PrEP Scale-Up and PEP in Central and Eastern Europe: Changes in Time and the Challenges We Face with No Expected HIV Vaccine in the near Future †
Abstract
:1. Introduction
2. Materials and Methods
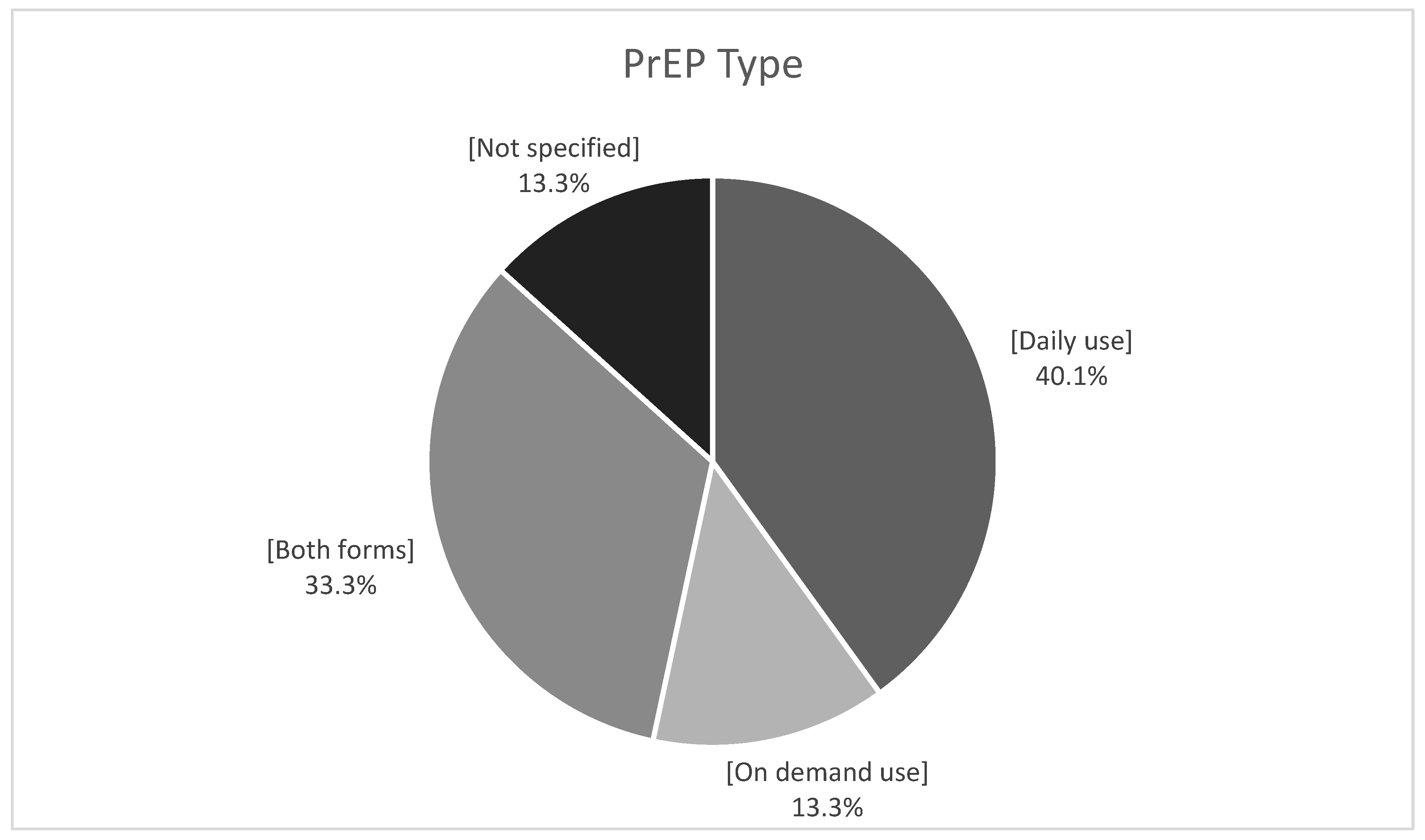
3. Results
4. Discussion
5. The Way Forward
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Eastern Europe and Central Asia may Face an Accelerated Increase in New HIV Infections and AIDS-Related Deaths Because of the Humanitarian Crisis Gripping the Entire Region. UNAIDS. Available online: https://www.unaids.org/en/keywords/eastern-europe-and-central-asia#:~:text=According%20to%20the%20UNAIDS%20Global,a%2048%25%20increase%20since%202010 (accessed on 12 November 2022).
