Educational Inequalities in COVID-19 Vaccination: A Cross-Sectional Study of the Adult Population in the Lazio Region, Italy
Abstract
:1. Introduction
2. Materials and Methods
2.1. Setting and Study Design
2.2. Sources of Data
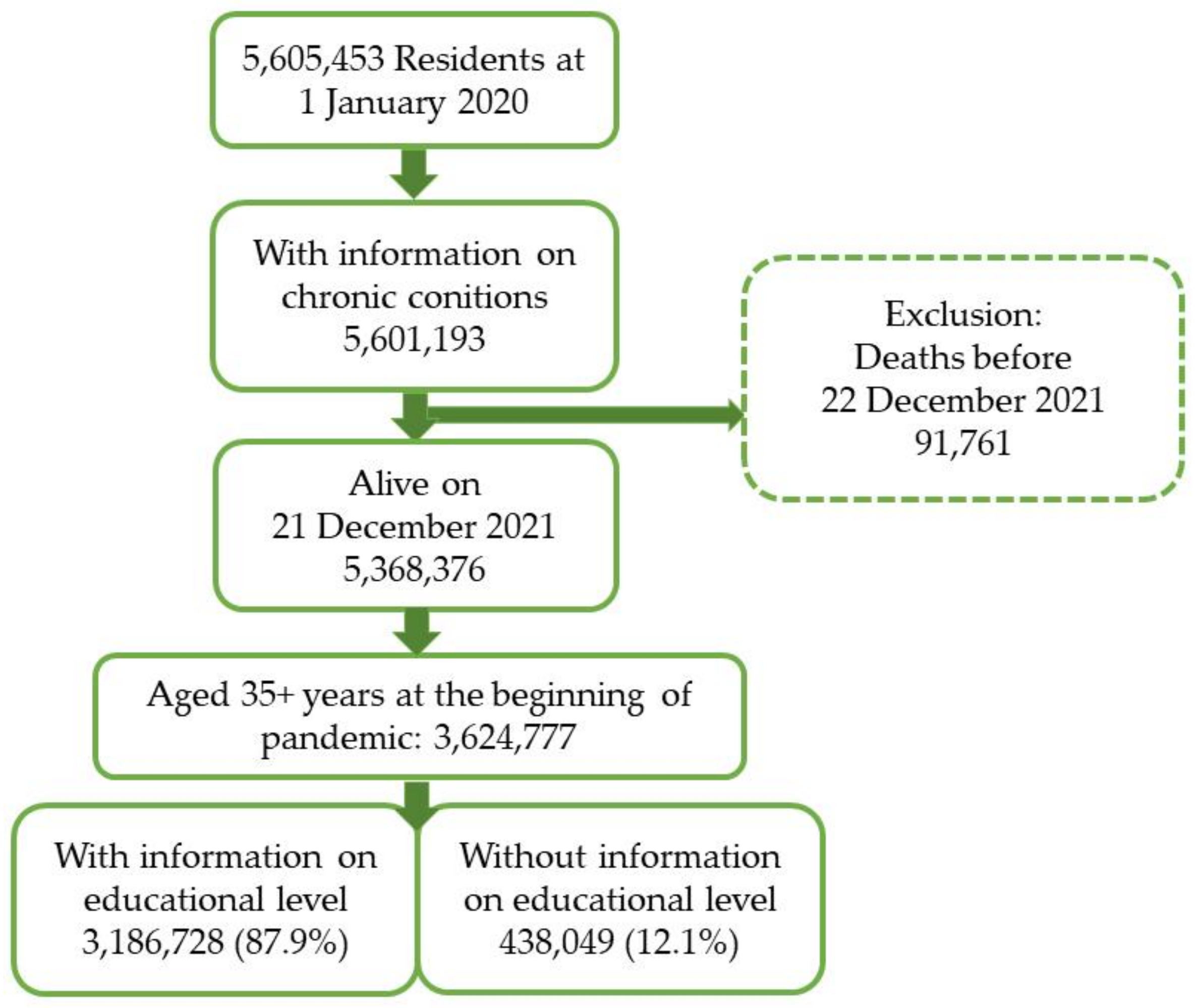
2.3. Study Population
2.4. Outcome and Other Variables
2.5. Statistical Analysis
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kawachi, I. COVID-19 and the “rediscovery” of health inequities. Int. J. Epidemiol. 2020, 49, 1415–1418. [Google Scholar] [CrossRef] [PubMed]
- Marmot, M.; Allen, J. COVID-19: Exposing and amplifying inequalities. J. Epidemiol. Community Health 2020, 74, 681–682. [Google Scholar] [CrossRef] [PubMed]
- Riou, J.; Panczak, R.; Althaus, C.L.; Junker, C.; Perisa, D.; Schneider, K.; Criscuolo, N.G.; Low, N.; Egger, M. Socioeconomic position and the COVID-19 care cascade from testing to mortality in Switzerland: A population-based analysis. Lancet Public Health 2021, 6, e683–e691. [Google Scholar] [CrossRef]
- Lewis, N.M.; Friedrichs, M.; Wagstaff, S.; Sage, K.; LaCross, N.; Bui, D.; McCaffrey, K.; Barbeau, B.; George, A.; Rose, C.; et al. Disparities in COVID-19 Incidence, Hospitalizations, and Testing, by Area-Level Deprivation—Utah, 3 March–9 July 2020. MMWR. Morb. Mortal. Wkly. Rep. 2020, 69, 1369–1373. [Google Scholar] [CrossRef]
- Abedi, V.; Olulana, O.; Avula, V.; Chaudhary, D.; Khan, A.; Shahjouei, S.; Li, J.; Zand, R. Racial, Economic, and Health Inequality and COVID-19 Infection in the United States. J. Racial Ethn. Health Disparities 2021, 8, 732–742. [Google Scholar] [CrossRef]
- Di Girolamo, C.; Bartolini, L.; Caranci, N.; Moro, M.L. Socioeconomic inequalities in overall and COVID-19 mortality during the first outbreak peak in Emilia-Romagna Region (Northern Italy). (Disuguaglianze Socioecon. nella mortalita Total. e Correl. al COVID-19 durante primo picco epidemico Reg. Emilia-Romagna). Epidemiol Prev. 2020, 44, 288–296. [Google Scholar] [CrossRef] [PubMed]
- Liao, T.F.; De Maio, F. Association of Social and Economic Inequality with Coronavirus Disease 2019 Incidence and Mortality across US Counties. JAMA Netw. Open 2021, 4, 1–10. [Google Scholar] [CrossRef]
- Marmot, M.; Allen, J.; Bell, R.; Bloomer, E.; Goldblatt, P. WHO European review of social determinants of health and the health divide. Lancet 2012, 380, 1011–1029. [Google Scholar] [CrossRef]
