Better Late Than Never: Predictors of Delayed COVID-19 Vaccine Uptake in Poland
Abstract
:1. Introduction
2. Methods
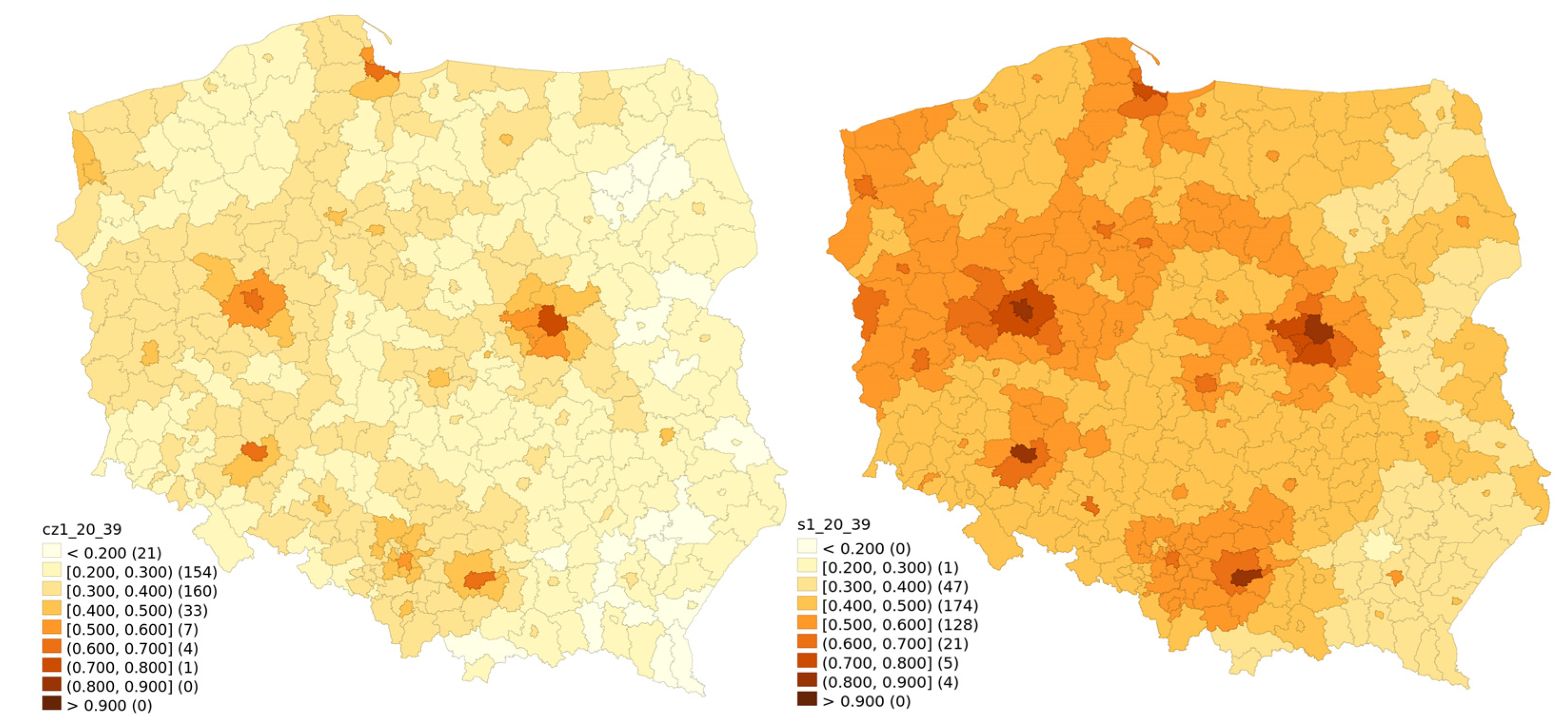
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Raport Szczepień Przeciwko COVID-19—Portal Gov.pl. Available online: https://www.gov.pl/web/szczepimysie/raport-szczepien-przeciwko-covid-19 (accessed on 27 February 2022).
