Trends in HPV and HPV Vaccine Awareness among Gay and Bisexual Males in the U.S
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Source and Study Population
2.2. Outcome Variables
2.3. Independent Variables
2.4. Statistical Analysis
3. Results
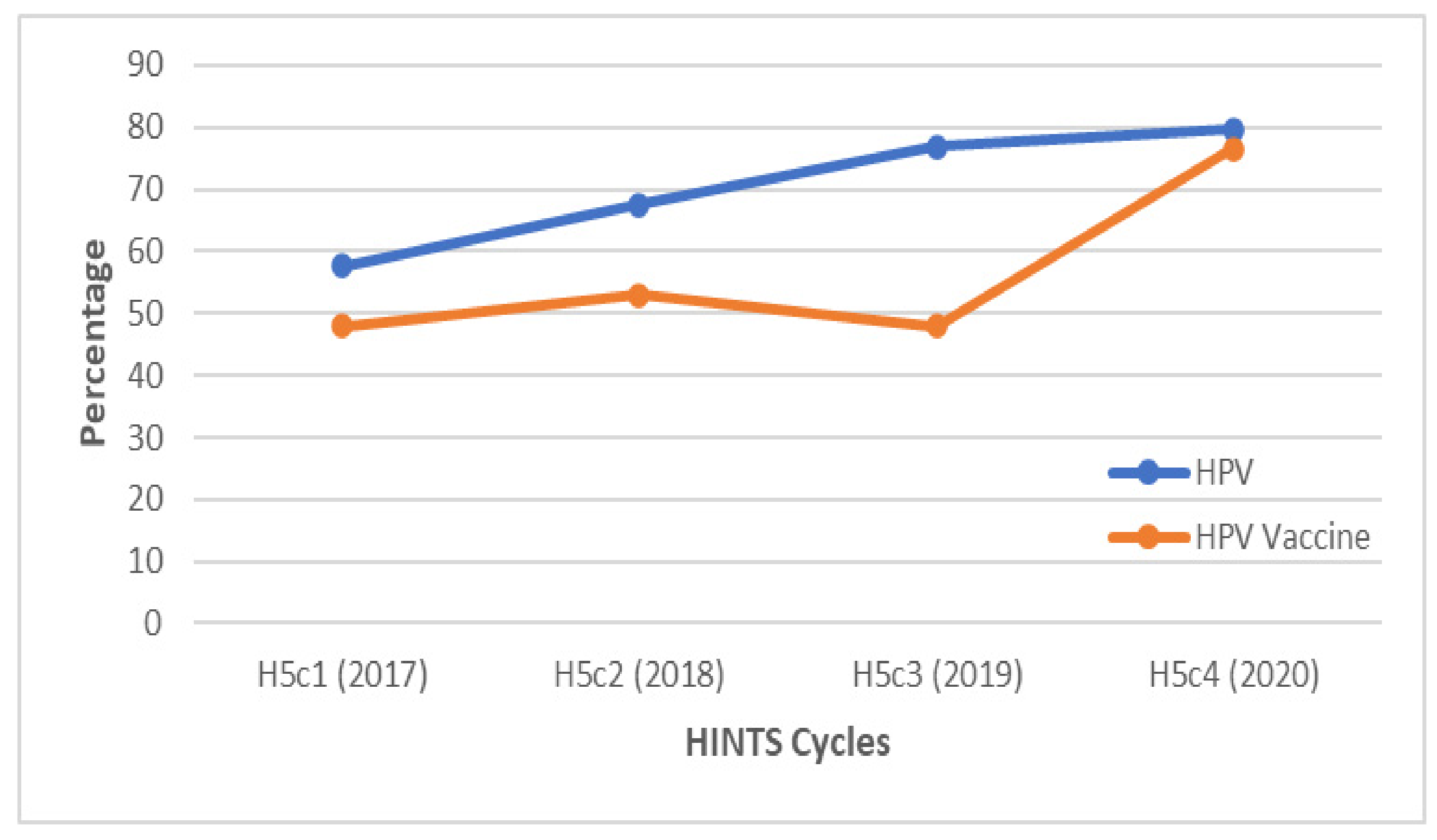
3.1. Trends in HPV Awareness
3.2. Trends in HPV Vaccine Awareness
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Centers for Disease Control and Prevention HPV Fact Sheet. Available online: https://www.cdc.gov/std/hpv/stdfact-hpv.htm (accessed on 1 February 2022).