- European Centre for Disease Prevention and Control, WHO Regional Office for Europe. HIV/AIDS Surveillance in Europe 2020–2019 Data. Stockholm: ECDC. 2020. Available online: https://www.ecdc.europa.eu/sites/default/files/documents/hiv-surveillance-report-2020.pdf (accessed on 12 November 2022).
- European Centre for Disease Prevention and Control, WHO Regional Office for Europe. HIV/AIDS Surveillance in Europe 2022–2021 Data. Copenhagen: WHO Regional Office for Europe. 2022. Available online: https://reliefweb.int/report/world/hivaids-surveillance-europe-2022–2021-data (accessed on 15 December 2022).
- Kuehn, B.M. Reduced HIV Testing and Diagnoses During COVID-19 Pandemic. JAMA 2022, 328, 519. [Google Scholar] [CrossRef] [PubMed]
- Skrzat-Klapaczynska, A.; Kowalska, J.D.; Afonina, L.; Antonyak, S.; Balayan, T.; Begovac, J.; Bursa, D.; Dragovic, G.; Gokengin, D.; Harxhi, A.; et al. The Management of HIV Care Services in Central and Eastern Europe: Data from the Euroguidelines in Central and Eastern Europe Network Group. Int. J. Environ. Res. Public Health 2022, 19, 7595. [Google Scholar] [CrossRef] [PubMed]
- UNAIDS 2025 AIDS Targets. Available online: https://www.unaids.org/sites/default/files/2025-AIDS-Targets_en.pdf (accessed on 12 November 2022).
- Hannah, S.; Chinyenze, K.; Shattock, R.; Yola, N.; Warren, M. HIV vaccines in 2022: Where to from here? J. Int. AIDS Soc. 2022, 25, e25923. [Google Scholar] [CrossRef] [PubMed]
- Strömdahl, S.; Hickson, F.; Pharris, A.; Sabido, M.; Baral, S.; Thorson, A. ECDC 2021 HIV Report. A systematic review of evidence to inform HIV prevention interventions among men who have sex with men in Europe. Euro. Surveill. 2015, 20, 21096. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bavinton, B.R.; Grulich, A.E. HIV pre-exposure prophylaxis: Scaling up for impact now and in the future. Lancet Public Health 2021, 6, e528–e533. [Google Scholar] [CrossRef] [PubMed]
- Chou, R.; Evans, C.; Hoverman, A.; Sun, C.; Dana, T.; Bougatsos, C.; Grusing, S.; Korthuis, T.P. Preexposure prophylaxis for the prevention of HIV infection: Evidence report and systematic review for the US Preventive Services Task Force. JAMA 2019, 321, 2214–2230. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rutstein, S.E.; Smith, D.K.; Dalal, S.; Baggaley, R.C.; Cohen, M.S. Initiation, discontinuation, and restarting HIV pre-exposure prophylaxis: Ongoing implementation strategies. Lancet HIV 2020, 7, e721–e730. [Google Scholar] [CrossRef]
