Inactivated Recombinant Rabies Virus Displaying the Nipah Virus Envelope Glycoproteins Induces Systemic Immune Responses in Mice
Abstract
:1. Introduction
2. Materials and Methods
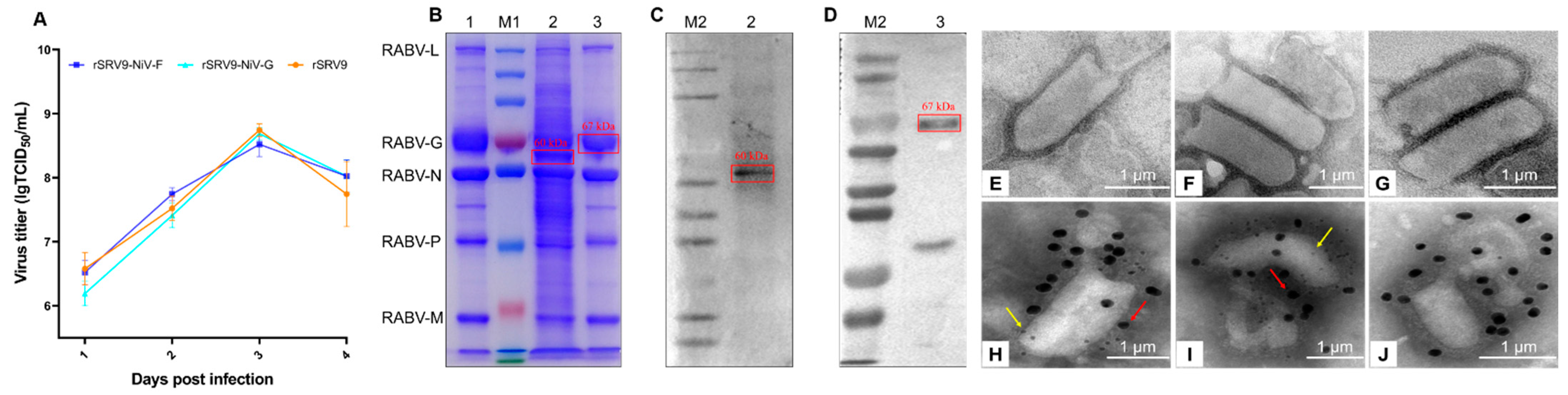
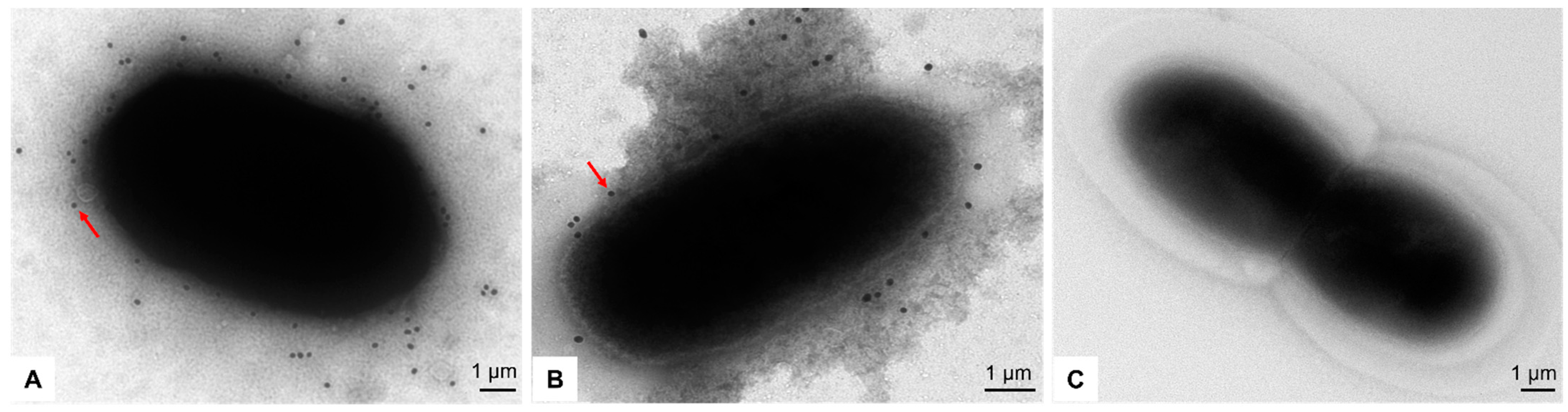
2.1. Identification of Recombinant RABVs Displaying the F or G proteins of NiV
2.1.1. Rescue of Recombinant RABVs Displaying the F or G Proteins of NiV
2.1.2. Direct Immunofluorescence
2.1.3. Indirect Immunofluorescence
2.1.4. Sucrose Density Gradient Centrifugation
2.1.5. Western Blotting
2.1.6. Transmission Electron Microscopy
2.1.7. Immunoelectron Microscopy
2.1.8. Multi-Step Growth Kinetic Curve
2.2. Analysis of Recombinant RABVs Displaying the F or G Proteins of NiV
2.2.1. Preparation of Immunogen
2.2.2. Immunization of Mice
2.2.3. Splenic Lymphocyte Proliferation Assay
2.2.4. Cytokine Detections by ELISA and ELISpot
2.2.5. Indirect ELISA
2.3. Preparation of the Bacterial-Like Particles Displaying the F or G Proteins of NiV
2.3.1. Rescue of Recombinant Baculovirus
2.3.2. Preparation of Gram-Positive Enhancer Matrix Particles
2.3.3. Construction of the Bacterial-Like Particles
2.4. Cross-Reaction between the Recombinant RABVs and the BLPs
2.5. Statistical Analysis
3. Results
3.1. Identification of Recombinant RABVs Displaying the F or G Proteins of NiV
3.2. The Immunogenicity of Recombinant RABVs Displaying the F or G Proteins of NiV
3.3. The Reactivity of the Immune Sera against Recombinant RABVs Displaying the F or G Proteins of NiV
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Devnath, P.; Wajed, S.; Das, R.C.; Kar, S.; Islam, I.; Masud, H. The pathogenesis of Nipah virus: A review. Microb. Pathog. 2022, 170, 105693. [Google Scholar] [CrossRef]
- Alam, A.M. Nipah virus, an emerging zoonotic disease causing fatal encephalitis. Clin. Med. 2022, 22, 348–352. [Google Scholar] [CrossRef] [PubMed]
- Liew, Y.J.M.; Ibrahim, P.A.S.; Ong, H.M.; Chong, C.N.; Tan, C.T.; Schee, J.P.; Román, R.G.; Cherian, N.G.; Wong, W.F.; Chang, L.-Y. The Immunobiology of Nipah Virus. Microorganisms 2022, 10, 1162. [Google Scholar] [CrossRef] [PubMed]
- Johnson, K.; Vu, M.; Freiberg, A.N. Recent advances in combating Nipah virus. Fac. Rev. 2021, 10, 74. [Google Scholar] [CrossRef] [PubMed]