- McQuillan, G.; Kruszon-Moran, D.; Markowitz, L.E.; Unger, E.R.; Paulose-Ram, R. Prevalence of HPV in Adults Aged 18–69: United States, 2011–2014. NCHS Data Br. 2017, 280. Available online: https://www.cdc.gov/nchs/products/databriefs/db280.htm (accessed on 1 February 2022).
- Saraiya, M.; Unger, E.R.; Thompson, T.D.; Lynch, C.F.; Hernandez, B.Y.; Lyu, C.W.; Steinau, M.; Watson, M.; Wilkinson, E.J.; Hopenhayn, C.; et al. US Assessment of HPV Types in Cancers: Implications for Current and 9-Valent HPV Vaccines. J. Natl. Cancer Inst. 2015, 107, djv086. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Food and Drug Administration News Release: FDA Approves Expanded Use of Gardasil 9 to Include Individuals 27 through 45 Years Old. Available online: https://www.fda.gov/news-events/press-announcements/fda-approves-expanded-use-gardasil-9-include-individuals-27-through-45-years-old (accessed on 1 February 2022).
- Centers for Disease Control and Prevention Gay and Bisexual Men’s Health. Available online: https://www.cdc.gov/msmhealth/STD.htm (accessed on 1 February 2022).
- Reiter, P.L.; McRee, A.; Katz, M.L.; Paskett, E.D. Human Papillomavirus Vaccination Among Young Adult Gay and Bisexual Men in the United States. Am. J. Public Health 2015, 105, 96–102. [Google Scholar] [CrossRef] [PubMed]
- Jemal, A.; Simard, E.P.; Dorell, C.; Noone, A.; Markowitz, L.E.; Kohler, B.; Eheman, C.; Saraiya, M.; Bandi, P.; Saslow, D.; et al. Annual report to the nation on the status of cancer, 1975–2009, featuring the burden and trends in human papillomavirus (HPV)-associated cancers and HPV vaccination coverage levels. J. Natl. Cancer Inst. 2013, 105, 175–201. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meites, E.; Winer, R.L.; Newcomb, M.E.; Gorbach, P.M.; Querec, T.D.; Rudd, J.; Collins, T.; Lin, J.; Moore, J.; Remble, T.; et al. Vaccine Effectiveness Against Prevalent Anal and Oral Human Papillomavirus Infection Among Men Who Have Sex with Men-United States, 2016–2018. J. Infect. Dis. 2020, 222, 2052–2060. [Google Scholar] [CrossRef]
- Nyitray, A.G.; Carvalho da Silva, R.J.; Baggio, M.L.; Lu, B.; Smith, D.; Abrahamsen, M.; Papenfuss, M.; Villa, L.L.; Lazcano-Ponce, E.; Giuliano, A.R. Age-specific prevalence of and risk factors for anal human papillomavirus (HPV) among men who have sex with women and men who have sex with men: The HPV in men (HIM) study. J. Infect. Dis. 2011, 203, 49–57. [Google Scholar] [CrossRef] [Green Version]
- Marra, E.; Lin, C.; Clifford, G.M. Type-specific anal human papillomavirus prevalence among men, according to sexual preference and HIV status: A systematic literature review and meta-analysis. J. Infect. Dis. 2019, 219, 590–598. [Google Scholar] [CrossRef] [Green Version]
- Cranston, R.D.; Carballo-Diéguez, A.; Gundacker, H.; Richardson, B.A.; Giguere, R.; Dolezal, C.; Siegel, A.; KunjaraNaAyudhya, R.P.; Gomez, K.; Piper, J.M.; et al. Prevalence and determinants of anal human papillomavirus infection in men who have sex with men and transgender women. Int. J. STD AIDS 2019, 30, 154–162. [Google Scholar] [CrossRef]
- Bosch, F.X.; Broker, T.R.; Forman, D.; Moscicki, A.; Gillison, M.L.; Doorbar, J.; Stern, P.L.; Stanley, M.; Arbyn, M.; Poljak, M.; et al. Comprehensive control of human papillomavirus infections and related diseases. Vaccine 2013, 31 (Suppl. 7), H1–H31. [Google Scholar] [CrossRef] [Green Version]
- Gorbach, P.M.; Cook, R.; Gratzer, B.; Collins, T.; Parrish, A.; Moore, J.; Kerndt, P.R.; Crosby, R.A.; Markowitz, L.E.; Meites, E. Human Papillomavirus Vaccination Among Young Men Who Have Sex With Men and Transgender Women in 2 US Cities, 2012–2014. Sex. Transm. Dis. 2017, 44, 436–441. [Google Scholar] [CrossRef]
- Chido-Amajuoyi, O.G.; Jackson, I.; Yu, R.; Shete, S. Declining awareness of HPV and HPV vaccine within the general US population. Hum. Vaccines Immunother. 2021, 17, 420–427. [Google Scholar] [CrossRef]
- Hoss, A.; Meyerson, B.E.; Zimet, G.D. State statutes and regulations related to human papillomavirus vaccination. Hum. Vaccines Immunother. 2019, 15, 1519–1526. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Keim-Malpass, J.; Mitchell, E.M.; DeGuzman, P.B.; Stoler, M.H.; Kennedy, C. Legislative activity related to the human papillomavirus (HPV) vaccine in the United States (2006–2015): A need for evidence-based policy. Risk Manag. Healthc. Policy 2017, 10, 29–32. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- President’s Cancer Panel Annual Report 2012-2013-Accelerating H Vaccine Uptake: Urgency for Action to Prevent Cancer. Available online: https://deainfo.nci.nih.gov/advisory/pcp/annualreports/hpv/ (accessed on 4 February 2022).
