Immunogenicity and Protective Efficacy of a Recombinant Pichinde Viral-Vectored Vaccine Expressing Influenza Virus Hemagglutinin Antigen in Pigs
Abstract
:1. Introduction
2. Materials and Methods
2.1. Cells, Reagents, and Viruses
2.2. Experimental Vaccines
2.3. Antigen Expression In Vitro
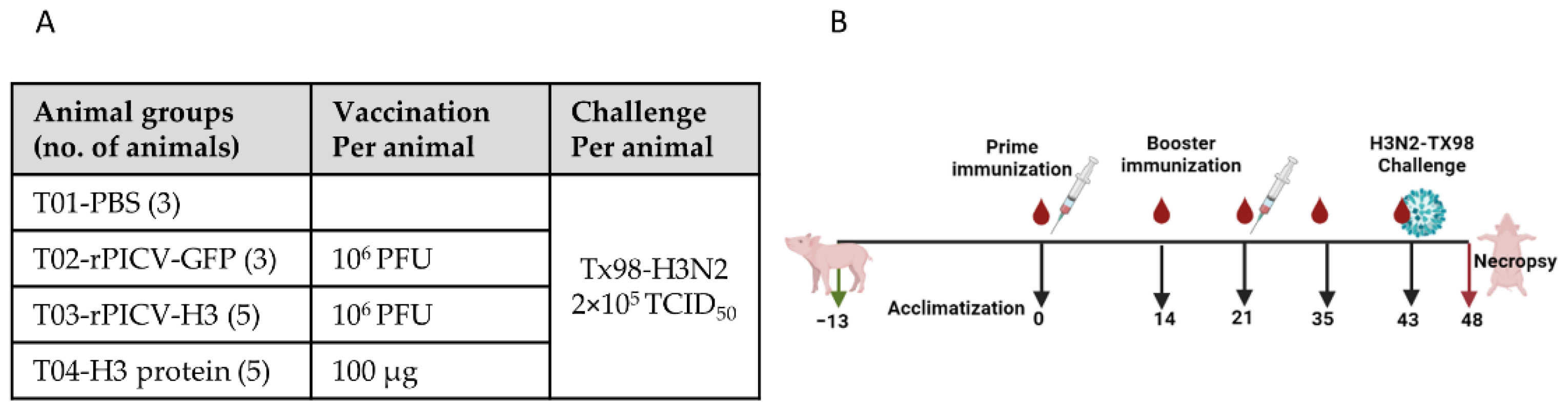
2.4. Animal Experiment
2.5. Serological Assay
2.6. Quantification of Viral Load
2.7. Lung Pathological Analysis
2.8. Statistical Analysis
3. Results
3.1. rPICV Vector Expressed High Levels of Gene-of-Insterest in Pig Cells
3.2. Pigs Inoculated with rPICV-GFP Do Not Transmit the Virus to Contact Pigs
3.3. Pigs Immunized with rPICV-H3 or H3-Protein Subunit Vaccines Mounted a Robust Antibody Response
3.4. Pigs Immunized with rPICV-H3 and H3-Protein Vaccines Were Protected against Challenge with the Homologous H3N2 IAV-S Strain
3.5. Pigs Immunized with H3-Protein Vaccine or rPICV-H3 Vectored Vaccine Tested Negative for IAV-S NP Antibodies by a Commercial ELISA Kit
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Rajao, D.S.; Anderson, T.K.; Gauger, P.C.; Vincent, A.L. Pathogenesis and Vaccination of Influenza A Virus in Swine. Curr. Top Microbiol. Immunol. 2014, 385, 307–326. [Google Scholar] [PubMed]
- Haden, C.; Painter, T.; Fangman, T.; Holtkamp, D.J. Assessing Production Parameters and Economic Impact of Swine Influenza, PRRS and Mycoplasma hyopneumoniae on Finishing Pigs in a Large Production System. In Proceedings of the American Association of Swine Veterinarians Annual Meeting, Denver, CO, USA, 10–13 March 2012; Available online: https://vetmed.iastate.edu/sites/default/files/vdpam/Cara%20Haden%20AASV%20Abstract.pdf (accessed on 14 July 2022).
