Effectiveness of COVID-19 Vaccination in Preventing All-Cause Mortality among Adults during the Third Wave of the Epidemic in Hungary: Nationwide Retrospective Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Setting
2.2. Vaccination Status
2.3. Studied Variables
2.4. Statistical Analysis
2.5. Ethical Approval
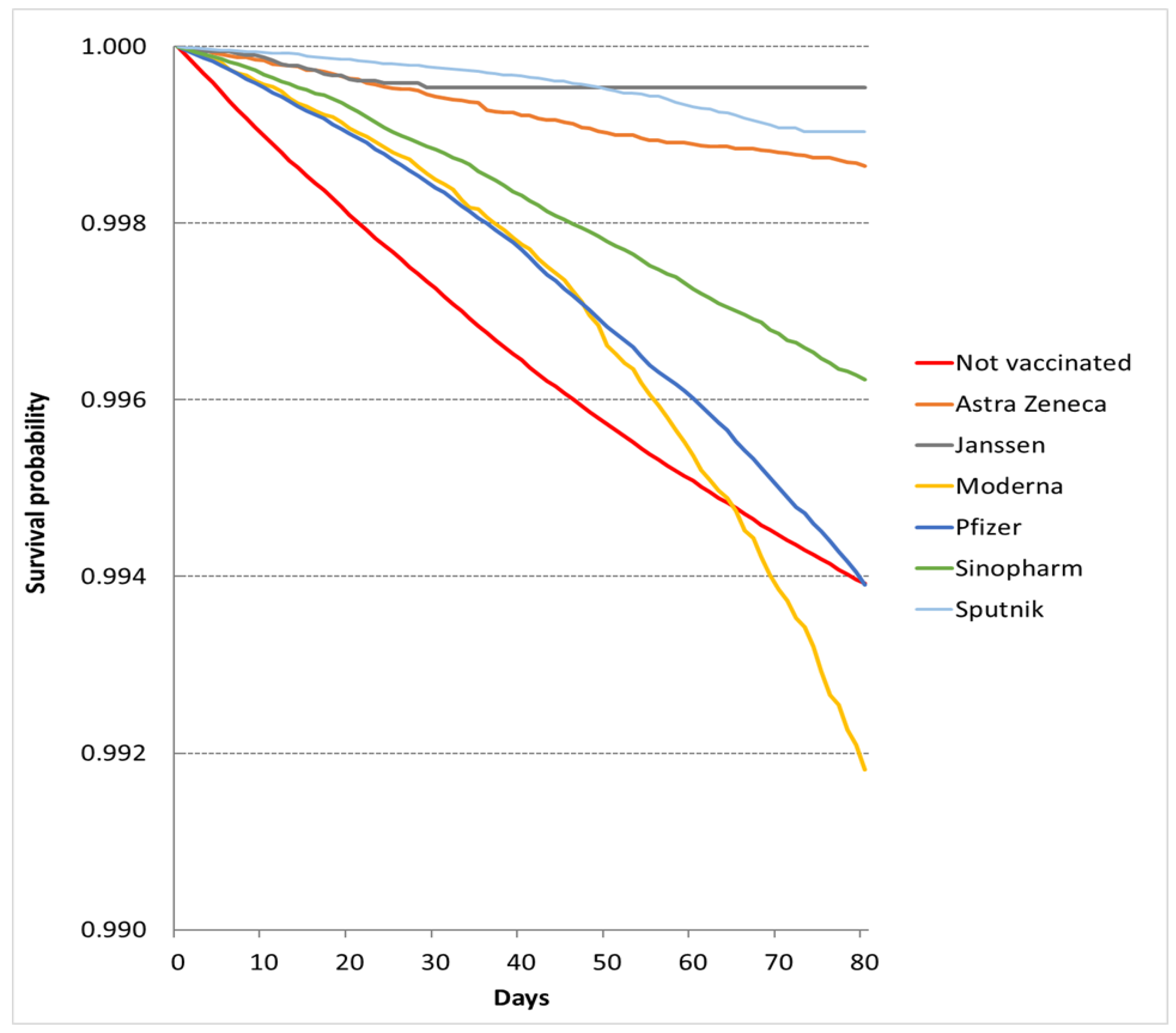
3. Results
3.1. Epidemic Period
3.2. Nonepidemic Period
3.3. Vaccine Effectiveness (VE) in Preventing All-Cause Mortality
4. Discussion
4.1. Main Findings
4.2. Strengths and Limitations
4.3. Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- COVID-19 Data Repository by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University. Available online: https://coronavirus.jhu.edu/map.html (accessed on 20 February 2022).
