Assessment of Seroconversion after SARS-CoV-2 Vaccination in Patients with Lung Cancer
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Study End Points
2.3. Laboratory Analysis
2.4. Statistical Analysis
3. Results
3.1. Patient Characteristics
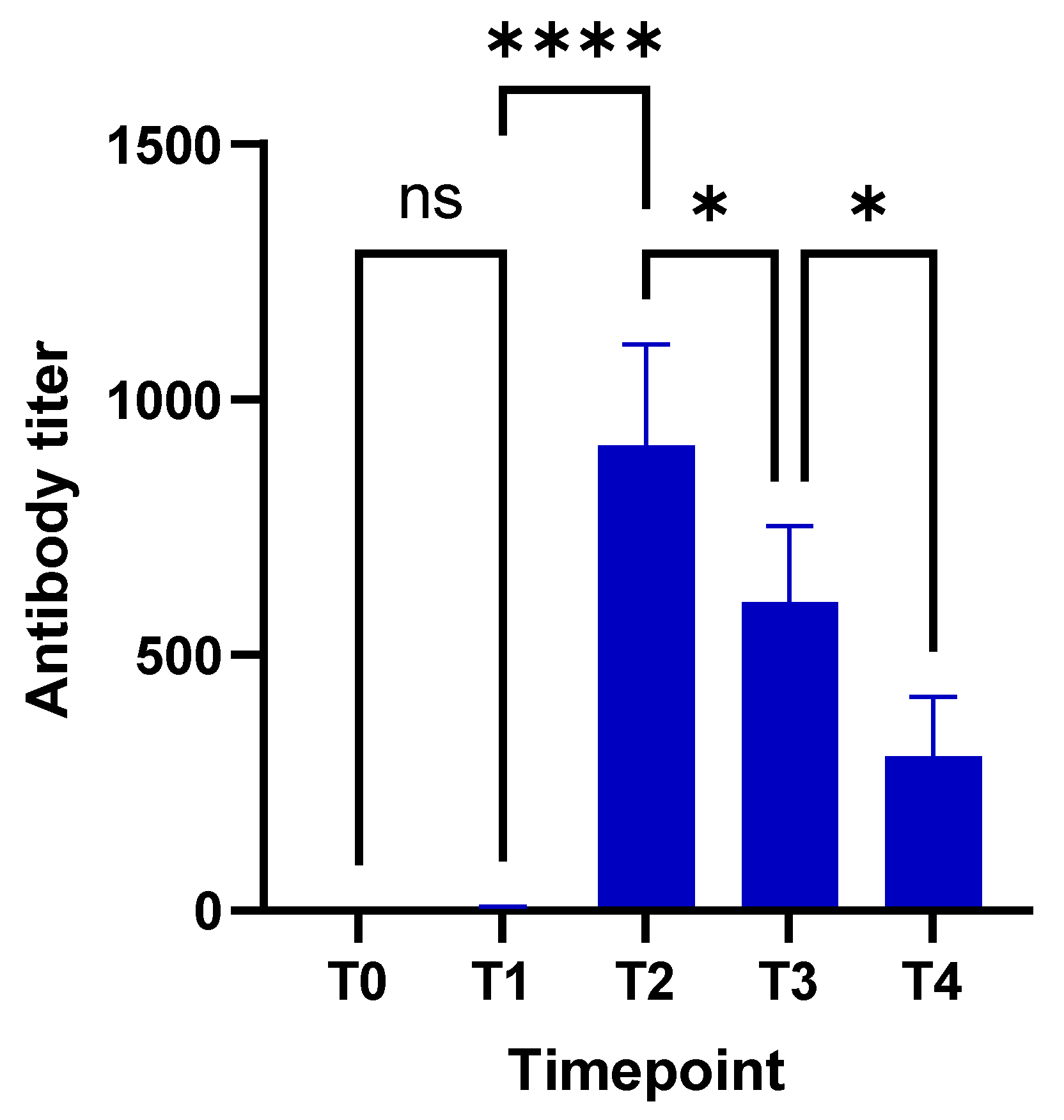
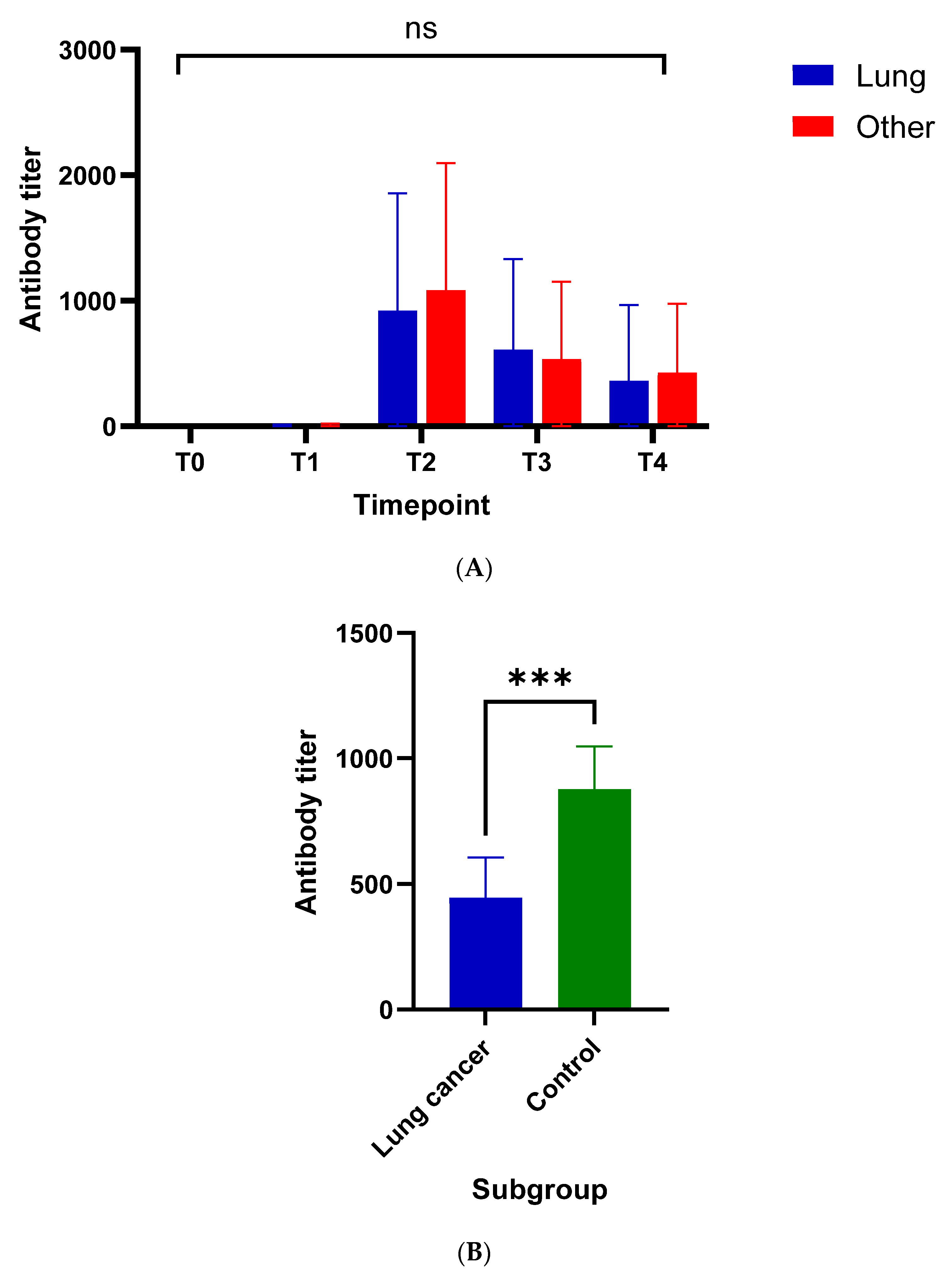
3.2. Evaluation of Humoral Response
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Characteristics | Group A (N [%]) | Group B (N [%]) | Group C (N [%]) |
|---|---|---|---|
| Total | 125 | 35 | 86 |
| Gender | |||
| Males | 96 (76.8) | 16 (45.7) | 24 (27.9) |
| Females | 29 (23.2) | 19 (54.3) | 62 (72.1) |
| Age * | 68 (46–91) | 59 (37–85) | 50 (21–90) |
| BMI * | 26.1 (15.6–49.9) | ||
| Smoking status | |||
| Active | 20 (16.0) | 5 (14.3) | 25 (29.1) |
| Former | 100 (80.0) | 24 (68.6) | 19 (22.1) |
| Never | 5 (4.0) | 6 (17.1) | 42 (48.8) |
| Comorbidities *,+ | 1 (0–4) | 0 (0–3) | 0 (0–2) |
| Vaccine | |||
| BNT162b2 | 100 (80.0) | 23 (65.7) | 78 (90.7) |
| mRNA-1273 | 10 (8.0) | 7 (20.0) | 3 (3.5) |
| AZD1222 | 15 (12.0) | 5 (14.3) | 5 (5.8) |
| Histologic subtype | |||
| NSCLC | 104 (83.2) | ||
| SCLC | 21 (16.8) | ||
| Previous lines of systemic therapy * | 0 (0–5) | ||
| Treatment regimen | |||
| Immunotherapy | 60 (48.0) | ||
| Chemotherapy | 34 (27.2) | ||
| Combination | 29 (23.2) | ||
| Targeted therapy | 2 (1.6) | ||
| Radiotherapy | 40 (32.0) | ||
| Immunomodulatory agents | 27 (26.1) | ||
| Disease progression | 27 (21.6) | ||
| Time Points (Weeks) | Number of Patients Sampled (%) | Number of Patients That Received the BNT162b2 Vaccine (%) | Mean/Median IU/mL (Interquartile Range) |
|---|---|---|---|
| T0 (baseline) | 28 (22.4) | 21 (87.5) | 0.4/0.4 (0) |
| T1 (two to three) | 41 (32.8) | 37 (90.2) | 5.0/0.4 (3.3) |
| T2 (six ± one) | 41 (32.8) | 29 (70.7) | 910.7/527.0 (1641.5) |
| T3 (12 ± three) | 93 (74.4) | 69 (74.2) | 603.7/323.0 (563.3) |
| T4 (24 ± three) | 73 (58.4) | 55 (75.3) | 301.9/141.0 (312.5) |

References
- Yesudhas, D.; Srivastava, A.; Gromiha, M.M. COVID-19 outbreak: History, mechanism, transmission, structural studies and therapeutics. Infection 2021, 49, 199–213. [Google Scholar] [CrossRef] [PubMed]