- Walkowiak, M.P.; Walkowiak, J.B.; Walkowiak, D. COVID-19 Passport as a Factor Determining the Success of National Vaccination Campaigns: Does It Work? The Case of Lithuania vs. Poland. Vaccines 2021, 9, 1498. [Google Scholar] [CrossRef] [PubMed]
- Grabowski, J.; Witkowska, N.; Bidzan, L. Letter to the Editor: Excess All-Cause Mortality during Second Wave of COVID-19—The Polish Perspective. Eurosurveillance 2021, 26, 2100117. [Google Scholar] [CrossRef] [PubMed]
- Centrum Badania Opinii Społecznej [Centre for Public Opinion Research]. Polacy o Szczepieniach Przeciw COVID-19 [The Poles on the COVID-19 Vacciantion]. 2021. Available online: https://www.cbos.pl/SPISKOM.POL/2021/K_075_21.PDF (accessed on 27 February 2022).
- Walkowiak, M.P.; Walkowiak, D. Predictors of COVID-19 Vaccination Campaign Success: Lessons Learnt from the Pandemic So Far. A Case Study from Poland. Vaccines 2021, 9, 1153. [Google Scholar] [CrossRef] [PubMed]
- Sowa, P.; Kiszkiel, Ł.; Laskowski, P.P.; Alimowski, M.; Szczerbiński, Ł.; Paniczko, M.; Moniuszko-Malinowska, A.; Kamiński, K. COVID-19 Vaccine Hesitancy in Poland—Multifactorial Impact Trajectories. Vaccines 2021, 9, 876. [Google Scholar] [CrossRef] [PubMed]
- Jarynowski, A.; Wójta-Kempa, M.; Płatek, D.; Czopek, K. Attempt to Understand Public-Health Relevant Social Dimensions of Covid-19 Outbreak in Poland. SSRN 2020, 4, 7–44. [Google Scholar] [CrossRef] [Green Version]
- Harada, T.; Watanabe, T. Changes in Vaccine Hesitancy in Japan across Five Months during the COVID-19 Pandemic and Its Related Factors. Vaccines 2021, 10, 25. [Google Scholar] [CrossRef]
- Le Maréchal, M.; Batel, A.; Bouvier, S.; Mahdhaoui, H.; Margotton, M.; Vittoz, J.-P.; Brudieu, E.; Chevallier, C.; Bedouch, P.; Touati, S.; et al. “When Did You Decide to Receive the Covid-19 Vaccine?” Survey in a High-Volume Vaccination Center. Hum. Vaccines Immunother. 2022, 17, 5099–5104. [Google Scholar] [CrossRef]
- Chaudhuri, K.; Chakrabarti, A.; Chandan, J.S.; Bandyopadhyay, S. COVID-19 Vaccine Hesitancy in the UK: A Longitudinal Household Cross-Sectional Study. BMC Public Health 2022, 22, 104. [Google Scholar] [CrossRef]
- Goodwin, R.; Ben-Ezra, M.; Takahashi, M.; Luu, L.-A.N.; Borsfay, K.; Kovács, M.; Hou, W.K.; Hamama-Raz, Y.; Levin, Y. Psychological Factors Underpinning Vaccine Willingness in Israel, Japan and Hungary. Sci. Rep. 2022, 12, 439. [Google Scholar] [CrossRef]
- Rane, M.S.; Kochhar, S.; Poehlein, E.; You, W.; Robertson, M.K.M.; Zimba, R.; Westmoreland, D.A.; Romo, M.L.; Kulkarni, S.G.; Chang, M.; et al. Determinants and Trends of COVID-19 Vaccine Hesitancy and Vaccine Uptake in a National Cohort of U.S. Adults: A Longitudinal Study. Am. J. Epidemiol. 2022, kwab293. [Google Scholar] [CrossRef]
- Purvis, R.S.; Hallgren, E.; Moore, R.A.; Willis, D.E.; Hall, S.; Gurel-Headley, M.; McElfish, P.A. Trusted Sources of COVID-19 Vaccine Information among Hesitant Adopters in the United States. Vaccines 2021, 9, 1418. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, E.B.; Daoust, J.-F.; Vikse, J.; Nelson, V. “Until I Know It’s Safe for Me”: The Role of Timing in COVID-19 Vaccine Decision-Making and Vaccine Hesitancy. Vaccines 2021, 9, 1417. [Google Scholar] [CrossRef] [PubMed]
- Bajos, N.; Spire, A.; Silberzan, L.; EPICOV study group. The Social Specificities of Hostility toward Vaccination against Covid-19 in France. PLoS ONE 2022, 17, e0262192. [Google Scholar] [CrossRef] [PubMed]
