Vaccine Hesitancy and Perceptions of the Community about Polio in High-Risk Areas of Karachi, Sindh, Pakistan
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mach, O.; Tangermann, R.H.; Wassilak, S.G.; Singh, S.; Sutter, R.W. Outbreaks of Paralytic Poliomyelitis During 1996–2012: The Changing Epidemiology of a Disease in the Final Stages of Eradication. J. Infect. Dis. 2014, 210 (Suppl. 1), S275–S282. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aylward, R.B.; Linkins, J. Polio eradication: Mobilizing and managing the human resources. Bull. World Health Organ. 2005, 83, 268–273. [Google Scholar] [PubMed]
- Rana, M.S.; Usman, M.; Ikram, A.; Salman, M.; Zaidi, S.S.Z.; Umair, M. The negative impact of the COVID-19 Pandemic on immunization and the positive impact on Polio eradication in Pakistan and Afghanistan. J. Infect. 2022, 85, 174–211. [Google Scholar] [CrossRef] [PubMed]
- Bandyopadhyay, A.S.; Macklin, G.R. Global Polio Eradication: Progress and Challenges. Hum. Viruses Dis. Treat. Vaccines 2021, 629–649. [Google Scholar] [CrossRef]
- Greene, S.A.; Ahmed, J.; Datta, S.D.; Burns, C.C.; Quddus, A.; Vertefeuille, J.F.; Wassilak, S.G. Progress toward polio eradica-tion—Worldwide, January 2017–March 2019. Morb. Mortal. Wkly. Rep. 2019, 68, 458–462. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ittefaq, M.; Baines, A.; Abwao, M.; Shah, S.F.A.; Ramzan, T. “Does Pakistan still have polio cases?”: Exploring discussions on polio and polio vaccine in online news comments in Pakistan. Vaccine 2021, 39, 480–486. [Google Scholar] [CrossRef]
- Ozawa, S.; Stack, M.L. Public trust and vaccine acceptance-international perspectives. Hum. Vaccines Immunother. 2013, 9, 1774–1778. [Google Scholar] [CrossRef]
- Yufika, A.; Wagner, A.L.; Nawawi, Y.; Wahyuniati, N.; Anwar, S.; Yusri, F.; Haryanti, N.; Wijayanti, N.P.; Rizal, R.; Fitriani, D.; et al. Parents’ hesitancy towards vaccination in Indonesia: A cross-sectional study in Indonesia. Vaccine 2020, 38, 2592–2599. [Google Scholar] [CrossRef]
- Horst, A.; Watkins, S. Enhancing Smallholder Incomes by Linking to High Value Markets in Pakistan’s Punjab and Sindh Provinces; World Bank: Washington, DC USA, 2022. [Google Scholar] [CrossRef]
- The Express Tribune. Fake News Hinders the Antipolio Campaign in K-P. 2019 Apr 23. Available online: https://tribune.com.pk/story/1957206/1-fake-news-hinders-anti-polio-campaign-k-p/ (accessed on 28 November 2022).
- Pakistan National Emergency Action Plan for Polio Eradication (NEAP) 2020. Available online: https://polioeradication.org/wp-content/uploads/2020/11/Pakistan-NEAP-2020.pdf (accessed on 18 December 2022).
- Pakistan bureau of statistics. 2017 Census of Pakistan. Available online: https://www.pbs.gov.pk/content/final-results-census-2017 (accessed on 18 December 2022).
- Openepi Software. The Sample Size for Frequency in a Population. Available online: https://www.openepi.com/SampleSize/SSPropor.htm (accessed on 18 December 2022).
