Understanding the Variability of Certain Biological Properties of H1N1pdm09 Influenza Viruses
Abstract
1. Introduction
2. Materials and Methods
3. Results
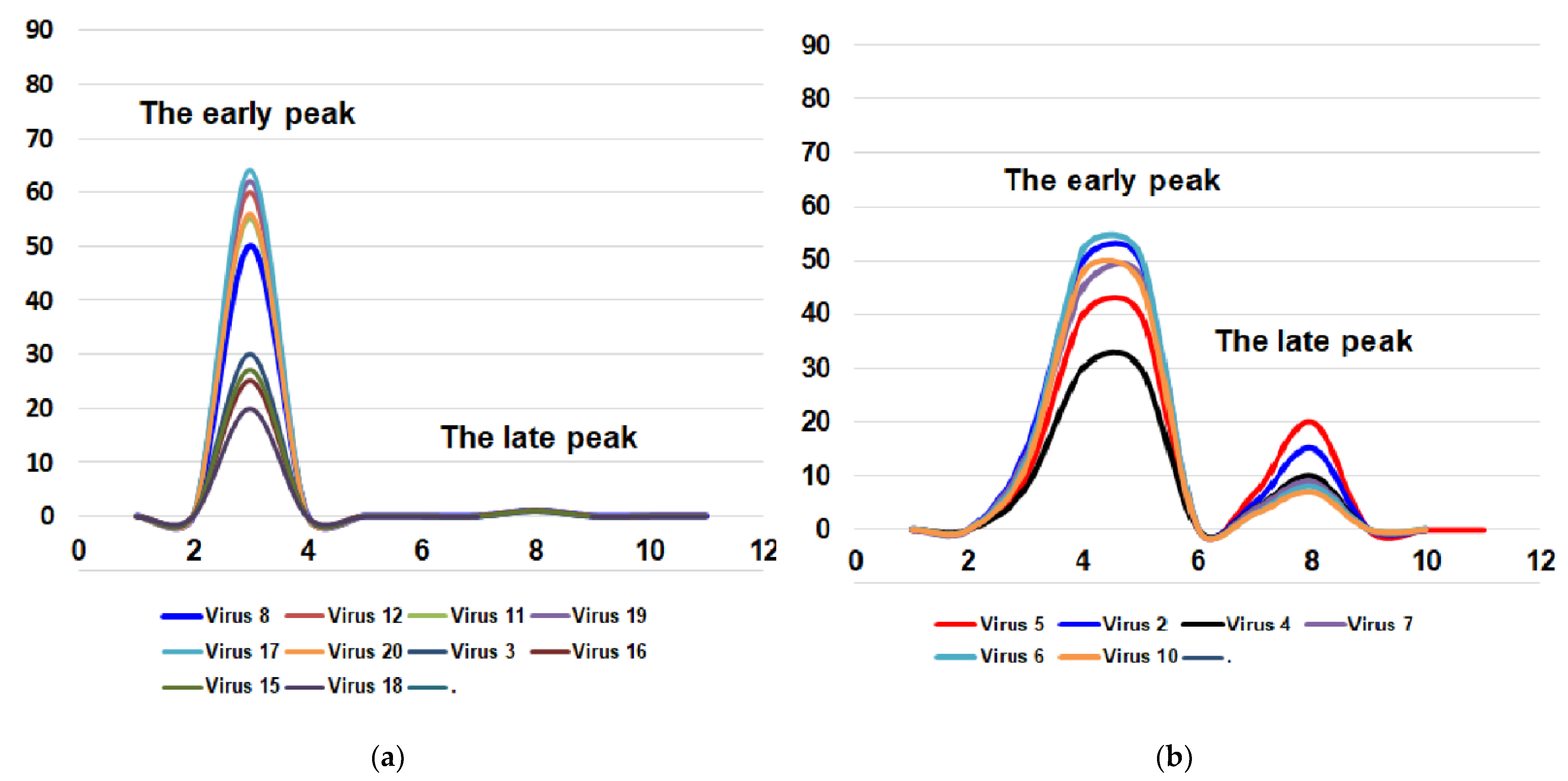
3.1. Toxicity for Mice
3.2. Pathogenicity for Mice
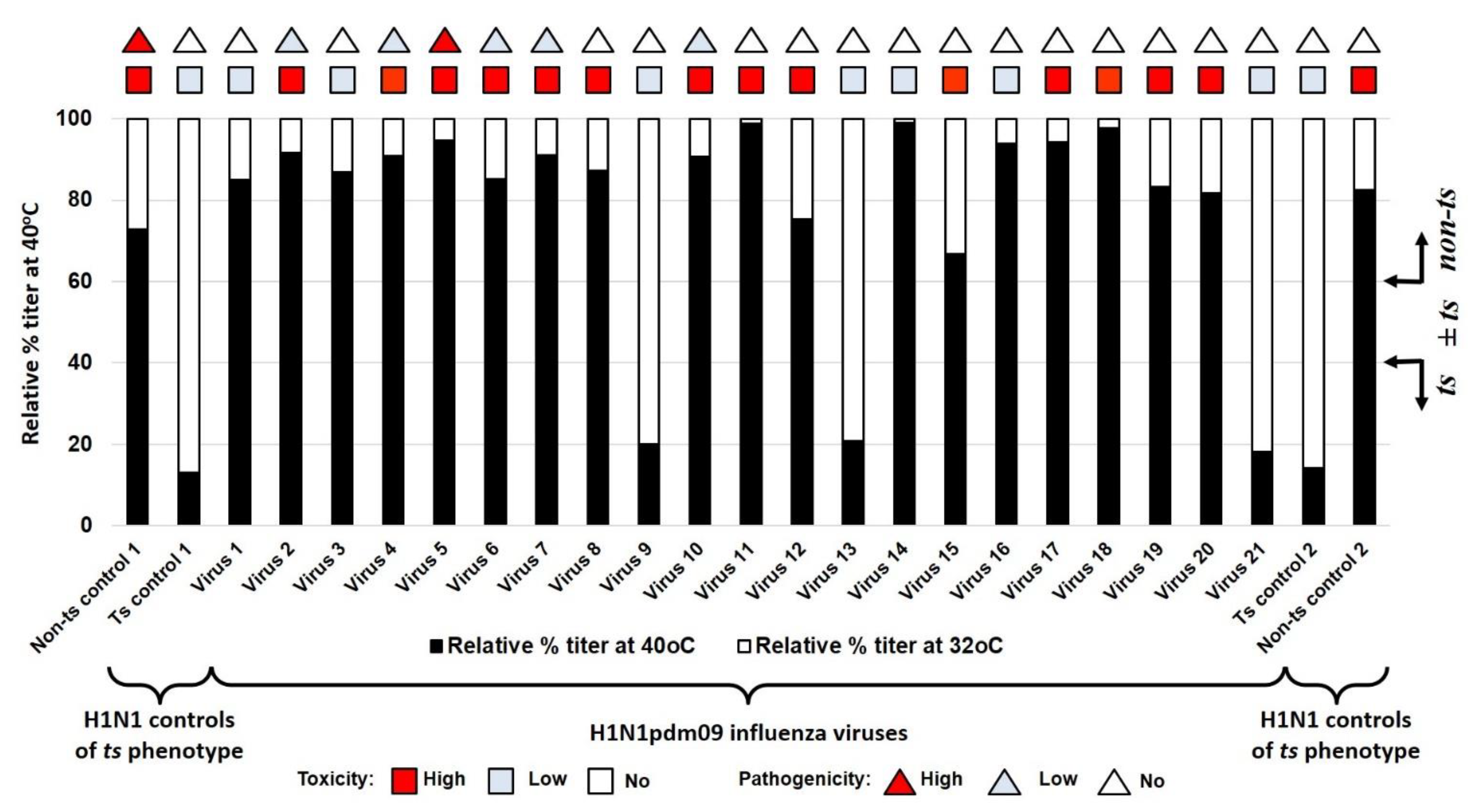
3.3. Temperature Sensitivity of Reproduction of A(H1N1)pdm09 Influenza Viruses (ts Phenotype)
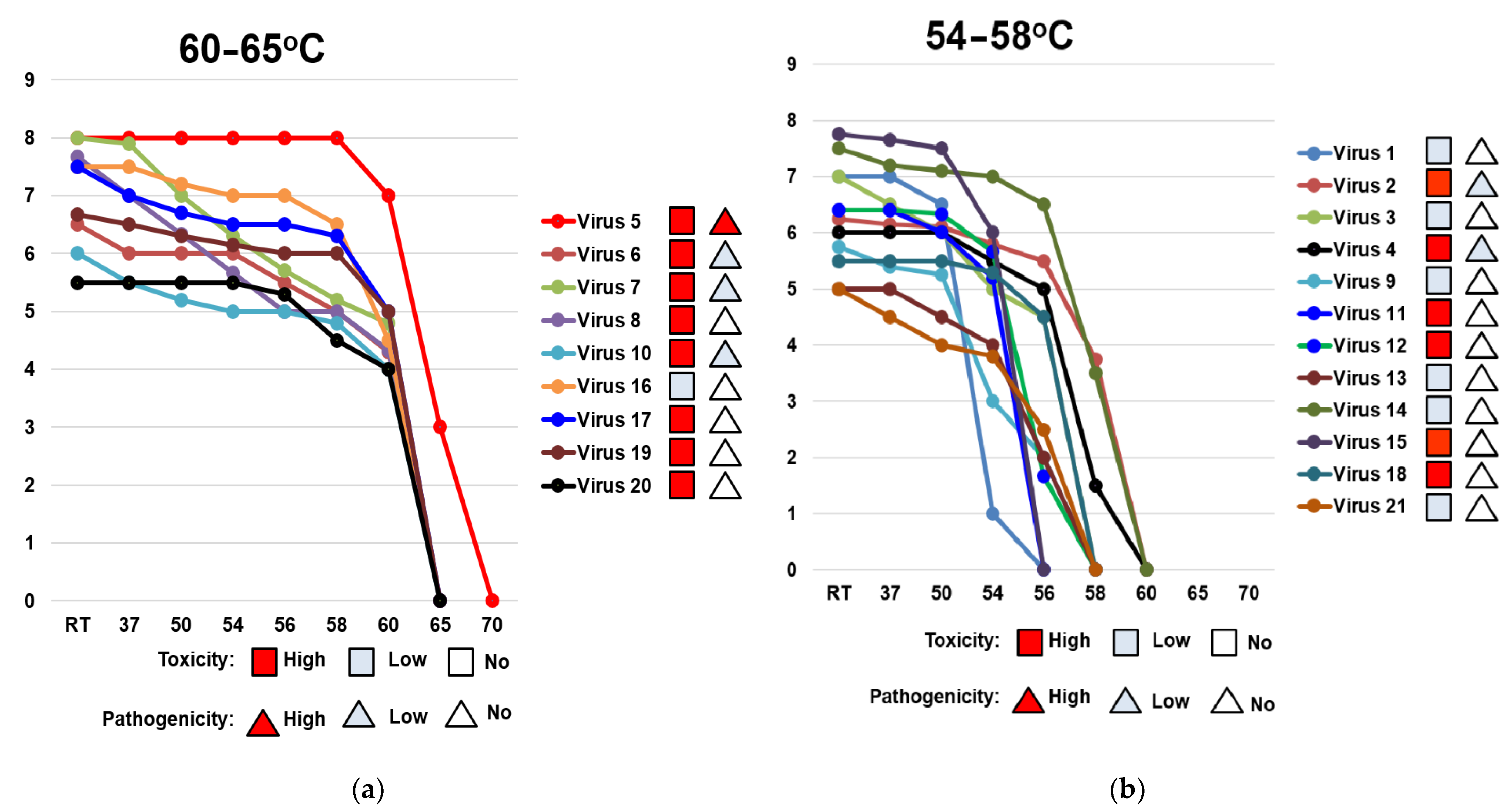
3.4. Thermal Stability of the Hemagglutinin of A(H1N1)pdm09 Viruses
