Assessing Barriers to Human Papillomavirus (HPV) Vaccination in At-Risk Rural Communities of Western North Carolina, United States
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- De Villiers, E.-M.; Fauquet, C.; Broker, T.R.; Bernard, H.-U.; zur Hausen, H. Classification of papillomaviruses. Virology 2004, 324, 17–27. [Google Scholar] [CrossRef] [PubMed]
- Petrosky, E.; Bocchini, J.A.; Hariri, S.; Chesson, H.; Curtis, C.R.; Saraiya, M.; Unger, E.R.; Markowitz, L.E.; Centers for Disease Control and Prevention (CDC). Use of 9-valent human papillomavirus (HPV) vaccine: Updated HPV vaccination recommendations of the advisory committee on immunization practices. MMWR Morb. Mortal. Wkly. Rep. 2015, 64, 300–304. [Google Scholar] [PubMed]
- Meites, E.; Kempe, A.; Markowitz, L.E. Use of a 2-Dose Schedule for Human Papillomavirus Vaccination—Updated Recommendations of the Advisory Committee on Immunization Practices. MMWR Morb. Mortal. Wkly. Rep. 2016, 65, 1405–1408. [Google Scholar] [CrossRef] [PubMed]
- Kreisel, K.M.; Spicknall, I.H.; Gargano, J.W.; Lewis, F.M.T.; Lewis, R.M.; Markowitz, L.E.; Roberts, H.; Johnson, A.S.; Song, R.; St Cyr, S.B.; et al. Sexually Transmitted Infections Among US Women and Men: Prevalence and Incidence Estimates, 2018. Sex Transm. Dis. 2021, 48, 208–214. [Google Scholar] [CrossRef]
- Hirth, J. Disparities in HPV vaccination rates and HPV prevalence in the United States: A review of the literature. Hum. Vaccines Immunother. 2019, 15, 146–155. [Google Scholar] [CrossRef]
- Office of Disease Prevention and Health Promotion. Social Determinants of Health. Healthy People 2030. U.S. Department of Health and Human Services. Available online: https://health.gov/healthypeople/objectives-and-data/social-determinants-health (accessed on 12 August 2023).
- Elam-Evans, L.D.; Yankey, D.; Singleton, J.A.; Sterrett, N.; Markowitz, L.E.; Williams, C.L.; Fredua, B.; McNamara, L.; Stokley, S. National, Regional, State, and Selected Local Area Vaccination Coverage Among Adolescents Aged 13–17 Years—United States, 2019. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1109–1116. [Google Scholar] [CrossRef]
- Holman, D.M.; Benard, V.; Roland, K.B.; Watson, M.; Liddon, N.; Stokley, S. Barriers to human papillomavirus vaccination among US adolescents: A systematic review of the literature. JAMA Pediatr. 2014, 168, 76–82. [Google Scholar] [CrossRef]
- Walker, T.Y.; Elam-Evans, L.D.; Yankey, D.; Markowitz, L.E.; Williams, C.L.; Fredua, B.; Singleton, J.A.; Stokley, S. National, Regional, State, and Selected Local Area Vaccination Coverage Among Adolescents Aged 13–17 Years—United States, 2018. MMWR Morb. Mortal. Wkly. Rep. 2019, 68, 718–723. [Google Scholar] [CrossRef]
- Rosen, B.L.; Shepard, A.; Kahn, J.A. US Health Care Clinicians’ Knowledge, Attitudes, and Practices Regarding Human Papillomavirus Vaccination: A Qualitative Systematic Review. Acad. Pediatr. 2018, 18, S53–S65. [Google Scholar] [CrossRef]
- Allen, J.D.; Othus, M.K.; Shelton, R.C.; Li, Y.; Norman, N.; Tom, L.; del Carmen, M.G. Parental decision making about the HPV vaccine. Cancer Epidemiol. Biomark. Prev. 2010, 19, 2187–2198. [Google Scholar] [CrossRef]
- Sonawane, K.; Zhu, Y.; Montealegre, J.R.; Lairson, D.R.; Bauer, C.; McGee, L.U.; Giuliano, A.R.; Deshmukh, A.A. Parental intent to initiate and complete the human papillomavirus vaccine series in the USA: A nationwide, cross-sectional survey. Lancet Public Health 2020, 5, e484–e492. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. AFIX (Assessment, Feedback, Incentives, and eXchange). Available online: https://stacks.cdc.gov/view/cdc/26473 (accessed on 12 August 2023).