- Badaloni, C.; Cesaroni, G.; Forastiere, F.; Perucci, C.A. Cambiamenti temporali nella speranza di vita per genere e livello socioeconomico, Roma 1991–2005. Epidemiol Prev. 2008, 2005, 301–306. [Google Scholar]
- Paglione, L.; Angelici, L.; Davoli, M.; Agabiti, N.; Cesaroni, G. Mortality inequalities by occupational status and type of job in men and women: Results from the Rome Longitudinal Study. BMJ Open 2020, 10, e033776. [Google Scholar] [CrossRef]
- Cesaroni, G.; Agabiti, N.; Forastiere, F.; Perucci, C.A. Socioeconomic differences in stroke incidence and prognosis under a universal healthcare system. Stroke 2009, 40, 2812–2819. [Google Scholar] [CrossRef] [Green Version]
- Agabiti, N.; Pirani, M.; Schifano, P.; Cesaroni, G.; Davoli, M.; Bisanti, L.; Caranci, N.; Costa, G.; Forastiere, F.; Marinacci, C.; et al. Income level and chronic ambulatory care sensitive conditions in adults: A multicity population-based study in Italy. BMC Public Health 2009, 9, 457. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kirchmayer, U.; Agabiti, N.; Belleudi, V.; Davoli, M.; Fusco, D.; Stafoggia, M.; Arcà, M.; Barone, A.P.; Perucci, C.A. Socio-demographic differences in adherence to evidence-based drug therapy after hospital discharge from acute myocardial infarction: A population-based cohort study in Rome, Italy. J. Clin. Pharm. Ther. 2012, 37, 37–44. [Google Scholar] [CrossRef] [PubMed]
- Angelici, L.; Sorge, C.; Di Martino, M.; Cappai, G.; Stafoggia, M.; Agabiti, N.; Girardi, E.; Lanini, S.; Nicastri, E.; Davoli, M.; et al. Incidence of SARS-CoV-2 Infection and Related Mortality by Education Level During Three Phases of the 2020 Pandemic: A Population-Based Cohort Study in Rome. J. Clin. Med. 2022, 11, 877. [Google Scholar] [CrossRef]
- Callaghan, T.; Moghtaderi, A.; Lueck, J.A.; Hotez, P.; Strych, U.; Dor, A.; Fowler, E.F.; Motta, M. Correlates and disparities of intention to vaccinate against COVID-19. Soc. Sci. Med. 2021, 272, 113638. [Google Scholar] [CrossRef] [PubMed]
- Brailovskaia, J.; Schneider, S.; Margraf, J. To vaccinate or not to vaccinate!? Predictors of willingness to receive COVID-19 vaccination in Europe, the U.S., and China. PLoS ONE 2021, 16, e0260230. [Google Scholar] [CrossRef]