- Yousuf, H.; van der Linden, S.; van Essen, T.; Gommers, D.; Scherder, E.; Narula, J.; Hofstra, L. Dutch Perspectives toward Governmental Trust, Vaccination, Myths, and Knowledge about Vaccines and COVID-19. JAMA Netw. Open 2021, 4, e2140529. [Google Scholar] [CrossRef] [PubMed]
- Reiter, P.L.; Pennell, M.L.; Katz, M.L. Acceptability of a COVID-19 Vaccine among Adults in the United States: How Many People Would Get Vaccinated? Vaccine 2020, 38, 6500–6507. [Google Scholar] [CrossRef] [PubMed]
- Fridman, A.; Gershon, R.; Gneezy, A. COVID-19 and Vaccine Hesitancy: A Longitudinal Study. PLoS ONE 2021, 16, e0250123. [Google Scholar] [CrossRef]
- Kreps, S.; Prasad, S.; Brownstein, J.S.; Hswen, Y.; Garibaldi, B.T.; Zhang, B.; Kriner, D.L. Factors Associated with US Adults’ Likelihood of Accepting COVID-19 Vaccination. JAMA Netw. Open 2020, 3, e2025594. [Google Scholar] [CrossRef]
- Basiw. Available online: https://basiw.mz.gov.pl/index.html#/visualisation?id=3653 (accessed on 27 February 2022).
- GUS—Bank Danych Lokalnych. Available online: https://bdl.stat.gov.pl/BDL/dane/podgrup/temat (accessed on 27 February 2022).
- Zhang, E.J.; Chughtai, A.A.; Heywood, A.; MacIntyre, C.R. Influence of Political and Medical Leaders on Parental Perception of Vaccination: A Cross-Sectional Survey in Australia. BMJ Open 2019, 9, e025866. [Google Scholar] [CrossRef] [Green Version]
- Albrecht, D. Vaccination, Politics and COVID-19 Impacts. BMC Public Health 2022, 22, 96. [Google Scholar] [CrossRef]
- Huynh, H.P.; Zsila, Á.; Martinez-Berman, L. Psychosocial Predictors of Intention to Vaccinate Against the Coronavirus (COVID-19). Behav. Med. 2021, 1–15. [Google Scholar] [CrossRef]
- Walkowiak, M.P.; Walkowiak, D. Underestimation in Reporting Excess COVID-19 Death Data in Poland during the First Three Pandemic Waves. Int. J. Environ. Res. Public Health 2022, 19, 3692. [Google Scholar] [CrossRef] [PubMed]
- Contoli, B.; Possenti, V.; Minardi, V.; Binkin, N.J.; Ramigni, M.; Carrozzi, G.; Masocco, M. What Is the Willingness to Receive Vaccination against COVID-19 among the Elderly in Italy? Data from the PASSI d’Argento Surveillance System. Front. Public Health 2021, 9, 736976. [Google Scholar] [CrossRef] [PubMed]
- Salali, G.D.; Uysal, M.S. Effective Incentives for Increasing COVID-19 Vaccine Uptake. Psychol. Med. 2021, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.; Lai, A.H.Y.; Wang, J.; Asim, S.; Chan, P.S.-F.; Wang, Z.; Yeoh, E.K. Multilevel Determinants of COVID-19 Vaccine Uptake Among South Asian Ethnic Minorities in Hong Kong: Cross-Sectional Web-Based Survey. JMIR Public Health Surveill. 2021, 7, e31707. [Google Scholar] [CrossRef] [PubMed]
- Furman, F.M.; Zgliczyński, W.S.; Jankowski, M.; Baran, T.; Szumowski, Ł.; Pinkas, J. The State of Vaccine Confidence in Poland: A 2019 Nationwide Cross-Sectional Survey. Int. J. Environ. Res. Public Health 2020, 17, 4565. [Google Scholar] [CrossRef]
- Kubicek, P. Martin Åberg and Mikael Sandberg, Social Capital and Democratisation: Roots of Trust in Post-Communist Poland and Ukraine (Aldershot: Ashgate, 2003), Xvi, 332 Pp. + Maps, Figures. Natl. Pap. 2003, 31, 517–518. [Google Scholar] [CrossRef]
- Civil Society and Social Capital in Post-Communist Eastern Europe. Available online: https://www.routledge.com/Civil-Society-and-Social-Capital-in-Post-Communist-Eastern-Europe/Cox/p/book/9781138953666 (accessed on 22 February 2022).
