HPV Vaccination and Cervical Cancer Screening: Assessing Awareness, Attitudes, and Adherence in Detained Women
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Population Recruitment and Data Collection
2.3. Survey Instrument
2.4. Statistical Analysis
2.5. Pilot Study and Ethical Statement
3. Results
3.1. Socio-Demographic, Detention, and Anamnestic Characteristics of the Study Population
3.2. Knowledge about HPV Infection, Cervical Cancer, and Related Prevention
3.3. Attitudes towards HPV Infection, Cervical Cancer, and Related Prevention
3.4. Preventive Behavior towards HPV Infection and Cervical Cancer
3.5. Sources of Information
4. Discussions
4.1. Knowledge and Attitudes about HPV Infection, Cervical Cancer, and Related Prevention
4.2. Preventive Behavior towards HPV Infection and Cervical Cancer
4.3. Public Health Implications of the Study
4.4. Limitations of the Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kombe, A.J.K.; Li, B.; Zahid, A.; Mengist, H.M.; Bounda, G.A.; Zhou, Y.; Jin, T. Epidemiology and burden of human papillomavirus and related diseases, molecular pathogenesis, and vaccine evaluation. Front. Public Health 2021, 8, 2028. [Google Scholar] [CrossRef]
- Binswanger, I.A.; Mueller, S.; Clark, C.B.; Cropsey, K.L. Risk factors for cervical cancer in criminal justice settings. J. Womens Health 2011, 20, 1839–1845. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Escobar, N.; Plugge, E. Prevalence of human papillomavirus infection, cervical intraepithelial neoplasia and cervical cancer in imprisoned women worldwide: A systematic review and meta-analysis. J. Epidemiol. Community Health 2020, 74, 95–102. [Google Scholar] [CrossRef] [PubMed]
- Niccolai, L.M.; Julian, P.J.; Meek, J.I.; McBride, V.; Hadler, J.L.; Sosa, L.E. Declining rates of high-grade cervical lesions in young women in Connecticut, 2008–2011. Cancer Epidemiol. Biomark. Prev. 2013, 22, 1446–1450. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Markowitz, L.E.; Dunne, E.F.; Saraiya, M.; Chesson, H.W.; Curtis, C.R.; Gee, J.; Bocchini, J.A., Jr.; Unger, E.R. Human papillomavirus vaccination: Recommendations of the Advisory Committee on Immunization Practices (ACIP). Morb. Mortal. Wkly. Rep. Recomm. Rep. 2014, 63, 1–30. [Google Scholar]
- Pileggi, C.; Flotta, D.; Bianco, A.; Nobile, C.G.; Pavia, M. Is HPV DNA testing specificity comparable to that of cytological testing in primary cervical cancer screening? Results of a meta-analysis of randomized controlled trials. Int. J. Cancer 2014, 135, 166–177. [Google Scholar] [CrossRef]
- Ministero della Salute. Piano Nazionale Prevenzione Vaccinale 2017–2019. Available online: https://www.salute.gov.it/portale/vaccinazioni/dettaglioContenutiVaccinazioni.jsp?lingua=italiano&id=4828&area=vaccinazioni&menu=vuoto (accessed on 2 August 2022).
- Ministero della Salute. Screening Oncologici. Available online: https://www.salute.gov.it/portale/donna/dettaglioContenutiDonna.jsp?lingua=italiano&id=4511&area=Salute%20donna&menu=prevenzione#:~:text=Screening%20per%20il%20tumore%20del%20collo%20dell’utero&text=I%20test%20per%20lo%20screening,i%2025%20e%20i%2064%20anni (accessed on 2 August 2022).
- World Health Organization. Declaration on Prison Health as Part of Public Health. Moscow, 2003. Available online: https://www.euro.who.int/__data/assets/pdf_file/0007/98971/E94242.pdf (accessed on 2 August 2022).
- World Health Organization. Prisons and Health. Available online: https://www.euro.who.int/__data/assets/pdf_file/0005/249188/Prisons-and-Health.pdf (accessed on 2 August 2022).
