Perceived Vaccine Availability and the Uptake of Measles Vaccine in Sudan: The Mediating Role of Vaccination Hesitancy. Vaccines. 2022; 10(10):1674. https://doi.org/10.3390/vaccines10101674
Chicago/Turabian StyleSabahelzain, Majdi M., Ahmed Tagelsir, Yasir Ahmed Mohammed Elhadi, and Omayma Abdalla. 2022. "Perceived Vaccine Availability and the Uptake of Measles Vaccine in Sudan: The Mediating Role of Vaccination Hesitancy" Vaccines 10, no. 10: 1674. https://doi.org/10.3390/vaccines10101674
APA StyleSabahelzain, M. M., Tagelsir, A., Elhadi, Y. A. M., & Abdalla, O. (2022). Perceived Vaccine Availability and the Uptake of Measles Vaccine in Sudan: The Mediating Role of Vaccination Hesitancy. Vaccines, 10(10), 1674. https://doi.org/10.3390/vaccines10101674






