Students as Community Vaccinators: Implementation of A Service-Learning COVID-19 Vaccination Program
Abstract
1. Introduction
2. Materials and Methods
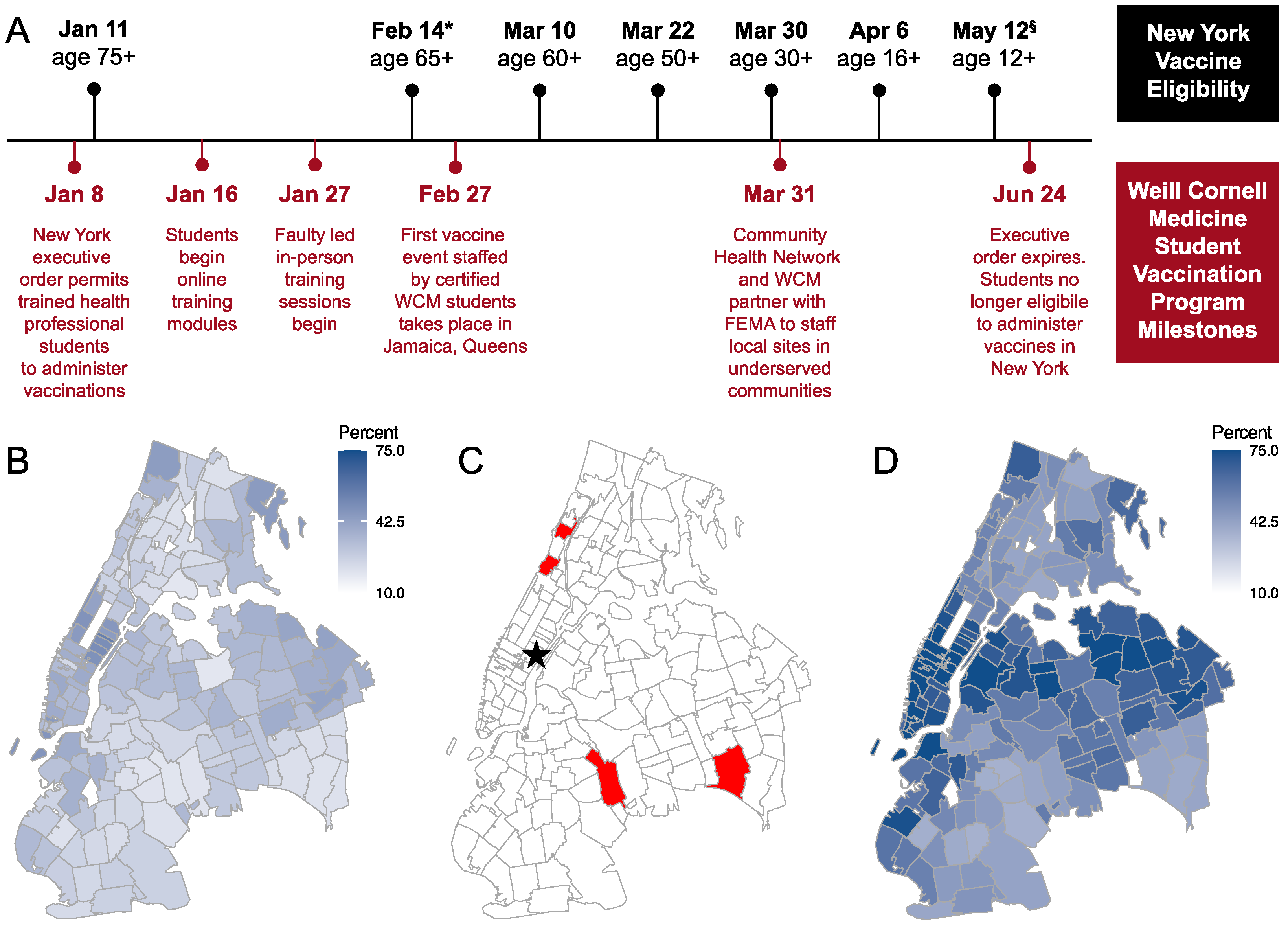
2.1. Program Development
2.2. Vaccination Events
2.3. Retrospective Survey Development and Administration
3. Results
3.1. Student Participants
3.2. Patient Demographics
3.3. Evaluation of the Vaccination Program
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Stewart, T.; Wubbena, Z.C. A systematic review of service-learning in medical education: 1998–2012. Teach. Learn. Med. 2015, 27, 115–122. [Google Scholar] [CrossRef]
- Hunt, J.B.; Bonham, C.; Jones, L. Understanding the goals of service learning and community-based medical education: A systematic review. Acad. Med. 2011, 86, 246–251. [Google Scholar] [CrossRef]
- LCME. Functions and Structure of a Medical School: Standards for Accreditation of Medical Education Programs Leading to the MD Degree; Liaison Committee on Medical Education: Washington, DC, USA, 2021. [Google Scholar]
- Tiako, M.J.N.; Johnson, S.F.; Nkinsi, N.T.; Landry, A. Normalizing Service Learning in Medical Education to Sustain Medical Student-Led Initiatives. Acad. Med. 2021, 96, 1634–1637. [Google Scholar] [CrossRef]
- Kochis, M.; Goessling, W. Learning During and From a Crisis: The Student-Led Development of a COVID-19 Curriculum. Acad. Med. 2020, 96, 399–401. [Google Scholar] [CrossRef]
- Alshak, M.N.; Li, H.A.; Wehmeyer, G.T. Medical Students as Essential Frontline Researchers During the COVID-19 Pandemic. Acad. Med. 2021, 96, 964–966. [Google Scholar] [CrossRef]
- de Moura Villela, E.F.; de Oliveira, F.M.; Leite, S.T.; Bollela, V.R. Student engagement in a public health initiative in response to COVID-19. Med. Educ. 2020, 54, 763–764. [Google Scholar] [CrossRef]
- Long, N.; Wolpaw, D.R.; Boothe, D.; Caldwell, C.; Dillon, P.; Gottshall, L.; Koetter, P.; Pooshpas, P.; Wolpaw, T.; Gonzalo, J.D. Contributions of Health Professions Students to Health System Needs during the COVID-19 Pandemic: Potential Strategies and Process for U. S. Medical Schools. Acad. Med. 2020, 10, 1679–1686. [Google Scholar] [CrossRef]
- Zhou, B.; Calkins, C.; Jayaraman, T.; Cassells, S.; Rotto, T.; Vaughan, L.; Srinivasan, M.; Schillinger, E. Implementing Value-Added Medical Education: Lessons Learned From the Student-Initiated Stanford Frontline COVID-19 Consult Service. Acad. Med. 2021, 96, 1690–1695. [Google Scholar] [CrossRef]