- GUS Jakość Życia i Kapitał Społeczny w Polsce. Wyniki Badania Spójności Społecznej. 2018. Available online: https://stat.gov.pl/obszary-tematyczne/warunki-zycia/dochody-wydatki-i-warunki-zycia-ludnosci/jakosc-zycia-i-kapital-spoleczny-w-polsce-wyniki-badania-spojnosci-spolecznej-2018,4,3.html (accessed on 27 February 2022).
- Domaradzki, J.; Walkowiak, D. Medical Students’ Voluntary Service During the COVID-19 Pandemic in Poland. Front. Public Health 2021, 9, 618608. [Google Scholar] [CrossRef]
- Domaradzki, J.; Walkowiak, D. Does Religion Influence the Motivations of Future Healthcare Professionals to Volunteer during the COVID-19 Pandemic in Poland? An Exploratory Study. J. Relig. Health 2021, 60, 1507–1520. [Google Scholar] [CrossRef]
- Lewenstein, B. Społeczeństwo rodzin czy obywateli—kapitał społeczny Polaków okresu transformacji. In Societas/Communitas; Instytut Stosowanych Nauk Społecznych Uniwersytetu Warszawskiego: Warsaw, Poland, 2006; Volume 1, pp. 163–196. [Google Scholar]
- Centrum Badania Opinii Społecznej [Centre for Public Opinion Research]. O Nieufności i Zaufaniu [On Mistrust and Trust]. 2018. Available online: https://www.cbos.pl/SPISKOM.POL/2018/K_035_18.PDF (accessed on 27 February 2022).
- Centrum Badania Opinii Społecznej [Centre for Public Opinion Research]. Zaufanie Społeczne [Social Trust]. 2020. Available online: https://www.cbos.pl/SPISKOM.POL/2020/K_043_20.PDF (accessed on 27 February 2022).
- Podemski, K. Społeczeństwo obywatelskie w Polsce 25 lat po wielkiej zmianie. Ruch Praw. Ekon. I Socjol. 2014, 76, 89–108. [Google Scholar] [CrossRef] [Green Version]
- Zybała, A. Społeczeństwo obywatelskie i polityka publiczna. Społeczeństwo Ob. 2015, 2, 35–53. [Google Scholar]
- Jasnosz, K. Kształtowanie się społeczeństwa obywatelskiego w Polsce po 1989 roku i jego obecna kondycja. Rocz. Adm. Publicznej 2020, 2020, 177–202. [Google Scholar] [CrossRef]
- Hawe, P.; Shiell, A. Social Capital and Health Promotion: A Review. Soc. Sci. Med. 2000, 51, 871–885. [Google Scholar] [CrossRef]
- Eriksson, M. Social Capital and Health—Implications for Health Promotion. Glob. Health Action 2011, 4, 5611. [Google Scholar] [CrossRef] [PubMed]
- Campbell, C. Social Capital, Social Movements and Global Public Health: Fighting for Health-Enabling Contexts in Marginalised Settings. Soc. Sci. Med. 2020, 257, 112153. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Williams, S.L.; Ronan, K. Combinations of Social Participation and Trust and Association with Health Status—An Australian Perspective. Health Promot. Int. 2014, 29, 608–620. [Google Scholar] [CrossRef] [Green Version]
- Nieminen, T.; Martelin, T.; Koskinen, S.; Aro, H.; Alanen, E.; Hyyppä, M.T. Social Capital as a Determinant of Self-Rated Health and Psychological Well-Being. Int. J. Public Health 2010, 55, 531–542. [Google Scholar] [CrossRef]
- Nieminen, T.; Prättälä, R.; Martelin, T.; Härkänen, T.; Hyyppä, M.T.; Alanen, E.; Koskinen, S. Social Capital, Health Behaviours and Health: A Population-Based Associational Study. BMC Public Health 2013, 13, 613. [Google Scholar] [CrossRef]