- Domgue, J.F.; Yu, R.K.; Shete, S. Trends in the rates of health-care providers’ recommendation for HPV vaccine from 2012 to 2018: A multi-round cross-sectional analysis of the health information national trends survey. Hum. Vaccines Immunother. 2021, 17, 3081–3089. [Google Scholar] [CrossRef] [PubMed]
- Heese, B.W.; Moser, R.P.; Finney Rutten, L.J.; Kreps, G.L. The health information national trends survey: Research from the baseline. J. Health Commun. 2006, 11 (Suppl. 1), vii–xvi. [Google Scholar] [CrossRef]
- Health Information National Trends Survey 5 (HINTS 5) Cycle 4 Methodology Report December 2020. Available online: https://hints.cancer.gov/docs/methodologyreports/HINTS5_Cycle4_MethodologyReport.pdf (accessed on 1 February 2022).
- Freedman Ellis, G.; Lumley, T.; Żółtak, T.; Schneider, B.; Krivitsky, P.N. ‘dplyr’-Like Syntax for Summary Statistics of Survey Data. R Package 2021, Version 1.1.0. Available online: https://cran.r-project.org/web/packages/srvyr/srvyr.pdf (accessed on 1 February 2022).
- Cooper, D.L.; Hernandez, N.D.; Rollins, L.; Akintobi, T.H.; McAllister, C. HPV vaccine awareness and the association of trust in cancer information from physicians among males. Vaccine 2017, 35, 2661–2667. [Google Scholar] [CrossRef] [Green Version]
- Newman, P.A.; Logie, C.H.; Doukas, N.; Asakura, K. HPV vaccine acceptability among men: A systematic review and meta-analysis. Sex. Transm. Infect. 2013, 89, 568–574. [Google Scholar] [CrossRef] [Green Version]
- Gerend, M.A.; Madkins, K.; Phillips, G., 2nd; Mustanski, B. Predictors of Human Papillomavirus Vaccination Among Young Men Who Have Sex With Men. Sex. Transm. Dis. 2016, 43, 185–191. [Google Scholar] [CrossRef]
- Americans are Visiting the Doctor Less Frequently, Census Bureau Reports. Available online: https://www.census.gov/newsroom/releases/archives/health_care_insurance/cb12-185.html (accessed on 4 February 2022).