- Hale, T.; Angrist, N.; Goldszmidt, R.; Kira, B.; Petherick, A.; Phillips, T.; Webster, S.; Cameron-Blake, E.; Hallas, L.; Majumdar, S.; et al. A Global Panel Database of Pandemic Policies (Oxford COVID-19 Government Response Tracker). Nat. Hum. Behav. 2021, 5, 529–538. [Google Scholar] [CrossRef]
- Mathieu, E.; Ritchie, H.; Ortiz-Ospina, E.; Roser, M.; Hasell, J.; Appel, C.; Giattino, C.; Rodés-Guirao, L. A Global Database of COVID-19 Vaccinations. Nat. Hum. Behav. 2021, 5, 947–953. [Google Scholar] [CrossRef]
- Ritchie, H.; Mathieu, E.; Rodés-Guirao, L.; Appel, C.; Giattino, C.; Ortiz-Ospina, E.; Hasell, J.; Macdonald, B.; Beltekian, D.; Roser, M. Coronavirus Pandemic (COVID-19). Our World in Data. 2020. Available online: https://ourworldindata.org/covid-vaccinations (accessed on 14 June 2022).
- Pilkington, V.; Keestra, S.M.; Hill, A. Global COVID-19 Vaccine Inequity: Failures in the First Year of Distribution and Potential Solutions for the Future. Front. Public Health 2022, 10, 821117. [Google Scholar] [CrossRef]
- Gallè, F.; Sabella, E.A.; Roma, P.; Ferracuti, S.; Da Molin, G.; Diella, G.; Montagna, M.T.; Orsi, G.B.; Liguori, G.; Napoli, C. Knowledge and Lifestyle Behaviors Related to COVID-19 Pandemic in People over 65 Years Old from Southern Italy. Int. J. Environ. Res. Public. Health 2021, 18, 10872. [Google Scholar] [CrossRef]
- Clements, J.M. Knowledge and Behaviors Toward COVID-19 Among US Residents During the Early Days of the Pandemic: Cross-Sectional Online Questionnaire. JMIR Public Health Surveill. 2020, 6, e19161. [Google Scholar] [CrossRef]
- Troiano, G.; Nardi, A. Vaccine Hesitancy in the Era of COVID-19. Public Health 2021, 194, 245–251. [Google Scholar] [CrossRef]
- Freeman, D.; Loe, B.S.; Chadwick, A.; Vaccari, C.; Waite, F.; Rosebrock, L.; Jenner, L.; Petit, A.; Lewandowsky, S.; Vanderslott, S.; et al. COVID-19 Vaccine Hesitancy in the UK: The Oxford Coronavirus Explanations, Attitudes, and Narratives Survey (Oceans) II. Psychol. Med. 2020, 1–15. [Google Scholar] [CrossRef]
- Sallam, M. COVID-19 Vaccine Hesitancy Worldwide: A Concise Systematic Review of Vaccine Acceptance Rates. Vaccines 2021, 9, 160. [Google Scholar] [CrossRef]
- Bíró-Nagy, A.; Szászi, Á.J. The Roots of COVID-19 Vaccine Hesitancy: Evidence from Hungary. J. Behav. Med. 2022, 1–16. [Google Scholar] [CrossRef]
- Dombrádi, V.; Joó, T.; Palla, G.; Pollner, P.; Belicza, É. Comparison of Hesitancy between COVID-19 and Seasonal Influenza Vaccinations within the General Hungarian Population: A Cross-Sectional Study. BMC Public Health 2021, 21, 2317. [Google Scholar] [CrossRef]
- Zheng, C.; Shao, W.; Chen, X.; Zhang, B.; Wang, G.; Zhang, W. Real-World Effectiveness of COVID-19 Vaccines: A Literature Review and Meta-Analysis. Int. J. Infect. Dis. 2022, 114, 252–260. [Google Scholar] [CrossRef]
- Liu, Q.; Qin, C.; Liu, M.; Liu, J. Effectiveness and Safety of SARS-CoV-2 Vaccine in Real-World Studies: A Systematic Review and Meta-Analysis. Infect. Dis. Poverty 2021, 10, 132. [Google Scholar] [CrossRef]
- Food and Drug Administration. Janssen COVID-19 Vaccine Emergency Use Authorization Letter. Silver Spring, MD: US Department of Health and Human Services. Available online: https://www.fda.gov/media/146303/download (accessed on 20 February 2022).