- Poortinga, W. Do Health Behaviors Mediate the Association between Social Capital and Health? Prev. Med. 2006, 43, 488–493. [Google Scholar] [CrossRef]
- Rönnerstrand, B. Social Capital and Immunization against the 2009 A(H1N1) Pandemic in the American States. Public Health 2014, 128, 709–715. [Google Scholar] [CrossRef]
- Rönnerstrand, B. Social Capital and Immunisation against the 2009 A(H1N1) Pandemic in Sweden. Scand. J. Public Health 2013, 41, 853–859. [Google Scholar] [CrossRef]
- Chuang, Y.-C.; Huang, Y.-L.; Tseng, K.-C.; Yen, C.-H.; Yang, L. Social Capital and Health-Protective Behavior Intentions in an Influenza Pandemic. PLoS ONE 2015, 10, e0122970. [Google Scholar] [CrossRef] [Green Version]
- Blair, R.A.; Morse, B.S.; Tsai, L.L. Public Health and Public Trust: Survey Evidence from the Ebola Virus Disease Epidemic in Liberia. Soc. Sci. Med. 2017, 172, 89–97. [Google Scholar] [CrossRef] [PubMed]
- Bartscher, A.K.; Seitz, S.; Siegloch, S.; Slotwinski, M.; Wehrhöfer, N. Social Capital and the Spread of Covid-19: Insights from European Countries. J. Health Econ. 2021, 80, 102531. [Google Scholar] [CrossRef] [PubMed]
- Bylok, F. Impact of Social Capital on Health Safety during the SARS-CoV-2 Flu Pandemic. Syst. Saf. Hum. Tech. Facil. Environ. 2021, 3, 304–311. [Google Scholar] [CrossRef]
- Imbulana Arachchi, J.; Managi, S. The Role of Social Capital in COVID-19 Deaths. BMC Public Health 2021, 21, 434. [Google Scholar] [CrossRef]
- Makridis, C.A.; Wu, C. How Social Capital Helps Communities Weather the COVID-19 Pandemic. PLoS ONE 2021, 16, e0245135. [Google Scholar] [CrossRef]
- Borgonovi, F.; Andrieu, E. Bowling Together by Bowling Alone: Social Capital and COVID-19. Soc. Sci. Med. 2020, 265, 113501. [Google Scholar] [CrossRef]
- Ferwana, I.; Varshney, L.R. Social Capital Dimensions Are Differentially Associated with COVID-19 Vaccinations, Masks, and Physical Distancing. PLoS ONE 2021, 16, e0260818. [Google Scholar] [CrossRef]
- James, E.K.; Bokemper, S.E.; Gerber, A.S.; Omer, S.B.; Huber, G.A. Persuasive Messaging to Increase COVID-19 Vaccine Uptake Intentions. Vaccine 2021, 39, 7158–7165. [Google Scholar] [CrossRef]



| Variable | Model without Lag | Model with Time Lag | Model with Spatial Lag |
|---|---|---|---|
| Const | 0.218 (0.0393) *** | 0.241 (0.0290) *** | 0.163 (0.0301) *** |
| Time lag | 0.430 (0.0373) *** | ||
| Spatial lag | 0.547 (0.0494) *** | ||
| Vote for Law and Justice | −0.155 (0.0217) *** | −0.0510 (0.0210) * | −0.0762 (0.0201) *** |
| Vote for Confederation | −1.534 (0.207) *** | −0.964 (0.188) *** | −0.810 (0.185) *** |
| Vote for Kukiz | −0.491 (0.0772) *** | −0.541 (0.066) *** | −0.378 (0.0688) *** |
| Voter turnout | 0.129 (0.0606) * | ||
| COVID−19 only deaths until 2021-06-30 | 0.0146 (0.00504) ** | 0.0119 (0.00457) ** | |
| Higher education | 0.164 (0.0591) ** | −0.152 (0.0542) *** | 0.290 (0.0443) *** |
| Employment rate | 0.473 (0.0637) *** | 0.177 (0.0532) *** | 0.193 (0.0370) *** |
| Adjusted R2 | 56.5% | 67.4% | 66.1% |
| Variable | Model without Lag | Model with Time Lag | Model with Spatial Lag |