- Heckathorn, D.D.; Cameron, C.J. Network Sampling: From Snowball and Multiplicity to Respondent-Driven Sampling. Annu. Rev. Sociol. 2017, 43, 101–119. [Google Scholar] [CrossRef]
- Dempsey, A.F.; Fuhrel-Forbis, A.; Konrath, S. Use of the Carolina HPV Immunization Attitudes and Beliefs Scale (CHIAS) in young adult women. PLoS ONE 2014, 9, e100193. [Google Scholar] [CrossRef]
- McRee, A.L.; Brewer, N.T.; Reiter, P.L.; Gottlieb, S.L.; Smith, J.S. The Carolina HPV immunization attitudes and beliefs scale (CHIAS): Scale development and associations with intentions to vaccinate. Sex Transm. Dis. 2010, 37, 234–239. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Rand, C.M.; Szilagyi, P.G.; Albertin, C.; Auinger, P. Additional health care visits needed among adolescents for human papillomavirus vaccine delivery within medical homes: A national study. Pediatrics 2007, 120, 461–466. [Google Scholar] [CrossRef]
- North Carolina General Assembly. § 90-21.5. Minor’s Consent Sufficient for Certain Medical Health Services. Available online: https://www.ncleg.gov/enactedlegislation/statutes/pdf/bysection/chapter_90/gs_90-21.5.pdf (accessed on 23 February 2023).
- Peterson, C.E.; Silva, A.; Holt, H.K.; Balanean, A.; Goben, A.H.; Dykens, J.A. Barriers and facilitators to HPV vaccine uptake among US rural populations: A scoping review. Cancer Causes Control 2020, 31, 801–814. [Google Scholar] [CrossRef] [PubMed]
- Fish, L.J.; Harrison, S.E.; McDonald, J.-A.; Yelverton, V.; Williams, C.; Walter, E.B.; Vasudevan, L. Key stakeholder perspectives on challenges and opportunities for rural HPV vaccination in North and South Carolina. Hum. Vaccines Immunother. 2022, 18, 2058264. [Google Scholar] [CrossRef]
- Dixon, B.E.; Zimet, G.D.; Xiao, S.; Tu, W.; Lindsay, B.; Church, A.; Downs, S.M. An Educational Intervention to Improve HPV Vaccination: A Cluster Randomized Trial. Pediatrics 2019, 143, e20181457. [Google Scholar] [CrossRef]
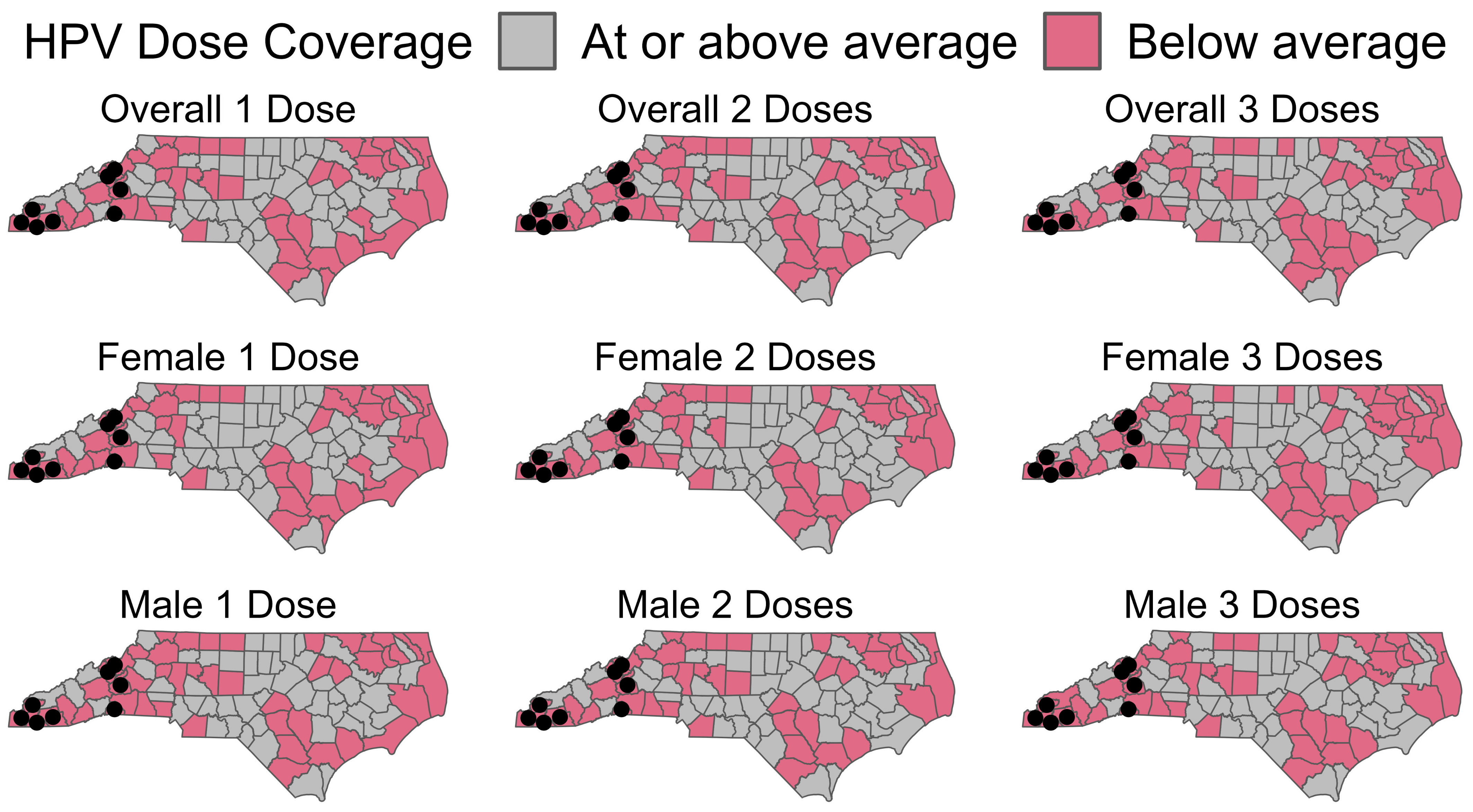
- Trogdon, J.G.; Ahn, T. Geospatial patterns in human papillomavirus vaccination uptake: Evidence from uninsured and publicly insured children in North Carolina. Cancer Epidemiol. Biomark. Prev. 2015, 24, 595–602. [Google Scholar] [CrossRef]
- Escoffery, C.; Riehman, K.; Watson, L.; Priess, A.S.; Borne, M.F.; Halpin, S.N.; Rhiness, C.; Wiggins, E.; Kegler, M.C. Facilitators and Barriers to the Implementation of the HPV VACs (Vaccinate Adolescents Against Cancers) Program: A Consolidated Framework for Implementation Research Analysis. Prev. Chronic Dis. 2019, 16, E85. [Google Scholar] [CrossRef]
