How Were Healthcare Workers after Anti-SARS-CoV-2 Vaccination? A Study of the Emotional Side Effects of Vaccination
Abstract
:1. Introduction
1.1. The Personal and Environmental Factors Considered
1.2. The Present Study
2. Methods
2.1. Participants
2.2. Procedure
2.3. Materials
2.3.1. Sociodemographic Characteristics
2.3.2. Your Experience with Anti-SARS-CoV-2 Vaccine
2.3.3. Personality Trait Measurements
2.3.4. Plan of Analysis
3. Results
3.1. Descriptive Statistics
3.2. Regression Models: Variables for Emotions
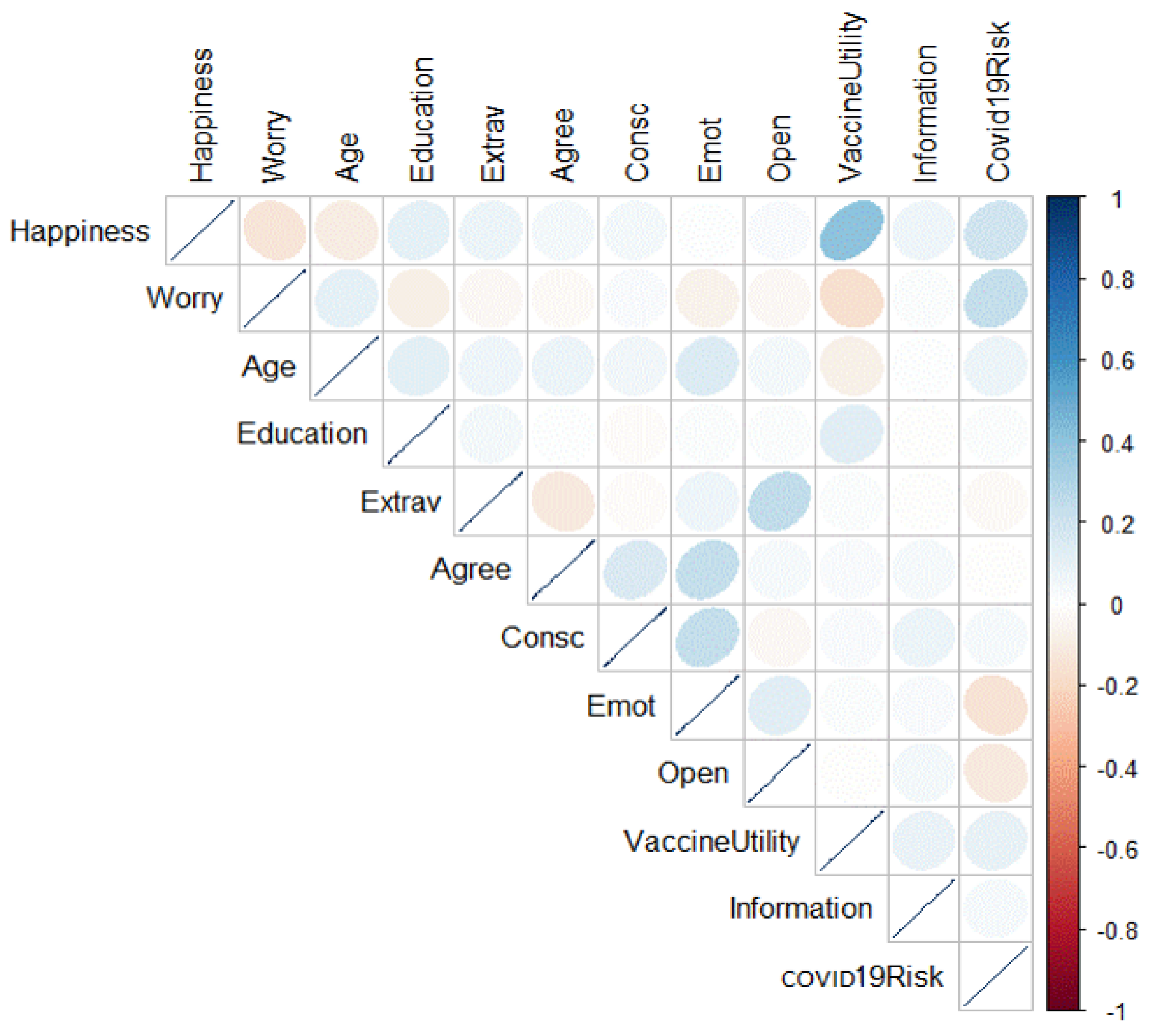
3.3. Associations between Variables
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Appendix A
| Qualification | N | % |
|---|---|---|
| Medical doctors | 3211 | 55.5 |
| Dentists | 111 | 1.9 |
| Nurses | 1549 | 26.8 |
| Other healthcare figures | 491 | 8.5 |
| Operator social health (OSS) | 70 | 1.2 |
| Pharmacists | 43 | 0.7 |
| First aid workers | 34 | 0.6 |
| Medicine students | 71 | 1.2 |
| Nurses students | 32 | 0.6 |
| Administratives | 42 | 0.7 |
| Others | 132 | 2.3 |
| Modalities | N | % |
|---|---|---|
| Social networking | 2427 | 41.9 |
| Scientific literature | 2035 | 35.1 |
| Personal experience | 4397 | 75.9 |
| Sharing risks and benefit | 2429 | 42 |
| Not promoting | 513 | 8.9 |
| M (SD) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age | 1.80 (0.76) | |||||||||||
| 2. Education | 5.09 (0.93) | 0.11 ** | ||||||||||
| 3. Extraversion | 4.16 (1.39) | 0.06 ** | 0.04 ** | |||||||||
| 4. Agreeableness | 5.43 (1.02) | 0.07 ** | 0.008 | −0.118 ** | ||||||||
| 5.Conscientiousness | 5.55 (1.07) | 0.05 ** | −0.017 | −0.012 | 0.158 ** | |||||||
| 6. Emotional stability | 4.68 (1.32) | 0.14 ** | 0.013 | 0.063 ** | 0.231 ** | 0.231 ** | ||||||
| 7. Openness | 4.50 (1.02) | 0.04 ** | 0.016 | 0.249 ** | 0.032 * | −0.032 | 0.123 ** | |||||
| 8. Vaccine utility | 6.71 (0.73) | −0.07 ** | 0.129 ** | 0.11 | 0.027 | 0.029 | 0.017 | −0.005 | ||||
| 9. Covid-19 risk | 4.43 (1.75) | 0.07 ** | 0.019 | −0.021 | −0.002 | 0.036 ** | −0.143 ** | −0.118 ** | 0.98 ** | |||