- Flotte, T.R.; Larkin, A.C.; Fischer, M.A.; Chimienti, S.N.; DeMarco, D.M.; Fan, P.-Y.; Collins, M.F. Accelerated Graduation and the Deployment of New Physicians During the COVID-19 Pandemic. Acad. Med. 2020, 95, 1492–1494. [Google Scholar] [CrossRef]
- Redford, G. “Itching to get back in”: Medical students graduate early to join the fight. In Association of American Medical Colleges; AAMC: Washington, DC, USA, 2020. [Google Scholar]
- Nanette, P.; Ribault, S.; Peyrot, S.; Villa, V.; Ritou, I.; Coiffet, M.; Al Gholam, C.; Jarraud, S.; Laurent, F.; Rode, G. Medical student engagement in a massive COVID-19-screening programme. Med. Educ. 2021, 55, 1299–1300. [Google Scholar] [CrossRef]
- Soled, D.; Goel, S.; Barry, D.; Erfani, P.; Joseph, N.; Kochis, M.; Uppal, N.; Velasquez, D.; Vora, K.; Scott, K.W. Medical Student Mobilization During a Crisis: Lessons From a COVID-19 Medical Student Response Team. Acad. Med. 2020, 95, 1384–1387. [Google Scholar] [CrossRef] [PubMed]
- Tsang, V.W.; Yu, A.; Haines, M.J.; Sagorin, Z.; Mitchell, D.; Ching, G.; Holmes, C.L.; Kestler, M. Transforming Disruption Into Innovation: A Partnership Between the COVID-19 Medical Student Response Team and the University of British Columbia. Acad. Med. 2021, 96, 1650–1654. [Google Scholar] [CrossRef] [PubMed]
- Weiss, C.; Traczuk, A.; Motley, R. Reopening a Student-Run Free Clinic During the COVID-19 Pandemic to Provide Care for People Experiencing Homelessness. Acad. Med. 2021, 97, 855–857. [Google Scholar] [CrossRef] [PubMed]
- Menon, A.; Klein, E.J.; Kollars, K.; Kleinhenz, A.L. Medical Students Are Not Essential Workers: Examining Institutional Responsibility During the COVID-19 Pandemic. Acad. Med. 2020, 95, 1149–1151. [Google Scholar] [CrossRef] [PubMed]
- Crosby, A.W. America’s Forgotten Pandemic: The Influenza of 1918, 2nd ed.; Cambridge University Press: Cambridge, UK, 2003; pp. 1–337. [Google Scholar]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef] [PubMed]
- U.S. COVID-19 Vaccine Tracker. Available online: https://www.mayoclinic.org/coronavirus-COVID-19/vaccine-tracker (accessed on 1 November 2021).
- Thomas, A.T.; Gilja, S.; Sikka, N.; Onuh, O.; Kellner, R.; Schussler, L.; Sun, M.; Hurtado, A.M. Peer-to-peer COVID-19 medical curriculum development during the pandemic. Med. Educ. 2021, 55, 1302–1303. [Google Scholar] [CrossRef]
- Klasen, J.M.; Meienberg, A.; Bogie, B.J.M. Medical student engagement during COVID-19: Lessons learned and areas for improvement. Med. Educ. 2021, 55, 115–118. [Google Scholar] [CrossRef]