- Brewer, N.T.; Hall, M.E.; Malo, T.L.; Gilkey, M.B.; Quinn, B.; Lathren, C. Announcements Versus Conversations to Improve HPV Vaccination Coverage: A Randomized Trial. Pediatrics 2017, 139, e20161764. [Google Scholar] [CrossRef]
- Gilkey, M.B.; McRee, A.L. Provider communication about HPV vaccination: A systematic review. Hum. Vaccines Immunother. 2016, 12, 1454–1468. [Google Scholar] [CrossRef]
- Zhu, X.; Jacobson, R.M.; MacLaughlin, K.L.; Sauver, J.S.; Griffin, J.M.; Finney Rutten, L.J. Parent-reported Barriers and Parental Beliefs Associated with Intentions to Obtain HPV Vaccination for Children in a Primary care Patient Population in Minnesota, USA. J. Community Health 2023, 48, 678–686. [Google Scholar] [CrossRef]
- Szilagyi, P.G.; Humiston, S.G.; Stephens-Shields, A.J.; Localio, R.; Breck, A.; Kelly, M.K.; Wright, M.; Grundmeier, R.W.; Albertin, C.; Shone, L.P.; et al. Effect of Training Pediatric Clinicians in Human Papillomavirus Communication Strategies on Human Papillomavirus Vaccination Rates: A Cluster Randomized Clinical Trial. JAMA Pediatr. 2021, 175, 901–910. [Google Scholar] [CrossRef]
- Shato, T.; Humble, S.; Anandarajah, A.; Barnette, A.; Brandt, H.M.; Garbutt, J.; Klesges, L.; Thompson, V.S.; Silver, M.I. Influences of sociodemographic characteristics and parental HPV vaccination hesitancy on HPV vaccination coverage in five US states. Vaccine 2023, 41, 3772–3781. [Google Scholar] [CrossRef]
- Rodriguez, S.A.; Mullen, P.D.; Lopez, D.M.; Savas, L.S.; Fernández, M.E. Factors associated with adolescent HPV vaccination in the U.S.: A systematic review of reviews and multilevel framework to inform intervention development. Prev. Med. 2020, 131, 105968. [Google Scholar] [CrossRef]
- Chido-Amajuoyi, O.G.; Talluri, R.; Wonodi, C.; Shete, S. Trends in HPV Vaccination Initiation and Completion Within Ages 9–12 Years: 2008–2018. Pediatrics 2021, 147, e2020012765. [Google Scholar] [CrossRef]
- Constable, C.; Caplan, A. Comparison of the implementation of human papillomavirus and hepatitis B vaccination programs in the United States: Implications for future vaccines. Vaccine 2020, 38, 954–962. [Google Scholar] [CrossRef]
- Johnson, K.L.; Lin, M.Y.; Cabral, H.; Kazis, L.E.; Katz, I.T. Variation in Human Papillomavirus Vaccine Uptake and Acceptability Between Female and Male Adolescents and Their Caregivers. J. Community Health 2017, 42, 522–532. [Google Scholar] [CrossRef]
