In Silico Analyses, Experimental Verification and Application in DNA Vaccines of Ebolavirus GP-Derived pan-MHC-II-Restricted Epitopes
Abstract
1. Introduction
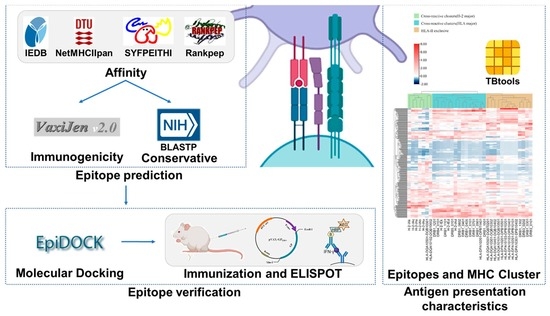
2. Methods
2.1. Acquisition of Antigen Sequences
2.2. Epitope Prediction
2.3. Immunogenicity Analysis
2.4. Conservation Analysis
2.5. Docking of pMHC Molecules
2.6. Epitopes and MHC-II Cluster
2.7. Differences in Affinity between MHC II and EBOV GP Peptides
2.8. Plasmid and His-Tagged Protein
2.9. Animals and Immunization
2.10. Peptides and ELISpot Assay
2.11. Serum Neutralization Test
2.12. Data Visualization and Statistical Analysis
3. Results
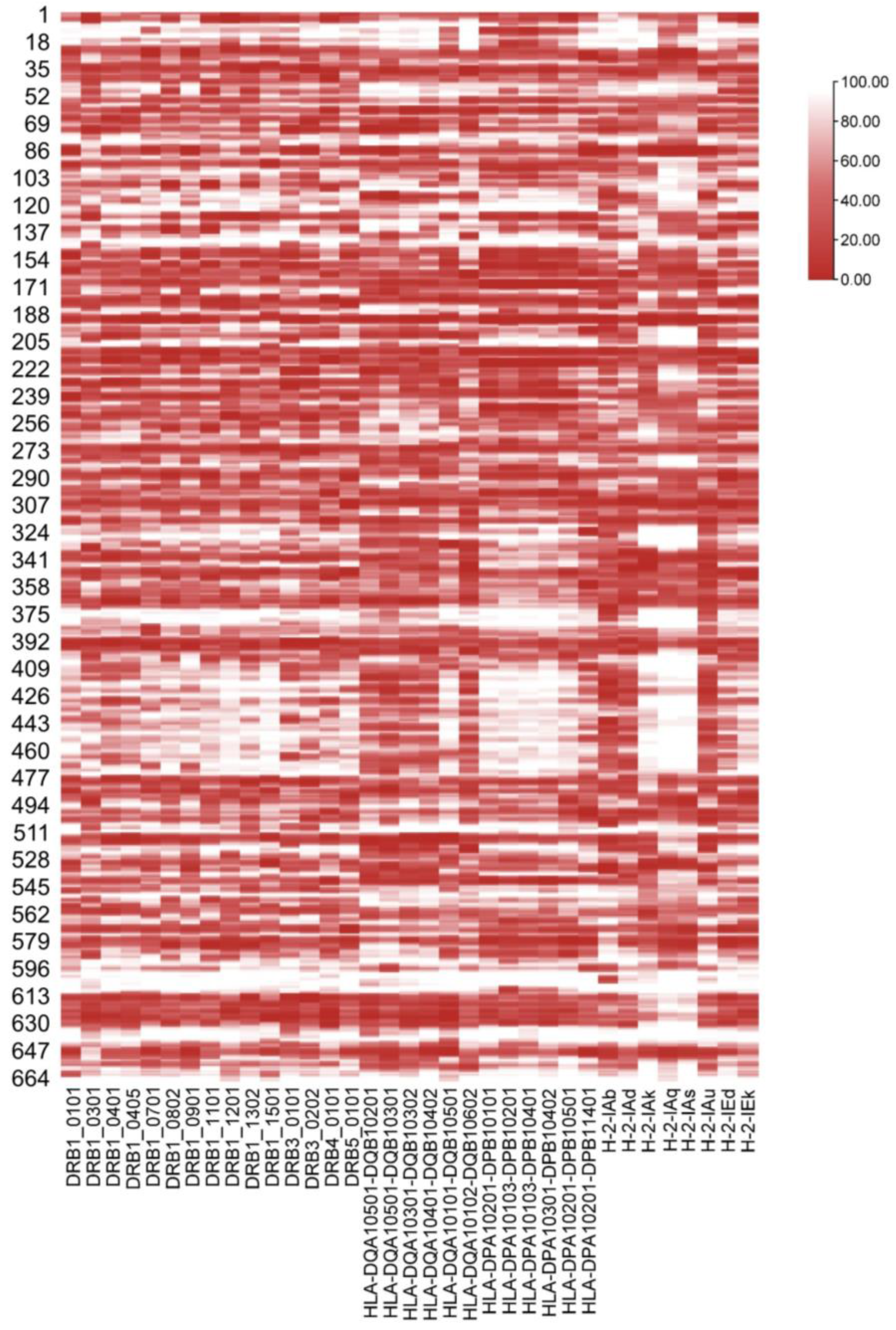
3.1. Screening of EBOV GP Peptides with High Affinity for Mouse H2-I and Major HLA-II Supertypes
3.2. Immunogenicity Analysis of EBOV GP 15-Mer Peptides
3.3. Conservation of EBOV GP MHC-II-Restricted Candidate Epitopes
3.4. Interaction between Pan-MHC Class II Molecules and 9-Mer Epitopes
3.5. Selective Epitope Docking with Pan MHC-II Molecules
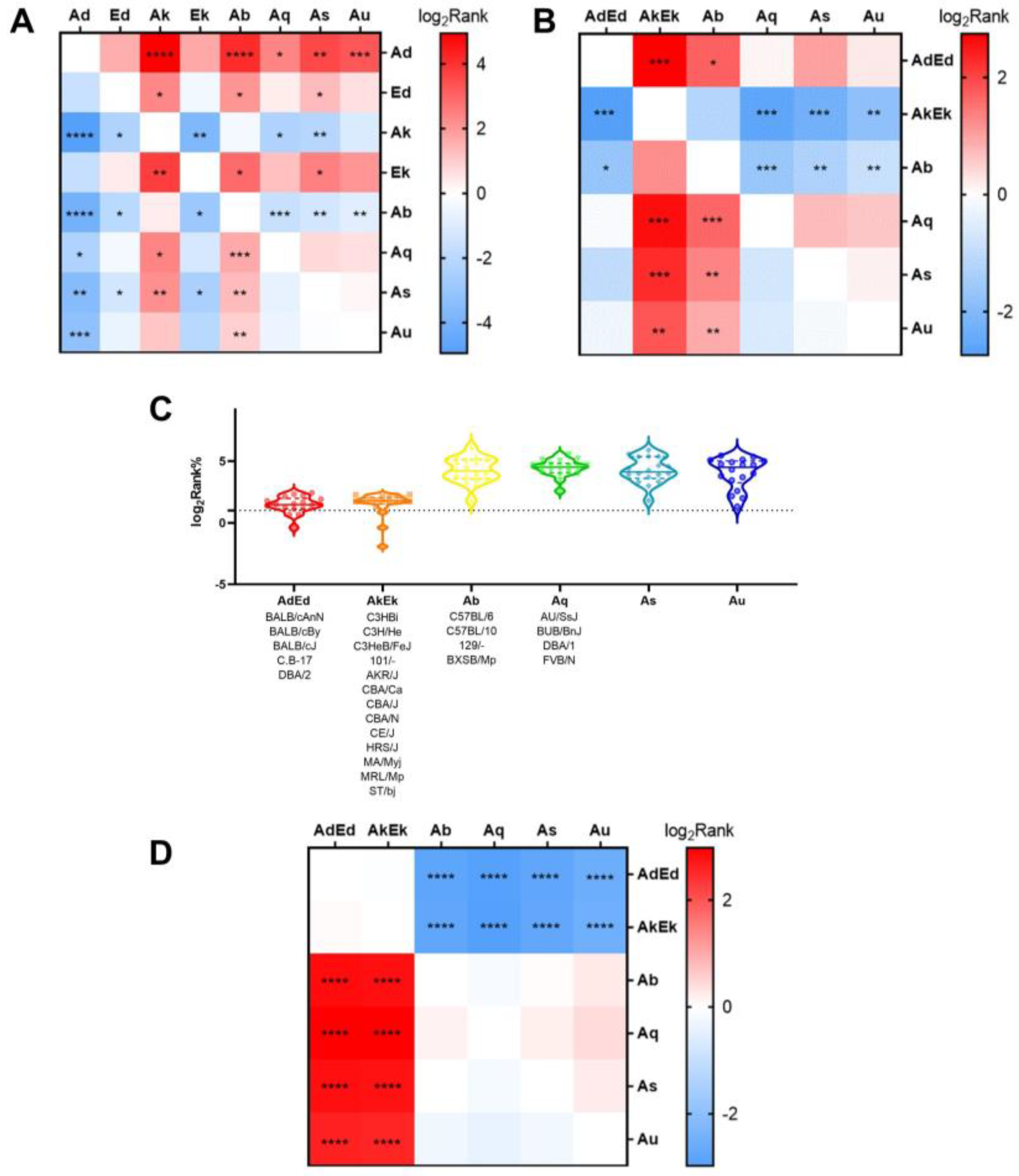
3.6. Differences in Binding Affinity between MHC II and EBOV GP 15-Mer Peptides
3.7. Experimental Verification
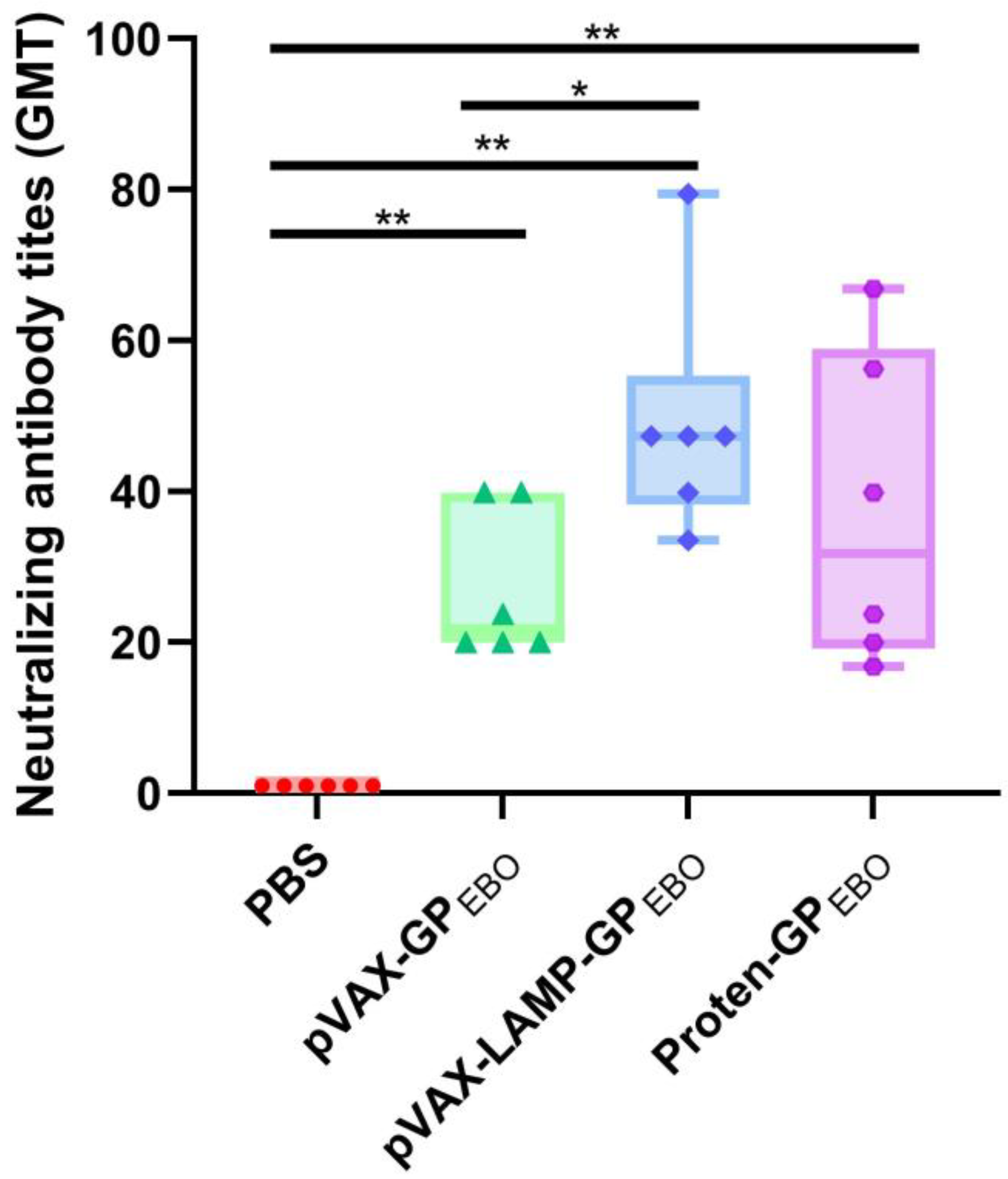
3.8. Efficient Establishment of the Antiviral Immune Response
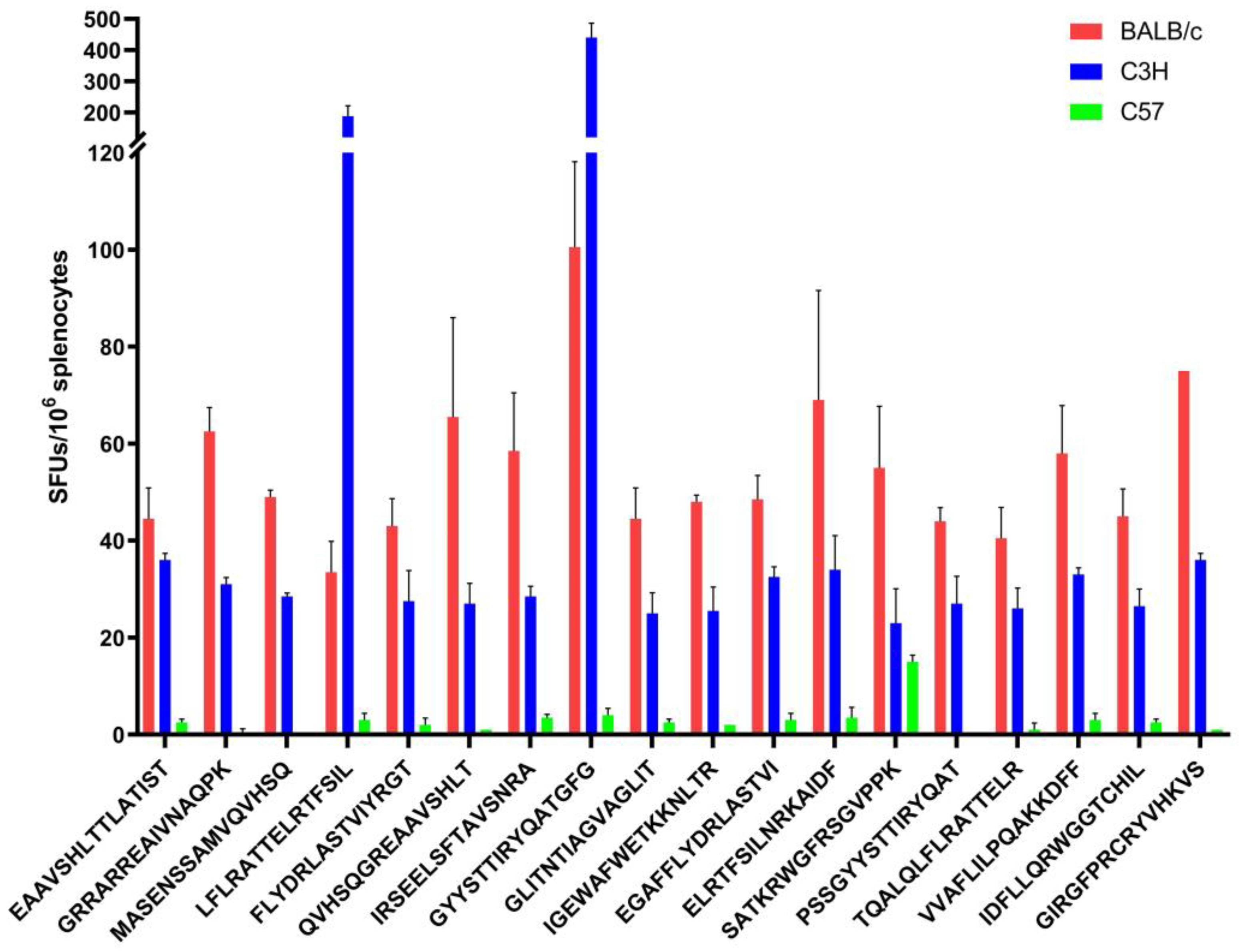
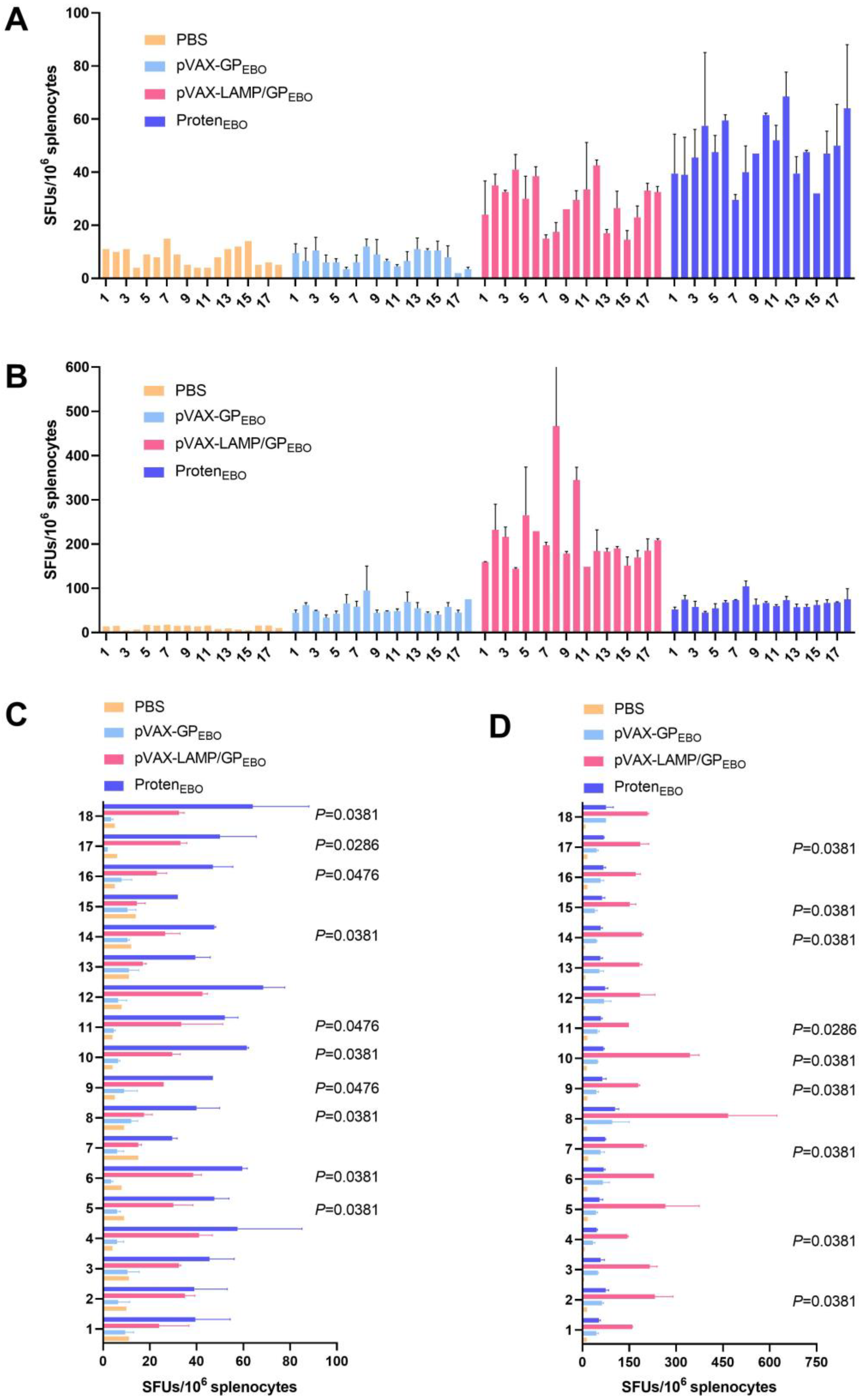
3.9. Evaluation of Cellular Immune Responses in Immunized Mice
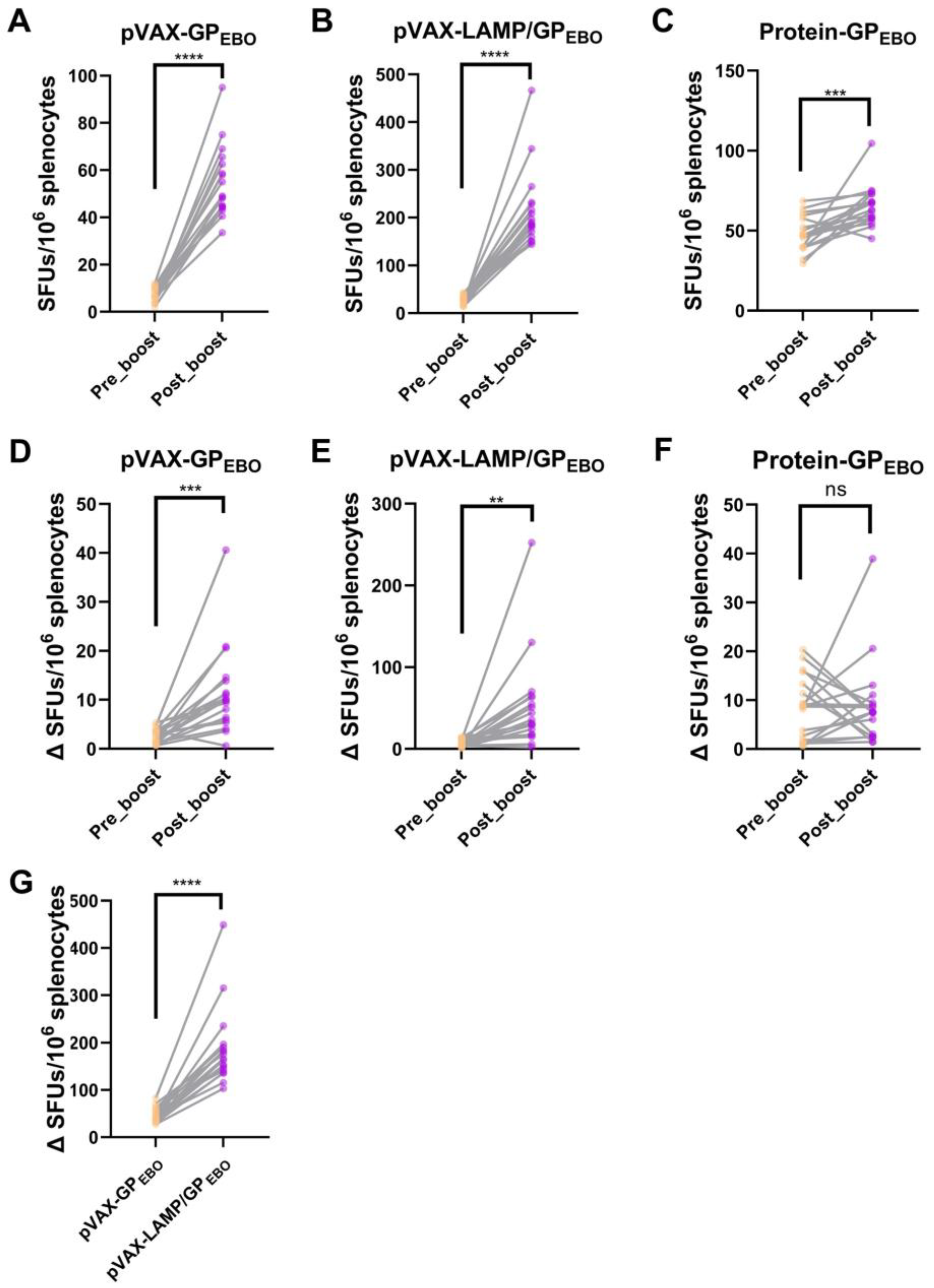
3.10. Immune Responses against 18 EBOV GP Peptides after Booster Immunization Were Significantly Improved
3.11. BALB/c Mice Immune Responses to Corresponding H-2-Id-Restricted Epitopes Amplified with Immune Boost
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Malvy, D.; McElroy, A.K.; de Clerck, H.; Günther, S.; van Griensven, J. Ebola virus disease. Lancet 2019, 393, 936–948. [Google Scholar] [CrossRef]
- Patel, P.R.; Shah, S.U. Ebola Virus. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Furuyama, W.; Marzi, A. Ebola Virus: Pathogenesis and Countermeasure Development. Annu. Rev. Virol. 2019, 6, 435–458. [Google Scholar] [CrossRef]
