Psychosocial Predictors of COVID-19 Vaccine Uptake among Pregnant Women: A Cross-Sectional Study in Greece
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Questionnaires
2.3. Statistical Analysis
3. Results
3.1. Socio-Demographic Characteristics
3.2. COVID-19-Related Vaccination Status
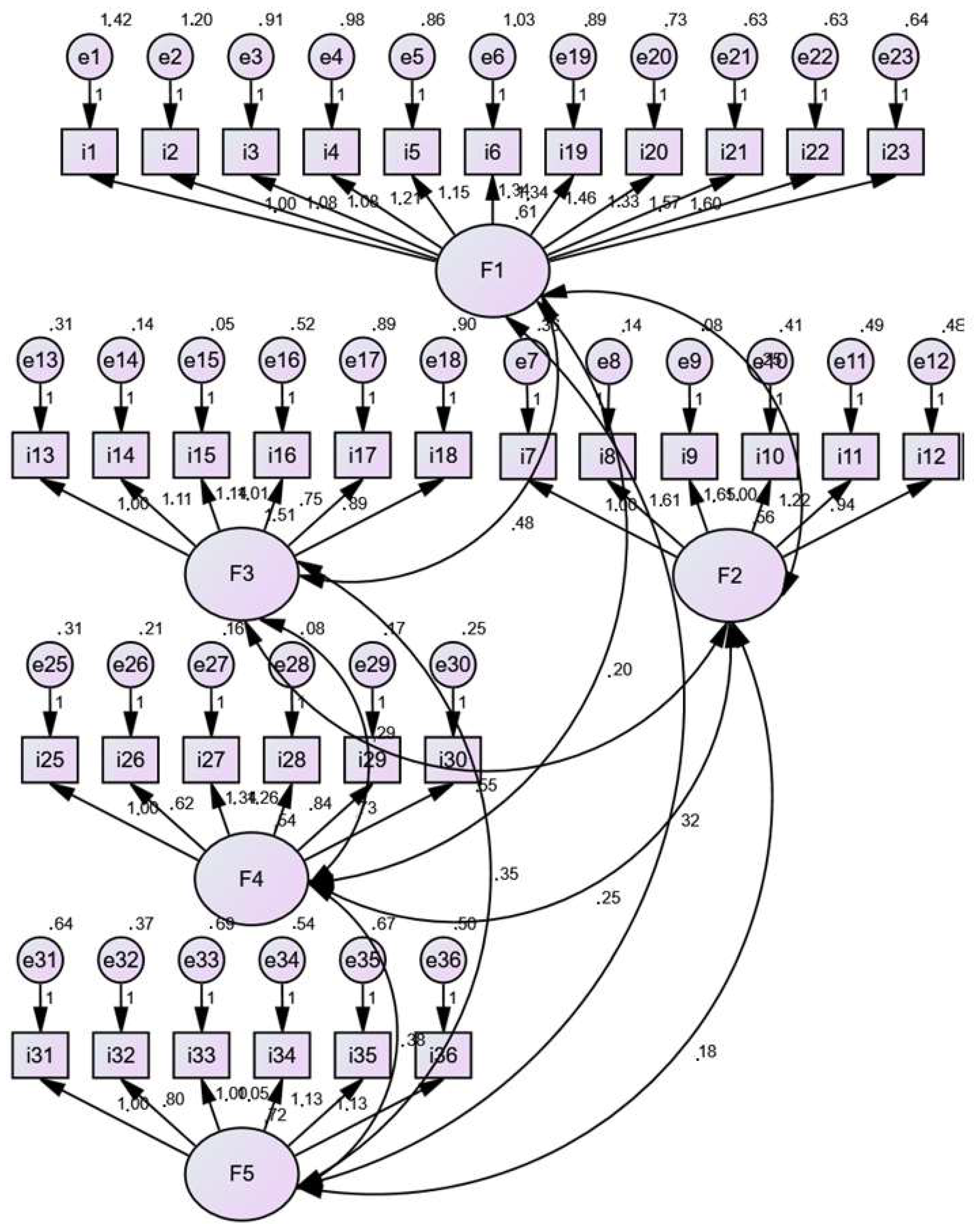
3.3. Validation of the COVID-19 Stress Scales
3.4. COVID-19-Related Stress
3.5. Predictors of COVID-19 Vaccine Uptake
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Barchielli, B.; Cricenti, C.; Gallè, F.; Sabella, E.A.; Liguori, F.; Da Molin, G.; Liguori, G.; Orsi, G.B.; Giannini, A.M.; Ferracuti, S.; et al. Climate Changes, Natural Resources Depletion, COVID-19 Pandemic, and Russian-Ukrainian War: What Is the Impact on Habits Change and Mental Health? Int. J. Environ. Res. Public Health 2022, 19, 11929. [Google Scholar] [CrossRef] [PubMed]
- Bourque, F.; Cunsolo Willox, A. Climate Change: The next Challenge for Public Mental Health? Int. Rev. Psychiatry 2014, 26, 415–422. [Google Scholar] [CrossRef] [PubMed]
- Galeotti, M.; Roson, R. Economic Impacts of Climate Change in Italy and the Mediterranean: Updating the Evidence. J. Sustain. Dev. 2012, 5, p27. [Google Scholar] [CrossRef]
- Sibbald, B. Physicians’ Roles on the Front Line of Climate Change. CMAJ 2013, 185, 195. [Google Scholar] [CrossRef]
- Warsini, S.; West, C.; Ed, G.D.; Res Meth, G.C.; Mills, J.; Usher, K. The Psychosocial Impact of Natural Disasters among Adult Survivors: An Integrative Review. Issues Ment. Health Nurs. 2014, 35, 420–436. [Google Scholar] [CrossRef] [PubMed]
- Pihkala, P. Eco-Anxiety, Tragedy, and Hope: Psychological and Spiritual Dimensions of Climate Change. Zygon 2018, 53, 545–569. [Google Scholar] [CrossRef]