- Sonawane, K.; Zhu, Y.; Lin, Y.Y.; Damgacioglu, H.; Lin, Y.; Montealegre, J.R.; Deshmukh, A.A. HPV Vaccine Recommendations and Parental Intent. Pediatrics 2021, 147, e2020026286. [Google Scholar] [CrossRef] [PubMed]
- Abouelella, D.K.; Canick, J.E.; Barnes, J.M.; Rohde, R.L.; Watts, T.L.; Adjei Boakye, E.; Osazuwa-Peters, N. Human papillomavirus vaccine uptake among teens before and during the COVID-19 pandemic in the United States. Hum. Vaccines Immunother. 2022, 18, 2148825. [Google Scholar] [CrossRef] [PubMed]
- Calo, W.A.; Lennon, R.P.; Ruffin Iv, M.T.; Keller, C.; Spanos, K.; D’Souza, G.; Kraschnewski, J.L. Support for HPV vaccine school-entry requirements in the United States: The role of exemption policies. Vaccine 2022, 40, 7426–7432. [Google Scholar] [CrossRef] [PubMed]


| Characteristic | Parent, N = 32 1 | Provider, N = 29 1 |
|---|---|---|
| Age | 36 (31, 41) | 37 (30, 50) |
| Unknown | 3 | 0 |
| Ethnicity | ||
| Hispanic or Latino | 5 (16%) | 1 (3.6%) |
| Non-Hispanic or Latino | 26 (81%) | 27 (96%) |
| Other | 1 (3.1%) | 0 (0%) |
| Unknown | 0 | 1 |
| Race | ||
| White alone | 29 (91%) | 27 (96%) |
| Black or African American | 1 (3.1%) | 0 (0%) |
| Multiracial | 1 (3.1%) | 0 (0%) |
| Other | 1 (3.1%) | 1 (3.6%) |
| Unknown | 0 | 1 |
| Gender | ||
| Female | 26 (84%) | 27 (96%) |
| Male | 5 (16%) | 1 (3.6%) |
| Unknown | 1 | 1 |
| County | ||
| Cherokee | 5 (16%) | 5 (17%) |
| Clay | 6 (19%) | 5 (17%) |
| Graham | 5 (16%) | 3 (10%) |
| Macon | 7 (22%) | 5 (17%) |
| McDowell | 5 (16%) | 5 (17%) |
| Polk | 4 (12%) | 5 (17%) |
| Yancey | 0 (0%) | 1 (3.4%) |
| Position, n (%) | Who Provided you with this survey today? | Number of Staff |
| MD/DO 2 | 0 (0) | 2 (6.9) |
| Physician Assistant | 0 (0) | 1 (3.4) |
| Nurse Practitioner | 0 (0) | 3 (10) |
| Nurse | 24 (75) | 20 (69) |
| Front desk/scheduling | 5 (16) | 1 (3.4) |
| Other | 3 (9.4) | 2 (6.9) |
| Provider/staff reported clinic characteristics | |
| What is the estimated patient volume per day in your practice setting?, Median (IQR) | 35 (20–50) |
| Unknown | 1 |
| What is the estimated volume of patients that are seen for vaccines per day in your practice setting?, Median (IQR) | 14 (10–20) |
| Unknown | 1 |
| Parent reported clinic characteristics | |
| How many times have you visited this clinic in the last year? | 2 (1, 3) |
| Unknown | 2 |
| How many times have you visited this clinic for vaccinations? | 2 (1, 2) |
| Unknown | 2 |