- Olukotun, O.; Williams, J.S.; Zhou, Z.; Akinboboye, O.; Egede, L.E. The association between history of incarceration and heart disease: Adults from the 1979 National Longitudinal Survey of Youth. Health Place 2022, 75, 102808. [Google Scholar] [CrossRef]
- Fovet, T.; Plancke, L.; Amariei, A.; Benradia, I.; Carton, F.; Sy, A.; Kyheng, M.; Tasniere, G.; Amad, A.; Danel, T.; et al. Mental disorders on admission to jail: A study of prevalence and a comparison with a community sample in the north of France. Eur. Psychiatry 2020, 63, e43. [Google Scholar] [CrossRef]
- Stürup-Toft, S.; O’Moore, E.J.; Plugge, E.H. Looking behind the bars: Emerging health issues for people in prison. Br. Med. Bull. 2018, 125, 15–23. [Google Scholar] [CrossRef] [Green Version]
- Dumont, D.M.; Brockmann, B.; Dickman, S.; Alexander, N.; Rich, J.D. Public health and the epidemic of incarceration. Annu. Rev. Public Health 2012, 33, 325–339. [Google Scholar] [CrossRef] [Green Version]
- Associazione Antigone. XVIII Rapporto sulle Condizioni di Detenzione. Available online: https://www.rapportoantigone.it/ (accessed on 2 August 2022).
- Massoglia, M.; Pridemore, W.A. Incarceration and health. Annu. Rev. Sociol. 2015, 41, 291–310. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. The WHO Prison Health Framework: A Framework for Assessment of Prison Health System Performance; WHO Regional Office for Europe: Copenhagen, Denmark, 2021; Available online: https://www.who.int/europe/publications/i/item/9789289055482 (accessed on 2 August 2022).
- Madeddu, G.; Vroling, H.; Oordt-Speets, A.; Babudieri, S.; O’Moore, É.; Noordegraaf, M.V.; Monarca, R.; Lopalco, P.L.; Hedrich, D.; Tavoschi, L. Vaccinations in prison settings: A systematic review to assess the situation in EU/EEA countries and in other high income countries. Vaccine 2019, 37, 4906–4919. [Google Scholar] [CrossRef] [PubMed]
- Vicente-Alcalde, N.; Ruescas-Escolano, E.; Harboe, Z.B.; Tuells, J. Vaccination coverage among prisoners: A systematic review. Int. J. Environ. Res. Public Health 2020, 17, 7589. [Google Scholar] [CrossRef] [PubMed]
- Salyer, C.; Lipnicky, A.; Bagwell-Gray, M.; Lorvick, J.; Cropsey, K.; Ramaswamy, M. Abnormal pap follow-up among criminal-legal involved women in three U.S. cities. Int. J. Environ. Res. Public Health 2021, 18, 6556. [Google Scholar] [CrossRef] [PubMed]
- Di Giuseppe, G.; Lanzano, R.; Silvestro, A.; Napolitano, F.; Pavia, M. Pattern and appropriateness of antimicrobial prescriptions for upper respiratory tract and dental infections in male prisoners in Italy. Antibiotics 2021, 10, 1419. [Google Scholar] [CrossRef]
- Di Giuseppe, G.; Pelullo, C.P.; Lanzano, R.; Lombardi, C.; Nese, G.; Pavia, M. COVID-19 Vaccination uptake and related determinants in detained subjects in Italy. Vaccines 2022, 10, 673. [Google Scholar] [CrossRef]
- Di Giuseppe, G.; Pelullo, C.P.; Lanzano, R.; Napolitano, F.; Pavia, M. Knowledge, attitudes, and behavior of incarcerated people regarding COVID-19 and related vaccination: A survey in Italy. Sci. Rep. 2022, 12, 960. [Google Scholar] [CrossRef]