- Baseler, L.; Chertow, D.S.; Johnson, K.M.; Feldmann, H.; Morens, D.M. The Pathogenesis of Ebola Virus Disease. Annu. Rev. Pathol. Mech. Dis. 2017, 12, 387–418. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.E.; Fusco, M.L.; Hessell, A.J.; Oswald, W.B.; Burton, D.R.; Saphire, E.O. Structure of the Ebola virus glycoprotein bound to an antibody from a human survivor. Nature 2008, 454, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Hoenen, T.; Groseth, A.; Feldmann, H. Therapeutic strategies to target the Ebola virus life cycle. Nat. Rev. Microbiol. 2019, 17, 593–606. [Google Scholar] [CrossRef] [PubMed]
- Sakurai, Y. Ebola virus host cell entry. Uirusu 2015, 65, 71–82. [Google Scholar] [CrossRef]
- Olukitibi, T.A.; Ao, Z.; Mahmoudi, M.; Kobinger, G.A.; Yao, X. Dendritic Cells/Macrophages-Targeting Feature of Ebola Glycoprotein and its Potential as Immunological Facilitator for Antiviral Vaccine Approach. Microorganisms 2019, 7, 402. [Google Scholar] [CrossRef]
- Agnolon, V.; Kiseljak, D.; Wurm, M.J.; Wurm, F.M.; Foissard, C.; Gallais, F.; Wehrle, S.; Muñoz-Fontela, C.; Bellanger, L.; Correia, B.E.; et al. Designs and Characterization of Subunit Ebola GP Vaccine Candidates: Implications for Immunogenicity. Front. Immunol. 2020, 11, 586595. [Google Scholar] [CrossRef]
- Cross, R.W.; Mire, C.E.; Feldmann, H.; Geisbert, T.W. Post-exposure treatments for Ebola and Marburg virus infections. Nat. Rev. Drug Discov. 2018, 17, 413–434. [Google Scholar] [CrossRef]
- Keshwara, R.; Johnson, R.F.; Schnell, M.J. Toward an Effective Ebola Virus Vaccine. Annu. Rev. Med. 2017, 68, 371–386. [Google Scholar] [CrossRef]
- Sharma, A.R.; Lee, Y.-H.; Nath, S.; Lee, S.-S. Recent developments and strategies of Ebola virus vaccines. Curr. Opin. Pharmacol. 2021, 60, 46–53. [Google Scholar] [CrossRef] [PubMed]
- Tomori, O.; Kolawole, M.O. Ebola virus disease: Current vaccine solutions. Curr. Opin. Immunol. 2021, 71, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Ehrhardt, S.A.; Zehner, M.; Krähling, V.; Cohen-Dvashi, H.; Kreer, C.; Elad, N.; Gruell, H.; Ercanoglu, M.S.; Schommers, P.; Gieselmann, L.; et al. Polyclonal and convergent antibody response to Ebola virus vaccine rVSV-ZEBOV. Nat. Med. 2019, 25, 1589–1600. [Google Scholar] [CrossRef] [PubMed]
