Attitudes and Behavior toward COVID-19 Vaccination in Japanese University Students: A Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Ethical Considerations
2.3. Measures
2.4. Statistical Analysis
3. Results
3.1. Analysis of Students/Faculty Staff Who Have Been Vaccinated Twice
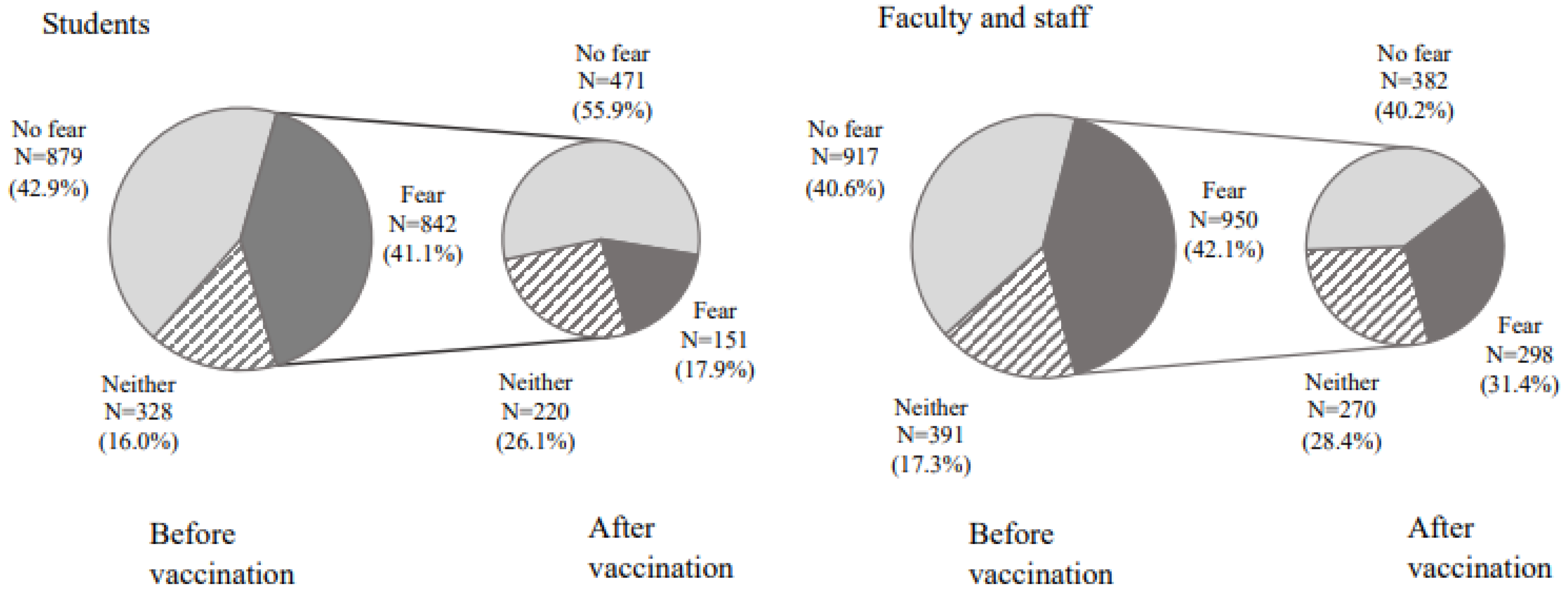
3.1.1. Fear of Vaccination before and after Vaccination
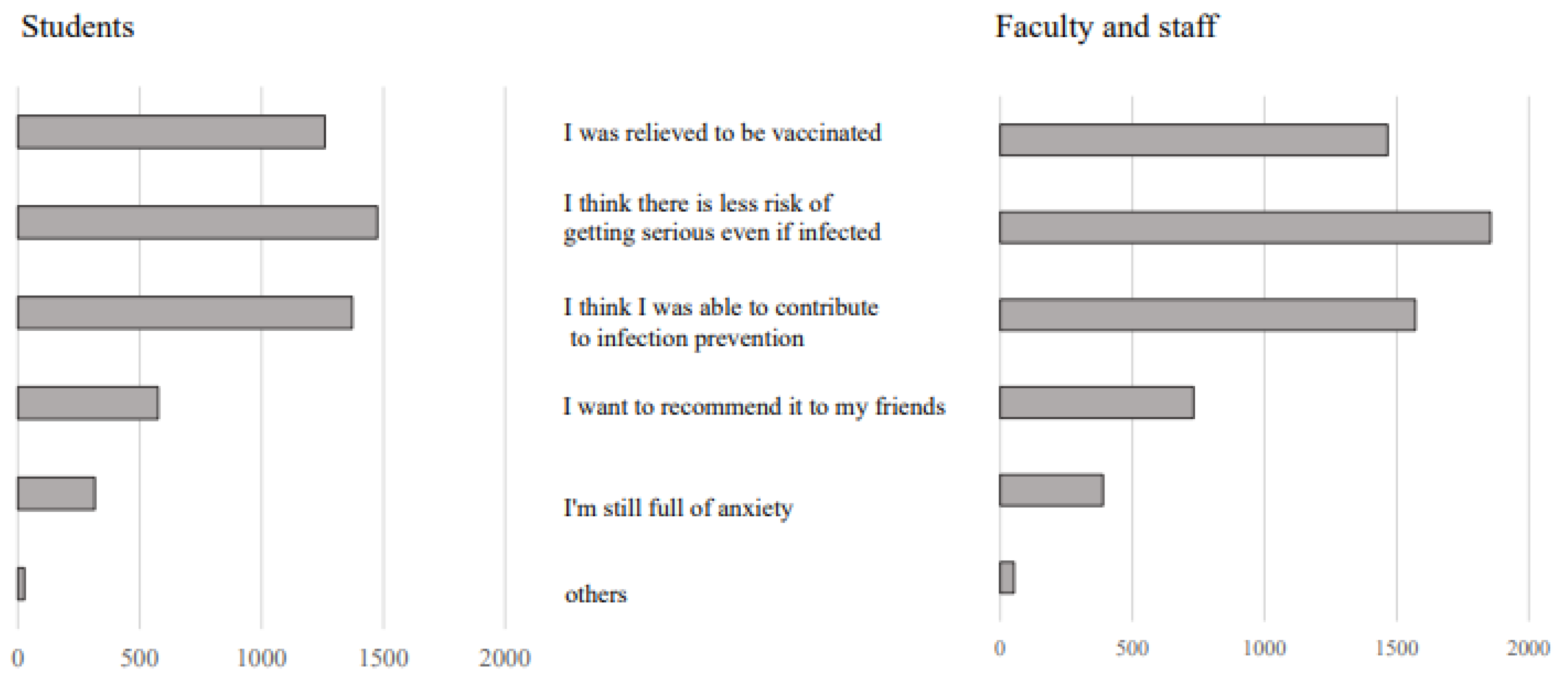
3.1.2. Impressions about Vaccination
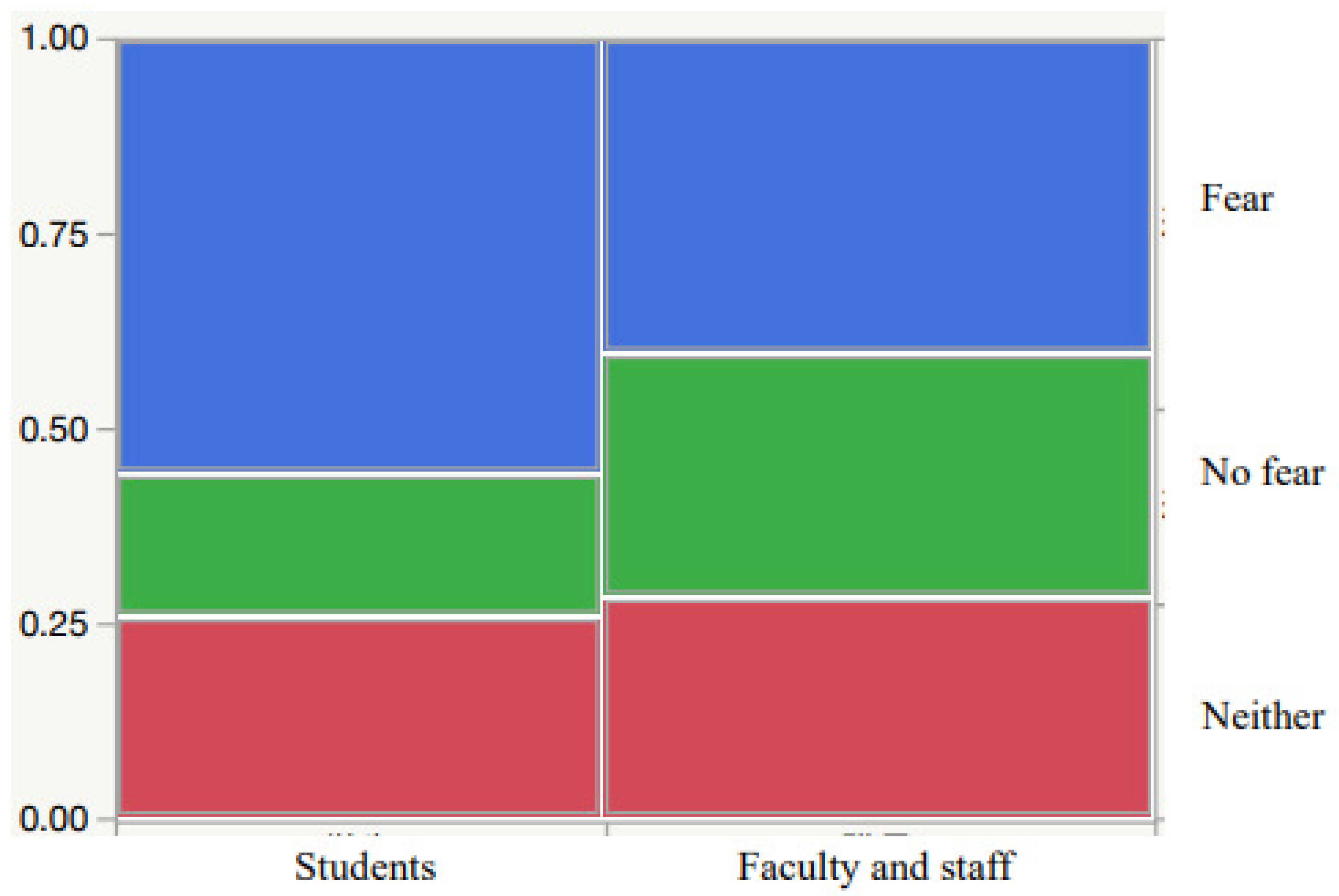
3.2. Comparison of Students and Faculty and Staff
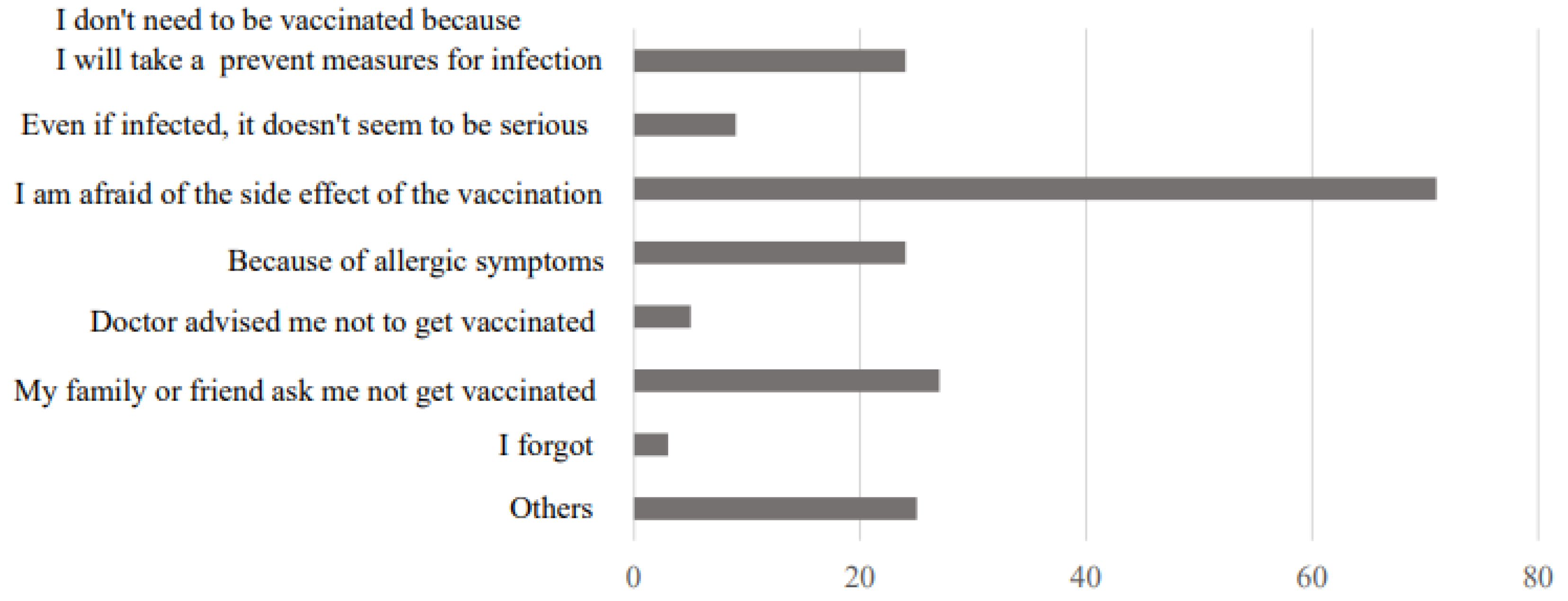