- Word Health Organization. Who Director-General’s Opening Remarks at the Media Briefing on COVID-19—11 March 2020. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 5 January 2022).
- Li, J.; Huang, D.Q.; Zou, B.; Yang, H.; Hui, W.Z.; Rui, F.; Yee, N.T.S.; Liu, C.; Nerurkar, S.N.; Kai, J.C.Y.; et al. Epidemiology of COVID-19: A systematic review and meta-analysis of clinical characteristics, risk factors, and outcomes. J. Med. Virol. 2021, 93, 1449–1458. [Google Scholar] [CrossRef] [PubMed]
- Desai, A.; Gupta, R.; Advani, S.; Ouellette, L.; Kuderer, N.M.; Lyman, G.H.; Li, A. Mortality in hospitalized patients with cancer and coronavirus disease 2019: A systematic review and meta-analysis of cohort studies. Cancer 2021, 127, 1459–1468. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Chai, P.; Yu, J.; Fan, X. Effects of cancer on patients with COVID-19: A systematic review and meta-analysis of 63,019 participants. Cancer Biol. Med. 2021, 18, 298–307. [Google Scholar] [CrossRef]
- Zarifkar, P.; Kamath, A.; Robinson, C.; Morgulchik, N.; Shah, S.F.H.; Cheng, T.K.M.; Dominic, C.; Fehintola, A.O.; Bhalla, G.; Ahillan, T.; et al. Clinical Characteristics and Outcomes in Patients with COVID-19 and Cancer: A Systematic Review and Meta-analysis. Clin. Oncol. 2021, 33, e180–e191. [Google Scholar] [CrossRef]
- Zhang, H.; Han, H.; He, T.; Labbe, K.E.; Hernandez, A.V.; Chen, H.; Velcheti, V.; Stebbing, J.; Wong, K.K. Clinical Characteristics and Outcomes of COVID-19-Infected Cancer Patients: A Systematic Review and Meta-Analysis. J. Natl. Cancer Inst. 2021, 113, 371–380. [Google Scholar] [CrossRef]
- Lei, H.; Yang, Y.; Zhou, W.; Zhang, M.; Shen, Y.; Tao, D.; Wang, L.; Lei, Q.; Wang, Y.; Wu, Y. Higher mortality in lung cancer patients with COVID-19? A systematic review and meta-analysis. Lung Cancer 2021, 157, 60–65. [Google Scholar] [CrossRef]
- Peravali, M.; Joshi, I.; Ahn, J.; Kim, C. A Systematic Review and Meta-Analysis of Clinical Characteristics and Outcomes in Patients With Lung Cancer with Coronavirus Disease 2019. JTO Clin. Res. Rep. 2021, 2, 100141. [Google Scholar] [CrossRef]