- Draper, S.J.; Heeney, J.L. Viruses as vaccine vectors for infectious diseases and cancer. Nat. Rev. Microbiol. 2010, 8, 62–73. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.K.; Dhama, K.; Chakraborty, S.; Tiwari, R.; Natesan, S.; Khandia, R.; Mourya, D.T. Nipah virus: Epidemiology, pathology, immunobiology and advances in diagnosis, vaccine designing and control strategies—A comprehensive review. Vet. Q. 2019, 39, 26–55. [Google Scholar] [CrossRef]
- Monath, T.P.; Nichols, R.; Tussey, L.; Scappaticci, K.; Pullano, T.G.; Whiteman, M.D.; Vasilakis, N.; Rossi, S.L.; Campos, R.K.; Azar, S.R.; et al. Recombinant vesicular stomatitis vaccine against Nipah virus has a favorable safety profile: Model for assessment of live vaccines with neurotropic potential. PLoS Pathog. 2022, 18, e1010658. [Google Scholar] [CrossRef]
- Kurup, D.; Fisher, C.R.; Smith, T.G.; Abreu-Mota, T.; Yang, Y.; Jackson, F.R.; Gallardo-Romero, N.; Franka, R.; Bronshtein, V.; Schnell, M.J. Inactivated Rabies Virus-Based Ebola Vaccine Preserved by Vaporization Is Heat-Stable and Immunogenic against Ebola and Protects Against Rabies Challenge. J. Infect. Dis. 2019, 220, 1521–1528. [Google Scholar] [CrossRef]
- Kurup, D.; Fisher, C.R.; Scher, G.; Yankowski, C.; Testa, A.; Keshwara, R.; Abreu-Mota, T.; Lambert, R.; Ferguson, M.; Rinaldi, W.; et al. Tetravalent Rabies-Vectored Filovirus and Lassa Fever Vaccine Induces Long-term Immunity in Nonhuman Primates. J. Infect. Dis. 2021, 224, 995–1004. [Google Scholar] [CrossRef]
- Chi, H.; Zheng, X.; Wang, X.; Wang, C.; Wang, H.; Gai, W.; Perlman, S.; Yang, S.; Zhao, J.; Xia, X. DNA vaccine encoding Middle East respiratory syndrome coronavirus S1 protein induces protective immune responses in mice. Vaccine 2017, 35, 2069–2075. [Google Scholar] [CrossRef]
- Jin, H.; Jiao, C.; Cao, Z.; Huang, P.; Chi, H.; Bai, Y.; Liu, D.; Wang, J.; Feng, N.; Li, N.; et al. An inactivated recombinant rabies virus displaying the Zika virus prM-E induces protective immunity against both pathogens. PLoS Negl. Trop. Dis. 2021, 15, e0009484. [Google Scholar] [CrossRef] [PubMed]
- Loomis, R.J.; DiPiazza, A.T.; Falcone, S.; Ruckwardt, T.J.; Morabito, K.M.; Abiona, O.M.; Chang, L.A.; Caringal, R.T.; Presnyak, V.; Narayanan, E.; et al. Chimeric Fusion (F) and Attachment (G) Glycoprotein Antigen Delivery by mRNA as a Candidate Nipah Vaccine. Front. Immunol. 2021, 12, 772864. [Google Scholar] [CrossRef] [PubMed]