3.5. Phylogenetic Trees of A(H1N1)pdm09 Influenza Viruses Genes
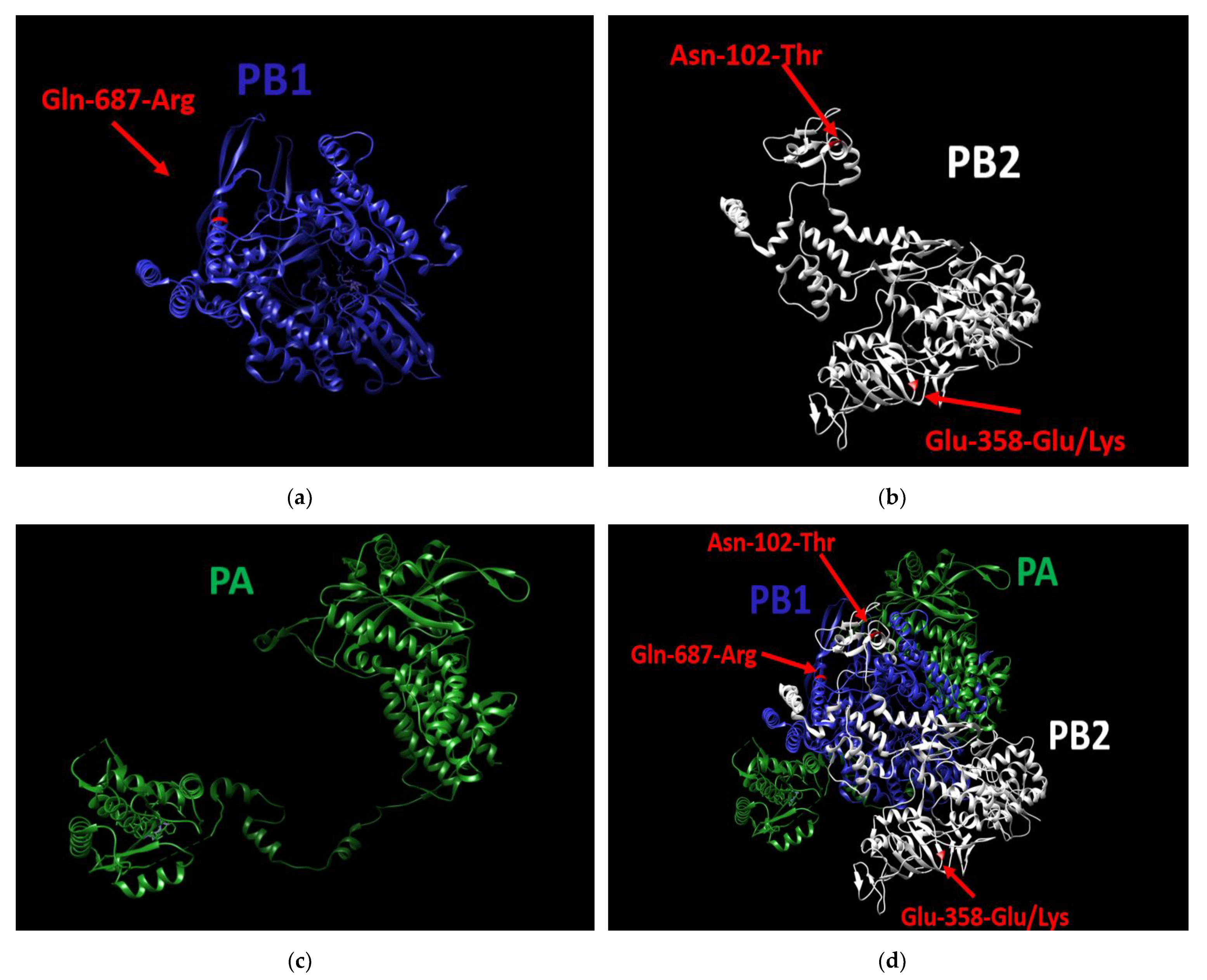
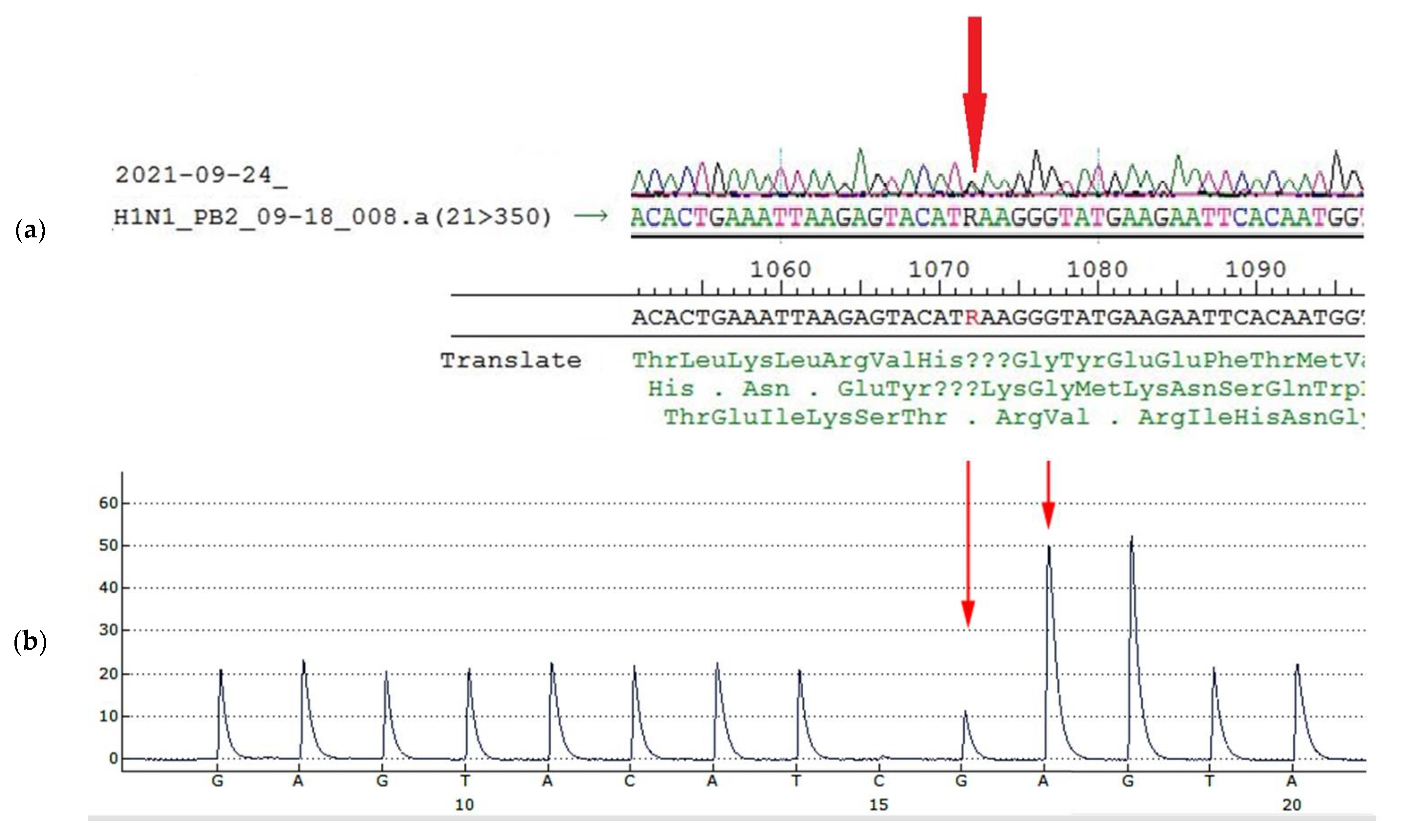
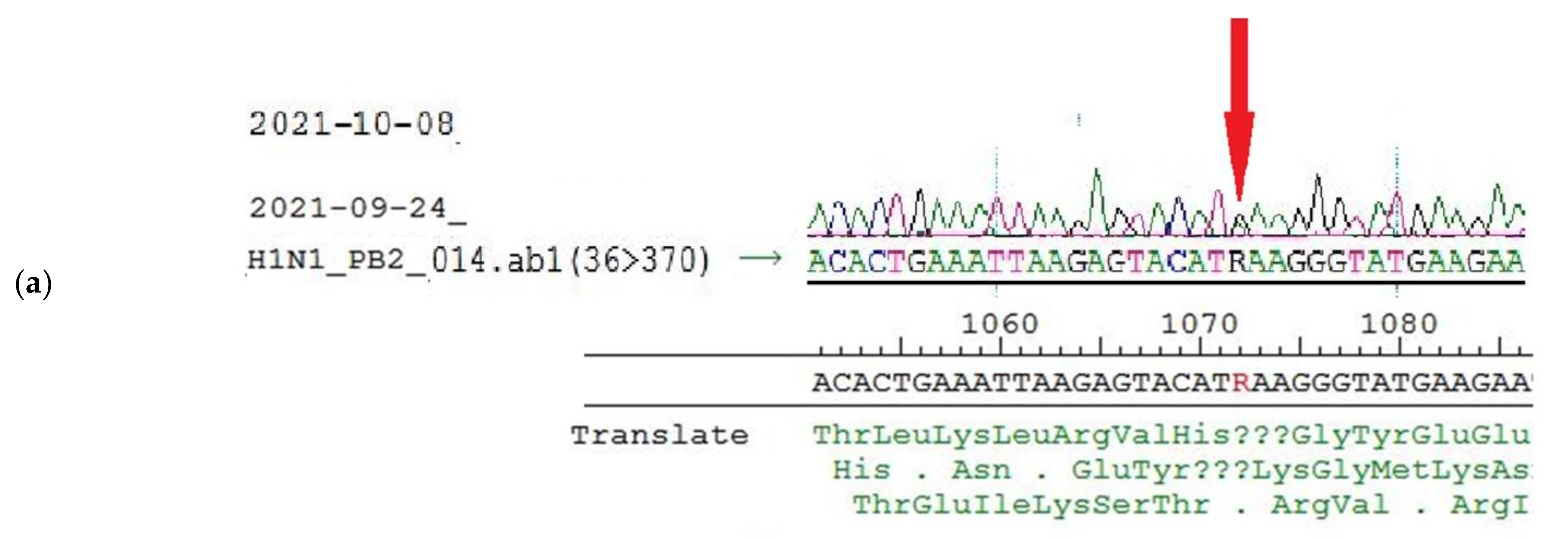
3.6. Presumed Molecular Basis for High Pathogenicity and Toxicity as A(H1N1)pdm09 Viral Properties
4. Discussion
5. Conclusions
6. Limitations
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Seasonal Ifluenza. Available online: https://www.euro.who.int/en/health-topics/communicable-diseases/influenza/seasonal-influenza (accessed on 1 February 2022).
- Spreeuwenberg, P.; Kroneman, M.; Paget, J. Reassessing the global mortality burden of the 1918 influenza pandemic. Am. J. Epidemiol. 2018, 187, 2561–2567. [Google Scholar] [CrossRef] [PubMed]
- WHO. Pandemic Influenza Risk Management Interim Guidance. Available online: https://www.icao.int/APAC/Meetings/2014%20CAPSCAAP7/Pandemic%20Influenza_Risk%20Management_Interim%20Guidance_Jun%202013%20WHO.pdf (accessed on 1 February 2022).
- Michaelis, M.; Doerr, H.W.; Cinatl, J., Jr. Novel swine-origin influenza A virus in humans: Another pandemic knocking at the door. Med. Microbiol. Immunol. 2009, 198, 175–183. [Google Scholar] [CrossRef] [PubMed]
- WHO. Pandemic Influenza. Available online: https://www.euro.who.int/en/health-topics/communicable-diseases/influenza/pandemic-influenza (accessed on 1 February 2022).