- Dolzhikova, I.V.; Zubkova, O.V.; Tukhvatulin, A.I.; Dzharullaeva, A.S.; Tukhvatulina, N.M.; Shcheblyakov, D.V.; Shmarov, M.M.; Tokarskaya, E.A.; Simakova, Y.V.; Egorova, D.A.; et al. Safety and immunogenicity of GamEvac-Combi, a heterologous VSV- and Ad5-vectored Ebola vaccine: An open phase I/II trial in healthy adults in Russia. Hum. Vaccines Immunother. 2017, 13, 613–620. [Google Scholar] [CrossRef] [PubMed]
- Milligan, I.D.; Gibani, M.M.; Sewell, R.; Clutterbuck, E.A.; Campbell, D.; Plested, E.; Nuthall, E.; Voysey, M.; Silva-Reyes, L.; McElrath, M.J.; et al. Safety and Immunogenicity of Novel Adenovirus Type 26- and Modified Vaccinia Ankara-Vectored Ebola Vaccines: A Randomized Clinical Trial. JAMA 2016, 315, 1610–1623. [Google Scholar] [CrossRef]
- Misasi, J.; Sullivan, N.J. Immunotherapeutic strategies to target vulnerabilities in the Ebolavirus glycoprotein. Immunity 2021, 54, 412–436. [Google Scholar] [CrossRef]
- Liu, Y.; Sun, B.; Pan, J.; Feng, Y.; Ye, W.; Xu, J.; Lan, M.; Sun, H.; Zhang, X.; Sun, Y.; et al. Construction and evaluation of DNA vaccine encoding Ebola virus glycoprotein fused with lysosome-associated membrane protein. Antivir. Res. 2021, 193, 105141. [Google Scholar] [CrossRef]
- Pishesha, N.; Harmand, T.J.; Ploegh, H.L. A guide to antigen processing and presentation. Nat. Rev. Immunol. 2022, 22, 751–764. [Google Scholar] [CrossRef]
- Liu, Y.; Sun, B.; Wang, J.; Sun, H.; Lu, Z.; Chen, L.; Lan, M.; Xu, J.; Pan, J.; Shi, J.; et al. In silico analyses and experimental validation of the MHC class-I restricted epitopes of Ebolavirus GP. Int. Immunol. 2022, 34, 313–325. [Google Scholar] [CrossRef]
- Martini, S.; Nielsen, M.; Peters, B.; Sette, A. The Immune Epitope Database and Analysis Resource Program 2003–2018: Reflections and outlook. Immunogenetics 2020, 72, 57–76. [Google Scholar] [CrossRef]