- Xu, S. COVID-19 Vaccination and Non–COVID-19 Mortality Risk—Seven Integrated Health Care Organizations, United States, 14 December 2020–31 July 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 1520–1524. [Google Scholar] [CrossRef]
- Macchia, A.; Ferrante, D.; Angeleri, P.; Biscayart, C.; Mariani, J.; Esteban, S.; Tablado, M.R.; de Quirós, F.G.B. Evaluation of a COVID-19 Vaccine Campaign and SARS-CoV-2 Infection and Mortality Among Adults Aged 60 Years and Older in a Middle-Income Country. JAMA Netw. Open 2021, 4, e2130800. [Google Scholar] [CrossRef]
- Eurich, D.T.; Johnstone, J.J.; Minhas-Sandhu, J.K.; Marrie, T.J.; Majumdar, S.R. Pneumococcal Vaccination and Risk of Acute Coronary Syndromes in Patients with Pneumonia: Population-Based Cohort Study. Heart 2012, 98, 1072–1077. [Google Scholar] [CrossRef]
- Jackson, L.A.; Nelson, J.C.; Benson, P.; Neuzil, K.M.; Reid, R.J.; Psaty, B.M.; Heckbert, S.R.; Larson, E.B.; Weiss, N.S. Functional Status Is a Confounder of the Association of Influenza Vaccine and Risk of All Cause Mortality in Seniors. Int. J. Epidemiol. 2006, 35, 345–352. [Google Scholar] [CrossRef]
- Simonsen, L.; Taylor, R.J.; Viboud, C.; Miller, M.A.; Jackson, L.A. Mortality Benefits of Influenza Vaccination in Elderly People: An Ongoing Controversy. Lancet Infect. Dis. 2007, 7, 658–666. [Google Scholar] [CrossRef]
- Mathieu, E.; Roser, M. How Do Death Rates from COVID-19 Differ between People Who Are Vaccinated and Those Who Are Not? Available online: https://ourworldindata.org/covid-deaths-by-vaccination (accessed on 20 February 2022).
- Polack, F.P.; Thomas, S.J.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Perez, J.L.; Pérez Marc, G.; Moreira, E.D.; Zerbini, C.; et al. Safety and Efficacy of the BNT162b2 MRNA Covid-19 Vaccine. N. Engl. J. Med. 2020, 383, 2603–2615. [Google Scholar] [CrossRef]
- Baden, L.R.; El Sahly, H.M.; Essink, B.; Kotloff, K.; Frey, S.; Novak, R.; Diemert, D.; Spector, S.A.; Rouphael, N.; Creech, C.B.; et al. Efficacy and Safety of the MRNA-1273 SARS-CoV-2 Vaccine. N. Engl. J. Med. 2021, 384, 403–416. [Google Scholar] [CrossRef]
- Voysey, M.; Clemens, S.A.C.; Madhi, S.A.; Weckx, L.Y.; Folegatti, P.M.; Aley, P.K.; Angus, B.; Baillie, V.L.; Barnabas, S.L.; Bhorat, Q.E.; et al. Safety and Efficacy of the ChAdOx1 NCoV-19 Vaccine (AZD1222) against SARS-CoV-2: An Interim Analysis of Four Randomised Controlled Trials in Brazil, South Africa, and the UK. Lancet 2021, 397, 99–111. [Google Scholar] [CrossRef]
- Logunov, D.Y.; Dolzhikova, I.V.; Shcheblyakov, D.V.; Tukhvatulin, A.I.; Zubkova, O.V.; Dzharullaeva, A.S.; Kovyrshina, A.V.; Lubenets, N.L.; Grousova, D.M.; Erokhova, A.S.; et al. Safety and Efficacy of an RAd26 and RAd5 Vector-Based Heterologous Prime-Boost COVID-19 Vaccine: An Interim Analysis of a Randomised Controlled Phase 3 Trial in Russia. Lancet 2021, 397, 671–681. [Google Scholar] [CrossRef]
- Al Kaabi, N.; Zhang, Y.; Xia, S.; Yang, Y.; Al Qahtani, M.M.; Abdulrazzaq, N.; Al Nusair, M.; Hassany, M.; Jawad, J.S.; Abdalla, J.; et al. Effect of 2 Inactivated SARS-CoV-2 Vaccines on Symptomatic COVID-19 Infection in Adults. JAMA 2021, 326, 35–45. [Google Scholar] [CrossRef] [PubMed]