| Where do you get most of your health information? | |
| Friends or family | 1 (3.1%) |
| Health Care Provider/Doctor’s Office | 15 (47%) |
| Health Department | 2 (6.2%) |
| Online/Internet | 8 (25%) |
| Other | 6 (19%) |
| The child attending the visit today is ___________. | |
| Female | 20 (65%) |
| Male | 11 (35%) |
| Unknown | 1 |
| Characteristic | Female, N = 20 | Male, N = 11 | p-Value 1 |
|---|---|---|---|
| How effective do you think the HPV vaccine is in preventing genital warts? n (%) | 0.18 | ||
| Slightly effective | 3 (15) | 0 (0) | |
| Moderately | 4 (20) | 5 (62) | |
| Very | 9 (45) | 2 (25) | |
| Extremely effective | 4 (20) | 1 (12) | |
| Unknown | 0 | 3 | |
| How effective do you think the HPV vaccine is in preventing cancer of the genitals (penis, vulva, vagina, cervix), n (%) | 0.79 | ||
| Slightly effective | 2 (10) | 1 (11) | |
| Moderately | 5 (25) | 4 (44) | |
| Very | 9 (45) | 3 (33) | |
| Extremely effective | 4 (20) | 1 (11) | |
| Unknown | 0 | 2 | |
| How effective do you think the HPV vaccine is in preventing cancer of the anus?, n (%) | 0.74 | ||
| Slightly effective | 2 (11) | 2 (25) | |
| Moderately | 5 (26) | 3 (38) | |
| Very | 8 (42) | 2 (25) | |
| Extremely effective | 4 (21) | 1 (12) | |
| Unknown | 1 | 3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
McNeil, C.J.; Barr, B.; Munawar, I.; DeWitt, M.E.; Myers, J.S.; Shetty, A.K. Assessing Barriers to Human Papillomavirus (HPV) Vaccination in At-Risk Rural Communities of Western North Carolina, United States. Vaccines 2023, 11, 1785. https://doi.org/10.3390/vaccines11121785
McNeil CJ, Barr B, Munawar I, DeWitt ME, Myers JS, Shetty AK. Assessing Barriers to Human Papillomavirus (HPV) Vaccination in At-Risk Rural Communities of Western North Carolina, United States. Vaccines. 2023; 11(12):1785. https://doi.org/10.3390/vaccines11121785
Chicago/Turabian StyleMcNeil, Candice J., Breona Barr, Iqra Munawar, Michael E. DeWitt, Jenny Snow Myers, and Avinash K. Shetty. 2023. "Assessing Barriers to Human Papillomavirus (HPV) Vaccination in At-Risk Rural Communities of Western North Carolina, United States" Vaccines 11, no. 12: 1785. https://doi.org/10.3390/vaccines11121785
APA StyleMcNeil, C. J., Barr, B., Munawar, I., DeWitt, M. E., Myers, J. S., & Shetty, A. K. (2023). Assessing Barriers to Human Papillomavirus (HPV) Vaccination in At-Risk Rural Communities of Western North Carolina, United States. Vaccines, 11(12), 1785. https://doi.org/10.3390/vaccines11121785