- Lanzano, R.; Pelullo, C.P.; Della Polla, G.; Di Giuseppe, G.; Pavia, M. Assessment of perceived health status and access to healthcare services of male detained subjects: A survey in Italy. Public Health, 2022; under review. [Google Scholar]
- Kelly, P.J.; Allison, M.; Ramaswamy, M. Cervical cancer screening among incarcerated women. PLoS ONE 2018, 13, e0199220. [Google Scholar] [CrossRef]
- Ramaswamy, M.; Diaz, F.; Pankey, T.; Hunt, S.L.; Parl, A.; Kelly, P.J. Correlates of preincarceration health care use among women and men in jail. J. Correct. Health Care 2015, 21, 286–297. [Google Scholar] [CrossRef] [Green Version]
- Allison, M.; Musser, B.; Satterwhite, C.; Ault, K.; Kelly, P.; Ramaswamy, M. Human papillomavirus vaccine knowledge and intention among adult inmates in Kansas, 2016–2017. Am. J. Public Health 2018, 108, 1000–1002. [Google Scholar] [CrossRef]
- Acheampong, L.K.; Effah, K.; Amuah, J.E.; Tekpor, E.; Wormenor, C.M.; Gedzah, I.; Kemawor, S.; Kachana, A.C.; Danso, P.A.; Essel, N.O.M.; et al. Determining the prevalence of high-risk human papillomavirus infection using a novel cervical precancer screening approach in incarcerated women at the Nsawam Medium Security Prison, Ghana. Ecancermedicalscience 2021, 15, 1248. [Google Scholar] [CrossRef]
- Pelullo, C.P.; Cantore, F.; Lisciotto, A.; Di Giuseppe, G.; Pavia, M. Organized breast and cervical cancer screening: Attendance and determinants in Southern Italy. Cancers 2021, 13, 1578. [Google Scholar] [CrossRef] [PubMed]
- Mascaro, V.; Pileggi, C.; Currà, A.; Bianco, A.; Pavia, M. HPV vaccination coverage and willingness to be vaccinated among 18–30 year-old students in Italy. Vaccine 2019, 37, 3310–3316. [Google Scholar] [CrossRef] [PubMed]
- Fujii, H.; Nishimoto, N.; Yamaguchi, S.; Kurai, O.; Miyano, M.; Ueda, W.; Oba, H.; Aoki, T.; Kawada, N.; Okawa, K. The Alcohol Use Disorders Identification Test for Consumption (AUDIT-C) is more useful than pre-existing laboratory tests for predicting hazardous drinking: A cross-sectional study. BMC Public Health 2016, 16, 379. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bradley, K.A.; Rubinsky, A.D.; Lapham, G.T.; Berger, D.; Bryson, C.; Achtmeyer, C.; Hawkins, E.J.; Chavez, L.J.; Williams, E.C.; Kivlahan, D.R. Predictive validity of clinical AUDIT-C alcohol screening scores and changes in scores for three objective alcohol-related outcomes in a Veterans Affairs population. Addiction 2016, 111, 1975–1984. [Google Scholar] [CrossRef] [PubMed]
- Dawson, D.A.; Grant, B.F.; Stinson, F.S.; Zhou, Y. Effectiveness of the derived Alcohol Use Disorders Identification Test (AUDIT-C) in screening for alcohol use disorders and risk drinking in the US general population. Alcohol Clin. Exp. Res. 2005, 29, 844–854. [Google Scholar] [CrossRef] [PubMed]
- Italian Council of Ministers. Legislative Decree N.81/2008. Testo Unico sulla Salute e Sicurezza sul Lavoro. 2008. Available online: https://www.lavoro.gov.it/documenti-e-norme/studi-e-statistiche/Documents/Testo%20Unico%20sulla%20Salute%20e%20Sicurezza%20sul%20Lavoro/Testo-Unico-81-08-Edizione-Giugno%202016.pdf (accessed on 5 July 2022).