- Kovács, N.; Pálinkás, A.; Sipos, V.; Nagy, A.; Harsha, N.; Kőrösi, L.; Papp, M.; Ádány, R.; Varga, O.; Sándor, J. Factors Associated with Practice-Level Performance Indicators in Primary Health Care in Hungary: A Nationwide Cross-Sectional Study. Int. J. Environ. Res. Public Health 2019, 16, 3153. [Google Scholar] [CrossRef] [Green Version]
- Kovács, N.; Varga, O.; Nagy, A.; Pálinkás, A.; Sipos, V.; Kőrösi, L.; Ádány, R.; Sándor, J. The Impact of General Practitioners’ Gender on Process Indicators in Hungarian Primary Healthcare: A Nation-Wide Cross-Sectional Study. BMJ Open 2019, 9, e027296. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sándor, J.; Pálinkás, A.; Vincze, F.; Sipos, V.; Kovács, N.; Jenei, T.; Falusi, Z.; Pál, L.; Kőrösi, L.; Papp, M.; et al. Association between the General Practitioner Workforce Crisis and Premature Mortality in Hungary: Cross-Sectional Evaluation of Health Insurance Data from 2006 to 2014. Int. J. Environ. Res. Public Health 2018, 15, 1388. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- European Centre for Disease Prevention and Control. Data—National 14-Day Notification Rate (Cases and Deaths). Available online: https://www.ecdc.europa.eu/en/publications-data/data-national-14-day-notification-rate-covid-19 (accessed on 20 February 2022).
- Bogos, K.; Kiss, Z.; Kerpel Fronius, A.; Temesi, G.; Jenő, E.; Madurka, I.; Cselkó, Z.; Csanyi, P.; Abonyi-Tóth, Z.; Rokszin MD, G.; et al. Different Trends in Excess Mortality in a Central European Country Compared to Main European Regions in the Year of the COVID-19 Pandemic (2020): A Hungarian Analysis. Pathol. Oncol. Res. 2021, 27, 11609774. [Google Scholar] [CrossRef]
- Danics, K.; Pesti, A.; Törő, K.; Kiss-Dala, N.; Szlávik, J.; Lakatos, B.; Radnai, A.; Balázs, T.; Bacskai, M.; Dobi, D.; et al. A COVID-19-Association-Dependent Categorization of Death Causes in 100 Autopsy Cases. GeroScience 2021, 43, 2265–2287. [Google Scholar] [CrossRef]
- Gaal, P.; Szigeti, S.; Csere, M.; Gaskins, M.; Panteli, D. Hungary Health System Review. Health Syst. Transit. 2011, 13, 59–101. [Google Scholar]
- Hatcher, S.M.; Endres-Dighe, S.M.; Angulo, F.J.; Srivastava, A.; Nguyen, J.L.; Khan, F.; Martin, C.; Swerdlow, D.L.; McLaughlin, J.M.; Ubaka-Blackmore, N.; et al. COVID-19 Vaccine Effectiveness: A Review of the First 6 Months of COVID-19 Vaccine Availability (1 January–30 June 2021). Vaccines 2022, 10, 393. [Google Scholar] [CrossRef]
- Lichtner, G.; Balzer, F.; Haufe, S.; Giesa, N.; Schiefenhövel, F.; Schmieding, M.; Jurth, C.; Kopp, W.; Akalin, A.; Schaller, S.J.; et al. Predicting Lethal Courses in Critically Ill COVID-19 Patients Using a Machine Learning Model Trained on Patients with Non-COVID-19 Viral Pneumonia. Sci. Rep. 2021, 11, 13205. [Google Scholar] [CrossRef]
- Cosgrove, K.; Wharton, C. Predictors of COVID-19-Related Perceived Improvements in Dietary Health: Results from a US Cross-Sectional Study. Nutrients 2021, 13, 2097. [Google Scholar] [CrossRef] [PubMed]