- Di Pietro, M.L.; Poscia, A.; Teleman, A.A.; Maged, D.; Ricciardi, W. Vaccine hesitancy: Parental, professional, and public responsibility. Ann Ist Super Sanita 2017, 53, 157–162. [Google Scholar] [CrossRef]
- Sallam, M. COVID-19 Vaccine Hesitancy Worldwide: A Concise Systematic Review of Vaccine Acceptance Rates. Vaccines 2021, 9, 160. [Google Scholar] [CrossRef]
- Bullo, U.F.; Mehraj, J.; Raza, S.M.; Rasool, S.; Ansari, N.N.; Shaikh, A.A.; Phul, Z.A.; Memon, S.A.; Baloch, R.I.; Baloch, Z.A.; et al. An experience in mass administration of fractional dose inactivated polio vaccine through intradermal needle-free injectors in Karachi, Sindh, Pakistan. BMC Public Health 2021, 21, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Facciolà, A.; Visalli, G.; Orlando, A.; Bertuccio, M.P.; Spataro, P.; Squeri, R.; Picerno, I.; Di Pietro, A. Vaccine Hesitancy: An Overview on Parents’ Opinions about Vaccination and Possible Reasons of Vaccine Refusal. J. Public Health Res. 2019, 8, 1436. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Habib, M.A.; Soofi, S.B.; Ali, N.; Hussain, I.; Tabassum, F.; Suhag, Z.; Anwar, S.; Ahmed, I.; Bhutta, Z.A. Knowledge and perceptions of polio and polio immunization in polio high-risk areas of Pakistan. J. Public Health Policy 2017, 38, 16–36. [Google Scholar] [CrossRef] [PubMed]
- Closser, S.; Jooma, R.; Varley, E.; Qayyum, N.; Rodrigues, S.; Sarwar, A.; Omidian, P. Polio Eradication and Health Systems in Karachi: Vaccine Refusals in Context. Glob. Health Commun. 2015, 1, 32–40. [Google Scholar] [CrossRef] [Green Version]
- Masood, T.; Jaishri, M.; Subhash, G. Factors affecting full immunization coverage among children aged 12–23 months in urban and rural areas of Sindh. Indian J. Sci Technol 2020, 13, 1283–1292. [Google Scholar] [CrossRef]
- Chaudhry, A.; Javed, N.; Wattoo, M.M. Assessment of risk factors associated with oral polio vaccine refusal in Rahim Yar Khan District, Pakistan (2017). J. Biosaf. Biosecurity 2020, 2, 27–30. [Google Scholar] [CrossRef]
- Khan, S.A.; Ashfaq, M.; Ayub, A.; Jamil, A.; Badshah, J.; Ullah, I.; Shahabuddin, A.S.; Khalid, F. Developing a three-dimensional narrative to counter polio vaccine refusal in Charsadda. J. Glob. Health 2020, 10, 021301. [Google Scholar] [CrossRef]