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Statement on the First Meeting of the International Health Regulations (2005) Emergency Committee Regarding the Outbreak of Novel Coronavirus (2019-nCoV). Available online: https://www.who.int/news/item/23-01-2020-statement-on-the-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-nCoV) (accessed on 26 March 2022).
- World Health Organization. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19-11 March 2020. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 26 March 2022).
- World Health Organization. WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 26 March 2022).
- Ministry of Health, Labour and Welfare. Current Situation in Japan. Available online: https://www.mhlw.go.jp/stf/covid-19/kokunainohasseijoukyou_00006.html (accessed on 26 March 2022).
- Latkin, C.A.; Dayton, L.; Yi, G.; Colon, B.; Kong, X. Mask usage, social distancing, racial and gender correlates of COVID-19 vaccine intentions among adults in the US. PLoS ONE 2021, 16, e0246970. [Google Scholar] [CrossRef] [PubMed]
- Romer, D.; Jamieson, K.H. Conspiracy theories as barriers to controlling the spread of COVID-19 in the U.S. Soc. Sci. Med. 2020, 263, 113356. [Google Scholar] [CrossRef] [PubMed]
- Troiano, G.; Nardi, A. Vaccine hesitancy in the era of COVID-19. Public Health 2021, 194, 245–251. [Google Scholar] [CrossRef] [PubMed]
- Adhikari, B.; Cheah, P.Y. Vaccine hesitancy in the COVID-19 era. Lancet Infect. Dis. 2021, 21, 1086. [Google Scholar] [CrossRef]
- Sharma, M.; Davis, R.E.; Wilkerson, A.H. COVID-19 vaccine acceptance among college students: A theory-based analysis. Int. J. Environ. Res. Public Health 2021, 18, 4617. [Google Scholar] [CrossRef]
- Yadate, T.; Batra, K.; Netski, D.M.; Antonio, S.; Patros, M.J.; Besterm, J.C. Assessing acceptancy of COVID-19 vaccine booster dose among adult Americans: A cross-sectional study. Vaccines 2021, 9, 1424. [Google Scholar] [CrossRef]
- National Institute of Infectious Diseases. Current Situation of Infection. 16 December 2021. Available online: https://www.niid.go.jp/niid/en/2019-ncov-e/10868-covid19-ab63th-en.html (accessed on 26 March 2022).