- Reynisson, B.; Barra, C.; Kaabinejadian, S.; Hildebrand, W.H.; Peters, B.; Nielsen, M. Improved Prediction of MHC II Antigen Presentation through Integration and Motif Deconvolution of Mass Spectrometry MHC Eluted Ligand Data. J. Proteome Res. 2020, 19, 2304–2315. [Google Scholar] [CrossRef] [PubMed]
- Jensen, K.K.; Andreatta, M.; Marcatili, P.; Buus, S.; Greenbaum, J.A.; Yan, Z.; Sette, A.; Peters, B.; Nielsen, M. Improved methods for predicting peptide binding affinity to MHC class II molecules. Immunology 2018, 154, 394–406. [Google Scholar] [CrossRef] [PubMed]
- Rammensee, H.-G.; Bachmann, J.; Emmerich, N.P.N.; Bachor, O.A.; Stevanović, S. SYFPEITHI: Database for MHC ligands and peptide motifs. Immunogenetics 1999, 50, 213–219. [Google Scholar] [CrossRef] [PubMed]
- Reche, P.A.; Glutting, J.-P.; Zhang, H.; Reinherz, E.L. Enhancement to the RANKPEP resource for the prediction of peptide binding to MHC molecules using profiles. Immunogenetics 2004, 56, 405–419. [Google Scholar] [CrossRef] [PubMed]
- Zaharieva, N.; Dimitrov, I.; Flower, D.R.; Doytchinova, I. VaxiJen Dataset of Bacterial Immunogens: An Update. Curr. Comput. Aided-Drug Des. 2019, 15, 398–400. [Google Scholar] [CrossRef]
- Doytchinova, I.A.; Flower, D.R. VaxiJen: A server for prediction of protective antigens, tumour antigens and subunit vaccines. BMC Bioinform. 2007, 8, 4. [Google Scholar] [CrossRef]
- Atanasova, M.; Patronov, A.; Dimitrov, I.; Flower, D.R.; Doytchinova, I. EpiDOCK: A molecular docking-based tool for MHC class II binding prediction. Protein Eng. Des. Sel. 2013, 26, 631–634. [Google Scholar] [CrossRef]
- Chen, C.J.; Chen, H.; Zhang, Y.; Thomas, H.R.; Frank, M.H.; He, Y.H.; Xia, R. TBtools: An Integrative Toolkit Developed for Interactive Analyses of Big Biological Data. Mol. Plant 2020, 13, 1194–1202. [Google Scholar] [CrossRef]
- Jiang, D.-B.; Zhang, J.-P.; Cheng, L.-F.; Zhang, G.-W.; Li, Y.; Li, Z.-C.; Lu, Z.-H.; Zhang, Z.-X.; Lu, Y.-C.; Zheng, L.-H.; et al. Hantavirus Gc induces long-term immune protection via LAMP-targeting DNA vaccine strategy. Antivir. Res. 2018, 150, 174–182. [Google Scholar] [CrossRef]