- Vincent, A.L.; Lager, K.M.; Anderson, T.K. A Brief Introduction to Influenza A Virus in Swine. Methods Mol. Biol. 2014, 1161, 243–258. [Google Scholar] [PubMed]
- Anderson, T.K.; Macken, C.A.; Lewis, N.S.; Scheuermann, R.H.; Van Reeth, K.; Brown, I.H.; Swenson, S.L.; Simon, G.; Saito, T.; Berhane, Y.; et al. A Phylogeny-Based Global Nomenclature System and Automated Annotation Tool for H1 Hemagglutinin Genes from Swine Influenza A Viruses. MSphere 2016, 1, e00275-16. [Google Scholar] [CrossRef] [PubMed]
- Bolton, M.J.; Abente, E.J.; Venkatesh, D.; Stratton, J.A.; Zeller, M.; Anderson, T.K.; Lewis, N.S.; Vincent, A.L. Antigenic Evolution of H3N2 Influenza a Viruses in Swine in the United States from 2012 to 2016. Influenza Other Respir. Viruses 2019, 13, 83–90. [Google Scholar] [CrossRef] [PubMed]
- Walia, R.R.; Anderson, T.K.; Vincent, A.L. Regional Patterns of Genetic Diversity in Swine Influenza a Viruses in the United States from 2010 to 2016. Influenza Other Respir. Viruses 2019, 13, 262–273. [Google Scholar] [CrossRef] [PubMed]
- Souza, C.K.; Anderson, T.K.; Chang, J.; Venkatesh, D.; Lewis, N.S.; Pekosz, A.; Shaw-Saliba, K.; Rothman, R.E.; Chen, K.F.; Vincent, A.L. Antigenic Distance between North American Swine and Human Seasonal H3N2 Influenza A Viruses as an Indication of Zoonotic Risk to Humans. J. Virol. 2022, 96, e0137421. [Google Scholar] [CrossRef]
- Zeller, M.A.; Li, G.; Harmon, K.M.; Zhang, J.; Vincent, A.L.; Anderson, T.K.; Gauger, P.C. Complete Genome Sequences of Two Novel Human-Like H3N2 Influenza A Viruses, A/swine/Oklahoma/65980/2017 (H3N2) and A/Swine/Oklahoma/65260/2017 (H3N2), Detected in Swine in the United States. Microbiol. Resour. Announc. 2018, 7, e01203-18. [Google Scholar] [CrossRef]
- Anderson, T.K.; Nelson, M.I.; Kitikoon, P.; Swenson, S.L.; Korslund, J.A.; Vincent, A.L. Population dynamics of cocirculating swine influenza A viruses in the United States from 2009 to 2012. Influenza Other Respir. Viruses 2013, 7, 42–51. [Google Scholar] [CrossRef]
- Steel, J.; Lowen, A.C. Influenza A Virus Reassortment. In Influenza Pathogenesis and Control—Volume I; Compans, R., Oldstone, M., Eds.; Current Topics in Microbiology and Immunology; Springer: Cham, Swizterland, 2014; Volume 385, pp. 377–401. [Google Scholar]
- Ma, W. Swine influenza virus: Current status and challenge. Virus Res. 2020, 288, 198118. [Google Scholar] [CrossRef]
- Chen, J.; Wang, J.; Zhang, J.; Ly, H. Advances in Development and Application of Influenza Vaccines. Front. Immunol. 2021, 12, 711997. [Google Scholar] [CrossRef]
- Khatri, M.; Dwivedi, V.; Krakowka, S.; Manickam, C.; Ali, A.; Wang, L.; Qin, Z.; Renukaradhya, G.J.; Lee, C.W. Swine influenza H1N1 virus induces acute inflammatory immune responses in pig lungs: A potential animal model for human H1N1 influenza virus. J. Virol. 2010, 84, 11210–11218. [Google Scholar] [CrossRef] [PubMed]
- Sandbulte, M.R.; Spickler, A.R.; Zaabel, P.K.; Roth, J.A. Optimal Use of Vaccines for Control of Influenza A Virus in Swine. Vaccines 2015, 3, 22–73. [Google Scholar] [CrossRef] [PubMed]
- Vincent, A.L.; Ciacci-Zanella, J.R.; Lorusso, A.; Gauger, P.C.; Zanella, E.L.; Kehrli, M.E.; Janke, B.H.; Lager, K.M. Efficacy of inactivated swine influenza virus vaccines against the 2009 A/H1N1 influenza virus in pigs. Vaccine 2010, 28, 2782–2787. [Google Scholar] [CrossRef] [PubMed]