- Meites, E.; Krishna, N.K.; Markowitz, L.E.; Oster, A.M. Health care use and opportunities for human papillomavirus vaccination among young men who have sex with men. Sex. Transm. Dis. 2013, 40, 154–157. [Google Scholar] [CrossRef] [Green Version]
- Gilkey, M.B.; Moss, J.L.; Coyne-Beasley, T.; Hall, M.E.; Shah, P.D.; Brewer, N.T. Physician communication about adolescent vaccination: How is human papillomavirus vaccine different? Prev. Med. 2015, 77, 181–185. [Google Scholar] [CrossRef] [Green Version]
- Preston, S.M.; Darrow, W.W. Are Men Being Left Behind (Or Catching Up)? Differences in HPV Awareness, Knowledge, and Attitudes Between Diverse College Men and Women. Am. J. Men’s Health 2019, 13, 1557988319883776. [Google Scholar] [CrossRef]
- Cooper, D.L.; Zellner-Lawrence, T.; Mubasher, M.; Banerjee, A.; Hernandez, N.D. Examining HPV Awareness, Sexual Behavior, and Intent to Receive the HPV Vaccine Among Racial/Ethnic Male College Students 18-27 years. Am. J. Men’s Health 2018, 12, 1966–1975. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barnard, M.; George, P.; Perryman, M.L.; Wolff, L.A. Human papillomavirus (HPV) vaccine knowledge, attitudes, and uptake in college students: Implications from the Precaution Adoption Process Model. PLoS ONE 2017, 12, e0182266. [Google Scholar]