- Tagliamento, M.; Agostinetto, E.; Bruzzone, M.; Ceppi, M.; Saini, K.S.; de Azambuja, E.; Punie, K.; Westphalen, C.B.; Morgan, G.; Pronzato, P.; et al. Mortality in adult patients with solid or hematological malignancies and SARS-CoV-2 infection with a specific focus on lung and breast cancers: A systematic review and meta-analysis. Crit. Rev. Oncol. Hematol. 2021, 163, 103365. [Google Scholar] [CrossRef]
- Thakkar, A.; Gonzalez-Lugo, J.D.; Goradia, N.; Gali, R.; Shapiro, L.C.; Pradhan, K.; Rahman, S.; Kim, S.Y.; Ko, B.; Sica, R.A.; et al. Seroconversion rates following COVID-19 vaccination among patients with cancer. Cancer Cell 2021, 39, 1081–1090.e2. [Google Scholar] [CrossRef]
- Marra, A.; Generali, D.; Zagami, P.; Cervoni, V.; Gandini, S.; Venturini, S.; Morganti, S.; Passerini, R.; Orecchia, R.; Curigliano, G. Seroconversion in patients with cancer and oncology health care workers infected by SARS-CoV-2. Ann. Oncol. 2021, 32, 113–119. [Google Scholar] [CrossRef] [PubMed]
- Thakkar, A.; Pradhan, K.; Jindal, S.; Cui, Z.; Rockwell, B.; Shah, A.P.; Packer, S.; Sica, R.A.; Sparano, J.; Goldstein, D.Y.; et al. Patterns of seroconversion for SARS-CoV2-IgG in patients with malignant disease and association with anticancer therapy. Nat. Cancer 2021, 2, 392–399. [Google Scholar] [CrossRef] [PubMed]
- Cavanna, L.; Citterio, C.; Biasini, C.; Madaro, S.; Bacchetta, N.; Lis, A.; Cremona, G.; Muroni, M.; Bernuzzi, P.; Lo Cascio, G.; et al. COVID-19 vaccines in adult cancer patients with solid tumours undergoing active treatment: Seropositivity and safety. A prospective observational study in Italy. Eur. J. Cancer 2021, 157, 441–449. [Google Scholar] [CrossRef] [PubMed]
- Tran, S.; Truong, T.H.; Narendran, A. Evaluation of COVID-19 vaccine response in patients with cancer: An interim analysis. Eur. J. Cancer 2021, 159, 259–274. [Google Scholar] [CrossRef] [PubMed]
- Corti, C.; Antonarelli, G.; Scotte, F.; Spano, J.P.; Barriere, J.; Michot, J.M.; Andre, F.; Curigliano, G. Seroconversion rate after vaccination against COVID-19 in patients with cancer-a systematic review. Ann. Oncol. 2022, 33, 158–168. [Google Scholar] [CrossRef] [PubMed]