- Brüssow, H.; Zuber, S. Can a combination of vaccination and face mask wearing contain the COVID-19 pandemic? Microb. Biotechnol. 2022, 15, 721–737. [Google Scholar] [CrossRef]
- Ju, J.T.J.; Boisvert, L.N.; Zuo, Y.Y. Face masks against COVID-19: Standards, efficacy, testing and decontamination methods. Adv. Colloid. Interface Sci. 2021, 292, 102435. [Google Scholar] [CrossRef]
- Ortiz-Prado, E.; Simbaña-Rivera, K.; Gómez-Barreno, L.; Rubio-Neira, M.; Guaman, L.P.; Kyriakidis, N.C.; Muslin, C.; Jaramillo, A.M.G.; Barba-Ostria, C.; Cevallos-Robalino, D.; et al. Clinical, molecular, and epidemiological characterization of the SARS-CoV-2 virus and the Coronavirus Disease 2019 (COVID-19), a comprehensive literature review. Diagn. Microbiol. Infect. Dis. 2020, 98, 115094. [Google Scholar] [CrossRef]
- Howard, J.; Huang, A.; Li, Z.; Tufekci, Z.; Zdinal, V.; van der Westhuizen, H.M.; von Delft, A.; Price, A.; Fridman, L.; Tang, L.H.; et al. An evidence review of face masks against COVID-19. Proc. Natl. Acad. Sci. USA 2021, 118, e2014564118. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Bahav. Res. Meth. 2009, 41, 1149–1160. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lin, C.; Tu, P.; Beitsch, L.M. Confidence and Receptivity for COVID-19 vaccines: A rapid systematic review. Vaccines 2020, 9, 16. [Google Scholar] [CrossRef] [PubMed]
- Soares, P.; Rocha, J.V.; Moniz, M.; Gama, A.; Laires, P.A.; Pedro, A.R.; Dias, S.; Leite, A.; Nunes, C. Factors associated with COVID-19 vaccine hesitancy. Vaccines 2021, 9, 300. [Google Scholar] [CrossRef]
- Borges, J.; Byrne, M. Investigating COVID-19 risk perception and preventive behaviours in third-level students in Ireland. Acta Psychol. 2022, 224, 103535. [Google Scholar] [CrossRef]
- de Fiqueiredo, A.; Simas, C.; Karafillakis, E.; Paterson, P.; Larson, H.J. Mapping global trends in vaccine confidence and investigating barriers to vaccine uptake: A large-scale retrospective temporal modelling study. Lancet 2020, 396, 898–908. [Google Scholar] [CrossRef]
- Machida, M.; Nakamura, I.; Kojima, T.; Saito, R.; Nakaya, T.; Hanibuchi, T.; Takamiya, T.; Odagiri, Y.; Fukushima, N.; Kikuchi, H.; et al. Acceptance of a COVID-19 vaccine in Japan during the COVID-19 pandemic. Vaccines 2021, 9, 210. [Google Scholar] [CrossRef] [PubMed]
- Khubchandani, J.; Sharma, S.; Price, J.H.; Wiblishauser, M.J.; Sharma, M.; Webb, F.J. COVID-19 vaccination hesitancy in the United States: A rapid national assessment. J. Commun. Health 2021, 46, 270–277. [Google Scholar] [CrossRef]
- Kalam, M.A.; Davis, T.P., Jr.; Shano, S.; Uddin, M.N.; Islam, M.A.; Kanwagi, R.; Hassan, M.M.; Larson, H.J. Exploring the behavioral determinants of COBID-19 vaccine acceptance among an urban population in Bangladesh: Implications for behavior change interventions. PLoS ONE 2021, 16, e0256496. [Google Scholar] [CrossRef]
- Thaker, J.; Ganchoudhuri, S. The role of attitudes, norms, and efficacy on shifting COVID-19 vaccine intentions: A longitudinal study of COVID-19 vaccination intentions in New Zealand. Vaccines 2021, 9, 1132. [Google Scholar] [CrossRef]