| 10. Information | 5.28 (1.30) | 0.13 ** | 0.038 ** | 0.051 ** | 0.040 ** | 0.101 ** | −095 ** | 0.085 ** | 0.137 ** | 0.160 ** | ||
| 11. Happiness | 6.04 (1.44) | −0.09 ** | 0.107 ** | 0.077 ** | 0.047 ** | 0.040 ** | 0.004 | 0.025 | 0.403 ** | 0.193 ** | 0.177 ** | |
| 12. Worry | 2.74 (1.90) | 0.100 ** | −0.082 ** | −0.038 ** | −0.024 | 0.029 * | −0.067 ** | −0.039 ** | −0.161 ** | 0.238 ** | 0.014 | −0.140 ** |
References
- Wu, J.T.; Leung, K.; Leung, G.M. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: A modelling study. Lancet 2020, 26, 506–510, Erratum in 2020, 26, 1149–1150. [Google Scholar] [CrossRef] [Green Version]
- Hui, D.S.; Azhar, E.I.; Madani, T.A.; Ntoumi, F.; Kock, R.; Dar, O.; Ippolito, G.; McHugh, T.D.; Memish, Z.A.; Drosten, C.; et al. The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health—The latest 2019 novel coronavirus outbreak in Wuhan, China. Int. J. Infect. Dis. IJID Off. Publ. Int. Soc. Infect. Dis. 2020, 91, 264–266. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Murphy, J.; Vallières, F.; Bentall, R.P.; Shevlin, M.; McBride, O.; Hartman, T.K.; McKay, R.; Bennett, K.; Mason, L.; Gibson-Miller, J.; et al. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat. Commun. 2021, 12, 29. [Google Scholar] [CrossRef] [PubMed]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [Green Version]
- Spinelli, M.; Lionetti, F.; Pastore, M.; Fasolo, M. Parents’ stress and children’s psychological problems in families facing the COVID-19 outbreak in Italy. Front. Psychol. 2020, 11, 1713. [Google Scholar] [CrossRef]
- Wang, J.; Jing, R.; Lai, X.; Zhang, H.; Lyu, Y.; Knoll, M.D.; Fang, H. Acceptance of COVID-19 Vaccination during the COVID-19 Pandemic in China. Vaccines 2020, 8, 482. [Google Scholar] [CrossRef]
- National Institute of Health—National Institute of Allergy and Infectious Disease. Safety and Immunogenicity Study of 2019-nCoV Vaccine (mRNA- 1273) for Prophylaxis of SARS-CoV-2 Infection (COVID-19). Available online: https://clinicaltrials.gov/ct2/show/NCT04283461 (accessed on 20 March 2020).