- Foster, S.L.; Woolsey, C.; Borisevich, V.; Agans, K.N.; Prasad, A.N.; Deer, D.J.; Geisbert, J.B.; Dobias, N.S.; Fenton, K.A.; Cross, R.W.; et al. A recombinant VSV-vectored vaccine rapidly protects nonhuman primates against lethal Nipah virus disease. Proc. Natl. Acad. Sci. USA 2022, 119, e2200065119. [Google Scholar] [CrossRef] [PubMed]
- Isaacs, A.; Cheung, S.T.M.; Thakur, N.; Jaberolansar, N.; Young, A.; Modhiran, N.; Bailey, D.; Graham, S.P.; Young, P.R.; Chappell, K.J.; et al. Combinatorial F-G Immunogens as Nipah and Respiratory Syncytial Virus Vaccine Candidates. Viruses 2021, 13, 1942. [Google Scholar] [CrossRef]
- Wang, H.; Jin, H.; Feng, N.; Zheng, X.; Li, L.; Qi, Y.; Liang, M.; Zhao, Y.; Wang, T.; Gao, Y.; et al. Using rabies virus vaccine strain SRV9 as viral vector to express exogenous gene. Virus Genes 2015, 50, 299–302. [Google Scholar] [CrossRef]
- Coons, A.H. The beginnings of immunofluorescence. J. Immunol. 1961, 87, 499–503. [Google Scholar] [CrossRef]
- Topleninova, K.A. The application of the indirect fluorescent antibody method to detect rabies virus. Probl. Virol. 1961, 6, 190–193. [Google Scholar]
- Jin, H.; Bai, Y.; Wang, J.; Jiao, C.; Liu, D.; Zhang, M.; Li, E.; Huang, P.; Gong, Z.; Song, Y.; et al. A bacterium-like particle vaccine displaying Zika virus prM-E induces systemic immune responses in mice. Transbound. Emerg. Dis. 2022, 69, e2516–e2529. [Google Scholar] [CrossRef]
- Neurath, A.R.; Wiktor, T.J.; Koprowski, H. Density gradient centrifugation studies on rabies virus. J. Bacteriol. 1966, 92, 102–106. [Google Scholar] [CrossRef]
- Burnette, W.N. “Western blotting”: Electrophoretic transfer of proteins from sodium dodecyl sulfate--polyacrylamide gels to unmodified nitrocellulose and radiographic detection with antibody and radioiodinated protein A. Anal. Biochem. 1981, 112, 195–203. [Google Scholar] [CrossRef]
- Tizro, P.; Choi, C.; Khanlou, N. Sample Preparation for Transmission Electron Microscopy. Methods Mol. Biol. 2019, 1897, 417–424. [Google Scholar] [PubMed]
- Squarzoni, S.; Sabatelli, P.; Ognibene, A.; Toniolo, D.; Cartegni, L.; Cobianchi, F.; Petrini, S.; Merlini, L.; Maraldi, N. Immunocytochemical detection of emerin within the nuclear matrix. Neuromuscul. Disord. 1998, 8, 338–344. [Google Scholar] [CrossRef] [PubMed]
- Reed, L.J.; Muench, H. A simple method of estimating fifty percent endpoints. Am. J. Hyg. 1938, 27, 493–497. [Google Scholar]