- Li, J.B.; Yang, A.; Wang, L.X.; Zhang, M.C.; Lin, X.Q. Chinese public’s knowledge, perceived severity, and perceived controllability of COVID-19 and their associations with emotional and behavioural reactions, social participation, and precautionary behaviour: A national survey. BMC Public Health 2020, 20, 1589. [Google Scholar] [CrossRef]
- Lin, C.; Mullen, J.; Smith, D.; Kotarba, M.; Kaplan, S.J.; Tu, P. Hesitancy, and recommendation to patients: A systematic review. Vaccines 2021, 9, 713. [Google Scholar] [CrossRef] [PubMed]
- Sharma, M.; Barta, K.; Barta, R. A theory-based analysis of COVID-19 vaccine hesitancy among African Americans in the United States: A recent evidence. Healthcare 2021, 9, 1273. [Google Scholar] [CrossRef] [PubMed]
- Lu, H.; Weintz, C.; Pace, J.; Indana, D.; Linka, K.; Kuhl, E. Are college campuses superspreaders? A data-driven modeling study. Comput. Methods Biomech. Biomed. Engin. 2021, 24, 1136–1145. [Google Scholar] [CrossRef] [PubMed]
- Oosterhoff, B.; Palmer, C.A.; Wilson, J.; Shook, N. Adolescents’ motivations to engage in social distancing during the COVID-19 pandemic: Associations with mental and social health. J. Adolesc. Health 2020, 67, 179–185. [Google Scholar] [CrossRef]
- Kim, S.; Ko, Y.; Kim, Y.J.; Jung, E. The impact of social distancing and public behavior changes on COVID-19 transmission dynamics in the Republic of Korea. PLoS ONE 2020, 15, e0238684. [Google Scholar] [CrossRef]
- Siddiqui, S.; Qamar, A.H. Risk perception and protective behavior in the context of COVID-19: A qualitative exploration. Asian Bioeth. Rev. 2021, 13, 401–420. [Google Scholar] [CrossRef]
- Cohn-Shwartz, E.; Ayalon, L. COVID-19 protective bahaviors: The role of living arrangements and localities. J. Appl. Gerontol. 2021, 40, 799–803. [Google Scholar] [CrossRef]
- Jose, R.; Narendran, M.; Bindu, A.; Beevi, N.; Manju, L.; Benny, P.V. Public perception and preparedness for the pandemic COVID-19: A health belief model approach. Clin. Epidemiol. Glob. Health 2021, 9, 41–46. [Google Scholar] [CrossRef]
- Duan, Y.; Shang, B.; Liang, W.; Lin, Z.; Hu, C.; Baker, J.S.; Wang, Y.; He, J. Predicting hand washing, mask wearing and social distancing behaviors among older adults during the COVID-19 pandemic: An integrated social cognition model. BMC. Geriatr. 2022, 22, 91. [Google Scholar] [CrossRef]
- Tang, C.C.; Chen, H.; Wu, W.W. Factors influencing the protective behavior of individuals during COVID-19: A transnational survey. Sci. Rep. 2021, 11, 21654. [Google Scholar] [CrossRef]
- Zhong, J.; Zhong, C.; Qiu, L.; Li, J.; Lai, J.; Lu, W.; Wang, S.; Zhong, J.; Zhao, J.; Zhou, Y. Risk and protective factors for anxiety during COVID-19 pandemic. BMC Public Health 2021, 21, 1063. [Google Scholar] [CrossRef] [PubMed]
| Demography | Gender | Unvaccinated | One Vaccination | Two Vaccinations | Total |
|---|---|---|---|---|---|
| Students | Male | 42 | 11 | 1000 | 1053 |
| Female | 35 | 11 | 1049 | 1095 | |
| Neither | 1 | 0 | 11 | 12 | |
| Total | 78 | 22 | 2060 | 2160 | |