- Petrova, V.N.; Russell, C.A. The evolution of seasonal influenza viruses. Nat. Rev. Microbiol. 2018, 16, 47–60. [Google Scholar] [CrossRef] [PubMed]
- Lowen, A.C.; Mubareka, S.; Tumpey, T.M.; Garcia-Sastre, A.; Palese, P. The guinea pig as a transmission model for human influenza viruses. Proc. Natl. Acad. Sci. USA 2006, 103, 9988–9992. [Google Scholar] [CrossRef]
- Kiseleva, I.; Larionova, N.; Kuznetsov, V.; Rudenko, L. Phenotypic characteristics of novel swine-origin influenza A/California/07/2009 (H1N1) virus. Influenza Other Respir. Viruses 2010, 4, 1–5. [Google Scholar] [CrossRef]
- Lyons, D.M.; Lauring, A.S. Mutation and epistasis in influenza virus evolution. Viruses 2018, 10, 407. [Google Scholar] [CrossRef]
- Cox, N.J.; Kitame, F.; Kendal, A.P.; Maassab, H.F.; Naeve, C. Identification of sequence changes in the cold-adapted, live attenuated influenza vaccine strain, A/Ann Arbor/6/60 (H2N2). Virology 1988, 167, 554–567. [Google Scholar] [CrossRef]
- Herlocher, M.L.; Maassab, H.F.; Webster, R.G. Molecular and biological changes in the cold-adapted “master strain” A/AA/6/60 (H2N2) influenza virus. Proc. Natl. Acad. Sci. USA 1993, 90, 6032–6036. [Google Scholar] [CrossRef]
- Reeve, P.; Almond, J.W.; Felsenreich, V.; Pibermann, M.; Maassab, H.F. Studies with a cold-recombinant A/Victoria/3/75 (H3N2) virus. I. biologic, genetic, and biochemical characterization. J. Infect. Dis. 1980, 142, 850–856. [Google Scholar] [CrossRef]
- Larionova, N.; Kiseleva, I.; Isakova, I.; Litvinova, O.; Klimov, A.; Rudenko, L. Naturally occurring temperature-sensitive strains of influenza B virus. In Proceedings of the IVW-2004 Conference, Lisbon, Portugal, 24–26 May 2004; pp. 92–97. [Google Scholar]
- Kiseleva, I.; Larionova, N. Influenza virus ecology and evolution. In Influenza: A Century of Research; Kiseleva, I., Larionova, N., Eds.; Bentham Science Publisher: Sharjah, United Arab Emirates, 2021; pp. 63–97. [Google Scholar] [CrossRef]
- Henle, G.; Henle, W. Studies on the toxicity of influenza viruses: I. The effect of intracerebral injection of influenza viruses. J. Exp. Med. 1946, 84, 623–637. [Google Scholar] [CrossRef][Green Version]
- Henle, W.; Henle, G. Studies on the toxicity of influenza viruses. J Bacteriol. 1946, 51, 632. [Google Scholar] [PubMed]
- Henle, W.; Henle, G. Studies on the toxicity of influenza viruses. II. The effect of intra-abdominal and intravenous injection of influenza viruses. J. Exp. Med. 1946, 84, 639–660. [Google Scholar] [CrossRef] [PubMed]
- Nakowitsch, S.; Wolschek, M.; Morokutti, A.; Ruthsatz, T.; Krenn, B.M.; Ferko, B.; Ferstl, N.; Triendl, A.; Muster, T.; Egorov, A.; et al. Mutations affecting the stability of the haemagglutinin molecule impair the immunogenicity of live attenuated H3N2 intranasal influenza vaccine candidates lacking NS1. Vaccine 2011, 29, 3517–3524. [Google Scholar] [CrossRef] [PubMed]
- Pflug, A.; Lukarska, M.; Resa-Infante, P.; Reich, S.; Cusack, S. Structural insights into RNA synthesis by the influenza virus transcription-replication machine. Virus Res. 2017, 234, 103–117. [Google Scholar] [CrossRef] [PubMed]
- De Vlugt, C.; Sikora, D.; Pelchat, M. Insight into influenza: A virus cap-snatching. Viruses 2018, 10, 641. [Google Scholar] [CrossRef]
- Bouvier, N.M.; Palese, P. The biology of influenza viruses. Vaccine 2008, 26, D49–D53. [Google Scholar] [CrossRef]
- Isakova-Sivak, I.; Chen, L.M.; Matsuoka, Y.; Voeten, J.T.; Kiseleva, I.; Heldens, J.G.; den Bosch, H.; Klimov, A.; Rudenko, L.; Cox, N.J.; et al. Genetic bases of the temperature-sensitive phenotype of a master donor virus used in live attenuated influenza vaccines: A/Leningrad/134/17/57 (H2N2). Virology 2011, 412, 297–305. [Google Scholar] [CrossRef]
- Kiseleva, I.V.; Larionova, N.V.; Voeten, J.T.; Teley, L.C.; Drieszen-van der Cruijsen, S.K.; Heldens, J.G.; van den Bosch, J.F.; Rudenko, L.G. Leading role of genes coding polymerase complex in attenuation of domestic donor viruses for A and B live influenza vaccine. Zhurnal Mikrobiol. Epidemiol. Immunobiol. 2010, 6, 41–47. [Google Scholar]
- Kiseleva, I.V.; Voeten, J.T.; Teley, L.C.; Larionova, N.V.; Drieszen-van der Cruijsen, S.K.; Basten, S.M.; Heldens, J.G.; van den Bosch, H.; Rudenko, L.G. PB2 and PA genes control the expression of the temperature-sensitive phenotype of cold-adapted B/USSR/60/69 influenza master donor virus. J. Gen. Virol. 2010, 91, 931–937. [Google Scholar] [CrossRef]
- Klimov, A.I.; Kiseleva, I.V.; Alexandrova, G.I.; Cox, N.J. Genes coding for polymerase proteins are essential for attenuation of the cold–adapted A/Leningrad/134/17/57 (H2N2) influenza virus. In Proceedings of the Options for the Control of Influenza IV, Crete, Greece, 23–28 September 2000; pp. 955–959. [Google Scholar]
- IRD. Influenza Research Database. Available online: https://www.fludb.org/brc/home.spg?decorator=influenza (accessed on 2 December 2021).
- Reed, L.J.; Muench, H. A simple method of estimating fifty per cent endpoints. Am. J. Epidemiol. 1938, 27, 493–497. [Google Scholar] [CrossRef]
- Scholtissek, C. Stability of infectious influenza A viruses at low pH and at elevated temperature. Vaccine 1985, 3, 215–218. [Google Scholar] [CrossRef]
- Kiseleva, I.; Rekstin, A.; Al Farroukh, M.; Bazhenova, E.; Katelnikova, A.; Puchkova, L.; Rudenko, L. Non-mouse-adapted H1N1pdm09 virus as a model for influenza research. Viruses 2020, 12, 590. [Google Scholar] [CrossRef] [PubMed]
- Karkishenko, N.N.; Grachev, C.V. Manual for Laboratory Animals and Alternative Models in Biomedical Research. Moscow, Russia: Profile-2S. 2010. Available online: http://www.scbmt.ru/mag/rukovodstvo.pdf (accessed on 4 December 2021).
- European_Council. Directive 2010/63/EU of the European Parliament and of the Council of September 22, 2010, on the Protection of Animals Used for Scientific Purposes. Available online: http://eur-lex.europa.eu/legal-content/EN/TXT/?uri=celex%3A32010L0063 (accessed on 2 December 2021).
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. Jama 2013, 310, 2191–2194. [Google Scholar] [CrossRef] [PubMed]
- Russian Sanitary and Epidemiological Requirements for the Prevention of Infectious Diseases SP 3.3686-21 (approved 28 January 2021). Available online: https://www.rospotrebnadzor.ru/files/news/SP_infections_compressed.pdf (accessed on 2 December 2021).