- Vincent, A.L.; Lager, K.M.; Janke, B.H.; Gramer, M.R.; Richt, J.A. Failure of protection and enhanced pneumonia with a US H1N2 swine influenza virus in pigs vaccinated with an inactivated classical swine H1N1 vaccine. Vet. Microbiol. 2008, 126, 310–323. [Google Scholar] [CrossRef]
- Kitikoon, P.; Gauger, P.C.; Anderson, T.K.; Culhane, M.R.; Swenson, S.; Loving, C.L.; Perez, D.R.; Vincent, A.L. Swine influenza virus vaccine serologic cross-reactivity to contemporary US swine H3N2 and efficacy in pigs infected with an H3N2 similar to 2011-2012 H3N2v. Influenza Other Respir. Viruses 2013, 7, 32–41. [Google Scholar] [CrossRef]
- Gauger, P.C.; Vincent, A.L.; Loving, C.L.; Lager, K.M.; Janke, B.H.; Kehrli, M.E.; Roth, J.A. Enhanced pneumonia and disease in pigs vaccinated with an inactivated human-like (delta-cluster) H1N2 vaccine and challenged with pandemic 2009 H1N1 influenza virus. Vaccine 2011, 29, 2712–2719. [Google Scholar] [CrossRef]
- Richt, J.A.; Lekcharoensuk, P.; Lager, K.M.; Vincent, A.L.; Loiacono, C.M.; Janke, B.H.; Wu, W.H.; Yoon, K.J.; Webby, R.J.; Solorzano, A.; et al. Vaccination of pigs against swine influenza viruses by using an NS1-truncated modified live-virus vaccine. J. Virol. 2006, 80, 11009–11018. [Google Scholar] [CrossRef]
- Lee, J.; Li, Y.; Li, Y.; Cino-Ozuna, A.G.; Duff, M.; Lang, Y.; Ma, J.; Sunwoo, S.; Richt, J.A.; Ma, W. Bat influenza vectored NS1-truncated live vaccine protects pigs against heterologous virus challenge. Vaccine 2021, 39, 1943–1950. [Google Scholar] [CrossRef]
- Loving, C.L.; Lager, K.M.; Vincent, A.L.; Brockmeier, S.L.; Gauger, P.C.; Anderson, T.K.; Kitikoon, P.; Perez, D.R.; Kehrli, M.E. Efficacy in Pigs of Inactivated and Live Attenuated Influenza Virus Vaccines against Infection and Transmission of an Emerging H3N2 Similar to the 2011-2012 H3N2v. J. Virol. 2013, 87, 9895–9903. [Google Scholar] [CrossRef]
- Gauger, P.C.; Loving, C.L.; Khurana, S.; Lorusso, A.; Perez, D.R.; Kehrli, M.E., Jr.; Roth, J.A.; Golding, H.; Vincent, A.L. Live attenuated influenza A virus vaccine protects against A(H1N1)pdm09 heterologous challenge without vaccine associated enhanced respiratory disease. Virology 2014, 471–473, 93–104. [Google Scholar] [CrossRef] [Green Version]
- Abente, E.J.; Rajao, D.S.; Santos, J.; Kaplan, B.S.; Nicholson, T.L.; Brockmeier, S.L.; Gauger, P.C.; Perez, D.R.; Vincent, A.L. Comparison of Adjuvanted-Whole Inactivated Virus and Live-Attenuated Virus Vaccines against Challenge with Contemporary, Antigenically Distinct H3N2 Influenza A Viruses. J. Virol. 2018, 92, e01323-18. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.; Zeller, M.A.; Li, G.; Harmon, K.M.; Zhang, J.; Hoang, H.; Anderson, T.K.; Vincent, A.L.; Gauger, P.C. Detection of live attenuated influenza vaccine virus and evidence of reassortment in the U.S. swine population. J. Vet. Diagn. Investig. 2020, 32, 301–311. [Google Scholar] [CrossRef] [PubMed]
- Loeffen, W.L.; de Vries, R.P.; Stockhofe, N.; van Zoelen-Bos, D.; Maas, R.; Koch, G.; Moormann, R.J.; Rottier, P.J.; de Haan, C.A. Vaccination with a soluble recombinant hemagglutinin trimer protects pigs against a challenge with pandemic (H1N1) 2009 influenza virus. Vaccine 2011, 29, 1545–1550. [Google Scholar] [CrossRef] [PubMed]
- Vander Veen, R.; Kamrud, K.; Mogler, M.; Loynachan, A.T.; McVicker, J.; Berglund, P.; Owens, G.; Timberlake, S.; Lewis, W.; Smith, J.; et al. Rapid development of an efficacious swine vaccine for novel H1N1. PLoS Curr. 2009, 1, RRN1123. [Google Scholar] [CrossRef]