- McCormack, S.; Dunn, D.T.; Desai, M.; Dolling, D.I.; Gafos, M.; Gilson, R.; Sullivan, A.K.; Clarke, A.; Reeves, I.; Schembri, D.; et al. Pre-exposure prophylaxis to prevent the acquisition of HIV-1 infection (PROUD): Effectiveness results from the pilot phase of a pragmatic open-label randomised trial. Lancet 2016, 387, 53–60. [Google Scholar] [CrossRef] [Green Version]
- Molina, J.-M.; Capitant, C.; Spire, B.; Pialoux, G.; Cotte, L.; Charreau, I.; Tremblay, C.; Le Gall, J.-M.; Cua, E.; Pasquet, A. On-Demand Preexposure Prophylaxis in Men at High Risk for HIV-1 Infection. N. Engl. J. Med. 2015, 373, 2237–2246. [Google Scholar] [CrossRef]
- Landovitz, R.; Currier, J.S. Postexposure Prophylaxis for HIV Infection. N. Engl. J. Med. 2009, 361, 1768–1775. [Google Scholar] [CrossRef]
- Sultan, B.; Benn, P.; Waters, L. Current perspectives in HIV post-exposure prophylaxis. HIV/AIDS–Res. Palliat. Care 2014, 6, 147–158. [Google Scholar] [CrossRef] [Green Version]
- AVAC The Global PrEP Tracker. Available online: https://www.prepwatch.org/ (accessed on 13 November 2022).
- Hayes, R.; Smidt, A.J.; Pharris, A.; Azad, Y.; Brown, A.E.; Wheatherburn, P.; Hickson, F.; Delpech, V.; Noori, T. The ECDC Dublin Declaration Monitoring Network. Estimating the ‘PrEP Gap’: How implementation and access to PrEP differ between countries in Europe and Central Asia in 2019. Euro. Surveill. 2019, 24, 1900598. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ulla, P. HIV/AIDS in Eastern Europe and Central Asia. Available online: https://www.polsoz.fu-berlin.de/polwiss/forschung/systeme/polsystem/Ressourcen-Ordner/U-Pape_HIV-AIDS-in-Eastern-Europe-and-Central-Asia_ORE-2019.pdf (accessed on 16 December 2022). [CrossRef]
- Atun, R.A.; Mckee, M.; Drobniewski, F.; Coker, R. Analysis of how the health systems context shapes responses to the control of human immunodeficiency virus: Case-studies from the Russian Federation. Bull. World Health Organ. 2005, 83, 730–738. [Google Scholar] [PubMed]
- Atun, R.A.; McKee, M.; Coker, R.; Gurol-Urganci, İ. Health systems’ responses to 25 years of HIV in Europe: Inequities persist and challenges remain. Health Policy 2008, 86, 181–194. [Google Scholar] [CrossRef] [PubMed]
- Hamers, F.F.; Downs, A.M. HIV in central and eastern Europe. Lancet 2003, 361, 1035–1044. [Google Scholar] [CrossRef]
- Aibekova, L.; Foley, B.; Hortelano, G.; Raees, M.; Abdraimov, S.; Toichuv, R.; Syed, A. Molecular epidemiology of HIV-1 subtype A in former Soviet Union countries. PLoS ONE 2018, 13, e0191891. [Google Scholar] [CrossRef] [Green Version]
- Prevention Gap Report. UNAIDS; 2016. Available online: https://www.unaids.org/sites/default/files/media_asset/2016-prevention-gap-report_en.pdf (accessed on 16 December 2022).