- Stata Corporation. Stata Reference Manual Release 15.1; Stata Corporation: College Station, TX, USA, 2017. [Google Scholar]
- Moore, A.; Cox-Martin, M.; Dempsey, A.F.; Berenbaum Szanton, K.; Binswanger, I.A. HPV Vaccination in correctional care: Knowledge, attitudes, and barriers among incarcerated women. J. Correct. Health Care 2019, 25, 219–230. [Google Scholar] [CrossRef]
- Pankey, T.; Ramaswamy, M. Incarcerated women’s HPV awareness, beliefs, and experiences. Int. J. Prison Health 2015, 11, 49–58. [Google Scholar] [CrossRef] [Green Version]
- Ramaswamy, M.; Simmons, R.; Kelly, P.J. The development of a brief jail-based cervical health promotion intervention. Health Promot. Pract. 2015, 16, 432–442. [Google Scholar] [CrossRef]
- Roberson, M.L.; McGee-Avila, J.K. Justice-involved women and cervical cancer disparities: Issues of surveillance, education, and policy. J. Correct. Health Care 2021, 27, 205–209. [Google Scholar] [CrossRef]
- Brousseau, E.C.; Ahn, S.; Matteson, K.A. Cervical cancer screening access, outcomes, and prevalence of dysplasia in correctional facilities: A systematic review. J. Womens Health 2019, 28, 1661–1669. [Google Scholar] [CrossRef] [PubMed]
- Ramaswamy, M.; Kelly, P.J.; Koblitz, A.; Kimminau, K.S.; Engelman, K.K. Understanding the role of violence in incarcerated women’s cervical cancer screening and history. Women Health 2011, 51, 423–441. [Google Scholar] [CrossRef] [PubMed]
- Bianco, A.; Larosa, E.; Pileggi, C.; Nobile, G.A.; Pavia, M. Cervical and breast cancer screening participation and utilisation of maternal health services: A cross-sectional study among immigrant women in Southern Italy. BMJ Open 2017, 10, e016306. [Google Scholar] [CrossRef] [Green Version]
- Vaccarella, S.; Lortet-Tieulent, J.; Saracci, R.; Conway, D.I.; Straif, K.; Wild, C.P. (Eds.) Reducing Social Inequalities in Cancer: Evidence and Priorities for Research (IARC Scientific Publication No. 168); International Agency for Research on Cancer: Lyon, France, 2019; Available online: http://publications.iarc.fr/580 (accessed on 5 July 2022).
- Gabutti, G.; d’Anchera, E.; De Motoli, F.; Savio, M.; Stefanati, A. Human papilloma virus vaccination: Focus on the italian situation. Vaccines 2021, 9, 1374. [Google Scholar] [CrossRef] [PubMed]
- Nijhawan, A.E.; Salloway, R.; Nunn, A.S.; Poshkus, M.; Clarke, J.G. Preventive healthcare for underserved women: Results of a prison survey. J. Womens Health 2010, 19, 17–22. [Google Scholar] [CrossRef]
- Binswanger, I.A.; White, M.C.; Pérez-Stable, E.J.; Goldenson, J.; Tulsky, J.P. Cancer screening among jail inmates: Frequency, knowledge, and willingness. Am. J. Public Health 2005, 95, 1781–1787. [Google Scholar] [CrossRef]