- Fisher, W.A.; Kohut, T.; Salisbury, C.M.A.; Salvadori, M.I. Understanding human papillomavirus vaccination intentions: Comparative utility of the theory of reasoned action and the theory of planned behavior in vaccine target age women and men. J. Sex. Med. 2013, 10, 2455–2464. [Google Scholar] [CrossRef] [PubMed]
- Petroll, A.E.; Mosack, K.E. Physician awareness of sexual orientation and preventive health recommendations to men who have sex with men. Sex. Transm. Dis. 2011, 38, 63–67. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chan, A.; Brown, B.; Sepulveda, E.; Teran-Clayton, L. Evaluation of fotonovela to increase human papillomavirus vaccine knowledge, attitudes, and intentions in a low-income Hispanic community. BMC Res. Notes 2015, 8, 615. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blake, K.D.; Ottenbacher, A.J.; Finney Rutten, L.J.; Grady, M.A.; Kobrin, S.C.; Jacobson, R.M.; Hesse, B.W. Predictors of human papillomavirus awareness and knowledge in 2013: Gaps and opportunities for targeted communication strategies. Am. J. Prev. Med. 2015, 48, 402–410. [Google Scholar] [CrossRef] [Green Version]





| 2017 N = 61 | 2018 N = 60 | 2019 N = 100 | 2020 N = 67 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | (95% CI) | % | (95% CI) | % | (95% CI) | % | (95% CI) | |||||
| Overall | 57.6 | 53.3 | 61.8 | 67.6 | 61.9 | 73.4 | 76.8 | 74.8 | 78.9 | 79.7 | 77.2 | 82.1 |
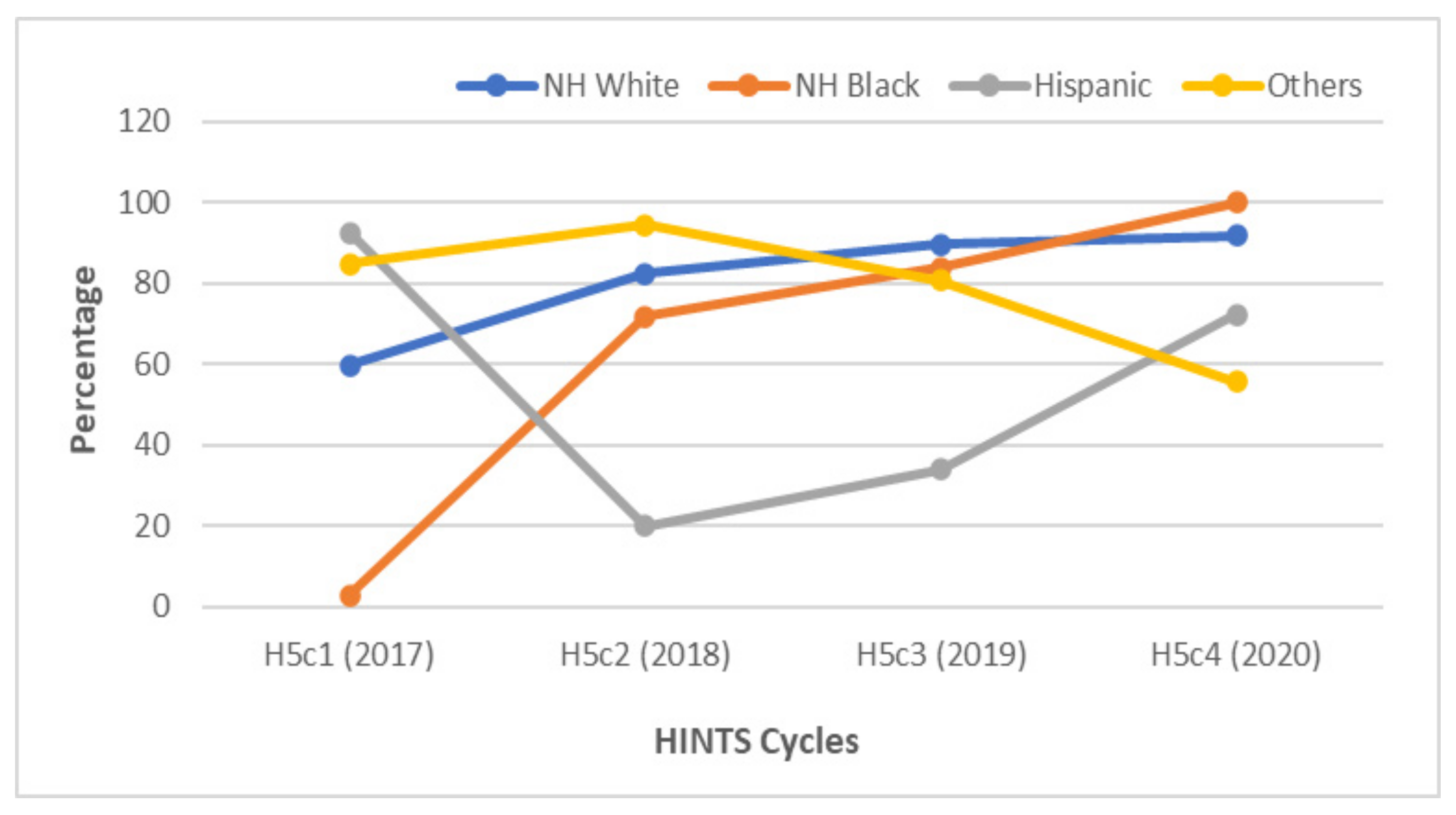
| Race/Ethnicity | ||||||||||||
| NH White | 59.7 | 55.3 | 64.1 | 82.4 | 77.4 | 87.5 | 89.6 | 88.6 | 90.7 | 91.7 | 89.9 | 93.5 |