- Matthew, D.; Eftychiou, L.; French, C.; Hare, A. ‘Just in time’ rapid learning during COVID-19. Med. Educ. 2021, 55, 1300–1301. [Google Scholar] [CrossRef]
- Castro, M.R.; Calthorpe, L.M.; Fogh, S.E.; McAllister, S.; Johnson, C.L.; Isaacs, E.D.; Ishizaki, A.; Kozas, A.; Lo, D.; Rennke, S.; et al. Lessons From Learners: Adapting Medical Student Education During and Post COVID-19. Acad. Med. 2021, 96, 1671–1679. [Google Scholar] [CrossRef]
- Gordon, M.; Kim, H.W.; Kennedy, W.; Di Bartolo, I.M. Utilising medical students as wellness coaches during the COVID-19 pandemic. Med. Educ. 2021, 55, 1306–1307. [Google Scholar] [CrossRef]
- Shibu, A. Medical student engagement during the COVID-19 pandemic—A student perspective. Med. Educ. 2021, 55, 768. [Google Scholar] [CrossRef] [PubMed]
- Grilo, S.A.; Catallozzi, M.; Desai, U.; Sein, A.S.; Baumgart, C.Q.; Timmins, G.; Edelman, D.; Amiel, J.M. Columbia COVID-19 Student Service Corps: Harnessing student skills and galvanizing the power of service learning. FASEB BioAdvances 2020, 3, 166–174. [Google Scholar] [CrossRef] [PubMed]
- Magklara, E.; Angelis, S.; Solia, E.; Katsimantas, A.; Kourlaba, G.; Kostakis, G.; Tsakotos, G.; Zaoutis, T.; Filippou, D. The Role of Medical Students During COVID-19 Era. A Review. Acta Biomed. Atenei Parm. 2021, 92, 2021032. [Google Scholar]
- Schuiteman, S.; Ibrahim, N.I.; Hammoud, A.; Kruger, L.; Mangrulkar, R.S.; Daniel, M. The Role of Medical Student Government in Responding to COVID-19. Acad. Med. 2020, 96, 62–67. [Google Scholar] [CrossRef]
- Edelman, D.S.; Desai, U.A.; Soo-Hoo, S.; Catallozzi, M. Responding to hospital system and student curricular needs: COVID-19 Student Service Corps. Med. Educ. 2020, 54, 853–854. [Google Scholar] [CrossRef]
- Sinclair, T.; Bell, B.I.; Perez, K.; Klyde, D.; Veith, M.; Weinstock, R.; Cassese, T.; Nosanchuk, J.D. Rapid Mobilization of Medical Student Volunteers to Administer Vaccines During the COVID-19 Pandemic. J. Med. Educ. Curric. Dev. 2022, 9, 1–6. [Google Scholar] [CrossRef]
- Dong, E.; Du, H.; Gardner, L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect. Dis. 2020, 20, 533–534. [Google Scholar] [CrossRef]
- Shuftan, N. COVID-19 Health System Response Monitor (HSRM). 2022. Available online: https://eurohealthobservatory.who.int/monitors/hsrm/analyses/hsrm/who-is-tasked-with-administering-COVID-19-vaccines-in-europe (accessed on 31 May 2022).