- Emerson, A.; Allison, M.; Kelly, P.J.; Ramaswamy, M. Barriers and facilitators of implementing a collaborative HPV vaccine program in an incarcerated population: A case study. Vaccine 2020, 38, 2566–2571. [Google Scholar] [CrossRef]
- Emerson, A.M.; Smith, S.; Lee, J.; Kelly, P.J.; Ramaswamy, M. Effectiveness of a Kansas City, jail-based intervention to improve cervical health literacy and screening, one-year post-intervention. Am. J. Health Promot. 2020, 34, 87–90. [Google Scholar] [CrossRef]
- Plugge, E.; Fitzpatrick, R. Factors affecting cervical screening uptake in prisoners. J. Med. Screen. 2004, 11, 48–49. [Google Scholar] [CrossRef]
- Kouyoumdjian, F.G.; McConnon, A.; Herrington, E.R.S.; Fung, K.; Lofters, A.; Hwang, S.W. Cervical cancer screening access for women who experience imprisonment in Ontario, Canada. JAMA Netw. Open 2018, 1, e185637. [Google Scholar] [CrossRef] [Green Version]
- Da Silva, E.R.P.; de Souza, A.S.; de Souza, T.G.B.; Tsuha, D.H.; Barbieri, A.R. Screening for cervical cancer in imprisoned women in Brazil. PLoS ONE 2017, 12, e0187873. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ruiz-Maza, J.C.; Soto-Azpilcueta, R.A.; Sanchez-Salvatierra, J.; Torres-Prado, Y. Cytological screening for cervical cancer and associated factors in the penitentiary population of Peru. Rev. Esp. Sanid. Penit. 2018, 20, 103–110. [Google Scholar] [PubMed]
- Martin, R.E.; Hislop, T.G.; Grams, G.D.; Calam, B.; Jones, E.; Moravan, V. Evaluation of a cervical cancer screening intervention for prison inmates. Can. J. Public Health 2004, 95, 285–289. [Google Scholar] [CrossRef]
| Knowledge Items | Yes | Do Not Know | No |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| HPV is a sexually transmitted disease (STD) | 88 (41.1) | 104 (48.6) | 22 (10.3) |
| HPV can cause: | |||
| Abnormal PAP smears | 85 (39.7) | 117 (54.7) | 12 (5.6) |
| Cervical cancer | 78 (36.4) | 118 (55.1) | 18 (8.5) |
| Genital warts | 63 (29.4) | 134 (62.6) | 17 (8) |
| Bladder infection | 66 (30.8) | 131 (61.2) | 17 (8) |
| Skin cancer | 19 (8.9) | 147 (68.7) | 48 (22.4) |
| Oral cancer | 36 (16.8) | 140 (65.4) | 38 (17.8) |
| HPV vaccination is effective at preventing genital warts | 84 (39.2) | 110 (51.4) | 20 (9.4) |
| HPV vaccination is effective in preventing cervical cancer | 98 (45.8) | 100 (46.7) | 16 (7.5) |
| HPV vaccination prevents other STDs such as HIV, chlamydia, and others | 28 (13.1) | 153 (71.5) | 33 (15.4) |
| HPV vaccination is effective in women who are already sexually active | 41 (19.2) | 153 (71.5) | 20 (9.3) |