- Green, M.S.; Abdullah, R.; Vered, S.; Nitzan, D. A study of ethnic, gender and educational differences in attitudes toward COVID-19 vaccines in Israel—Implications for vaccination implementation policies. Isr. J. Health Policy Res. 2021, 10, 26. [Google Scholar] [CrossRef]
- Elliott, T.; Yehia, B.R.; Winegar, A.L.; Raja, J.K.; Jones, A.; Shockley, E.; Cacchione, J. Analysis of COVID-19 vaccine non-intent by essential vs non-essential worker, demographic, and socioeconomic status among 101,048 US adults. PLoS ONE 2021, 16, e0258540. [Google Scholar] [CrossRef]
- Shakeel, C.S.; Mujeeb, A.A.; Mirza, M.S.; Chaudhry, B.; Khan, S.J. Global COVID-19 Vaccine Acceptance: A Systematic Review of Associated Social and Behavioral Factors. Vaccines 2022, 10, 110. [Google Scholar] [CrossRef]
- Rosano, A.; Pacelli, B.; Zengarini, N.; Costa, G.; Cislaghi, C.; Caranci, N. Update and review of the 2011 italian deprivation index calculated at the census section level. Epidemiol. Prev. 2020, 44, 162–170. [Google Scholar] [CrossRef]
- Rehman, S.U.; Ahmed, M.A.; Adnan, G.; Khan, M.A. Reorganising for COVID-19 Pandemic: A Review of Structural Modifications by the Department of Internal Medicine in Low to Middle-income Countries. J. Coll. Physicians Surg. Pak. 2020, 30, 176–177. [Google Scholar] [CrossRef] [PubMed]
- Caspi, G.; Dayan, A.; Eshal, Y.; Liverant-Taub, S.; Twig, G.; Shalit, U.; Lewis, Y.; Shina, A.; Caspi, O. Socioeconomic disparities and COVID-19 vaccination acceptance: A nationwide ecologic study. Clin. Microbiol. Infect. 2021, 27, 1502–1506. [Google Scholar] [CrossRef] [PubMed]
- Kelly, B.J.; Southwell, B.G.; McCormack, L.A.; Bann, C.M.; MacDonald, P.D.M.; Frasier, A.M.; Bevc, C.A.; Brewer, N.T.; Squiers, L.B. Correction to: Predictors of willingness to get a COVID-19 vaccine in the U.S. BMC Infect. Dis. 2021, 21, 383. [Google Scholar] [CrossRef] [PubMed]
- Burger, A.E.; Reither, E.N.; Mamelund, S.-E.; Lim, S. Black-white disparities in 2009 H1N1 vaccination among adults in the United States: A cautionary tale for the COVID-19 pandemic. Vaccine 2021, 39, 943–951. [Google Scholar] [CrossRef] [PubMed]
- Abdul-Mutakabbir, J.C.; Casey, S.; Jews, V.; King, A.; Simmons, K.; Hogue, M.D.; Belliard, J.C.; Peverini, R.; Veltman, J. A three-tiered approach to address barriers to COVID-19 vaccine delivery in the Black community. Lancet Glob. Health 2021, 9, e749–e750. [Google Scholar] [CrossRef]