- World Health Organization. DRAFT Landscape of COVID-19 Candidate Vaccines. Available online: https://www.who.int/blueprint/priority-diseases/key-action/novel-coronavirus-landscape-ncov.pdf (accessed on 20 April 2020).
- Pfizer and Biontech Announce Vaccine Candidate against COVID-19 Achieved Success in First Interim Analysis from Phase 3 Study. Available online: https://www.pfizer.com/news/press-release/press-release-detail/pfizer-and-biontech-announce-vaccine-candidate-against (accessed on 9 November 2020).
- European Centre for Disease Prevention and Control. Available online: https://www.ecdc.europa.eu/en/about-ecdc (accessed on 5 January 2021).
- Ministero Della Salute. 2020. Available online: https://www.salute.gov.it/portale/home.html (accessed on 20 November 2020).
- Malik, A.A.; McFadden, S.M.; Elharake, J.; Omer, S.B. Determinants of COVID-19 vaccine acceptance in the US. eClinicalMedicine 2020, 26, 100495. [Google Scholar] [CrossRef]
- MacDonald, N.E.; Eskola, J.; Liang, X.; Chaudhuri, M.; Dube, E.; Gellin, B.; Goldstein, S.; Larson, H.; Manzo, M.L.; Reingold, A.; et al. Vaccine Hesitancy: Definition, Scope and Determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef]
- Karafillakis, E.; Larson, H.J. The benefit of the doubt or doubts over benefits? A systematic literature review of perceived risks of vaccines in European populations. Vaccine 2017, 35, 4840–4850. [Google Scholar] [CrossRef]
- Muñoz, D.C.; Llamas, L.M.; Bosch-Capblanch, X. Exposing concerns about vaccination in low-and middle-income countries: A systematic review. Int. J. Public Health 2015, 60, 767–780. [Google Scholar] [CrossRef] [Green Version]
- Mascherini, M.; Nivakoski, S. Social media use and vaccine hesitancy in the European Union. Vaccine 2022, 40, 2215–2225. [Google Scholar] [CrossRef] [PubMed]
- European Parliament. European Parliament Resolution of 19 April 2018 on Vaccine Hesitancy and Drop in Vaccination Rates in Europe (2017/2951 RSP). Available online: https://www.europarl.europa.eu/doceo/document/TA-8-2018-0188_EN.pdf (accessed on 20 January 2021).
- World Health Organization. Ten Threats to Global Health in 2019. Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 20 November 2020).