- Usher, K.; Durkin, J.; Bhullar, N. Eco-Anxiety: How Thinking about Climate Change-Related Environmental Decline Is Affecting Our Mental Health. Int. J. Ment. Health Nurs. 2019, 28, 1233–1234. [Google Scholar] [CrossRef] [PubMed]
- Innocenti, M.; Santarelli, G.; Faggi, V.; Castellini, G.; Manelli, I.; Magrini, G.; Galassi, F.; Ricca, V. Psychometric Properties of the Italian Version of the Climate Change Anxiety Scale. J. Clim. Chang. Health 2021, 3, 100080. [Google Scholar] [CrossRef]
- The Armed Conflict Location & Event Data Project. ACLED Conflict Severity Index: A New Measure of the Complexities of Conflict. Available online: https://acleddata.com/conflict-severity-index/ (accessed on 23 January 2023).
- Bogic, M.; Njoku, A.; Priebe, S. Long-Term Mental Health of War-Refugees: A Systematic Literature Review. BMC Int. Health Hum. Rights 2015, 15, 29. [Google Scholar] [CrossRef] [PubMed]
- Borho, A.; Viazminsky, A.; Morawa, E.; Schmitt, G.M.; Georgiadou, E.; Erim, Y. The Prevalence and Risk Factors for Mental Distress among Syrian Refugees in Germany: A Register-Based Follow-up Study. BMC Psychiatry 2020, 20, 362. [Google Scholar] [CrossRef] [PubMed]
- Sheather, J. As Russian Troops Cross into Ukraine, We Need to Remind Ourselves of the Impact of War on Health. BMJ 2022, 376, o499. [Google Scholar] [CrossRef]
- Kurapov, A.; Pavlenko, V.; Drozdov, A.; Bezliudna, V.; Reznik, A.; Isralowitz, R. Toward an Understanding of the Russian-Ukrainian War Impact on University Students and Personnel. J. Loss Trauma 2022, 1–8. [Google Scholar] [CrossRef]
- Worldometer. COVID-19 Pandemic. Available online: https://www.worldometers.info/coronavirus/?fbclid=IwAR3T5FX-sv_X1GABioSDrcHEHSxg694_LZmDFQ3lFJjsBQQmiTemxcAow5k#countries (accessed on 23 January 2023).