- Mallhi, T.H.; Liaqat, A.; Abid, A.; Khan, Y.H.; Alotaibi, N.H.; Alzarea, A.I.; Tanveer, N.; Khan, T.M. Multilevel Engagements of Pharmacists During the COVID-19 Pandemic: The Way Forward. Front. Public Heal. 2020, 8, 561924. [Google Scholar] [CrossRef]
- Mediratta, R.P.; Rizal, R.; Xie, J.; Kambhampati, S.; Hills-Evans, K.; Montacute, T.; Zhang, M.; Zaw, C.; He, J.; Sanchez, M.; et al. Galvanizing medical students in the administration of influenza vaccines: The Stanford Flu Crew. Adv. Med. Educ. Pr. 2015, 6, 471–477. [Google Scholar] [CrossRef][Green Version]
- Hannings, A.N.; Duke, L.J.; Logan, L.D.; Upchurch, B.L.; Kearney, J.C.; Darley, A.; Welch, L.H.; Brooks, K.L.; McElhannon, M.B. Patient perceptions of student pharmacist–run mobile influenza vaccination clinics. J. Am. Pharm. Assoc. 2018, 59, 228–231.e1. [Google Scholar] [CrossRef]
- Brown, S.H.; Fisher, E.L.; Taylor, A.Q.; Neuzil, K.E.; Trump, S.W.; Sack, D.E.; Fricker, G.P.; Miller, R.F. Influenza vaccine community outreach: Leveraging an interprofessional healthcare student workforce to immunize marginalized populations. Prev. Med. 2021, 147, 106460. [Google Scholar] [CrossRef] [PubMed]
- Hays, A.; Schriever, C.; Rudzinski, J.; Lynch, J.L.; Genrich, E.; Schriever, A. Fostering Interprofessional Education Through a Multidisciplinary, Community-Based Pandemic Mass Vaccination Exercise. Am. J. Public Heal. 2018, 108, 358–360. [Google Scholar] [CrossRef] [PubMed]
- Eldred, S.V.; Hamid, H.S.; Snider, J.C.; Weinberg, S.H.; Speck, N.; Reed, B.D.; Riley, M. A Medical Student-Driven “Vaccine Blitz” at a School-Based Health Center as an Effective Way to Improve Adolescent Vaccination Rates. Fam. Med. 2015, 47, 546–548. [Google Scholar] [PubMed]
| Student Vaccinator Characteristic | % (N = 128) |
|---|---|
| Program | |
| MD | 68 (87) |
| MD-PhD | 32 (41) |
| Class Year | |
| 2 | 13 (16) |
| 3 | 34 (44) |
| 4+ | 53 (68) |
| Patient Demographic | % (N = 14,293) |
|---|---|
| Age | |
| <18 | 17 (2451) |
| 18–24 | 12 (1683) |
| 25–34 | 18 (2548) |
| 35–44 | 18 (2555) |
| 45–54 | 15 (2147) |
| 55–64 | 13 (1796) |
| 65+ | 7 (1057) |
| Sex at Birth | |
| Female | 50 (7145) |
| Male | 48 (6822) |
| Race/Ethnicity | |
| White | 10 (1390) |
| Black | 30 (4345) |
| Asian | 10 (1365) |
| Hispanic | 39 (5557) |
| Other | 9 (1287) |
| Program Evaluation Question | % (N = 50) |
|---|---|
| Did you feel you had adequate training and preparation to participate? | |
| Yes | 100% (49) |