| HPV vaccination is effective in women who have already been exposed to HPV | 23 (10.8) | 161 (75.2) | 30 (14) |
| HPV infection usually goes away in its own | 168 (78.5) | 45 (21.1) | 1 (0.4) |
| Strongly Agree or Agree | Uncertain | Strongly Disagree or Disagree | |
|---|---|---|---|
| Items | n (%) | n (%) | n (%) |
| I will get HPV infection during my life | 34 (15.9) | 62 (28.9) | 118 (55.2) |
| My lifestyle increases the risk to get HPV infection | 20 (9.3) | 56 (26.1) | 138 (64.6) |
| I have the same risk of HPV infection as women who have never been incarcerated | 57 (26.7) | 79 (36.9) | 78 (36.4) |
| I have the same risk of cervical cancer as women who have never been incarcerated | 73 (34.1) | 77 (36) | 64 (29.9) |
| HPV infection transmission is easy through sexual partners | 153 (71.5) | 50 (23.4) | 11 (5.1) |
| It is embarrassing to have genital warts | 152 (71) | 54 (25.3) | 8 (3.7) |
| Being diagnosed with cervical cancer would have major negative consequences on my life | 162 (75.7) | 45 (21) | 7 (3.3) |
| Cervical cancer can cause death | 147 (68.7) | 56 (26.1) | 11 (5.2) |
| Generally, vaccines are more dangerous than safe | 50 (23.4) | 52 (24.3) | 112 (52.3) |
| HPV vaccination is safe | 79 (36.9) | 112 (52.3) | 23 (10.8) |
| HPV vaccination can cause serious side effects | 20 (9.3) | 153 (71.5) | 41 (19.2) |
| HPV vaccination is not necessary if I get regular PAP test | 73 (34.1) | 99 (46.2) | 42 (19.7) |
| HPV vaccination can save my life * | 36 (46.8) | 28 (36.3) | 13 (16.9) |
| Items | n (%) |
|---|---|
| Have you ever got HPV vaccination? 1 | |
| Yes | 0 (0) |
| No | 77 (100) |
| Have you ever received a diagnosis of HPV infection? | |
| Yes | 8 (3.3) |
| No | 206 (96.7) |
| Have you ever had a PAP smear included in a screening program? 2 | |
| Yes | 28 (13.5) |
| No | 173 (83.2) |
| Do not know | 7 (3.3) |
| Where did you take a PAP smear? 3 | |
| In the community, before incarceration | 11 (39.3) |
| In prison | 13 (46.4) |
| Both | 4 (14.3) |
| Have you ever had an abnormal PAP smear? 3 | |
| Yes | 4 (14.3) |
| No | 23 (82.1) |
| Do not know | 1 (3.6) |
| After the abnormal PAP smear test, what did you do? 4 | |
| Colposcopy/biopsy | 3 (75) |
| I took another PAP smear | 1 (25) |
| Have you ever had a diagnosis of cervical cancer? | |
| Yes | 4 (1.8) |
| No | 210 (98.2) |
| Did you follow (are you following) a specific treatment for the cervical cancer? 5 | |
| Surgery | 3 (75) |
| Chemotherapy and radiotherapy | 1 (25) |
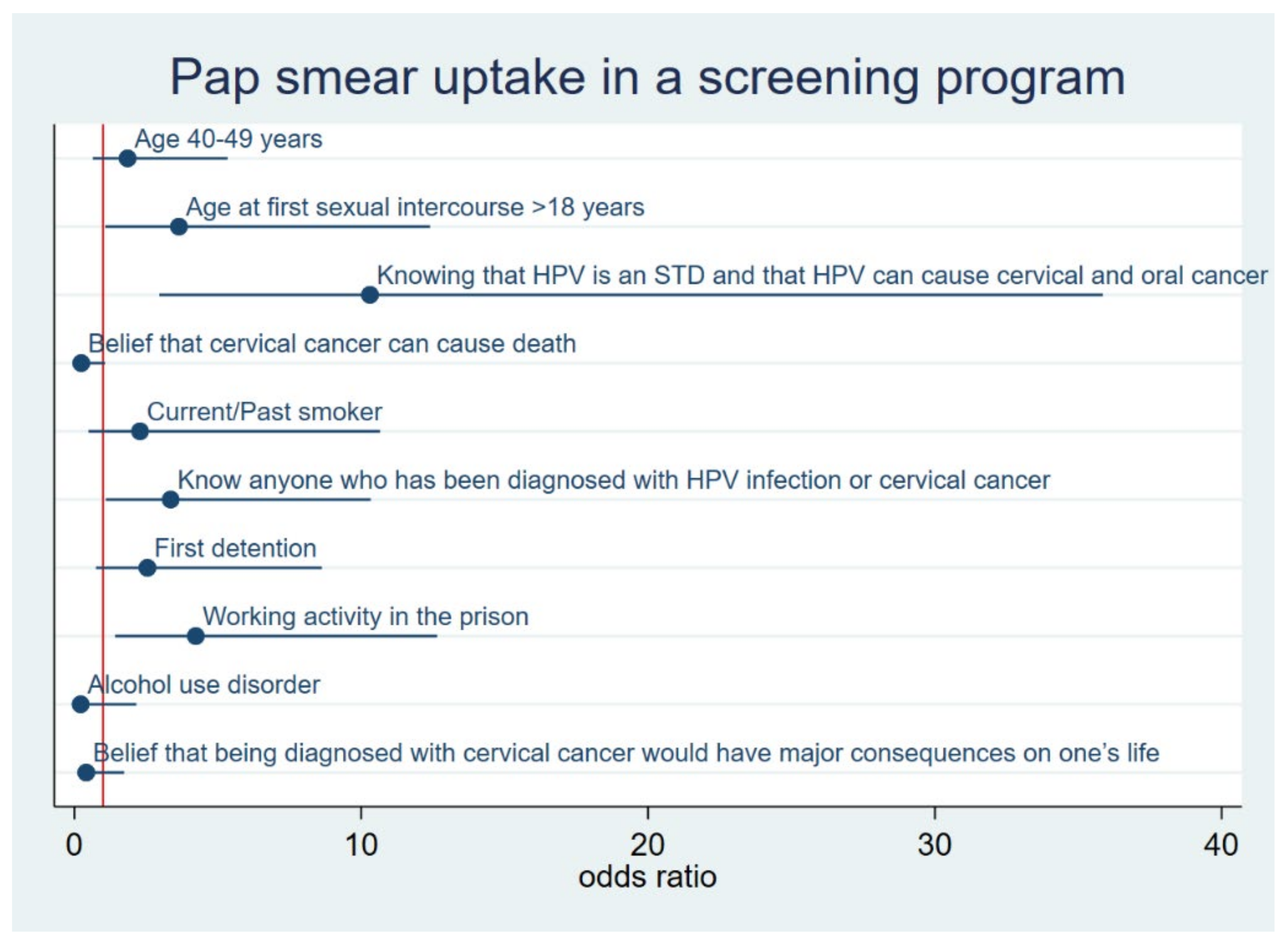
| ^ Model. Pap Smear Uptake in a Screening Program | Total | Pap Smear Uptake | |||
|---|---|---|---|---|---|
| OR | 95% CI ° | p | n | n (%) | |