- Du, X.; Zheng, G.; Jin, H.; Kang, Y.; Wang, J.; Xiao, C.; Zhang, S.; Zhao, L.; Chen, A.; Wang, B. The adjuvant effects of co-stimulatory molecules on cellular and memory responses to HBsAg DNA vaccination. J. Gene Med. 2007, 9, 136–146. [Google Scholar] [CrossRef] [PubMed]
- Engvall, E.; Perlmann, P. Enzyme-linked immunosorbent assay (ELISA). Quantitative assay of immunoglobulin G. Immunochemistry 1971, 8, 871–874. [Google Scholar] [CrossRef]
- Satterfield, B.A.; Dawes, B.E.; Milligan, G.N. Status of vaccine research and development of vaccines for Nipah virus. Vaccine 2016, 34, 2971–2975. [Google Scholar] [CrossRef]
- Nimmerjahn, F.; Ravetch, J.V. Divergent immunoglobulin g subclass activity through selective Fc receptor binding. Science 2005, 310, 1510–1512. [Google Scholar] [CrossRef]
- Forthal, D.N.; Moog, C. Fc receptor-mediated antiviral antibodies. Curr. Opin. HIV AIDS 2009, 4, 388–393. [Google Scholar] [CrossRef]
- Leeansyah, E.; Wines, B.D.; Crowe, S.M.; Jaworowski, A. The mechanism underlying defective Fcgamma receptor-mediated phagocytosis by HIV-1-infected human monocyte-derived macrophages. J. Immunol. 2007, 178, 1096–1104. [Google Scholar] [CrossRef]
- Pelegrin, M.; Naranjo-Gomez, M.; Piechaczyk, M. Antiviral Monoclonal Antibodies: Can They Be More Than Simple Neutralizing Agents? Trends Microbiol. 2015, 23, 653–665. [Google Scholar] [CrossRef]
- Liu, Q.; Fan, C.; Li, Q.; Zhou, S.; Huang, W.; Wang, L.; Sun, C.; Wang, M.; Wu, X.; Ma, J.; et al. Antibody-dependent-cellular-cytotoxicity-inducing antibodies significantly affect the post-exposure treatment of Ebola virus infection. Sci. Rep. 2017, 7, 45552. [Google Scholar] [CrossRef]
- Rockx, B. Recent developments in experimental animal models of Henipavirus infection. Pathog. Dis. 2014, 71, 199–206. [Google Scholar] [CrossRef] [PubMed]
- Dhondt, K.P.; Horvat, B. Henipavirus infections: Lessons from animal models. Pathogens 2013, 2, 264–287. [Google Scholar] [CrossRef] [PubMed]
- Guillaume, V.; Contamin, H.; Loth, P.; Georges-Courbot, M.-C.; Lefeuvre, A.; Marianneau, P.; Chua, K.B.; Lam, S.K.; Buckland, R.; Deubel, V.; et al. Nipah virus: Vaccination and passive protection studies in a hamster model. J. Virol. 2004, 78, 834–840. [Google Scholar] [CrossRef] [PubMed]
- Weingartl, H.M.; Berhane, Y.; Caswell, J.L.; Loosmore, S.; Audonnet, J.C.; Roth, J.A.; Czub, M. Recombinant nipah virus vaccines protect pigs against challenge. J. Virol. 2006, 80, 7929–7938. [Google Scholar] [CrossRef]