- Guven, D.C.; Sahin, T.K.; Kilickap, S.; Uckun, F.M. Antibody Responses to COVID-19 Vaccination in Cancer: A Systematic Review. Front. Oncol. 2021, 11, 759108. [Google Scholar] [CrossRef]
- Gounant, V.; Ferre, V.M.; Soussi, G.; Charpentier, C.; Flament, H.; Fidouh, N.; Collin, G.; Namour, C.; Assoun, S.; Bizot, A.; et al. Efficacy of Severe Acute Respiratory Syndrome Coronavirus-2 Vaccine in Patients With Thoracic Cancer: A Prospective Study Supporting a Third Dose in Patients with Minimal Serologic Response After Two Vaccine Doses. J. Thorac. Oncol. 2021, 17, 239–251. [Google Scholar] [CrossRef]
- Sakuraba, A.; Luna, A.; Micic, D. Serologic response following SARS-COV2 vaccination in patients with cancer: A systematic review and meta-analysis. J. Hematol. Oncol. 2022, 15, 15. [Google Scholar] [CrossRef]
- Giuliano, A.R.; Lancet, J.E.; Pilon-Thomas, S.; Dong, N.; Jain, A.G.; Tan, E.; Ball, S.; Tworoger, S.S.; Siegel, E.M.; Whiting, J.; et al. Evaluation of Antibody Response to SARS-CoV-2 mRNA-1273 Vaccination in Patients with Cancer in Florida. JAMA Oncol. 2022, e220001. [Google Scholar] [CrossRef]
- Callender, L.A.; Curran, M.; Bates, S.M.; Mairesse, M.; Weigandt, J.; Betts, C.J. The Impact of Pre-existing Comorbidities and Therapeutic Interventions on COVID-19. Front. Immunol. 2020, 11, 1991. [Google Scholar] [CrossRef]
- Levin, E.G.; Lustig, Y.; Cohen, C.; Fluss, R.; Indenbaum, V.; Amit, S.; Doolman, R.; Asraf, K.; Mendelson, E.; Ziv, A.; et al. Waning Immune Humoral Response to BNT162b2 Covid-19 Vaccine over 6 Months. N. Engl. J. Med. 2021, 385, e84. [Google Scholar] [CrossRef] [PubMed]
- Bianchi, F.P.; Stefanizzi, P.; Germinario, C.A.; Migliore, G.; Vimercati, L.; Martinelli, A.; Lobifaro, A.; Diella, G.; Larocca, A.M.V.; Control Room Working, G.; et al. Medium-to-Long-Term Immunogenicity of BNT162b2 mRNA COVID-19 Vaccine: A Retrospective Cohort Study. Vaccines 2022, 10, 417. [Google Scholar] [CrossRef] [PubMed]
- Nomura, Y.; Sawahata, M.; Nakamura, Y.; Kurihara, M.; Koike, R.; Katsube, O.; Hagiwara, K.; Niho, S.; Masuda, N.; Tanaka, T.; et al. Age and Smoking Predict Antibody Titres at 3 Months after the Second Dose of the BNT162b2 COVID-19 Vaccine. Vaccines 2021, 9, 1042. [Google Scholar] [CrossRef] [PubMed]