- Perry, M.; Akbari, A.; Cottrell, S.; Gravenor, M.B.; Roberts, R.; Lyons, R.A.; Bedston, S.; Torabi, F.; Griffiths, L. Inequalities in coverage of COVID-19 vaccination: A population register based cross-sectional study in Wales, UK. Vaccine 2021, 39, 6256–6261. [Google Scholar] [CrossRef] [PubMed]
- Carson, S.L.; Casillas, A.; Castellon-lopez, Y.; Mansfield, L.N.; Morris, D.A. COVID-19 Vaccine Decision-making Factors in Racial and Ethnic Minority Communities in Los Angeles, California. JAMA Netw Open. 2021, 4, e2127582. [Google Scholar] [CrossRef]
- Nowak, G.J.; Gellin, B.G.; MacDonald, N.E.; Butler, R.; Eskola, J.; Liang, X.; Chaudhuri, M.; Dube, E.; Gellin, B.; Goldstein, S.; et al. Addressing vaccine hesitancy: The potential value of commercial and social marketing principles and practices. Vaccine 2015, 33, 4204–4211. [Google Scholar] [CrossRef] [Green Version]
- Jarrett, C.; Wilson, R.; O’Leary, M.; Eckersberger, E.; Larson, H.J.; Eskola, J.; Liang, X.; Chaudhuri, M.; Dube, E.; Gellin, B.; et al. Strategies for addressing vaccine hesitancy—A systematic review. Vaccine 2015, 33, 4180–4190. [Google Scholar] [CrossRef] [Green Version]
| Characteristic | N | % | % No Vaccination | % Partial Vaccination | % Completed Vaccination |
|---|---|---|---|---|---|
| Study population | 3,186,728 | 100 | 10.3 | 1.5 | 88.1 |
| Sex | |||||
| Males | 1,467,434 | 46.0 | 10.0 | 1.5 | 88.4 |
| Females | 1,719,294 | 54.0 | 10.6 | 1.5 | 87.9 |
| Age, mean (sd) | 58.9 (14.3) | 56.2 (14.8) | 53.8 (13.9) | 59.3 (14.2) | |
| Place of birth | |||||
| Italy | 2,931,917 | 92.0 | 9.0 | 1.5 | 89.5 |
| Other Countries | 254,811 | 8.0 | 25.4 | 2.1 | 72.5 |
| Level of education 1 | |||||
| High | 576,382 | 18.1 | 8.9 | 1.4 | 89.7 |
| Medium | 1,245,099 | 39.1 | 11.0 | 1.6 | 87.4 |
| Low | 1,365,247 | 42.8 | 10.4 | 1.5 | 88.1 |
| Deprivation quantile 2 | |||||
| Q1 (low) | 647,691 | 20.3 | 9.2 | 1.3 | 89.5 |
| Q2 | 642,586 | 20.2 | 9.7 | 1.4 | 88.9 |
| Q3 | 637,238 | 20.0 | 10.0 | 1.5 | 88.5 |
| Q4 | 627,070 | 19.7 | 10.7 | 1.6 | 87.8 |
| Q5 (high) | 616,831 | 19.4 | 11.9 | 1.8 | 86.4 |
| Number of chronic conditions | |||||
| 0 | 1,597,725 | 50.1 | 13.0 | 1.9 | 85.1 |
| 1 | 738,096 | 23.2 | 8.5 | 1.3 | 90.2 |
| 2 | 403,689 | 12.7 | 7.1 | 1.1 | 91.8 |
| 3+ | 447,218 | 14.0 | 6.7 | 1.0 | 92.4 |
| Characteristic | OR1 | 95%CI | OR2 | 95%CI | ||
|---|---|---|---|---|---|---|
| Sex | ||||||