- Jiang, D.-B.; Sun, L.-J.; Cheng, L.-F.; Zhang, J.-P.; Xiao, S.-B.; Sun, Y.-J.; Yang, S.-Y.; Wang, J.; Zhang, F.-L.; Yang, K. Recombinant DNA vaccine of Hantavirus Gn and LAMP1 induced long-term immune protection in mice. Antivir. Res. 2017, 138, 32–39. [Google Scholar] [CrossRef]
- Jiang, D.-B.; Sun, Y.-J.; Cheng, L.-F.; Zhang, G.-F.; Dong, C.; Jin, B.-Q.; Song, C.-J.; Ma, Y.; Zhang, F.-L.; Yang, K. Construction and evaluation of DNA vaccine encoding Hantavirus glycoprotein N-terminal fused with lysosome-associated membrane protein. Vaccine 2015, 33, 3367–3376. [Google Scholar] [CrossRef] [PubMed]
- Paul, P.; Hoorn, T.v.D.; Jongsma, M.L.; Bakker, M.J.; Hengeveld, R.; Janssen, L.; Cresswell, P.; Egan, D.A.; van Ham, M.; Brinke, A.T.; et al. A Genome-wide Multidimensional RNAi Screen Reveals Pathways Controlling MHC Class II Antigen Presentation. Cell 2011, 145, 268–283. [Google Scholar] [CrossRef] [PubMed]
- Unanue, E.R.; Turk, V.; Neefjes, J. Variations in MHC Class II Antigen Processing and Presentation in Health and Disease. Annu. Rev. Immunol. 2016, 34, 265–297. [Google Scholar] [CrossRef] [PubMed]
- Gregers, T.F.; Fleckenstein, B.; Vartdal, F.; Roepstorff, P.; Bakke, O.; Sandlie, I. MHC class II loading of high or low affinity peptides directed by Ii/peptide fusion constructs: Implications for T cell activation. Int. Immunol. 2003, 15, 1291–1299. [Google Scholar] [CrossRef][Green Version]
- Sun, B.; Zhang, J.; Li, Z.; Xie, M.; Luo, C.; Wang, Y.; Chen, L.; Wang, Y.; Jiang, D.; Yang, K. Integration: Gospel for immune bioinformatician on epitope-based therapy. Front. Immunol. 2023, 14, 1075419. [Google Scholar] [CrossRef]
- Salod, Z.; Mahomed, O. Mapping Potential Vaccine Candidates Predicted by VaxiJen for Different Viral Pathogens between 2017–2021—A Scoping Review. Vaccines 2022, 10, 1785. [Google Scholar] [CrossRef]
- Sun, B.; Zhang, J.; Wang, J.; Liu, Y.; Sun, H.; Lu, Z.; Chen, L.; Ding, X.; Pan, J.; Hu, C.; et al. Comparative Immunoreactivity Analyses of Hantaan Virus Glycoprotein-Derived MHC-I Epitopes in Vaccination. Vaccines 2022, 10, 564. [Google Scholar] [CrossRef]