- Arat, A.; Burström, B.; Östberg, V.; Hjern, A. Social inequities in vaccination coverage among infants and pre-school children in Europe and Australia—A systematic review. BMC Public Health 2019, 19, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Yang, L.; Jin, H.; Lin, L. Vaccination against COVID-19: A systematic review and meta-analysis of acceptability and its predictors. Prev. Med. 2021, 150, 106694. [Google Scholar] [CrossRef]
- Lazarus, J.V.; Ratzan, S.C.; Palayew, A.; Gostin, L.O.; Larson, H.J.; Rabin, K.; Kimball, S.; El-Mohandes, A. A global survey of potential acceptance of a COVID-19 vaccine. Nat. Med. 2021, 27, 225–228. [Google Scholar] [CrossRef] [PubMed]
- Bertoncello, C.; Ferro, A.; Fonzo, M.; Zanovello, S.; Napoletano, G.; Russo, F.; Baldo, V.; Cocchio, S. Socioeconomic Determinants in Vaccine Hesitancy and Vaccine Refusal in Italy. Vaccines 2020, 8, 276. [Google Scholar] [CrossRef] [PubMed]
- Volpp, K.G.; Loewenstein, G.; Buttenheim, A.M. Behaviorally informed strategies for a national COVID-19 vaccine promotion program. JAMA 2021, 325, 125–126. [Google Scholar] [CrossRef]
- McCrae, R.R.; Costa, P.T., Jr. Adding Liebe und Arbeit: The full five-factor model and well-being. Personal. Soc. Psychol. Bull. 1991, 17, 227–232. [Google Scholar] [CrossRef]
- Tellegen, A. Structures of mood and personality and their relevance to assessing anxiety, with an emphasis on self-report. In Anxiety and the Anxiety Disorders; Tuma, A.H., Mason, J., Eds.; Erlbaum: Hillsdale, NJ, USA, 1985; pp. 681–706. [Google Scholar]
- Lucas, R.E.; Diener, E.; Grob, A.; Suh, E.M.; Shao, L. Cross-cultural evidence for the fundamental features of extraversion. J. Personal. Soc. Psychol. 2000, 79, 452. [Google Scholar] [CrossRef]
- Vaidya, J.G.; Gray, E.K.; Haig, J.; Watson, D. On the temporal stability of personality: Evidence for differential stability and the role of life experiences. J. Personal. Soc. Psychol. 2002, 83, 1469. [Google Scholar] [CrossRef]
- Dong, Y.; Dai, T.; Wei, Y.; Zhang, L.; Zheng, M.; Zhou, F. A systematic review of SARS-CoV-2 vaccine candidates. Signal Transduct. Target. Ther. 2020, 5, 1–14. [Google Scholar] [CrossRef]
- Center Disease Control and Prevention. 2021. Available online: https://www.cdc.gov/ (accessed on 20 January 2021).
- Ledford, H. COVID vaccines and blood clots: Five key questions. Nature 2021, 592, 495–496. [Google Scholar] [CrossRef] [PubMed]
- Brewer, N.T.; Chapman, G.B.; Rothman, A.J.; Leask, J.; Kempe, A. Understanding and increasing vaccination behaviors: Putting psychology into action. Psychol. Sci. Public Interest 2018, 18, 149–207. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Casiday, R.; Cresswell, T.; Wilson, D.; Panter-Brick, C. A survey of UK parental attitudes to the MMR vaccine and trust in medical authority. Vaccine 2006, 24, 177–184. [Google Scholar] [CrossRef] [PubMed]
- Gore, P.; Madhavan, S.; Curry, D.; McClung, G.; Castiglia, M.; Rosenbluth, S.A.; Smego, R.A. Predictors of childhood immunization completion in a rural population. Soc. Sci. Med. 1999, 48, 1011–1027. [Google Scholar] [CrossRef]
- Taylor, J.A.; Darden, P.M.; Brooks, D.A.; Hendricks, J.W.; Wasserman, R.C.; Bocian, A.B. Association between parents’ preferences and perceptions of barriers to vaccination and the immunization status of their children: A study from Pediatric Research in Office Settings and the National Medical Association. Pediatrics 2002, 110, 1110–1116. [Google Scholar] [CrossRef]
- Gilkey, M.B.; McRee, A.L.; Magnus, B.E.; Reiter, P.L.; Dempsey, A.F.; Brewer, N.T. Vaccination confidence and parental refusal/delay of early childhood vaccines. PloS ONE 2016, 11, e0159087. [Google Scholar] [CrossRef] [Green Version]
- Karlsson, L.C.; Lewandowsky, S.; Antfolk, J.; Salo, P.; Lindfelt, M.; Oksanen, T.; Kivimäki, M.; Soveri, A. The association between vaccination confidence, vaccination behavior, and willingness to recommend vaccines among Finnish healthcare workers. PLoS ONE 2019, 14, e0224330. [Google Scholar] [CrossRef]
- KFF COVID-19 Vaccine Monitor: December 2020. Kaiser Family Foundation. 2020. Available online: https://www.kff.org/coronavirus-covid-19/report/kff-covid-19-vaccine-monitor-december-2020/ (accessed on 29 December 2020).