- Kowalska, J.D.; Oprea, C.; de Witt, S.; Pozniak, A.; Gökengin, D.; Youle, M.; Lundgren, J.D.; Horban, A.; ECEE Network Group. Euroguidelines in Central and Eastern Europe (ECEE) conference and the Warsaw Declaration—A comprehensive meeting report. HIV Med. 2017, 18, 370–375. [Google Scholar] [CrossRef] [Green Version]
- Kowalska, J.D.; Bursa, D.; Gökengin, D.; Jilich, D.; Tomazic, J.; Vasylyev, M.; Bukovinowa, P.; Mulabdic, V.; Antonyak, S.; Horban, A.; et al. HIV health care providers are ready to introduce pre-exposure prophylaxis in Central and Eastern Europe and neighbouring countries: Data from the Euroguidelines in Central and Eastern Europe (ECEE) Network Group. HIV Med. 2018, 19, 629–633. [Google Scholar] [CrossRef]
- Balayan, T.; Begovac, J.; Skrzat-Klapaczynska, A.; Aho, I.; Alexiev, I.; Bukovinova, P.; Salemovic, D.; Gokengin, D.; Harxhi, A.; Holban, T.; et al. Where are we with pre-exposure prophylaxis use in Central and Eastern Europe? Data from the Euroguidelines in Central and Eastern Europe (ECEE) Network Group. HIV Med. 2021, 22, 67–72. [Google Scholar] [CrossRef]
- Segal, K. The evolution of oral PrEP access: Tracking trends in global oral PrEP use over time. HIV Research for Prevention Congress (HIV R4P; virtual); Jan 28 2021; Oral abstract OA11.01. J. Int. AIDS Soc. 2021, 24, e25659:27. [Google Scholar]
- Schaefer, R.; Schmidt, H.-M.A.; Ravasi, G.; Mozalevskis, A.; Rewari, B.B.; Lule, F.; Yeboue, K.; Brink, A.; Konath, N.M.; Sharma, M.; et al. Adoption of guidelines on and use of oral pre-exposure prophylaxis: A global summary and forecasting study. Lancet HIV 2021, 8, e502–e510. [Google Scholar] [CrossRef] [PubMed]
- Annequin, M.; Villes, V.; Delabre, R.M.; Alain, T.; Morel, S.; Michels, D.; Schmidt, A.J.; Velter, A.; Castro, D.R. Are PrEP services in France reaching all those exposed to HIV who want to take PrEP? MSM respondents who are eligible but not using PrEP (EMIS 2017). AIDS Care 2020, 32, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Gokengin, D.; Oprea, C.; Begovac, J.; Horban, A.; Nazlı Zeka, A.; Sedlacek, D.; Allabergan, B.; Almamedova, E.A.; Balayan, T.; Banhegy, D.; et al. HIV care in Central and Eastern Europe: How close are we to the target? Int. J. Infect. Dis. 2018, 70, 121–130. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- van Dijk, M.; de Wit, J.B.F.; Guadamuz, T.E.; Martinez, J.E.; Jonas, K.J. Slow Uptake of PrEP: Behavioral Predictors and the Influence of Price on PrEP Uptake Among MSM with a High Interest in PrEP. AIDS Behav. 2021, 25, 2382–2390. [Google Scholar] [CrossRef] [PubMed]
- Frankis, J.; Young, I.; Flowers, P.; McDaid, L. Who Will Use Pre-Exposure Prophylaxis (PrEP) and Why?: Understanding PrEP Awareness and Acceptability amongst Men Who Have Sex with Men in the UK—A Mixed Methods Study. PLoS ONE 2016, 11, e0151385. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goedel, W.C.; Mayer, K.H.; Mimiaga, M.J.; Duncan, D.T. Considerable interest in pre-exposure prophylaxis uptake among men who have sex with men recruited from a popular geosocial-networking smartphone application in London. Glob. Public Health 2019, 14, 112–121. [Google Scholar] [CrossRef] [PubMed]
- Bull, L.; Dimitrijevic, P.; Beverley, S.; Scarborough, A.; Mandalia, S.; Dosekun, O.; Barber, T.; Reeves, I.; McCormack, S.; Rayment, M. Perceived need of, and interest in, HIV pre-exposure prophylaxis amongst men who have sex with men attending three sexual health clinics in London, UK. Int. J. STD AIDS 2018, 29, 435–442. [Google Scholar] [CrossRef]