- Sun, H.; Lu, Z.; Xuan, G.; Liu, N.; Wang, T.; Liu, Y.; Lan, M.; Xu, J.; Feng, Y.; Xu, S.; et al. Integrative Analysis of HTNV Glycoprotein Derived MHC II Epitopes by In Silico Prediction and Experimental Validation. Front. Cell. Infect. Microbiol. 2021, 11, 671694. [Google Scholar] [CrossRef]
- Vijayan, R.; Subbarao, N.; Manoharan, N. In Silico Analysis of Conformational Changes Induced by Normal and Mutation of Macrophage Infectivity Potentiator Catalytic Residues and its Interactions with Rapamycin. Interdiscip. Sci. Comput. Life Sci. 2015, 7, 326–333. [Google Scholar] [CrossRef]
- Patronov, A.; Dimitrov, I.; Flower, D.R.; Doytchinova, I. Peptide binding prediction for the human class II MHC allele HLA-DP2: A molecular docking approach. BMC Struct. Biol. 2011, 11, 32. [Google Scholar] [CrossRef]
- Shukla, P.; Pandey, P.; Prasad, B.; Robinson, T.; Purohit, R.; D’Cruz, L.G.; Tambuwala, M.M.; Mutreja, A.; Harkin, J.; Rai, T.S.; et al. Immuno-informatics analysis predicts B and T cell consensus epitopes for designing peptide vaccine against SARS-CoV-2 with 99.82% global population coverage. Brief. Bioinform. 2022, 23, bbab496. [Google Scholar] [CrossRef] [PubMed]
- Lohia, N.; Baranwal, M. An Immunoinformatics Approach in Design of Synthetic Peptide Vaccine Against Influenza Virus. Immunoinformatics 2020, 2131, 229–243. [Google Scholar] [CrossRef]
- Randolph, H.E.; Barreiro, L.B. Herd Immunity: Understanding COVID-19. Immunity 2020, 52, 737–741. [Google Scholar] [CrossRef]
- Mehra, N.K.; Kaur, G. MHC-based vaccination approaches: Progress and perspectives. Expert Rev. Mol. Med. 2003, 5, 1–17. [Google Scholar] [CrossRef]
- Gulukota, K.; DeLisi, C. HLA allele selection for designing peptide vaccines. Genet. Anal. Biomol. Eng. 1996, 13, 81–86. [Google Scholar] [CrossRef] [PubMed]
- Eskelinen, E.-L. Roles of LAMP-1 and LAMP-2 in lysosome biogenesis and autophagy. Mol. Asp. Med. 2006, 27, 495–502. [Google Scholar] [CrossRef]