- Caserotti, M.; Girardi, P.; Rubaltelli, E.; Tasso, A.; Lotto, L.; Gavaruzzi, T. Associations of COVID-19 risk perception with vaccine hesitancy over time for Italian residents. Soc. Sci. Med. 2021, 272, 113688. [Google Scholar] [CrossRef]
- Lu, W.; Wang, H.; Lin, Y.; Li, L. Psychological status of medical workforce during the COVID-19 pandemic: A cross-sectional study. Psychiatry Res. 2020, 288, 112936. [Google Scholar] [CrossRef]
- Ran, L.; Chen, X.; Wang, Y.; Wu, W.; Zhang, L.; Tan, X. Risk factors of healthcare workers with coronavirus disease 2019: A retrospective cohort study in a designated hospital of Wuhan in China. Clin. Infect. Dis. 2020, 71, 2218–2221. [Google Scholar] [CrossRef] [Green Version]
- Larson, H.J.; Jarrett, C.; Eckersberger, E.; Smith, D.M.D.; Paterson, P. Understanding Vaccine Hesitancy around Vaccines and Vaccination from a Global Perspective: A Systematic Review of Published Literature, 2007–2012. Vaccine 2014, 32, 2150–2159. [Google Scholar] [CrossRef] [PubMed]
- Lane, S.; MacDonald, N.E.; Marti, M.; Dumolard, L. Vaccine hesitancy around the globe: Analysis of three years of WHO/UNICEF Joint Reporting Form data-2015–2017. Vaccine 2018, 36, 3861–3867. [Google Scholar] [CrossRef] [PubMed]
- Cornwall, W. Officials gird for a war on vaccine misinformation. Science 2020, 369, 14–15. [Google Scholar] [CrossRef] [PubMed]
- Enserink, M.; Cohen, J. Fact-Checking Judy Mikovits, the Controversial Virologist Attacking Anthony Fauci in a Viral Conspiracy Video. SciencInsider, 8 May 2020. Available online: https://www.science.org/content/article/fact-checking-judy-mikovits-controversial-virologist-attacking-anthony-fauci-viral (accessed on 8 May 2020).
- Fadda, M.; Albanese, E.; Suggs, L.S. When a COVID-19 vaccine is ready, will we all be ready for it? Int. J. Public Health 2020, 65, 711–712. [Google Scholar] [CrossRef] [PubMed]
- Bozzola, E.; Spina, G.; Russo, R.; Bozzola, M.; Corsello, G.; Villani, A. Mandatory vaccinations in European countries, undocumented information, false news and the impact on vaccination uptake: The position of the Italian pediatric society. Ital. J. Pediatrics 2018, 44, 1–4. [Google Scholar] [CrossRef]
- Goodman, J.L.; Grabenstein, J.D.; Braun, M.M. Answering Key Questions About COVID-19 Vaccines. JAMA 2020, 324, 2027–2028. [Google Scholar] [CrossRef]
- Dubé, E.; MacDonald, N.E. COVID-19 vaccine hesitancy. Nat. Rev. Nephrol. 2022, 2022, 18. [Google Scholar]
- Wentzell, E.; Racila, A.M. The social experience of participation in a COVID-19 vaccine trial: Subjects’ motivations, others’ concerns, and insights for vaccine promotion. Vaccine 2021, 39, 2445–2451. [Google Scholar] [CrossRef]