- Fynan, E.F.; Webster, R.G.; Fuller, D.H.; Haynes, J.R.; Santoro, J.C.; Robinson, H.L. DNA vaccines: Protective immunizations by parenteral, mucosal, and gene-gun inoculations. Proc. Natl. Acad. Sci. USA 1993, 90, 11478–11482. [Google Scholar] [CrossRef] [PubMed]
- Larsen, D.L.; Karasin, A.; Olsen, C.W. Immunization of pigs against influenza virus infection by DNA vaccine priming followed by killed-virus vaccine boosting. Vaccine 2001, 19, 2842–2853. [Google Scholar] [CrossRef]
- Said, A.; Lange, E.; Beer, M.; Damiani, A.; Osterrieder, N. Recombinant equine herpesvirus 1 (EHV-1) vaccine protects pigs against challenge with influenza A(H1N1)pmd09. Virus Res. 2013, 173, 371–376. [Google Scholar] [CrossRef]
- Xu, J.; Huang, D.; Liu, S.; Lin, H.; Zhu, H.; Liu, B.; Lu, C. Immune responses and protection efficacy of a recombinant swinepox virus expressing HA1 against swine H3N2 influenza virus in mice and pigs. Virus Res. 2012, 167, 188–195. [Google Scholar] [CrossRef]
- Wesley, R.D.; Tang, M.; Lager, K.M. Protection of weaned pigs by vaccination with human adenovirus 5 recombinant viruses expressing the hemagglutinin and the nucleoprotein of H3N2 swine influenza virus. Vaccine 2004, 22, 3427–3434. [Google Scholar] [CrossRef]
- Joshi, L.R.; Knudsen, D.; Pineyro, P.; Dhakal, S.; Renukaradhya, G.J.; Diel, D.G. Protective Efficacy of an Orf Virus-Vector Encoding the Hemagglutinin and the Nucleoprotein of Influenza A Virus in Swine. Front. Immunol. 2021, 12, 747574. [Google Scholar] [CrossRef]
- McLay, L.; Liang, Y.; Ly, H. Comparative analysis of disease pathogenesis and molecular mechanisms of New World and Old World arenavirus infections. J. Gen. Virol. 2014, 95 Pt 1, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Dhanwani, R.; Zhou, Y.; Huang, Q.; Verma, V.; Dileepan, M.; Ly, H.; Liang, Y. A Novel Live Pichinde Virus-Based Vaccine Vector Induces Enhanced Humoral and Cellular Immunity after a Booster Dose. J. Virol. 2015, 90, 2551–2560. [Google Scholar] [CrossRef] [PubMed]
- Dhanwani, R.; Ly, H.; Liang, Y. Recombinant Tri-Segmented Pichinde Virus as a Novel Live Viral Vaccine Platform. Methods Mol. Biol. 2017, 1581, 169–179. [Google Scholar]
- Kumar, P.; Sharafeldin, T.A.; Kumar, R.; Huang, Q.; Liang, Y.; Goyal, S.M.; Porter, R.E.; Ly, H.; Mor, S.K. Development of a Recombinant Pichinde Virus-Vectored Vaccine against Turkey Arthritis Reovirus and Its Immunological Response Characterization in Vaccinated Animals. Pathogens 2021, 10, 197. [Google Scholar] [CrossRef] [PubMed]
- Brisse, M.; Huang, Q.; Rahman, M.; Di, D.; Liang, Y.; Ly, H. RIG-I and MDA5 Protect Mice From Pichinde Virus Infection by Controlling Viral Replication and Regulating Immune Responses to the Infection. Front. Immunol. 2021, 12, 801811. [Google Scholar] [CrossRef] [PubMed]
- Sun, H.; Sur, J.H.; Sillman, S.; Steffen, D.; Vu, H.L.X. Design and characterization of a consensus hemagglutinin vaccine immunogen against H3 influenza A viruses of swine. Vet. Microbiol. 2019, 239, 108451. [Google Scholar] [CrossRef] [PubMed]
- Reed, L.J.; Muench, H. A simple method of estimating fifty per cent endpoints. Am. J. Epidemiol. 1938, 27, 493–497. [Google Scholar] [CrossRef]
- Halbur, P.G.; Paul, P.S.; Frey, M.L.; Landgraf, J.; Eernisse, K.; Meng, X.J.; Lum, M.A.; Andrews, J.J.; Rathje, J.A. Comparison of the pathogenicity of two US porcine reproductive and respiratory syndrome virus isolates with that of the Lelystad virus. Vet. Pathol. 1995, 32, 648–660. [Google Scholar] [CrossRef]