- Mire, C.E.; Versteeg, K.M.; Cross, R.W.; Agans, K.N.; Fenton, K.A.; Whitt, M.A.; Geisbert, T.W. Single injection recombinant vesicular stomatitis virus vaccines protect ferrets against lethal Nipah virus disease. Virol. J. 2013, 10, 353. [Google Scholar] [CrossRef]
- Lo, M.K.; Bird, B.H.; Chattopadhyay, A.; Drew, C.P.; Martin, B.E.; Coleman, J.D.; Rose, J.K.; Nichol, S.T.; Spiropoulou, C.F. Single-dose replication-defective VSV-based Nipah virus vaccines provide protection from lethal challenge in Syrian hamsters. Antivir. Res. 2014, 101, 26–29. [Google Scholar] [CrossRef]
- Yoneda, M.; Georges-Courbot, M.-C.; Ikeda, F.; Ishii, M.; Nagata, N.; Jacquot, F.; Raoul, H.; Sato, H.; Kai, C. Recombinant measles virus vaccine expressing the Nipah virus glycoprotein protects against lethal Nipah virus challenge. PLoS ONE 2013, 8, e58414. [Google Scholar] [CrossRef]




| Primers | Sequence (5′ → 3′) |
|---|---|
| NiV/F-F | GACCGTACGGCCACCATGGCAGTTATACTTAACAAGAGAT |
| NiV/F-R | GGCGTTTAAACCTACGTCCCAATGTAATAGAGATCC |
| NiV/G-F | TAGCGTACGGCCACCATGCCGACAGAAAGCAAGAAAGTTA |
| NiV/G-R | CAAGTTTAAACTTATGTACATTGCTCTGGTATCTTA |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, Z.; Zhu, Y.; Yan, F.; Jin, H.; Wang, Q.; Zhao, Y.; Feng, N.; Wang, T.; Li, N.; Yang, S.; et al. Inactivated Recombinant Rabies Virus Displaying the Nipah Virus Envelope Glycoproteins Induces Systemic Immune Responses in Mice. Vaccines 2023, 11, 1758. https://doi.org/10.3390/vaccines11121758
Li Z, Zhu Y, Yan F, Jin H, Wang Q, Zhao Y, Feng N, Wang T, Li N, Yang S, et al. Inactivated Recombinant Rabies Virus Displaying the Nipah Virus Envelope Glycoproteins Induces Systemic Immune Responses in Mice. Vaccines. 2023; 11(12):1758. https://doi.org/10.3390/vaccines11121758
Chicago/Turabian StyleLi, Zhengrong, Yanting Zhu, Feihu Yan, Hongli Jin, Qi Wang, Yongkun Zhao, Na Feng, Tiecheng Wang, Nan Li, Songtao Yang, and et al. 2023. "Inactivated Recombinant Rabies Virus Displaying the Nipah Virus Envelope Glycoproteins Induces Systemic Immune Responses in Mice" Vaccines 11, no. 12: 1758. https://doi.org/10.3390/vaccines11121758
APA StyleLi, Z., Zhu, Y., Yan, F., Jin, H., Wang, Q., Zhao, Y., Feng, N., Wang, T., Li, N., Yang, S., Xia, X., & Cong, Y. (2023). Inactivated Recombinant Rabies Virus Displaying the Nipah Virus Envelope Glycoproteins Induces Systemic Immune Responses in Mice. Vaccines, 11(12), 1758. https://doi.org/10.3390/vaccines11121758