- Nicola, M.; Alsafi, Z.; Sohrabi, C.; Kerwan, A.; Al-Jabir, A.; Iosifidis, C.; Agha, M.; Agha, R. The Socio-Economic Implications of the Coronavirus Pandemic (COVID-19): A Review. Int. J. Surg. 2020, 78, 185–193. [Google Scholar] [CrossRef] [PubMed]
- Khalifa, S.A.M.; Swilam, M.M.; El-Wahed, A.A.A.; Du, M.; El-Seedi, H.H.R.; Kai, G.; Masry, S.H.D.; Abdel-Daim, M.M.; Zou, X.; Halabi, M.F.; et al. Beyond the Pandemic: COVID-19 Pandemic Changed the Face of Life. Int. J. Environ. Res. Public Health 2021, 18, 5645. [Google Scholar] [CrossRef] [PubMed]
- Shi, L.; Lu, Z.-A.; Que, J.-Y.; Huang, X.-L.; Liu, L.; Ran, M.-S.; Gong, Y.-M.; Yuan, K.; Yan, W.; Sun, Y.-K.; et al. Prevalence of and Risk Factors Associated With Mental Health Symptoms Among the General Population in China During the Coronavirus Disease 2019 Pandemic. JAMA Netw. Open 2020, 3, e2014053. [Google Scholar] [CrossRef]
- Zhou, H.; Geng, H.; Dong, C.; Bai, T. The Short-Term Harvesting Effects of Ambient Particulate Matter on Mortality in Taiyuan Elderly Residents: A Time-Series Analysis with a Generalized Additive Distributed Lag Model. Ecotoxicol. Environ. Saf. 2021, 207, 111235. [Google Scholar] [CrossRef]
- Mallapaty, S. Can COVID Vaccines Stop Transmission? Scientists Race to Find Answers. Nat. News 2021. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control. Data on COVID-19 Vaccination in the EU/EEA. Available online: https://www.ecdc.europa.eu/en/publications-data/data-covid-19-vaccination-eu-eea (accessed on 20 February 2022).
- World Health Organization WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/table (accessed on 20 February 2022).
- Centers for Diseases. Control and Prevention COVID Data Tracker Weekly Review. Available online: https://www.cdc.gov/coronavirus/2019-ncov/covid-data/covidview/index.html (accessed on 20 February 2022).
- Centers for Diseases. Control and Prevention. COVID-19 Vaccine Effectiveness Research. Available online: https://www.cdc.gov/vaccines/covid-19/effectiveness-research/protocols.html (accessed on 20 February 2022).

| Deaths, N (%) | Censored, N (%) | Total, N (Vaccine Share %) | Observed Person-Days | Mortality Rate Per 100,000 Person-Days | |
|---|---|---|---|---|---|
| AstraZeneca | 176 (0.05%) | 333,304 (99.95%) | 333,480 (5.21%) | 10,094,843 | 1.74% [1.49–2.00%] |
| Janssen | 26 (0.03%) | 78,369 (99.97%) | 78,395 (1.22%) | 1,638,877 | 1.59% [0.98–2.19%] |
| Moderna | 684 (0.28%) | 242,732 (99.72%) | 243,416 (3.80%) | 9,304,244 | 7.35% [6.82–7.88%] |
| Pfizer | 4804 (0.30%) | 1,599,446 (99.70%) | 1,604,250 (25.05%) | 70,949,254 | 6.77% [6.59–6.96%] |
| Sinopharm | 1973 (0.21%) | 917,637 (99.79%) | 919,610 (14.36%) | 43,526,230 | 4.53% [4.34–4.73%] |
| Sputnik | 380 (0.04%) | 847,318 (99.96%) | 847,698 (13.24%) | 37,655,141 | 1.01% [0.91–1.11%] |
| p-value * | <0.001 | - | - | - | |
| Fully vaccinated | 8043 (0.20%) | 4,018,806 (99.80%) | 4,026,849 (62.87%) | 173,168,589 | 4.64% [4.55–4.74%] |
| Not vaccinated | 18,387 (0.77%) | 2,359,466 (99.23%) | 2,377,853 (37.13%) | 229,492,866 | 8.01% [7.90–8.12%] |
| p-value ** | <0.001 | - | - | - | |
| Total | 26,430 (0.41%) | 6,378,272 (99.59%) | 6,404,702 (100%) | 402,661,455 | 6.56% [6.49–6.64%] |