| Age, years | |||||
| 25–39 | 1 * | 65 | 6 (9.2) | ||
| 40–49 | 1.855 | 0.644–5.341 | 0.252 | 70 | 12 (17.1) |
| ≥50 | Backward elimination | 66 | 8 (12.1) | ||
| First detention | |||||
| No | 1 * | 67 | 8 (11.9) | ||
| Yes | 2.546 | 0.751–8.629 | 0.133 | 134 | 20 (14.9) |
| Working activity in the prison | |||||
| No | 1 * | 114 | 9 (7.9%) | ||
| Yes | 4.233 | 1.417–12.648 | 0.010 | 87 | 19 (21.8) |
| Smoking habit | |||||
| Never smoker | 1 * | 33 | 4 (12.1) | ||
| Current/past smoker | 2.288 | 0.491–10.655 | 0.291 | 168 | 24 (14.3) |
| Alcohol use disorder | |||||
| No | 1 * | 176 | 26 (14.8) | ||
| Yes | 0.218 | 0.022–2.160 | 0.193 | 25 | 2 (8) |
| Age at first sexual intercourse, years | |||||
| ≤15 | 1 * | 66 | 8 (12.1) | ||
| 16–18 | Backward elimination | 96 | 10 (10.4) | ||
| ≥19 | 3.645 | 1.071–12.397 | 0.038 | 39 | 8 (20.5) |
| Know anyone who has been diagnosed with HPV infection or cervical cancer | |||||
| No | 1 * | 153 | 16 (10.4) | ||
| Yes | 3.358 | 1.091–10.331 | 0.035 | 48 | 12 (25) |
| Knowing that HPV is an STD and that HPV can cause cervical and oral cancer | |||||
| No | 1 * | 177 | 19 (10.7) | ||
| Yes | 10.305 | 2.962–35.851 | <0.001 | 24 | 9 (37.5) |
| Belief that being diagnosed with cervical cancer would have major consequences on one’s life | |||||
| No | 1 * | 50 | 13 (26) | ||
| Yes | 0.413 | 0.098–1.734 | 0.228 | 151 | 15 (9.9) |
| Belief that cervical cancer can cause death | |||||
| No | 1 * | 62 | 16 (25.8) | ||
| Yes | 0.239 | 0.053–1.070 | 0.061 | 139 | 12 (8.6) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Di Giuseppe, G.; Folcarelli, L.; Lanzano, R.; Napolitano, F.; Pavia, M. HPV Vaccination and Cervical Cancer Screening: Assessing Awareness, Attitudes, and Adherence in Detained Women. Vaccines 2022, 10, 1280. https://doi.org/10.3390/vaccines10081280
Di Giuseppe G, Folcarelli L, Lanzano R, Napolitano F, Pavia M. HPV Vaccination and Cervical Cancer Screening: Assessing Awareness, Attitudes, and Adherence in Detained Women. Vaccines. 2022; 10(8):1280. https://doi.org/10.3390/vaccines10081280
Chicago/Turabian StyleDi Giuseppe, Gabriella, Lucio Folcarelli, Raffaele Lanzano, Francesco Napolitano, and Maria Pavia. 2022. "HPV Vaccination and Cervical Cancer Screening: Assessing Awareness, Attitudes, and Adherence in Detained Women" Vaccines 10, no. 8: 1280. https://doi.org/10.3390/vaccines10081280
APA StyleDi Giuseppe, G., Folcarelli, L., Lanzano, R., Napolitano, F., & Pavia, M. (2022). HPV Vaccination and Cervical Cancer Screening: Assessing Awareness, Attitudes, and Adherence in Detained Women. Vaccines, 10(8), 1280. https://doi.org/10.3390/vaccines10081280