- Khawcharoenporn, T.; Kendrick, S.; Smith, K. HIV risk perception and preexposure prophylaxis interest among a heterosexual population visiting a sexually transmitted infection clinic. AIDS Patient Care STDS 2012, 26, 222–233. [Google Scholar] [CrossRef]
- Clifton, S.; Nardone, A.; Field, N.; Mercer, C.H.; Tanton, C.; Macdowall, W.; Johnson, A.M.; Sonnenberg, P. HIV testing, risk perception, and behaviour in the British population. AIDS 2016, 30, 943–951. [Google Scholar] [CrossRef] [Green Version]
- Nazlı, A.; Garner, A.; Gökengin, D. Awareness of HIV pre-exposure prophylaxis among men who have sex with men using apps for sexual encounters in Turkiye. Int. J. STD AIDS 2022, 33, 1124–1133. [Google Scholar] [CrossRef]
- Moseholm, E.; Gillece, Y.; Collins, B. Achievements and gaps to provide pre-exposure prophylaxis (PrEP) for women across the European Region—Results from a European survey study. J. Virus Erad. 2021, 7, 100026. [Google Scholar] [CrossRef] [PubMed]
- Benn, P.; Fisher, M. HIV and post-exposure prophylaxis. Clin. Med. 2008, 8, 319–322. [Google Scholar] [CrossRef] [PubMed]
- Beekmann, S.E.; Henderson, D.K. Protection of healthcare workers from bloodborne pathogens. Curr. Opin. Infect. Dis. 2005, 18, 331–336. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, I.; Williams, S. Occupational exposure to HIV and post-exposure prophylaxis in healthcare workers. Occup. Med. 2000, 50, 387–391. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mengistu, D.A.; Tolera, S.T.; Demmu, Y.M. Worldwide Prevalence of Occupational Exposure to Needle Stick Injury among Healthcare Workers: A Systematic Review and Meta-Analysis. Can. J. Infect. Dis. Med. Microbiol. 2021, 2021, 6637584. [Google Scholar] [CrossRef]
- Mengistu, D.A.; Dirirsa, G.; Mati, E.; Ayele, D.M.; Bayu, K.; Deriba, W.; Alemu, F.K.; Demmu, Y.M.; Asefa, Y.A.; Geremew, A. Global Occupational Exposure to Blood and Body Fluids among Healthcare Workers: Systematic Review and Meta-Analysis. Can. J. Infect. Dis. Med. Microbiol. 2022, 2022, 5732046. [Google Scholar] [CrossRef]
- Cardo, D.M.; Culver, D.H.; Ciesielski, C.A.; Srivastava, P.U.; Marcus, R.; Abiteboul, D.; Heptonstall, J.; Ippolito, G.; Lot, F.; McKibben, P.S.; et al. A case–control study of HIV seroconversion in health care workers after percutaneous exposure. New Engl. J. Med. 1997, 337, 1485–1490. [Google Scholar] [CrossRef]
- Sonder, G.J.B.; van den Hoek, A.; Regez, R.M.; Brinkman, K.; Prins, J.M.; Mulder, J.W.; Veenstra, J.; Claessen, F.A.; Coutinho, R.A. Trends in HIV postexposure prophylaxis prescription and after sexual exposure in Amsterdam, 2000–2004. Sex. Transm. Inf. 2007, 34, 288–293. [Google Scholar] [CrossRef]
- Laporte, A.; Jourdan, N.; Bouvet, E.; Lamontagne, F.; Pillonel, J.; Desenclos, J.C. Post-exposure prophylaxis after non-occupational HIV exposure: Impact of recommendations on physicians’ experiences and attitudes. AIDS 2002, 16, 397–405. [Google Scholar] [CrossRef]
- Updated Guidelines for Antiretroviral Postexposure Prophylaxis After Sexual, Injection Drug Use, or Other Nonoccupational Exposure to HIV—United States, 2016, CDC. Available online: https://www.cdc.gov/hiv/pdf/programresources/cdc-hiv-npep-guidelines.pdf (accessed on 12 November 2022).