| NH Black | 2.73 | 0 | 41.9 | 71.8 | 64.1 | 79.5 | 83.9 | 80.8 | 87.1 | 100 | 100 | 100 |
| Hispanic | 92.4 | 88.7 | 96.2 | 19.9 | 1.69 | 38.1 | 34.0 | 26.0 | 41.9 | 72.2 | 61.6 | 82.8 |
| Others | 84.7 | 76.7 | 92.6 | 94.5 | 78.3 | 100 | 80.7 | 79.1 | 82.4 | 55.5 | 41.9 | 69.0 |
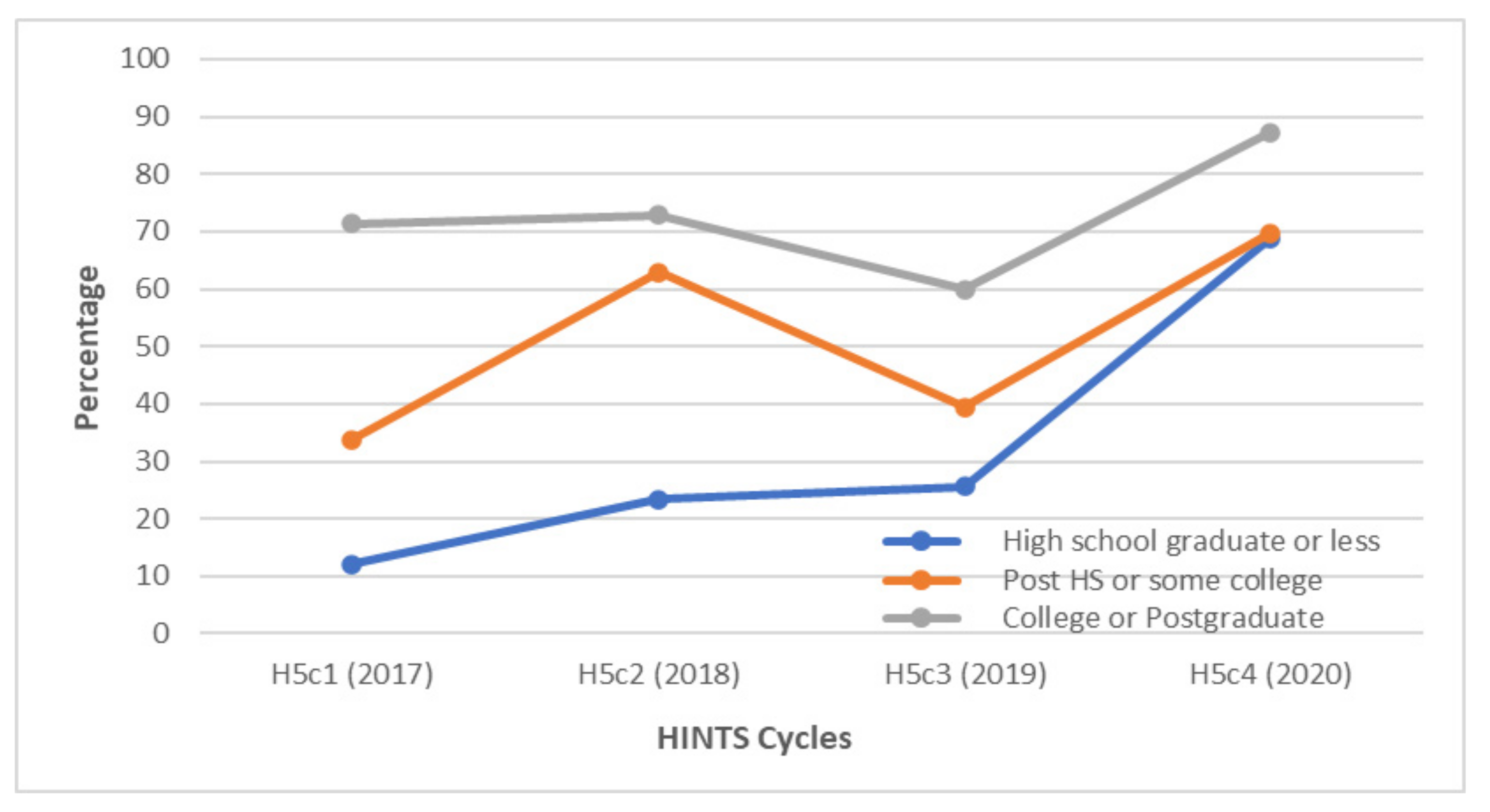
| Education | ||||||||||||
| H. school grad or less | 12.1 | 1.96 | 22.3 | 26.8 | 17.2 | 36.4 | 81.7 | 79.5 | 83.8 | 89.8 | 81.8 | 97.8 |
| Post HS or some college | 46.6 | 39.3 | 54.0 | 88.8 | 84.3 | 93.2 | 67.2 | 61.9 | 72.6 | 66.9 | 61.5 | 72.3 |
| College or postgraduate | 83.1 | 80.2 | 86.0 | 86.2 | 84.1 | 88.3 | 84.0 | 83.0 | 85.1 | 90.9 | 89.0 | 92.8 |
| Household Income | ||||||||||||
| Less than $35,000 | 33.4 | 24.4 | 42.5 | 52.9 | 46.9 | 58.9 | 52.7 | 49.8 | 55.6 | 77.9 | 72.8 | 83.1 |
| $35,000 to <$50,000 | 26.2 | 13.0 | 39.4 | 46.7 | 27.3 | 66.1 | 94.1 | 93.3 | 94.9 | 41.4 | 34.4 | 48.4 |
| $50,000 to <$75,000 | 77.5 | 68.3 | 86.6 | 97.2 | 95.1 | 99.3 | 98.6 | 98.4 | 98.9 | 96.3 | 93.7 | 99.0 |
| $75,000 or more | 78.1 | 73.0 | 83.3 | 69.1 | 59.6 | 78.7 | 72.9 | 68.9 | 76.8 | 97.4 | 96.2 | 98.5 |
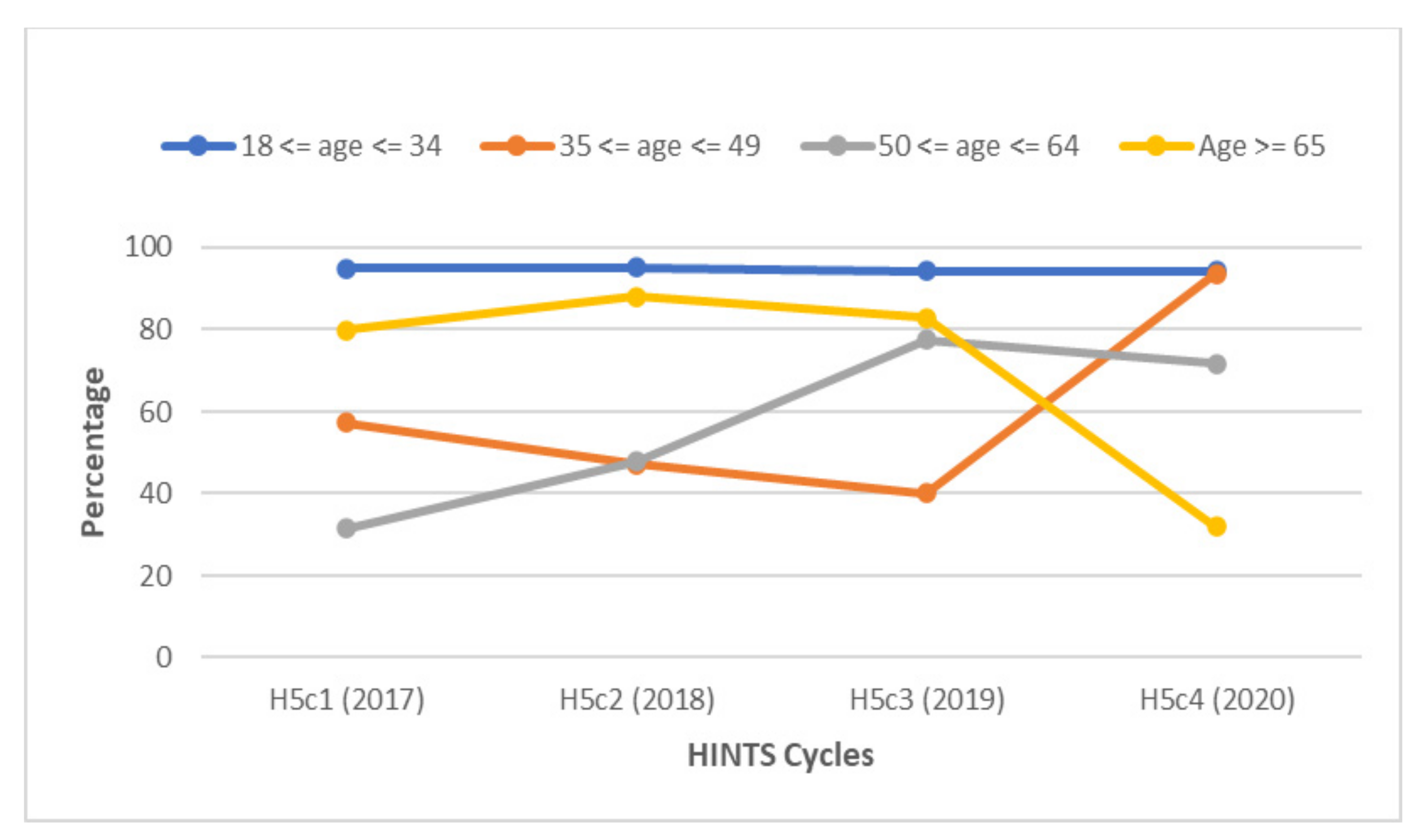
| Age | ||||||||||||
| 18 ≤ age ≤ 34 | 95.0 | 92.8 | 97.3 | 95.1 | 92.5 | 97.8 | 94.2 | 93.9 | 94.5 | 94.2 | 92.4 | 95.9 |
| 35 ≤ age ≤ 49 | 57.3 | 49.9 | 64.6 | 47.2 | 27.8 | 66.6 | 40.1 | 30.1 | 50.1 | 93.7 | 90.6 | 96.9 |
| 50 ≤ age ≤ 64 | 31.4 | 25.1 | 37.7 | 47.9 | 40.2 | 55.6 | 77.4 | 75.5 | 79.3 | 71.8 | 65.1 | 78.5 |