- Rossman, J.S.; Lamb, R.A. Influenza virus assembly and budding. Virology 2011, 411, 229–236. [Google Scholar] [CrossRef]
- Dou, D.; Revol, R.; Ostbye, H.; Wang, H.; Daniels, R. Influenza A Virus Cell Entry, Replication, Virion Assembly and Movement. Front. Immunol. 2018, 9, 1581. [Google Scholar] [CrossRef]
- Sautto, G.A.; Kirchenbaum, G.A.; Ross, T.M. Towards a universal influenza vaccine: Different approaches for one goal. Virol. J. 2018, 15, 17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rajao, D.S.; Loving, C.L.; Gauger, P.C.; Kitikoon, P.; Vincent, A.L. Influenza A virus hemagglutinin protein subunit vaccine elicits vaccine-associated enhanced respiratory disease in pigs. Vaccine 2014, 32, 5170–5176. [Google Scholar] [CrossRef] [PubMed]
- Braucher, D.R.; Henningson, J.N.; Loving, C.L.; Vincent, A.L.; Kim, E.; Steitz, J.; Gambotto, A.A.; Kehrli, M.E., Jr. Intranasal vaccination with replication-defective adenovirus type 5 encoding influenza virus hemagglutinin elicits protective immunity to homologous challenge and partial protection to heterologous challenge in pigs. Clin. Vaccine Immunol. 2012, 19, 1722–1729. [Google Scholar] [CrossRef] [PubMed]
- Murugavelu, P.; Perween, R.; Shrivastava, T.; Singh, V.; Ahmad Parray, H.; Singh, S.; Chiranjivi, A.K.; Thiruvengadam, R.; Singh, S.; Yadav, N.; et al. Non-neutralizing SARS-CoV-2 directed polyclonal antibodies demonstrate cross-reactivity with the HA glycans of influenza virus. Int. Immunopharmacol. 2021, 99, 108020. [Google Scholar] [CrossRef]
- Turlewicz-Podbielska, H.; Pomorska-Mol, M. Porcine Coronaviruses: Overview of the State of the Art. Virol. Sin. 2021, 36, 833–851. [Google Scholar] [CrossRef]
- Takemae, N.; Tsunekuni, R.; Uchida, Y.; Ito, T.; Saito, T. Experimental infection of pigs with H1 and H3 influenza A viruses of swine by using intranasal nebulization. BMC Vet. Res. 2018, 14, 115. [Google Scholar] [CrossRef] [Green Version]





Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kumari, S.; Chaudhari, J.; Huang, Q.; Gauger, P.; De Almeida, M.N.; Liang, Y.; Ly, H.; Vu, H.L.X. Immunogenicity and Protective Efficacy of a Recombinant Pichinde Viral-Vectored Vaccine Expressing Influenza Virus Hemagglutinin Antigen in Pigs. Vaccines 2022, 10, 1400. https://doi.org/10.3390/vaccines10091400
Kumari S, Chaudhari J, Huang Q, Gauger P, De Almeida MN, Liang Y, Ly H, Vu HLX. Immunogenicity and Protective Efficacy of a Recombinant Pichinde Viral-Vectored Vaccine Expressing Influenza Virus Hemagglutinin Antigen in Pigs. Vaccines. 2022; 10(9):1400. https://doi.org/10.3390/vaccines10091400
Chicago/Turabian StyleKumari, Sushmita, Jayeshbhai Chaudhari, Qinfeng Huang, Phillip Gauger, Marcelo Nunes De Almeida, Yuying Liang, Hinh Ly, and Hiep L. X. Vu. 2022. "Immunogenicity and Protective Efficacy of a Recombinant Pichinde Viral-Vectored Vaccine Expressing Influenza Virus Hemagglutinin Antigen in Pigs" Vaccines 10, no. 9: 1400. https://doi.org/10.3390/vaccines10091400
APA StyleKumari, S., Chaudhari, J., Huang, Q., Gauger, P., De Almeida, M. N., Liang, Y., Ly, H., & Vu, H. L. X. (2022). Immunogenicity and Protective Efficacy of a Recombinant Pichinde Viral-Vectored Vaccine Expressing Influenza Virus Hemagglutinin Antigen in Pigs. Vaccines, 10(9), 1400. https://doi.org/10.3390/vaccines10091400