- Carlsson, S.R.; Fukuda, M. Structure of human lysosomal membrane glycoprotein 1. Assignment of disulfide bonds and visualization of its domain arrangement. J. Biol. Chem. 1989, 264, 20526–20531. [Google Scholar] [CrossRef]
- Gupta, V.; Tabiin, T.M.; Sun, K.; Chandrasekaran, A.; Anwar, A.; Yang, K.; Chikhlikar, P.; Salmon, J.; Brusic, V.; Marques, E.T.; et al. SARS coronavirus nucleocapsid immunodominant T-cell epitope cluster is common to both exogenous recombinant and endogenous DNA-encoded immunogens. Virology 2006, 347, 127–139. [Google Scholar] [CrossRef]
- Gilbert, P.B.; Montefiori, D.C.; McDermott, A.B.; Fong, Y.; Benkeser, D.; Deng, W.; Zhou, H.; Houchens, C.R.; Martins, K.; Jayashankar, L.; et al. Immune correlates analysis of the mRNA-1273 COVID-19 vaccine efficacy clinical trial. Science 2022, 375, 43–50. [Google Scholar] [CrossRef]
- Sette, A.; Moutaftsi, M.; Moyron-Quiroz, J.; McCausland, M.M.; Davies, D.H.; Johnston, R.J.; Peters, B.; Benhnia, M.R.-E.; Hoffmann, J.; Su, H.-P.; et al. Selective CD4+ T cell help for antibody responses to a large viral pathogen: Deterministic linkage of specificities. Immunity 2008, 28, 847–858. [Google Scholar] [CrossRef]
- Li, P.; Gregg, J.L.; Wang, N.; Zhou, D.; O’Donnell, P.; Blum, J.S.; Crotzer, V.L. Compartmentalization of class II antigen presentation: Contribution of cytoplasmic and endosomal processing. Immunol. Rev. 2005, 207, 206–217. [Google Scholar] [CrossRef] [PubMed]
- Czerkinsky, C.; Andersson, G.; Ekre, H.-P.; Nilsson, L.; Klareskog, L.; Ouchterlony, Ö. Reverse ELISPOT assay for clonal analysis of cytokine production I. Enumeration of gamma-interferon-secreting cells. J. Immunol. Methods 1988, 110, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Chong, M.M.W.; Littman, D.R. Plasticity of CD4+ T cell lineage differentiation. Immunity 2009, 30, 646–655. [Google Scholar] [CrossRef] [PubMed]


| MHC-Ⅱ Haplotypes | Prediction Tools | GP Epitopes | GP (Short Listed) |
|---|---|---|---|
| H2-A | IEDB | 19 + 4(b, d) | 121 |
| NetMHCⅡpan | 5 + 1 + 5 + 2 + 3 + 3(b, d, k, q, s, u) | ||
| Rankpep | 13 + 13 + 14 + 14 + 14 + 14(b, d, k, q, s, u) | ||
| SYFPEITHI | 66 + 10(d, k) | ||
| H2-E | IEDB | 8(d) | 89 |