| Age ≥ 65 | 79.9 | 75.2 | 84.7 | 88.0 | 84.1 | 91.9 | 82.9 | 79.9 | 85.9 | 32.2 | 26.3 | 38.2 |
| 2017 | 2018 | 2019 | 2020 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | (95% CI) | % | (95% CI) | % | (95% CI) | % | (95% CI) | |||||
| Overall | 48.0 | 44.4 | 51.6 | 53.0 | 46.9 | 59.2 | 47.9 | 46.5 | 49.3 | 76.6 | 73.8 | 79.5 |
| Race/Ethnicity | ||||||||||||
| NH White | 50.9 | 46.5 | 55.2 | 71.8 | 65.1 | 78.4 | 58.1 | 56.9 | 59.3 | 87.6 | 85.2 | 89.9 |
| NH Black | 2.73 | 0 | 41.9 | 31.1 | 20.2 | 42.0 | 80.6 | 78.8 | 82.4 | 100 | 100 | 100 |
| Hispanic | 49.7 | 37.9 | 61.4 | 10.2 | 0.818 | 19.6 | 18.9 | 14.5 | 23.3 | 72.2 | 61.6 | 82.8 |
| Others | 84.1 | 76.0 | 92.2 | 94.5 | 78.3 | 100 | 36.4 | 32.7 | 40.2 | 53.6 | 40.0 | 67.2 |
| Education | ||||||||||||
| High school graduate or less | 12.1 | 1.96 | 22.3 | 23.4 | 11.2 | 35.6 | 25.6 | 23.3 | 27.9 | 68.8 | 45.2 | 92.3 |
| Post HS or some college | 33.8 | 27.4 | 40.2 | 62.9 | 50.3 | 75.5 | 39.4 | 35.9 | 43.0 | 69.8 | 64.6 | 74.9 |
| College or Postgraduate | 71.4 | 67.0 | 75.7 | 72.9 | 68.4 | 77.5 | 59.9 | 58.6 | 61.2 | 87.3 | 85.1 | 89.5 |
| Household Income | ||||||||||||
| Less than $35,000 | 24.0 | 17.0 | 31.1 | 24.1 | 19.6 | 28.7 | 33.3 | 31.3 | 35.2 | 72.2 | 66.1 | 78.3 |
| $35,000 to <$50,000 | 26.2 | 13.0 | 39.4 | 46.7 | 27.3 | 66.1 | 18.6 | 15.7 | 21.4 | 42.6 | 35.5 | 49.7 |
| $50,000 to <$75,000 | 67.6 | 57.3 | 77.8 | 92.8 | 87.6 | 97.9 | 63.0 | 60.8 | 65.2 | 100 | 100 | 100 |