- WHO. EACS Guidelines. Version 11.1 October 2022. Available online: https://www.eacsociety.org/media/guidelines-11.1_final_09-10.pdf (accessed on 12 November 2022).
- WHO Guidelines on Post-Exposure Prophylaxis for HIV and the Use of Co-Trimoxazole Prophylaxis for HIV-Related Infections among Adults, Adolescents and Children: Recommendations for a Public Health Approach. December 2014. Available online: http://apps.who.int/iris/bitstream/handle/10665/145719/9789241508193_eng.pdf;jsessionid=4EFA3BE8D9928EDEF9A2CC4E8DA91381?sequence=1 (accessed on 12 November 2022).
- Prati, G.; Zani, B.; Pietrantoni, L. PEP and TasP Awareness among Italian MSM, PLWHA, and High-Risk Heterosexuals and Demographic, Behavioral, and Social Correlates. PLoS ONE 2016, 11, e0157339. [Google Scholar] [CrossRef]
- Bryant, J.; Baxter, L.; Hird, S. Non-occupational postexposure prophylaxis for HIV: A systematic review. Health Technol. Assess. 2009, 13, 1–82. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Duteil, C.; de La Rochebrochard, E.; Piron, P.; Segouin, C.; Troude, P. What do patients consulting in a free sexual health center know about HIV transmission and post-exposure prophylaxis? BMC Public Health 2021, 21, 494. [Google Scholar] [CrossRef] [PubMed]
- Ayieko, J.; Petersen, M.L.; Kamya, M.R.; Havlir, D.V. PEP for HIV prevention: Are we missing opportunities to reduce new infections? J. Int. AIDS Soc. 2022, 25, e25942. [Google Scholar] [CrossRef] [PubMed]
- Izulla, P.; McKinnon, L.T.; Munyao, J.; Ireri, N.; Nagelkerke, N.; Gakii, G.; Gelmon, L.; Nangami, M.; Kaul, R.; Kimani, J. Repeat Use of Post-exposure Prophylaxis for HIV Among Nairobi Based Female Sex Workers Following Sexual Exposure. AIDS Behav. 2016, 20, 1549–1555. [Google Scholar] [CrossRef]
| PrEP Availability and Accessibility | n (%) |
|---|---|
| PrEP licensed | 15 (68.2%) |
| PrEP in guidelines | |
| In national HIV guidelines | 12 (54.5%) |
| Specific PrEP guidelines | 1(4.5%) |
| No need for guidelines to prescribe PrEP | 1 (4.5%) |
| PrEP prescription | |
| Free of charge within the public health system | 5 (22.7%) |
| Free of charge within the public health system but patient has to pay for drugs | 6 (27.3%) |
| Free of charge within the public health system but patient has to pay for drugs and tests | 1 (4.5%) |
| In public practice | 2 (9.1%) |
| Not prescribed | 2 (9.1%) |
| Other settings * | 6 (27.3%) |
| Formulations available in pharmacies | |
| Generic form | 6 (27.2%) |
| Both forms | 4 (18.2%) |
| Not available | 10 (45.5%) |
| Available in other settings | 2 (9.1%) |
| Barriers | Percentage |
|---|---|
| Lack of knowledge/awareness among people who are in need | 59.1% |
| Not being reimbursed | 50.0% |
| Low perception of HIV risk | 45.5% |
| Lack of knowledge among healthcare providers | 40.9% |
| Fear of stigma and discrimination | 31.8% |
| PrEP not being licensed | 22.7% |
| Fear of side effects | 13.6% |
| Lack of decentralization | 13.6% |
| Other * | 27.3% |
| PrEP Availability, Accessibility and Use | 2018 | 2021 |