|---|---|---|---|
| Const | 0.0734 (0.0490) | 0.0156 (0.0307) | −0.0687 (0.0283) * |
| Time lag | 0.661 (0.0367) *** | ||
| Spatial lag | 0.699 (0.0376) *** | ||
| Vote for Law and Justice | −0.198 (0.0271) *** | −0.0568 (0.0163) *** | |
| Vote for Confederation | −2.096 (0.258) *** | −1.038 (0.212) *** | −0.896 (0.193) *** |
| Vote for Kukiz | −0.295 (0.0964) ** | −0.429 (0.0729) *** | |
| Voter turnout | 0.448 (0.0756) *** | 0.207 (0.0408) *** | |
| COVID-19 only deaths until 2021-06-30 | 0.0228 (0.00629) *** | 0.00962 (0.00485) * | |
| Higher education | −0.222 (0.0738) ** | −0.294 (0.0532) *** | |
| Employment rate | 0.568 (0.0795) *** | 0.334 (0.0619) *** | |
| Adjusted R2 | 57.4% | 71.8% | 75.9% |
| Variable | Model without Lag | Model with Time Lag | Model with Spatial Lag |
|---|---|---|---|
| Const | 0.376 (0.0415) *** | −0.00192 (0.0429) | 0.112 (0.0241) *** |
| Time lag | 0.682 (0.0459) *** | ||
| Spatial lag | 0.568 (0.0505) *** | ||
| Vote for Law and Justice | −0.0728 (0.0267) ** | ||
| Vote for Confederation | −0.750 (0.258) ** | 0.693 (0.203) *** | −0.466 (0.180) *** |
| Vote for Kukiz | −0.299 (0.0948) ** | −0.391 (0.0739) *** | |
| Voter turnout | 0.107 (0.0539) * | ||
| COVID-19 only deaths until 2021-06-30 | |||
| Higher education | −0.772 (0.0625) *** | −0.844 (0.0523) *** | −0.687 (0.0459) *** |
| Employment rate | 0.219 (0.0654) *** | 0.216 (0.0412) *** | |
| Adjusted R2 | 39.2% | 60.5% | 55.0% |
| Variable | Model without Lag | Model with Time Lag | Model With Spatial Lag |
|---|---|---|---|
| Const | 0.796 (0.0949) *** | −1.072 (0.0803) *** | 0.299 (0.0909) *** |
| Time lag | 2.301 (0.0772) *** | ||
| Spatial lag | 0.541 (0.0489) *** | ||
| Vote for Law and Justice | −0.997 (0.0634) *** | −0.239 (0.0449) *** | −0.537 (0.0686) *** |
| Vote for Confederation | −3.483 (0.611) *** | −1.4776 (0.544) ** | |
| Vote for Kukiz | |||
| Voter turnout | 0.958 (0.153) *** | 0.270 (0.0913) *** | 0.475 (0.139) *** |
| COVID-19 only deaths until 2021-06-30 | 0.0581 (0.0159) *** | 0.0327 (0.0141) * | |
| Higher education | −0.499 (0.179) ** | −0.755 (0.0990) *** | 0.407 (0.163) ** |
| Employment rate | |||
| Adjusted R2 | 64.1% | 87.9% | 72.9% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Walkowiak, M.P.; Domaradzki, J.; Walkowiak, D. Better Late Than Never: Predictors of Delayed COVID-19 Vaccine Uptake in Poland. Vaccines 2022, 10, 528. https://doi.org/10.3390/vaccines10040528
Walkowiak MP, Domaradzki J, Walkowiak D. Better Late Than Never: Predictors of Delayed COVID-19 Vaccine Uptake in Poland. Vaccines. 2022; 10(4):528. https://doi.org/10.3390/vaccines10040528
Chicago/Turabian StyleWalkowiak, Marcin Piotr, Jan Domaradzki, and Dariusz Walkowiak. 2022. "Better Late Than Never: Predictors of Delayed COVID-19 Vaccine Uptake in Poland" Vaccines 10, no. 4: 528. https://doi.org/10.3390/vaccines10040528
APA StyleWalkowiak, M. P., Domaradzki, J., & Walkowiak, D. (2022). Better Late Than Never: Predictors of Delayed COVID-19 Vaccine Uptake in Poland. Vaccines, 10(4), 528. https://doi.org/10.3390/vaccines10040528