- Marshall, S.; Moore, A.C.; Sahm, L.J.; Fleming, A. Parent Attitudes about Childhood Vaccines: Point Prevalence Survey of Vaccine Hesitancy in an Irish Population. Pharmacy 2021, 9, 188. [Google Scholar] [CrossRef]
- Zarak, M.S.; Sana, H.; Arshad, Z.; Saleem, A.; Shah, M.; Tareen, H.; Ullah, S.; Baloch, S.; Kakar, S.; Kakar, K. Understanding the reasons for refusal of polio vaccine by families in Quetta Block, Pakistan. East. Mediterr. Health J. 2022, 28, 498–505. [Google Scholar] [CrossRef]
- Barchielli, B.; Cricenti, C.; Gallè, F.; Sabella, E.A.; Liguori, F.; Da Molin, G.; Liguori, G.; Orsi, G.B.; Giannini, A.M.; Ferracuti, S.; et al. Climate Changes, Natural Resources Depletion, COVID-19 Pandemic, and Russian-Ukrainian War: What Is the Impact on Habits Change and Mental Health? Int. J. Environ. Res. Public Health 2022, 19, 11929. [Google Scholar] [CrossRef]
- Shah, S.F.A.; Ginossar, T.; Weiss, D. “This is a Pakhtun disease”: Pakhtun health journalists’ perceptions of the barriers and facilitators to polio vaccine acceptance among the high-risk Pakhtun community in Pakistan. Vaccine 2019, 37, 3694–3703. [Google Scholar] [CrossRef] [PubMed]

| Variables | Number | Percentage |
|---|---|---|
| Districts | ||
| Central | 50 | 15.4 |
| East | 75 | 23.1 |
| Korangi | 10 | 3.1 |
| Malir | 40 | 12.3 |
| South | 10 | 3.1 |
| West | 140 | 43.0 |
| Total children in the household | ||
| Mean (±Standard Deviation) | 3.391 | 2.428 |
| Total under-five children in the household | ||
| Mean (±Standard Deviation) | 1.815 | 1.175 |
| Gender of the child (under five) | ||
| Female | 141 | 43.4 |
| Male | 184 | 56.6 |
| Common childhood health problems (multiple response variables) | ||
| Respiratory tract infections | 206 | 33 |
| Gastrointestinal infections | 123 | 19.7 |
| Fever | 205 | 32.8 |
| Other infectious diseases | 44 | 7.0 |
| Other non-communicable diseases | 33 | 5.3 |
| No major health issues | 14 | 2.2 |
| When last visited health care facility for treatment of child | ||
| Within the past 3 months | 219 | 67.4 |
| Between the last 3–6 months | 47 | 14.5 |
| Between 6–12 months | 8 | 2.5 |
| More than 12 months | 8 | 2.5 |
| Don’t know/don’t remember | 43 | 13.1 |
| Preferred facility for treatment of child | ||
| Private | 264 | 81.2 |
| Government | 28 | 8.7 |
| Both | 33 | 10.1 |