| No | 0% (0) |
| Did you feel protected wearing appropriate PPE and adhering to NYS guidelines? | |
| Yes | 100% (50) |
| No | 0% (0) |
| How comfortable did you feel with IM injections prior to training? | |
| Not at all or somewhat comfortable | 98% (49) |
| Comfortable or very comfortable | 2% (1) |
| How comfortable did you feel with IM injections post-training? | |
| Not at all or somewhat comfortable | 24% (12) |
| Comfortable or very comfortable | 76% (38) |
| How comfortable do you feel with IM injections now [i.e., post vaccination program)? | |
| Not at all or somewhat comfortable | 0% (0) |
| Comfortable or very comfortable | 100% (49) |
| How comfortable did you feel talking to patients about the COVID-19 vaccine prior to volunteering? | |
| Not at all or somewhat comfortable | 70% (35) |
| Comfortable or very comfortable | 30% (15) |
| How comfortable do you feel talking to patients about the COVID-19 vaccine after volunteering? | |
| Not at all or somewhat comfortable | 0% (0) |
| Comfortable or very comfortable | 100% (50) |
| Would you sign up for similar volunteer efforts in the future? | |
| Yes | 100% (50) |
| No | 0% (0) |
| Program Evaluation Question |
|---|
Why did you volunteer?
|
| How did this add to your professional development? |
|
| How did this experience add to your medical education? |
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Griswold, A.R.; Klein, J.; Dusaj, N.; Zhu, J.; Keeler, A.; Abramson, E.L.; Gurvitch, D. Students as Community Vaccinators: Implementation of A Service-Learning COVID-19 Vaccination Program. Vaccines 2022, 10, 1058. https://doi.org/10.3390/vaccines10071058
Griswold AR, Klein J, Dusaj N, Zhu J, Keeler A, Abramson EL, Gurvitch D. Students as Community Vaccinators: Implementation of A Service-Learning COVID-19 Vaccination Program. Vaccines. 2022; 10(7):1058. https://doi.org/10.3390/vaccines10071058
Chicago/Turabian StyleGriswold, Andrew R., Julia Klein, Neville Dusaj, Jeff Zhu, Allegra Keeler, Erika L. Abramson, and Dana Gurvitch. 2022. "Students as Community Vaccinators: Implementation of A Service-Learning COVID-19 Vaccination Program" Vaccines 10, no. 7: 1058. https://doi.org/10.3390/vaccines10071058
APA StyleGriswold, A. R., Klein, J., Dusaj, N., Zhu, J., Keeler, A., Abramson, E. L., & Gurvitch, D. (2022). Students as Community Vaccinators: Implementation of A Service-Learning COVID-19 Vaccination Program. Vaccines, 10(7), 1058. https://doi.org/10.3390/vaccines10071058