| $75,000 or more | 66.5 | 61.0 | 72.0 | 57.0 | 47.9 | 66.2 | 57.2 | 53.9 | 60.4 | 92.9 | 91.1 | 94.6 |
| Age | ||||||||||||
| 18 ≤ age ≤ 34 | 79.2 | 73.8 | 84.7 | 91.3 | 87.3 | 95.2 | 62.9 | 61.0 | 64.7 | 94.2 | 92.4 | 95.9 |
| 35 ≤ age ≤ 49 | 39.8 | 33.3 | 46.3 | 30.0 | 16.6 | 43.4 | 13.1 | 9.64 | 16.5 | 86.5 | 81.0 | 92.1 |
| 50 ≤ age ≤ 64 | 28.6 | 22.7 | 34.4 | 34.2 | 28.7 | 39.8 | 60.6 | 58.5 | 62.6 | 68.7 | 61.8 | 75.5 |
| Age ≥ 65 | 70.8 | 63.4 | 78.2 | 41.0 | 33.7 | 48.2 | 32.1 | 29.0 | 35.1 | 28.2 | 22.8 | 33.6 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chidobem, I.; Tian, F.; Ogbuokiri, E.; Mgbodile, F.; Mgbodile, C.; Jokar, T.O.; Shah, M.A.; Pierre-Louis, F. Trends in HPV and HPV Vaccine Awareness among Gay and Bisexual Males in the U.S. Vaccines 2022, 10, 604. https://doi.org/10.3390/vaccines10040604
Chidobem I, Tian F, Ogbuokiri E, Mgbodile F, Mgbodile C, Jokar TO, Shah MA, Pierre-Louis F. Trends in HPV and HPV Vaccine Awareness among Gay and Bisexual Males in the U.S. Vaccines. 2022; 10(4):604. https://doi.org/10.3390/vaccines10040604
Chicago/Turabian StyleChidobem, Ikechukwu, Fan Tian, Esther Ogbuokiri, Francis Mgbodile, Chisom Mgbodile, Tahereh Orouji Jokar, Muhammad Ahsan Shah, and Frantz Pierre-Louis. 2022. "Trends in HPV and HPV Vaccine Awareness among Gay and Bisexual Males in the U.S" Vaccines 10, no. 4: 604. https://doi.org/10.3390/vaccines10040604