- Head, K.J.; Biederman, E.; Sturm, L.A.; Zimet, G.D. A retrospective and prospective look at strategies to increase adolescent HPV vaccine uptake in the United States. Hum. Vaccines Immunother. 2018, 14, 1626–1635. [Google Scholar] [CrossRef] [Green Version]
- Mohammed, K.; Vivian, E.; Loux, T.; Arnold, L.D. Factors Associated With Parents’ Intent to Vaccinate Adolescents for Human Papillomavirus: Findings From the 2014 National Immunization Survey–Teen. Prev. Chronic Dis. 2017, 14, E45. [Google Scholar] [CrossRef] [Green Version]
- Sturm, L.; Donahue, K.; Kasting, M.; Kulkarni, A.; Brewer, N.T.; Zimet, G.D. Pediatrician-Parent Conversations About Human Papillomavirus Vaccination: An Analysis of Audio Recordings. J. Adolesc. Health 2017, 61, 246–251. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Verger, P.; Scronias, D.; Dauby, N.; Adedzi, K.A.; Gobert, C.; Bergeat, M.; Gagneur, A.; Dubé, E. Attitudes of healthcare workers towards COVID-19 vaccination: A survey in France and French-speaking parts of Belgium and Canada, 2020. Eurosurveillance 2021, 26, 2002047. [Google Scholar] [CrossRef]
- Napolitano, F.; D’Alessandro, A.; Angelillo, I.F. Investigating Italian parent’ vaccine hesitancy: A cross-sectional survey. Hum. Vaccines Immunother. 2018, 14, 1558–1565. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Danchin, M.H.; Costa-Pinto, J.; Attwell, K.; Willaby, H.; Wiley, K.; Hoq, M.; Leask, J.; Perrett, K.P.; O’Keefe, J.; Giles, M.L.; et al. Vaccine decision-making begins in pregnancy: Correlation between vaccine concerns, intentions and maternal vaccination with subsequent childhood vaccine uptake. Vaccine 2018, 36, 6473–6479. [Google Scholar] [CrossRef] [PubMed]
- Dubé, E.; Gagnon, D.; Ouakki, M.; Bettinger, J.; Witteman, H.; MacDonald, S.; Fisher, W.; Saini, V.; Greyson, D. Measuring vaccine acceptance among Canadian parents: A survey of the Canadian Immunization Research Network. Vaccine 2018, 36, 545–552. [Google Scholar] [CrossRef]
- Eller, N.M.; Henrikson, N.B.; Opel, D.J. Vaccine Information Sources and Parental Trust in Their Child’s Health Care Provider. Health Educ. Behav. 2019, 46, 445–453. [Google Scholar] [CrossRef]
- Omer, S.B.; Benjamin, R.M.; Brewer, N.T.; Buttenheim, A.M.; Callaghan, T.; Caplan, A.; Carpiano, R.M.; Clinton, C.; DiResta, R.; Elharake, J.A.; et al. Promoting COVID-19 vaccine acceptance: Recommendations from the Lancet Commission on Vaccine Refusal, Acceptance, and Demand in the USA. Lancet 2021, 398, 2186–2192. [Google Scholar] [CrossRef]
- Smith, L.E.; Amlôt, R.; Weinman, J.A.; Yiend, J.; Rubin, G.J. A systematic review of factors affecting vaccine uptake in young children. Vaccine 2017, 35, 6059–6069. [Google Scholar] [CrossRef] [Green Version]
- Bianco, A.; Pileggi, C.; Iozzo, F.; Nobile, C.G.A.; Pavia, M. Vaccination against Human Papilloma Virus infection in male adolescents: Knowledge, attitudes, and acceptability among parents in Italy. Hum. Vaccines Immunother. 2014, 10, 2536–2542. [Google Scholar] [CrossRef] [Green Version]