| Faculty and staff | Male | 5 | 2 | 1096 | 1103 |
| Female | 18 | 2 | 1162 | 1182 | |
| neither | 0 | 0 | 4 | 4 | |
| Total | 23 | 4 | 2262 | 2289 |
| Students N (%) | Faculty and Staff N (%) | ||
|---|---|---|---|
| Gender | Male | 1000 (48.8) | 1096 (48.5) |
| Female | 1049 (51.2) | 1162 (51.5) | |
| Fear of vaccination (before vaccination) | Yes | 842 (41.1) | 950 (42.1) |
| No | 879 (42.9) | 917 (40.6) | |
| Neither | 328 (16.0) | 391 (17.3) | |
| Trust in vaccination (before vaccination) | I totally believe | 164 (8.0) | 205 (9.1) |
| I believe to some extent | 1664 (81.2) | 1819 (80.6) | |
| I don‘t believe much | 94 (4.6) | 82 (3.6) | |
| Neither | 127 (6.2) | 152 (6.7) |
| Students N (%) | Faculty and Staff N (%) | ||
|---|---|---|---|
| Changes in feelings and behavior after vaccination | Yes | 567 (27.7) ** | 503 (22.3) |
| No | 1482 (72.3) | 1755 (77.7) ** | |
| Act with peace of mind after vaccination | Yes | 1141(55.7) ** | 866 (38.4) |
| No | 282 (13.8) | 426 (18.8) ** | |
| Neither | 626 (30.5) | 966 (42.8) ** | |
| Anxiety about infection after vaccination | Increased | 16 (0.8) | 20 (0.9) |
| Reduced | 822 (40.1) | 981 (43.4) | |
| No change | 1154 (56.3) | 1217 (54.0) | |
| I have no anxiety from before | 57 (2.8) | 40 (1.8) |
| Students N (%) | Faculty and Staff N (%) | ||
|---|---|---|---|
| Changes in range of action after vaccination | Extended | 271 (13.2) ** | 87 (3.9) |
| Narrowed | 6 (0.3) | 21 (0.9) | |
| No change | 1770 (86.4) | 2140 (94.8) | |
| Neither | 2 (0.1) | 10 (0.4) | |
| Contact with people after vaccination | Increased | 214 (10.4) ** | 53 (2.4) |
| Reduced | 16 (0.8) | 33 (1.5) ** | |
| No change | 1818 (88.7) | 2167 (96.0) | |
| Neither | 1 (0.1) | 5 (0.2) | |
| About infection prevention after vaccination | Be more careful | 97 (4.7) | 115 (5.1) |
| Little to be careful | 117 (5.7) ** | 32 (1.4) | |
| No change | 1799 (87.8) | 2066 (91.5) ** | |
| Neither | 36 (1.8) | 45 (2.0) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Okamoto, Y.; Hiyama, T.; Miyake, Y.; Yoshino, A.; Miyauchi, S.; Tanaka, J. Attitudes and Behavior toward COVID-19 Vaccination in Japanese University Students: A Cross-Sectional Study. Vaccines 2022, 10, 863. https://doi.org/10.3390/vaccines10060863
Okamoto Y, Hiyama T, Miyake Y, Yoshino A, Miyauchi S, Tanaka J. Attitudes and Behavior toward COVID-19 Vaccination in Japanese University Students: A Cross-Sectional Study. Vaccines. 2022; 10(6):863. https://doi.org/10.3390/vaccines10060863
Chicago/Turabian StyleOkamoto, Yuri, Toru Hiyama, Yoshie Miyake, Atsuo Yoshino, Shunsuke Miyauchi, and Junko Tanaka. 2022. "Attitudes and Behavior toward COVID-19 Vaccination in Japanese University Students: A Cross-Sectional Study" Vaccines 10, no. 6: 863. https://doi.org/10.3390/vaccines10060863
APA StyleOkamoto, Y., Hiyama, T., Miyake, Y., Yoshino, A., Miyauchi, S., & Tanaka, J. (2022). Attitudes and Behavior toward COVID-19 Vaccination in Japanese University Students: A Cross-Sectional Study. Vaccines, 10(6), 863. https://doi.org/10.3390/vaccines10060863