- Isakova-Sivak, I.; Stepanova, E.; Mezhenskaya, D.; Matyushenko, V.; Prokopenko, P.; Sychev, I.; Wong, P.F.; Rudenko, L. Influenza vaccine: Progress in a vaccine that elicits a broad immune response. Expert Rev. Vaccines 2021, 20, 1097–1112. [Google Scholar] [CrossRef]
- Chu, C.M.; Tian, S.F.; Ren, G.F.; Zhang, Y.M.; Zhang, L.X.; Liu, G.Q. Occurrence of temperature-sensitive influenza A viruses in nature. J. Virol. 1982, 41, 353–359. [Google Scholar] [CrossRef]
- Yamaya, M.; Nishimura, H.; Lusamba Kalonji, N.; Deng, X.; Momma, H.; Shimotai, Y.; Nagatomi, R. Effects of high temperature on pandemic and seasonal human influenza viral replication and infection-induced damage in primary human tracheal epithelial cell cultures. Heliyon 2019, 5, e01149. [Google Scholar] [CrossRef]
- Kiseleva, I.V.; Klimov, A.I.; Grigor’eva, E.P.; Larionova, N.V.; Aleksandrova, G.I.; Rudenko, L.G. Genetic and phenotypic analysis of heterogeneous population of a cold-adapted donor of the A/Leningrad/134/17/57 (H2N2) attenuation and of the donor-based reassortant influenza vaccine strains. Vopr. Virusol. 2005, 50, 14–18. [Google Scholar]
- Maassab, H.F.; DeBorde, D.C. Development and characterization of cold-adapted viruses for use as live virus vaccines. Vaccine 1985, 3, 355–369. [Google Scholar] [CrossRef]
- Rudenko, L.G.; Kiseleva, I.V.; Larionova, N.V.; Grigorieva, E.P.; Naikhin, A.N. Analysis of some factors influencing immunogenicity of live cold–adapted reassortant influenza vaccines. In Proceedings of the Options for the Control of Influenza V, Okinawa, Japan, 6–9 October 2003; pp. 542–546. [Google Scholar]
- Massin, P.; van der Werf, S.; Naffakh, N. Residue 627 of PB2 is a determinant of cold sensitivity in RNA replication of avian influenza viruses. J. Virol. 2001, 75, 5398–5404. [Google Scholar] [CrossRef]
- Giles, B.M.; Ross, T.M. A computationally optimized broadly reactive antigen (COBRA) based H5N1 VLP vaccine elicits broadly reactive antibodies in mice and ferrets. Vaccine 2011, 29, 3043–3054. [Google Scholar] [CrossRef]
- McCauley, J.W.; Penn, C.R. The critical cut-off temperature of avian influenza viruses. Virus Res. 1990, 17, 191–198. [Google Scholar] [CrossRef]
- Mims, C.A. An analysis of the toxicity for mice of influenza virus. II. Intravenous toxicity. Br. J. Exp. Pathol. 1960, 41, 593–598. [Google Scholar] [PubMed]
- Fang, J.; Bredow, S.; Taishi, P.; Majde, J.A.; Krueger, J.M. Synthetic influenza viral double-stranded RNA induces an acute-phase response in rabbits. J. Med Virol. 1999, 57, 198–203. [Google Scholar] [CrossRef]
- Kimura-Takeuchi, M.; Majde, J.A.; Toth, L.A.; Krueger, J.M. The role of double-stranded RNA in induction of the acute-phase response in an abortive influenza virus infection model. J. Infect. Dis. 1992, 166, 1266–1275. [Google Scholar] [CrossRef] [PubMed]
- Majde, J.A.; Brown, R.K.; Jones, M.W.; Dieffenbach, C.W.; Maitra, N.; Krueger, J.M.; Cady, A.B.; Smitka, C.W.; Maassab, H.F. Detection of toxic viral-associated double-stranded RNA (dsRNA) in influenza-infected lung. Microb. Pathog. 1991, 10, 105–115. [Google Scholar] [CrossRef]
- Majde, J.A. Viral double-stranded RNA, cytokines, and the flu. J. Interferon. Cytokine Res. 2000, 20, 259–272. [Google Scholar] [CrossRef] [PubMed]
- Kiseleva, I.; Larionova, N. Influenza prophylaxis and treatment. In Influenza: A Century of Research; Kiseleva, I., Larionova, N., Eds.; Bentham Science Publisher: Sharjah, United Arab Emirates, 2021; pp. 98–141. [Google Scholar] [CrossRef]
- Kiseleva, I.; Larionova, N. Life cycle of influenza virus. In Influenza: A Century of Research; Kiseleva, I., Larionova, N., Eds.; Bentham Science Publisher: Sharjah, United Arab Emirates, 2021; pp. 26–62. [Google Scholar] [CrossRef]
- Choi, E.J.; Lee, Y.J.; Lee, J.M.; Kim, Y.J.; Choi, J.H.; Ahn, B.; Kim, K.; Han, M.G. The effect of mutations derived from mouse-adapted H3N2 seasonal influenza A virus to pathogenicity and host adaptation. PLoS ONE 2020, 15, e0227516. [Google Scholar] [CrossRef]
- Gabriel, G.; Czudai-Matwich, V.; Klenk, H.D. Adaptive mutations in the H5N1 polymerase complex. Virus Res. 2013, 178, 53–62. [Google Scholar] [CrossRef]
- Gabriel, G.; Fodor, E. Molecular determinants of pathogenicity in the polymerase complex. Curr. Top. Microbiol. Immunol. 2014, 385, 35–60. [Google Scholar] [CrossRef]
- Hu, M.; Yuan, S.; Zhang, K.; Singh, K.; Ma, Q.; Zhou, J.; Chu, H.; Zheng, B.J. PB2 substitutions V598T/I increase the virulence of H7N9 influenza A virus in mammals. Virology 2017, 501, 92–101. [Google Scholar] [CrossRef]
- Manz, B.; Schwemmle, M.; Brunotte, L. Adaptation of avian influenza A virus polymerase in mammals to overcome the host species barrier. J. Virol. 2013, 87, 7200–7209. [Google Scholar] [CrossRef] [PubMed]