| NetMHCⅡpan | 4 + 3(d, k) | ||
| Rankpep | 14 + 13 + 14 + 14(b, d, k, s) | ||
| SYFPEITHI | 18 + 35(d, k) | ||
| DRB1 | IEDB | 32 | 43 |
| NetMHCⅡpan | 36 | ||
| Rankpep | 19 | ||
| SYFPEITHI | 26 | ||
| DRB3/4/5 | IEDB | 30 | 31 |
| NetMHCⅡpan | 31 | ||
| Rankpep | 3 | ||
| SYFPEITHI | 0 | ||
| DQ | IEDB | 15 | 19 |
| NetMHCⅡpan | 15 | ||
| Rankpep | 8 | ||
| SYFPEITHI | 0 | ||
| DP | IEDB | 13 | 8 |
| NetMHCⅡpan | 13 | ||
| Rankpep | 0 | ||
| SYFPEITHI | 0 |
| MHC-II Haplotypes | Interspecies− Intraspecies+ | Interspecies+Intraspecies+ |
|---|---|---|
| DRB1 | 13 | 30 |
| DRB3/4/5 | 13 | 18 |
| DQA1/DQB1 | 6 | 13 |
| DPB1 | 0 | 8 |
| H2-A | 65 | 87 |
| H2-E | 19 | 63 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, J.; Sun, B.; Shen, W.; Wang, Z.; Liu, Y.; Sun, Y.; Zhang, J.; Liu, R.; Wang, Y.; Bai, T.; et al. In Silico Analyses, Experimental Verification and Application in DNA Vaccines of Ebolavirus GP-Derived pan-MHC-II-Restricted Epitopes. Vaccines 2023, 11, 1620. https://doi.org/10.3390/vaccines11101620
Zhang J, Sun B, Shen W, Wang Z, Liu Y, Sun Y, Zhang J, Liu R, Wang Y, Bai T, et al. In Silico Analyses, Experimental Verification and Application in DNA Vaccines of Ebolavirus GP-Derived pan-MHC-II-Restricted Epitopes. Vaccines. 2023; 11(10):1620. https://doi.org/10.3390/vaccines11101620
Chicago/Turabian StyleZhang, Junqi, Baozeng Sun, Wenyang Shen, Zhenjie Wang, Yang Liu, Yubo Sun, Jiaxing Zhang, Ruibo Liu, Yongkai Wang, Tianyuan Bai, and et al. 2023. "In Silico Analyses, Experimental Verification and Application in DNA Vaccines of Ebolavirus GP-Derived pan-MHC-II-Restricted Epitopes" Vaccines 11, no. 10: 1620. https://doi.org/10.3390/vaccines11101620
APA StyleZhang, J., Sun, B., Shen, W., Wang, Z., Liu, Y., Sun, Y., Zhang, J., Liu, R., Wang, Y., Bai, T., Ma, Z., Luo, C., Qiao, X., Zhang, X., Yang, S., Sun, Y., Jiang, D., & Yang, K. (2023). In Silico Analyses, Experimental Verification and Application in DNA Vaccines of Ebolavirus GP-Derived pan-MHC-II-Restricted Epitopes. Vaccines, 11(10), 1620. https://doi.org/10.3390/vaccines11101620