| HR * for 1 April 2021 to 20 June 2021 Period | HR * for 21 June 2021 to 15 August 2021 Period | Difference of Hazard Ratios | Effectiveness in Preventing All-Cause-Mortality | |
|---|---|---|---|---|
| AstraZeneca | 0.129 [0.111–0.150] | 0.317 [0.294–0.341] | 0.408 [0.345–0.482] | 0.592 [0.518–0.655] |
| Janssen | 0.174 [0.118–0.255] | 0.707 [0.604–0.828] | 0.246 [0.162–0.372] | 0.754 [0.628–0.838] |
| Moderna | 0.187 [0.173–0.202] | 0.438 [0.409–0.469] | 0.427 [0.385–0.474] | 0.573 [0.526–0.615] |
| Pfizer | 0.197 [0.190–0.203] | 0.384 [0.370–0.399] | 0.513 [0.487–0.539] | 0.487 [0.461–0.513] |
| Sinopharm | 0.147 [0.140–0.154] | 0.312 [0.297–0.328] | 0.470 [0.439–0.504] | 0.530 [0.496–0.561] |
| Sputnik | 0.098 [0.088–0.108] | 0.221 [0.202–0.242] | 0.443 [0.386–0.507] | 0.557 [0.493–0.614] |
| Deaths, N (%) | Censored, N (%) | Total, N (Vaccine Share %) | Observed Person-Day | Mortality Rate per 100,000 Person-Days | |
|---|---|---|---|---|---|
| AstraZeneca | 792 (0.13%) | 592,609 (99.87%) | 593,401 (8.22%) | 28,240,807 | 2.80% [2.61–3.00%] |
| Janssen | 160 (0.16%) | 98,394 (99.84%) | 98,554 (1.37%) | 5,044,716 | 3.17% [2.69–3.66%] |
| Moderna | 1027 (0.32%) | 320,948 (99.68%) | 321,975 (4.46%) | 16,822,495 | 6.10% [5.74–6.47%] |
| Pfizer | 5603 (0.26%) | 2,123,839 (99.74%) | 2,129,442 (29.51%) | 108,239,884 | 5.18% [5.04–5.31%] |
| Sinopharm | 2203 (0.22%) | 977,239 (99.78%) | 979,442 (13.57%) | 52,933,464 | 4.16% [3.99–4.33%] |
| Sputnik | 520 (0.06%) | 866,277 (99.94%) | 866,797 (12.01%) | 47,374,813 | 1.10% [1.00–1.19%] |
| p-value * | <0.001 | - | - | - | |
| Fully vaccinated | 10,305 (0.21%) | 4,979,306 (99.79%) | 4,989,611 (69.15%) | 258,656,179 | 3.98% [3.91–4.06%] |
| Not vaccinated | 6548 (0.29%) | 2,219,631 (99.71%) | 2,226,179 (30.85%) | 123,049,996 | 5.32% [5.20–5.45%] |
| p-value ** | <0.001 | - | - | - | |
| Total | 16,853 (0.23%) | 7,198,937 (99.77%) | 7,215,790 (100%) | 381,706,175 | 4.42% [4.35–4.48%] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pálinkás, A.; Sándor, J. Effectiveness of COVID-19 Vaccination in Preventing All-Cause Mortality among Adults during the Third Wave of the Epidemic in Hungary: Nationwide Retrospective Cohort Study. Vaccines 2022, 10, 1009. https://doi.org/10.3390/vaccines10071009
Pálinkás A, Sándor J. Effectiveness of COVID-19 Vaccination in Preventing All-Cause Mortality among Adults during the Third Wave of the Epidemic in Hungary: Nationwide Retrospective Cohort Study. Vaccines. 2022; 10(7):1009. https://doi.org/10.3390/vaccines10071009
Chicago/Turabian StylePálinkás, Anita, and János Sándor. 2022. "Effectiveness of COVID-19 Vaccination in Preventing All-Cause Mortality among Adults during the Third Wave of the Epidemic in Hungary: Nationwide Retrospective Cohort Study" Vaccines 10, no. 7: 1009. https://doi.org/10.3390/vaccines10071009
APA StylePálinkás, A., & Sándor, J. (2022). Effectiveness of COVID-19 Vaccination in Preventing All-Cause Mortality among Adults during the Third Wave of the Epidemic in Hungary: Nationwide Retrospective Cohort Study. Vaccines, 10(7), 1009. https://doi.org/10.3390/vaccines10071009