- Mok, C.K.; Lee, H.H.; Lestra, M.; Nicholls, J.M.; Chan, M.C.; Sia, S.F.; Zhu, H.; Poon, L.L.; Guan, Y.; Peiris, J.S. Amino acid substitutions in polymerase basic protein 2 gene contribute to the pathogenicity of the novel A/H7N9 influenza virus in mammalian hosts. J. Virol. 2014, 88, 3568–3576. [Google Scholar] [CrossRef] [PubMed]
- Ping, J.; Dankar, S.K.; Forbes, N.E.; Keleta, L.; Zhou, Y.; Tyler, S.; Brown, E.G. PB2 and hemagglutinin mutations are major determinants of host range and virulence in mouse-adapted influenza A virus. J. Virol. 2010, 84, 10606–10618. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Frandsen, A.; Alfonso, R.; Nieto, A. Influenza virus polymerase: Functions on host range, inhibition of cellular response to infection and pathogenicity. Virus Res. 2015, 209, 23–38. [Google Scholar] [CrossRef] [PubMed]
- Song, H.; Qi, J.; Khedri, Z.; Diaz, S.; Yu, H.; Chen, X.; Varki, A.; Shi, Y.; Gao, G.F. An open receptor-binding cavity of hemagglutinin-esterase-fusion glycoprotein from newly-identified influenza D virus: Basis for its broad cell tropism. PLoS pathogens 2016, 12, e1005411. [Google Scholar] [CrossRef]
- Tan, L.; Su, S.; Smith, D.K.; He, S.; Zheng, Y.; Shao, Z.; Ma, J.; Zhu, H.; Zhang, G. A combination of HA and PA mutations enhances virulence in a mouse-adapted H6N6 influenza A virus. J. Virol. 2014, 88, 14116–14125. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, T.; Tisoncik-Go, J.; Tchitchek, N.; Watanabe, S.; Benecke, A.G.; Katze, M.G.; Kawaoka, Y. 1918 influenza virus hemagglutinin (HA) and the viral RNA polymerase complex enhance viral pathogenicity, but only HA induces aberrant host responses in mice. J. Virol. 2013, 87, 5239–5254. [Google Scholar] [CrossRef]
- Yamayoshi, S.; Yamada, S.; Fukuyama, S.; Murakami, S.; Zhao, D.; Uraki, R.; Watanabe, T.; Tomita, Y.; Macken, C.; Neumann, G.; et al. Virulence-affecting amino acid changes in the PA protein of H7N9 influenza A viruses. J. Virol. 2014, 88, 3127–3134. [Google Scholar] [CrossRef]
- Yen, H.L.; Liang, C.H.; Wu, C.Y.; Forrest, H.L.; Ferguson, A.; Choy, K.T.; Jones, J.; Wong, D.D.; Cheung, P.P.; Hsu, C.H.; et al. Hemagglutinin-neuraminidase balance confers respiratory-droplet transmissibility of the pandemic H1N1 influenza virus in ferrets. Proc. Natl. Acad. Sci. USA 2011, 108, 14264–14269. [Google Scholar] [CrossRef]
- Hale, B.G.; Randall, R.E.; Ortín, J.; Jackson, D. The multifunctional NS1 protein of influenza A viruses. J. Gen. Virol. 2008, 89, 2359–2376. [Google Scholar] [CrossRef]
- Pflug, A.; Guilligay, D.; Reich, S.; Cusack, S. Structure of influenza A polymerase bound to the viral RNA promoter. Nature 2014, 516, 355–360. [Google Scholar] [CrossRef] [PubMed]
- Sugiyama, K.; Obayashi, E.; Kawaguchi, A.; Suzuki, Y.; Tame, J.R.; Nagata, K.; Park, S.Y. Structural insight into the essential PB1-PB2 subunit contact of the influenza virus RNA polymerase. EMBO J. 2009, 28, 1803–1811. [Google Scholar] [CrossRef] [PubMed]




| A(H1N1)pdm09 Strain No/Designation | Source | Clade/Subclade | |
|---|---|---|---|
| 1 1 | A/CALIFORNIA/07/2009 | 2 CDC ID 2009712112 | 6 n.a. |
| 2 | A/Bolivia/559/2013 | CDC ID 2013760341 | 6B |
| 3 | A/Mississippi/10/2013 | CDC ID 2014700252 | 6B |
| 4 | A/New Hampshire/04/2013 | CDC ID 2013845913 | 6B |
| 5 | A/South Africa/3626/2013 | CDC ID 2014701384 | 6B |
| 6 | A/Florida/62/2014 | CDC ID 3000097732 | 6B |
| 7 | A/Laos/1187/2014 | CDC ID 3000095267 | 6B.1 |
| 8 | A/New York/61/2015 | CDC ID 3000412528 | 6B.1 |
| 9 | A/Slovenia/2903/2015 | 3 NIBSC lot 41730 | 6B.1 |
| 10 | A/Bangladesh/3002/2015 | CDC ID 3000411636 | 6B |
| 11 | A/Newcastle/67/2017 | WHO-CC ID 322513509 | 6B.1 |
| 12 | A/South Australia/272/2017 | WHO-CC ID 17-62350735 | 6B.1A |
| 13 | A/New Jersey/13/2018 | CDC ID 3026016623 | 6B.1A.1 |
| 14 | A/Darwin/123/2018 | WHO-CC ID 10010145 | 6B.1A5A |
| 15 | A/Brisbane/02/2018 | 4 WHO-CC ID SS18S304 | 6B.1A.1 |
| 16 | A/lowa/59/2018 | CDC ID 3026018252 | 6B.1A5A |
| 17 | A/lowa/12/2019 | CDC ID 3026019744 | 6B.1A5B |
| 18 | A/Victoria/2570/2019 | WHO-CC ID 10033413 | 6B.1A5A-156K |
| 19 | A/Guangdong-Maonan/SWL1536/2019 | NIBSC code 19/294 | 6B.1A5A-187A |
| 20 | A/Indiana/02/2020 | CDC ID 3026055186 | 6B.1A5A-156K |
| 21 | A/Arkansas/08/2020 | CDC ID 3026055197 | 6B.1A5A-156K |
| A(H1N1) past influenza viruses used as controls for evaluation of ts/non-ts phenotype | |||
| 22 | non-ts control 1, A/PR/8/34 | 5 ATCC ID VR-1469 | 6 n.a. |
| 23 | non-ts control 2, A/New Caledonia/20/99 | NIBSC code 07/226 | 7 delta-like clade |
| 24 | ts control 1, A/Florida/3/06 | ATCC ID VR-1893 | 7 delta2 |