- CDC. Interim Guidelines for COVID-19 Antibody Testing. Available online: https://www.cdc.gov/coronavirus/2019-ncov/lab/resources/antibody-tests-guidelines.html (accessed on 10 January 2022).
- FDA. Coronavirus (COVID-19) Update: FDA Authorizes Adaptive Biotechnologies T-Detect COVID Test. March 2021. Available online: https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-authorizes-adaptive-biotechnologies-t-detect-covid-test (accessed on 11 January 2022).
- Gomez, J.E. Analysis of Lung Cancer Patients Receiving SARS-CoV-2 Vaccines Revealed a Minority Subset with Poor Antibody Responses Relative to Controls. In Proceedings of the IASLC 2021 World Conference on Lung Cancer, Denver, CO, USA, 8–14 September 2021. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Trontzas, I.P.; Vathiotis, I.; Economidou, C.; Petridou, I.; Gomatou, G.; Grammoustianou, M.; Tsamis, I.; Syrigos, N.; Anagnostakis, M.; Fyta, E.; et al. Assessment of Seroconversion after SARS-CoV-2 Vaccination in Patients with Lung Cancer. Vaccines 2022, 10, 618. https://doi.org/10.3390/vaccines10040618
Trontzas IP, Vathiotis I, Economidou C, Petridou I, Gomatou G, Grammoustianou M, Tsamis I, Syrigos N, Anagnostakis M, Fyta E, et al. Assessment of Seroconversion after SARS-CoV-2 Vaccination in Patients with Lung Cancer. Vaccines. 2022; 10(4):618. https://doi.org/10.3390/vaccines10040618
Chicago/Turabian StyleTrontzas, Ioannis P., Ioannis Vathiotis, Christina Economidou, Ioulia Petridou, Georgia Gomatou, Maria Grammoustianou, Ioannis Tsamis, Nikolaos Syrigos, Maximilian Anagnostakis, Eleni Fyta, and et al. 2022. "Assessment of Seroconversion after SARS-CoV-2 Vaccination in Patients with Lung Cancer" Vaccines 10, no. 4: 618. https://doi.org/10.3390/vaccines10040618
APA StyleTrontzas, I. P., Vathiotis, I., Economidou, C., Petridou, I., Gomatou, G., Grammoustianou, M., Tsamis, I., Syrigos, N., Anagnostakis, M., Fyta, E., Sakka, V., Poulakou, G., Kotteas, E. A., & Syrigou, E. (2022). Assessment of Seroconversion after SARS-CoV-2 Vaccination in Patients with Lung Cancer. Vaccines, 10(4), 618. https://doi.org/10.3390/vaccines10040618