| EPI routine vaccination status of children | ||
| No | 70 | 21.5 |
| Yes (partial) | 94 | 28.9 |
| Yes (full) | 161 | 49.6 |
| EPI vaccination card availability | ||
| No | 186 | 57.2 |
| Yes | 105 | 32.3 |
| Variables | Number | Percentage |
|---|---|---|
| Polio teams visit your house | ||
| No | 3 | 0.9 |
| Yes | 322 | 99.1 |
| Number of times the Polio team visited | ||
| 1–10 | 40 | 12.3 |
| 11–24 | 194 | 59.7 |
| ≥36 | 80 | 24.6 |
| Reason for repeated visits of polio teams (multiple response variables) | ||
| Child health or vaccination | 218 | 67.5 |
| Job or Government Policy | 115 | 35.6 |
| conspiracy or data collection | 45 | 13.9 |
| To harm children | 46 | 14.2 |
| Don’t know | 49 | 15.2 |
| Rate behavior of the polio team (0 very bad to 10 very good) | ||
| 0 | 15 | 4.6 |
| 1–9 | 167 | 51.2 |
| 10 | 139 | 43.3 |
| Participant’s knowledge of polio | ||
| It’s a type of Paralysis | 74 | 22.8 |
| A type of a diseases | 130 | 40 |
| Don’t know | 116 | 35.7 |
| Participant’s knowledge about poliovirus-associated permanent disability | ||
| No | 79 | 24.3 |
| Yes | 241 | 74.2 |
| Polio vaccine importance score (0 not important to 10 highly important) | ||
| 0 | 138 | 42.5 |
| 1–9 | 132 | 40.7 |
| 10 | 46 | 14.2 |
| Ever refused for polio vaccine | ||
| No | 43 | 13.2 |
| Yes | 276 | 84.9 |
| Reason for polio refusal (multiple response variables) | ||
| no trust in vaccine quality | 112 | 37.3 |
| no trust in Polio Teams | 20 | 6.7 |
| afraid of side effects | 45 | 15.0 |
| Child was sick | 31 | 10.3 |
| Infertility | 26 | 8.7 |
| Misconception | 30 | 10.0 |
| Religious concerns | 20 | 6.7 |
| Elders don’t allow | 42 | 14.0 |
| Repeated Campaigns | 13 | 4.3 |
| Negative Video/Media | 39 | 13.0 |
| why this disease only | 27 | 9.0 |
| Prefer Private Vaccination | 25 | 8.3 |
| already vaccinated | 2 | 0.7 |
| Other reasons | 14 | 4.7 |
| No response | 7 | 2.3 |
| Anyone senior official came to convince for polio vaccination | ||
| Don’t know | 10 | 3.1 |
| No | 61 | 18.8 |
| Yes | 242 | 74.5 |
| Vaccinated child as per someone’s recommendation (multiple response variables) | ||
| No | 136 | 45.5 |
| CHW | 33 | 11.0 |
| Doctor | 28 | 9.4 |
| Other | 102 | 33.9 |
| The information source of the Polio campaign (multiple response variables) | ||
| CHW | 260 | 57.1 |
| TV | 68 | 14.9 |