| 25 | ts control 2, A/Solomon Islands/3/06 | NIBSC code 06/236 | 7 delta-like clade |
| Parameters | High | Low | No (Absence) |
|---|---|---|---|
| Toxicity for mice, %, on day six | >50  | ≤50  | 0  |
| Pathogenicity for mice, on day 14, log10 LD50 | ≥4.0  | ≤4.0  | <1.5 1  |
| A(H1N1)pdm09 Virus No/Designation | Acute Toxicity on D6 1 | Pathogenicity on Day 14 2 | ||||
|---|---|---|---|---|---|---|
| Lethality, % | Level of Toxicity | log LD50 3 | 1 LD50 in log EID50/mL 4 | Level of Pathogenicity | ||
| 1 | A/CALIFORNIA/7/2009 | 10% | low | <1.5 | >8.0 | No |
| 2 | A/Bolivia/559/2013 | 100% | high | 1.6 | 6.6 | low |
| 3 | A/Mississippi/10/2013 | 40% | low | <1.5 | >8.4 | No |
| 4 | A/New Hampshire/04/2013 | 50% | low | 1.7 | 6.5 | low |
| 5 | A/South Africa/3626/2013 | 80% | high | 5.0 | 4.2 | high |
| 6 | A/Florida/62/2014 | 80% | high | 2.0 | 5.5 | low |
| 7 | A/Laos/1187/2014 | 100% | high | 1.9 | 6.1 | low |
| 8 | A/New York/61/2015 | 60% | high | <1.5 | 6.6 | No |
| 9 | A/Slovenia/2903/2015 | 20% | low | <1.5 | >8.1 | No |
| 10 | A/Bangladesh/3002/2015 | 100% | high | 1.6 | 6.6 | low |
| 11 | A/Newcastle/67/2017 | 80% | high | <1.5 | >8.4 | No |
| 12 | A/South Australia/272/2017 | 90% | high | <1.5 | >8.4 | No |
| 13 | A/New Jersey/13/2018 | 10% | low | <1.5 | >7.2 | No |
| 14 | A/Darwin/123/2018 | 27% | low | <1.5 | >9.0 | No |
| 15 | A/Brisbane/02/2018 | 50% | low | <1.5 | >8.5 | No |
| 16 | A/Iowa/59/2018 | 40% | low | <1.5 | >8.2 | No |
| 17 | A/Iowa/12/2019 | 100% | high | <1.5 | 6.6 | No |
| 18 | A/Victoria/2570/2019 | 50% | low | <1.5 | >8.4 | No |
| 19 | A/Guangdong-Maonan/SWL1536/2019 | 90% | high | <1.5 | >9.0 | No |
| 20 | A/Arkansas/08/2020 | 80% | high | <1.5 | >8.2 | No |
| 21 | A/Indiana/02/20 | 20% | low | <1.5 | >8.3 | No |
| A(H1N1)pdm09 Virus No/Designation | HA Activity Temp. Threshold 1 | ||
|---|---|---|---|
| 1 | A/CALIFORNIA/07/2009 | 54 °C | Low |
| 2 | A/Bolivia/559/2013 | 58 °C | Low |
| 3 | A/Mississippi/10/2013 | 56 °C | Low |
| 4 | A/New Hampshire/04/2013 | 58 °C | Low |
| 5 | A/South Africa/3626/2013 | 65 °C | High |
| 6 | A/Florida/62/2014 | 60 °C | High |
| 7 | A/Laos/1187/2014 | 60 °C | High |
| 8 | A/New York/61/2015 | 60 °C | High |
| 9 | A/Slovenia/2903/2015 | 56 °C | Low |
| 10 | A/Bangladesh/3002/2015 | 60 °C | High |
| 11 | A/Newcastle/67/2017 | 54 °C | Low |
| 12 | A/South Australia/272/2017 | 58 °C | Low |
| 13 | A/New Jersey/13/2018 | 56 °C | Low |
| 14 | A/Darwin/123/2018 | 58 °C | Low |
| 15 | A/Brisbane/02/2018 | 54 °C | Low |
| 16 | A/lowa/59/2018 | 60 °C | High |
| 17 | A/lowa/12/2019 | 60 °C | High |
| 18 | A/Victoria/2570/2019 | 56 °C | Low |
| 19 | A/Guangdong-Maonan/SWL1536/2019 | 60 °C | High |
| 20 | A/Arkansas/08/2020 | 60 °C | High |
| 21 | A/Indiana/02/2020 | 56 °C | Low |
| Sequence Resource | Gene Segment | Nt Position | Nt Substitution | RNA Sequence | AA Position | AA Substitution |
|---|---|---|---|---|---|---|
| GISAID isolate (ID EPI_ISL_175880) | PB1 | 2060 | A 2060 G | CGG | 687 | Gln-687-Arg |
| PB2 | 305 | A 305 C | ACT | 102 | Asn-102-Thr | |
| 1071 | G 1071 R | RAA 1 | 358 | Glu-358-Glu/Lys | ||
| Virus stock used in this study | PB2 | 1071 | G 1071 R | RAA 1 | 358 | Glu-358-Glu/Lys |
| Virus isolates from mice | PB2 | 1071 | G 1071 R | RAA 1 | 358 | Glu-358-Glu/Lys |
| 154 3 A(H1N1)pdm09 isolates from the GISAID database | PB1 | 2060 | A 2 | CAG | 687 | Gln 2 |
| PB2 | 305 | A 2 | AAT | 102 | Asn 2 | |
| 1071 | G 2 | GAA | 358 | Glu 2 | ||
| 517 H1N1, H3N2, H2N2, H5N1, H5N8, H7N7, H7N9, H9N2 isolates from the GISAID database [34] | PB2 | 1071 | G 2 | GAA | 358 | Glu 2 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al Farroukh, M.; Kiseleva, I.; Bazhenova, E.; Stepanova, E.; Puchkova, L.; Rudenko, L. Understanding the Variability of Certain Biological Properties of H1N1pdm09 Influenza Viruses. Vaccines 2022, 10, 395. https://doi.org/10.3390/vaccines10030395
Al Farroukh M, Kiseleva I, Bazhenova E, Stepanova E, Puchkova L, Rudenko L. Understanding the Variability of Certain Biological Properties of H1N1pdm09 Influenza Viruses. Vaccines. 2022; 10(3):395. https://doi.org/10.3390/vaccines10030395
Chicago/Turabian StyleAl Farroukh, Mohammad, Irina Kiseleva, Ekaterina Bazhenova, Ekaterina Stepanova, Ludmila Puchkova, and Larisa Rudenko. 2022. "Understanding the Variability of Certain Biological Properties of H1N1pdm09 Influenza Viruses" Vaccines 10, no. 3: 395. https://doi.org/10.3390/vaccines10030395
APA StyleAl Farroukh, M., Kiseleva, I., Bazhenova, E., Stepanova, E., Puchkova, L., & Rudenko, L. (2022). Understanding the Variability of Certain Biological Properties of H1N1pdm09 Influenza Viruses. Vaccines, 10(3), 395. https://doi.org/10.3390/vaccines10030395