| Males | 1.000 | 1.000 | ||||
| Females | 1.086 | 1.078 | 1.094 | 1.063 | 1.055 | 1.071 |
| Age (1 year increase) | 0.985 | 0.985 | 0.985 | 0.996 | 0.996 | 0.997 |
| Place of birth | ||||||
| Italy | 1.000 | 1.000 | ||||
| Other Countries | 3.187 | 3.155 | 3.218 | 2.968 | 2.938 | 2.998 |
| Level of Education * | ||||||
| High | 1.000 | 1.000 | ||||
| Medium | 1.288 | 1.274 | 1.301 | 1.253 | 1.239 | 1.267 |
| Low | 1.414 | 1.399 | 1.430 | 1.391 | 1.375 | 1.407 |
| Deprivation Quantile | ||||||
| Q1 (Low) | 1.000 | 1.000 | ||||
| Q2 | 1.048 | 1.036 | 1.060 | 1.029 | 1.016 | 1.041 |
| Q3 | 1.073 | 1.061 | 1.086 | 1.037 | 1.024 | 1.050 |
| Q4 | 1.152 | 1.138 | 1.165 | 1.086 | 1.073 | 1.099 |
| Q5 (High) | 1.308 | 1.294 | 1.324 | 1.218 | 1.203 | 1.232 |
| Number of Chronic Conditions | ||||||
| 0 | 1.000 | 1.000 | ||||
| 1 | 0.651 | 0.645 | 0.658 | 0.664 | 0.657 | 0.671 |
| 2 | 0.552 | 0.545 | 0.560 | 0.563 | 0.555 | 0.571 |
| 3+ | 0.531 | 0.523 | 0.538 | 0.537 | 0.529 | 0.544 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cesaroni, G.; Calandrini, E.; Balducci, M.; Cappai, G.; Di Martino, M.; Sorge, C.; Nicastri, E.; Agabiti, N.; Davoli, M. Educational Inequalities in COVID-19 Vaccination: A Cross-Sectional Study of the Adult Population in the Lazio Region, Italy. Vaccines 2022, 10, 364. https://doi.org/10.3390/vaccines10030364
Cesaroni G, Calandrini E, Balducci M, Cappai G, Di Martino M, Sorge C, Nicastri E, Agabiti N, Davoli M. Educational Inequalities in COVID-19 Vaccination: A Cross-Sectional Study of the Adult Population in the Lazio Region, Italy. Vaccines. 2022; 10(3):364. https://doi.org/10.3390/vaccines10030364
Chicago/Turabian StyleCesaroni, Giulia, Enrico Calandrini, Maria Balducci, Giovanna Cappai, Mirko Di Martino, Chiara Sorge, Emanuele Nicastri, Nera Agabiti, and Marina Davoli. 2022. "Educational Inequalities in COVID-19 Vaccination: A Cross-Sectional Study of the Adult Population in the Lazio Region, Italy" Vaccines 10, no. 3: 364. https://doi.org/10.3390/vaccines10030364
APA StyleCesaroni, G., Calandrini, E., Balducci, M., Cappai, G., Di Martino, M., Sorge, C., Nicastri, E., Agabiti, N., & Davoli, M. (2022). Educational Inequalities in COVID-19 Vaccination: A Cross-Sectional Study of the Adult Population in the Lazio Region, Italy. Vaccines, 10(3), 364. https://doi.org/10.3390/vaccines10030364