|---|---|---|
| PrEP licensed | 13 (68.4%) | 15 (75%) |
| PrEP recommended in national guidelines | 10 (50%) | 11 (55%) |
| PrEP prescription | ||
| Free of charge within the public health system | 2 (10.5%) * | 5 (25%) |
| Free of charge within the public health system but patient has to pay for drugs | 4 (21.1%) * | 6 (30%) |
| Free of charge within the public health system but patient has to pay for drugs and tests | 1 (5.3%) * | 1 (5%) |
| In private practice | 1 (5.3%) * | 2 (10%) |
| PrEP is not prescribed | 4 (21.1%) * | 1 (5%) |
| PrEP availability in pharmacies | ||
| Original form | 1(5%) | 0 (0%) |
| Generic form | 4 (20%) | 7 (35%) |
| Both original and generic forms | 5 (25%) | 3 (15%) |
| Not available | 8 (40%) | 8 (40%) |
| Other availability | 2 (10%) | 2 (10%) |
| PrEP offering centers | 47 | 95 |
| Estimated number on PrEP | 4500 | 9000 |
| Informal PrEP use | 13 (68.4%) * | 15 (75%) |
| Countries | PrEP Available | PrEP Guidelines Available | PrEP Offering Centres Available | Informal PrEP Use | Non-Occupational PEP Available | Occupational PEP Available |
|---|---|---|---|---|---|---|
| Albania | √ | √ | ||||
| Armenia | √ | √ | √ | √ | √ | |
| Belarus | √ | √ | √ | √ | √ | |
| Bosnia and Herzegovina | √ | √ | √ | √ | √ | |
| Bulgaria | √ | √ | √ | √ | √ | |
| Croatia | √ | √ | √ | √ | √ | |
| Czech Republic | √ | √ | √ | √ | √ | √ |
| Estonia | √ | √ | √ | √ | √ | |
| Georgia | √ | √ | √ | √ | √ | |
| Greece | √ | √ | √ | |||
| Hungary | √ | √ | √ | √ | √ | √ |
| Lithuania | √ | √ | √ | √ | ||
| Macedonia | √ | √ | √ | |||
| Montenegro | √ | √ | √ | |||
| Poland | √ | √ | √ | √ | √ | √ |
| Romania | √ | √ | √ | √ | ||
| Russian Federation | √ | √ | √ | √ | √ | √ |
| Serbia | √ | |||||
| Slovakia | √ | √ | √ | √ | √ | |
| Slovenia | √ | √ | √ | √ | √ | √ |
| Turkiye | √ | √ | √ | √ | √ | |
| Ukraine | √ | √ | √ | √ | √ | √ |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gokengin, D.; Bursa, D.; Skrzat-Klapaczynska, A.; Alexiev, I.; Arsikj, E.; Balayan, T.; Begovac, J.; Cicic, A.; Dragovic, G.; Harxhi, A.; et al. PrEP Scale-Up and PEP in Central and Eastern Europe: Changes in Time and the Challenges We Face with No Expected HIV Vaccine in the near Future. Vaccines 2023, 11, 122. https://doi.org/10.3390/vaccines11010122
Gokengin D, Bursa D, Skrzat-Klapaczynska A, Alexiev I, Arsikj E, Balayan T, Begovac J, Cicic A, Dragovic G, Harxhi A, et al. PrEP Scale-Up and PEP in Central and Eastern Europe: Changes in Time and the Challenges We Face with No Expected HIV Vaccine in the near Future. Vaccines. 2023; 11(1):122. https://doi.org/10.3390/vaccines11010122
Chicago/Turabian StyleGokengin, Deniz, Dominik Bursa, Agata Skrzat-Klapaczynska, Ivailo Alexiev, Elena Arsikj, Tatevik Balayan, Josip Begovac, Alma Cicic, Gordana Dragovic, Arjan Harxhi, and et al. 2023. "PrEP Scale-Up and PEP in Central and Eastern Europe: Changes in Time and the Challenges We Face with No Expected HIV Vaccine in the near Future" Vaccines 11, no. 1: 122. https://doi.org/10.3390/vaccines11010122