- Napolitano, F.; Napolitano, P.; Angelillo, I.F. Seasonal influenza vaccination in pregnant women: Knowledge, attitudes, and behaviors in Italy. BMC Infect. Dis. 2017, 17, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Giusti, E.M.; Pedroli, E.; D’Aniello, G.E.; Badiale, C.S.; Pietrabissa, G.; Manna, C.; Badiale, M.S.; Riva, G.; Castelnuovo, G.; Molinari, E. The Psychological Impact of the COVID-19 Outbreak on Health Professionals: A Cross-Sectional Study. Front. Psychol. 2020, 11, 1684. [Google Scholar] [CrossRef] [PubMed]
- Rose, S.; Hartnett, J.; Pillai, S. Healthcare worker’s emotions, perceived stressors and coping mechanisms during the COVID-19 pandemic. PLoS ONE 2021, 16, e0254252. [Google Scholar]
- Rapisarda, V.; Vella, F.; Ledda, C.; Barattucci, M.; Ramaci, T. What Prompts Doctors to Recommend COVID-19 Vaccines: Is It a Question of Positive Emotion? Vaccines 2021, 9, 578. [Google Scholar] [CrossRef] [PubMed]
- Ledda, C.; Rapisarda, V.; Maltezou, H.C.; Contrino, E.; Conforto, A.; Maida, C.M.; Tramuto, F.; Vitale, F.; Costantino, C. Coverage rates against vaccine-preventable diseases among healthcare workers in Sicily (Italy). Eur. J. Public Health 2020, 31, 56. [Google Scholar] [CrossRef] [PubMed]
- Istat. 2020. Available online: https://www.istat.it/it/censimenti/popolazione-e-abitazioni (accessed on 15 January 2021).
- Qualtrics. Provo, Utah, USA. Available online: https://www.qualtrics.com (accessed on 15 January 2021).
- Uchida, Y.; Ogihara, Y. Personal or interpersonal construal of happiness: A cultural psychological perspective. Int. J. Wellbeing 2012, 2, 354–369. [Google Scholar] [CrossRef] [Green Version]
- Ricci, M.; Bellaby, P.; Flynn, R. Engaging the public on paths to sustainable energy: Who has to trust whom? Energy Policy 2010, 38, 2633–2640. [Google Scholar] [CrossRef]
- Smith, N.; Leiserowitz, A. The Role of Emotion in Global Warming Policy Support and Opposition. Risk Anal. 2013, 34, 937–948. [Google Scholar] [CrossRef] [Green Version]
- Linden, S.L.V.D. Determinants and measurement of climate change risk per- ception, worry, and concern. Oxford Encycl. Clim. Chang. Commun. 2017, 1, 53. [Google Scholar]
- Chiorri, C.; Bracco, F.; Piccinno, T.F.; Modafferi, C.; Battini, V. Psychometric Properties of a Revised Version of the Ten Item Personality Inventory. Eur. J. Psychol. Assess. 2015, 31, 109–119. [Google Scholar] [CrossRef] [Green Version]
- Gosling, S.D.; Rentfrow, P.J.; Swann, W.B., Jr. A very brief measure of the Big-Five personality domains. J. Res. Personal. 2003, 37, 504–528. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2017; Available online: https://www.R-project.org/ (accessed on 15 March 2021).