| Banner/pamphlet | 49 | 10.8 |
| Newspaper | 15 | 3.3 |
| Religious persons | 8 | 1.8 |
| Social Media/Mobile | 8 | 1.8 |
| Local Influencer/Neighbor/Relative | 14 | 3.1 |
| Other (Doctor, School) | 33 | 7.3 |
| Variables | Number | Percentage |
|---|---|---|
| Status of missed vaccination reasons | ||
| Reason changed | 263 | 80.9 |
| Reason remained same | 62 | 19.1 |
| Persistent missed vaccination reasons | ||
| Direct Refusal | 9 | 2.8 |
| Misconception | 38 | 11.7 |
| Religious Matter | 1 | 0.3 |
| Demands | 2 | 0.6 |
| Sickness | 9 | 2.8 |
| Outside UC | 3 | 0.9 |
| Reason changed | 263 | 80.9 |
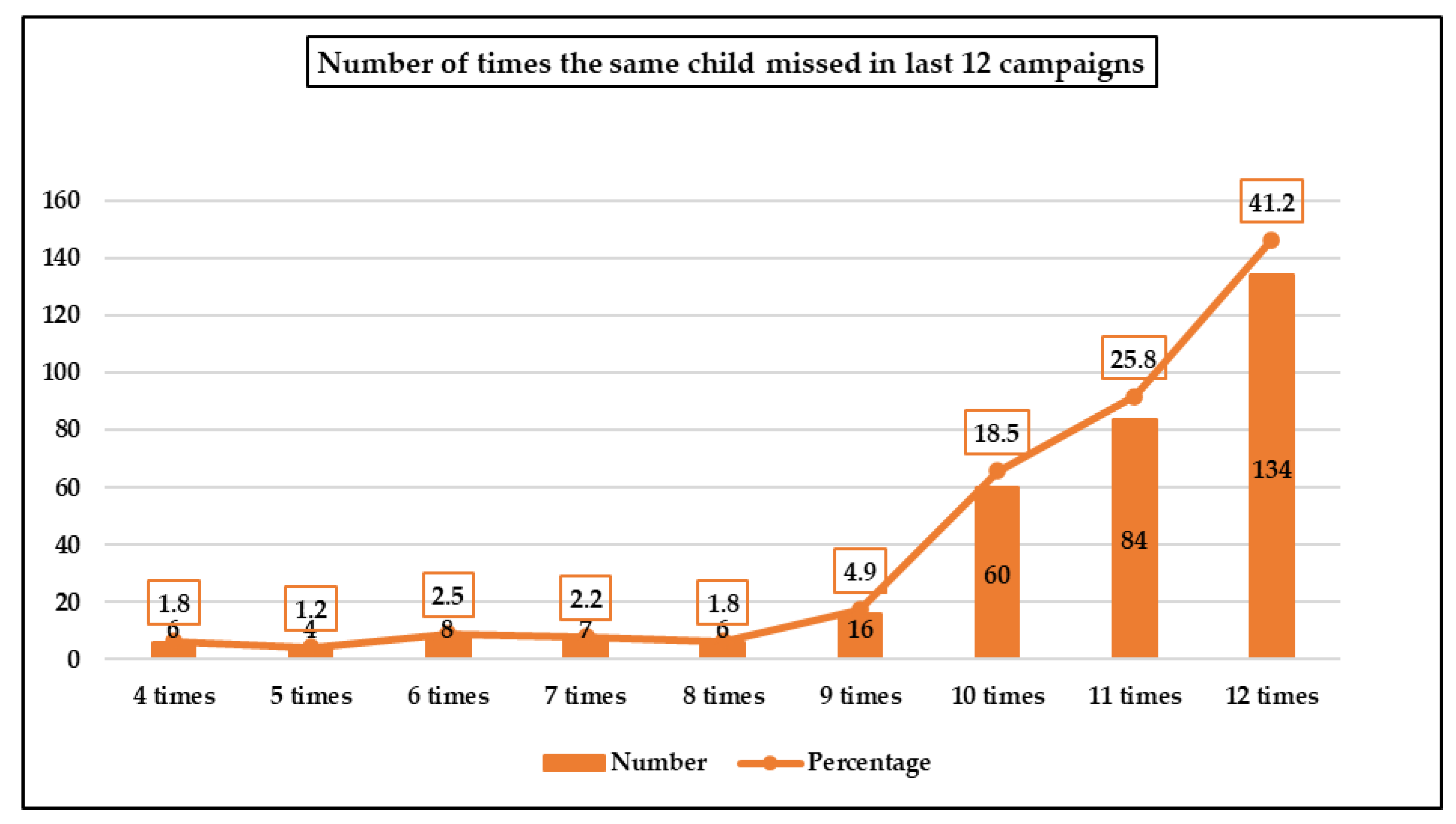
| Vaccination coverage status in the last 12 SIAs | ||
| Still missed child in all 12 SIAs | 53 | 16.3 |
| Once covered in the last 12 SIAs | 75 | 23.1 |
| Twice covered in the last 12 SIAs | 49 | 15.1 |
| Three or more times covered in the last 12 SIAs | 148 | 45.5 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abbasi, F.H.; Shaikh, A.A.; Mehraj, J.; Raza, S.M.; Rasool, S.; Bullo, U.F.; Mehraj, S.; Phul, Z.A.; Sahitia, S.; Zardari, A.A.; et al. Vaccine Hesitancy and Perceptions of the Community about Polio in High-Risk Areas of Karachi, Sindh, Pakistan. Vaccines 2023, 11, 70. https://doi.org/10.3390/vaccines11010070
Abbasi FH, Shaikh AA, Mehraj J, Raza SM, Rasool S, Bullo UF, Mehraj S, Phul ZA, Sahitia S, Zardari AA, et al. Vaccine Hesitancy and Perceptions of the Community about Polio in High-Risk Areas of Karachi, Sindh, Pakistan. Vaccines. 2023; 11(1):70. https://doi.org/10.3390/vaccines11010070
Chicago/Turabian StyleAbbasi, Fayaz Hussain, Ahmed Ali Shaikh, Jaishri Mehraj, Syed Musa Raza, Shumaila Rasool, Umar Farooq Bullo, Sandeep Mehraj, Zamir Ali Phul, Sundeep Sahitia, Asif Ali Zardari, and et al. 2023. "Vaccine Hesitancy and Perceptions of the Community about Polio in High-Risk Areas of Karachi, Sindh, Pakistan" Vaccines 11, no. 1: 70. https://doi.org/10.3390/vaccines11010070
APA StyleAbbasi, F. H., Shaikh, A. A., Mehraj, J., Raza, S. M., Rasool, S., Bullo, U. F., Mehraj, S., Phul, Z. A., Sahitia, S., Zardari, A. A., & Chandio, S. A. (2023). Vaccine Hesitancy and Perceptions of the Community about Polio in High-Risk Areas of Karachi, Sindh, Pakistan. Vaccines, 11(1), 70. https://doi.org/10.3390/vaccines11010070