- Kuha, J. AIC and BIC: Comparisons of assumptions and performance. Sociol. Methods Res. 2004, 33, 188–229. [Google Scholar] [CrossRef]
- Paterson, P.; Meurice, F.; Stanberry, L.R.; Glismann, S.; Rosenthal, S.L.; Larson, H.J. Vaccine hesitancy and healthcare providers. Vaccine 2016, 34, 6700–6706. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Collange, F.; Zaytseva, A.; Pulcini, C.; Bocquier, A.; Verger, P. Unexplained variations in general practitioners’ perceptions and practices regarding vaccination in France. Eur. J. Public Health 2018, 29, 2–8. [Google Scholar] [CrossRef] [PubMed]
- Chapman, G.B.; Coups, E.J. Emotions and preventive health behavior: Worry, regret, and influenza vaccination. Health Psychol. 2006, 25, 82. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Soiza, R.L.; Scicluna, C.; Thomson, E.C. Efficacy and safety of COVID-19 vaccines in older people. Age Ageing 2020, 50, 279–283. [Google Scholar] [CrossRef]
- Costa, P.T.; McCrae, R.R. Influence of extraversion and neuroticism on subjective well-being: Happy and unhappy people. J. Personal. Soc. Psychol. 1980, 38, 668. [Google Scholar] [CrossRef]
- Polack, F.P.; Thomas, S.J.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Perez, J.L.; Marc, G.P.; Moreira, E.D.; Zerbini, C.; et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N. Engl. J. Med. 2020, 383, 2603–2615. [Google Scholar] [CrossRef]
| Happiness | Worry | |||
|---|---|---|---|---|
| AIC | BIC | AIC | BIC | |
| Model 1 | 20,047.18 | 20,073.74 | 22,591.11 | 22,617.56 |
| Model 2 | 18,831.12 | 18,877.19 | 21,293.84 | 21,339.74 |
| Model 3 | 10,990.02 | 11,008.35 | 13,374.31 | 13,392.55 |
| Model 4 | 10,397.43 | 10,421.7 | 12,793.261 | 12,817.41 |
| Model 5 | 10,299.23 | 10,329.56 | 12,543.95 | 12,574.13 |
| Model 6 | 9191.746 | 9263.494 | 11,434.22 | 11,505.7 |
| Model 5 | B | t | p |
|---|---|---|---|
| Intercept | 0.00000 | 1.66 | 0.095 |
| Vaccine utility | 0.36464 | 22.58 | 0.001 *** |
| COVID-19 risk | 0.15001 | 9.30 | 0.001 *** |
| Information | 0.10252 | 6.33 | 0.001 *** |
| Model 6 | B | t | p |
|---|---|---|---|
| Intercept | 0.000 | 11.50 | 0.001 *** |
| Age | 0.07165 | 3.81 | 0.001 *** |
| Education | −0.07716 | −4.19 | 0.001 *** |
| Extraversion | −0.02631 | −1.41 | 0.157 |
| Agreeableness | −0.01991 | −1.07 | 0.284 |
| Consciousness | 0.03002 | 1.63 | 0.102 |
| Emotional stability | −0.0623 | −2.25 | 0.0241 * |
| Openness | −0.0251 | −0.72 | 0.470 |
| Vaccine utility | −0.1672 | −9.26 | 0.001 *** |
| COVID-19 risk | 0.25152 | 13.76 | 0.001 *** |
| Information | 0.01366 | 0.74 | 0.455 |
| Happiness | Worry | |
|---|---|---|
| Social network | 0.21 ** | −0.45 ** |
| Scientific literature | 0.15 ** | −0.02 |
| Personal experience | 0.21 ** | −0.06 ** |
| Risks and benefits | 0.06 ** | −0.01 |
| Not promoting | −0.25 ** | 0.06 ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Logrieco, M.G.M.; Logrieco, G.; Nicolì, I.; Pignatelli, F.; Lionetti, F.; Traglia, F.; Spinelli, M.; Di Domenico, A.; Fasolo, M. How Were Healthcare Workers after Anti-SARS-CoV-2 Vaccination? A Study of the Emotional Side Effects of Vaccination. Vaccines 2022, 10, 854. https://doi.org/10.3390/vaccines10060854
Logrieco MGM, Logrieco G, Nicolì I, Pignatelli F, Lionetti F, Traglia F, Spinelli M, Di Domenico A, Fasolo M. How Were Healthcare Workers after Anti-SARS-CoV-2 Vaccination? A Study of the Emotional Side Effects of Vaccination. Vaccines. 2022; 10(6):854. https://doi.org/10.3390/vaccines10060854
Chicago/Turabian StyleLogrieco, Maria Grazia Mada, Giuseppe Logrieco, Ilaria Nicolì, Francesca Pignatelli, Francesca Lionetti, Francesco Traglia, Maria Spinelli, Alberto Di Domenico, and Mirco Fasolo. 2022. "How Were Healthcare Workers after Anti-SARS-CoV-2 Vaccination? A Study of the Emotional Side Effects of Vaccination" Vaccines 10, no. 6: 854. https://doi.org/10.3390/vaccines10060854