- Zhang, S.X.; Batra, K.; Xu, W.; Liu, T.; Dong, R.K.; Yin, A.; Delios, A.Y.; Chen, B.Z.; Chen, R.Z.; Miller, S.; et al. Mental Disorder Symptoms during the COVID-19 Pandemic in Latin America—A Systematic Review and Meta-Analysis. Epidemiol. Psychiatr. Sci. 2022, 31, e23. [Google Scholar] [CrossRef] [PubMed]
- Salanti, G.; Peter, N.; Tonia, T.; Holloway, A.; White, I.R.; Darwish, L.; Low, N.; Egger, M.; Haas, A.D.; Fazel, S.; et al. The Impact of the COVID-19 Pandemic and Associated Control Measures on the Mental Health of the General Population: A Systematic Review and Dose-Response Meta-Analysis. Ann. Intern. Med. 2022, 175, 1560–1571. [Google Scholar] [CrossRef] [PubMed]
- Leung, C.M.C.; Ho, M.K.; Bharwani, A.A.; Cogo-Moreira, H.; Wang, Y.; Chow, M.S.C.; Fan, X.; Galea, S.; Leung, G.M.; Ni, M.Y. Mental Disorders Following COVID-19 and Other Epidemics: A Systematic Review and Meta-Analysis. Transl. Psychiatry 2022, 12, 205. [Google Scholar] [CrossRef] [PubMed]
- Khalil, A.; von Dadelszen, P.; Draycott, T.; Ugwumadu, A.; O’Brien, P.; Magee, L. Change in the Incidence of Stillbirth and Preterm Delivery During the COVID-19 Pandemic. JAMA 2020, 324, 705–706. [Google Scholar] [CrossRef] [PubMed]
- Lokken, E.M.; Huebner, E.M.; Taylor, G.G.; Hendrickson, S.; Vanderhoeven, J.; Kachikis, A.; Coler, B.; Walker, C.L.; Sheng, J.S.; Al-Haddad, B.J.S.; et al. Disease Severity, Pregnancy Outcomes, and Maternal Deaths among Pregnant Patients with Severe Acute Respiratory Syndrome Coronavirus 2 Infection in Washington State. Am. J. Obstet. Gynecol. 2021, 225, 77.e1–77.e14. [Google Scholar] [CrossRef]
- Vousden, N.; Bunch, K.; Morris, E.; Simpson, N.; Gale, C.; O’Brien, P.; Quigley, M.; Brocklehurst, P.; Kurinczuk, J.J.; Knight, M. The Incidence, Characteristics and Outcomes of Pregnant Women Hospitalized with Symptomatic and Asymptomatic SARS-CoV-2 Infection in the UK from March to September 2020: A National Cohort Study Using the UK Obstetric Surveillance System (UKOSS). PLoS ONE 2021, 16, e0251123. [Google Scholar] [CrossRef] [PubMed]
- Zambrano, L.D.; Ellington, S.; Strid, P.; Galang, R.R.; Oduyebo, T.; Tong, V.T.; Woodworth, K.R.; Nahabedian, J.F.; Azziz-Baumgartner, E.; Gilboa, S.M.; et al. Update: Characteristics of Symptomatic Women of Reproductive Age with Laboratory-Confirmed SARS-CoV-2 Infection by Pregnancy Status-United States, 22 January–3 October 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1641–1647. [Google Scholar] [CrossRef] [PubMed]
- Iacobucci, G. COVID-19 and Pregnancy: Vaccine Hesitancy and How to Overcome It. BMJ 2021, 375, n2862. [Google Scholar] [CrossRef] [PubMed]
- Pogue, K.; Jensen, J.L.; Stancil, C.K.; Ferguson, D.G.; Hughes, S.J.; Mello, E.J.; Burgess, R.; Berges, B.K.; Quaye, A.; Poole, B.D. Influences on Attitudes Regarding Potential COVID-19 Vaccination in the United States. Vaccines 2020, 8, E582. [Google Scholar] [CrossRef] [PubMed]
- Polack, F.P.; Thomas, S.J.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Perez, J.L.; Pérez Marc, G.; Moreira, E.D.; Zerbini, C.; et al. Safety and Efficacy of the BNT162b2 MRNA COVID-19 Vaccine. N. Engl. J. Med. 2020, 383, 2603–2615. [Google Scholar] [CrossRef]
- Falsaperla, R.; Leone, G.; Familiari, M.; Ruggieri, M. COVID-19 Vaccination in Pregnant and Lactating Women: A Systematic Review. Expert Rev. Vaccines 2021, 20, 1619–1628. [Google Scholar] [CrossRef] [PubMed]
- Fu, W.; Sivajohan, B.; McClymont, E.; Albert, A.; Elwood, C.; Ogilvie, G.; Money, D. Systematic Review of the Safety, Immunogenicity, and Effectiveness of COVID-19 Vaccines in Pregnant and Lactating Individuals and Their Infants. Int. J. Gynaecol. Obstet. 2022, 156, 406–417. [Google Scholar] [CrossRef] [PubMed]
- Garg, I.; Shekhar, R.; Sheikh, A.B.; Pal, S. COVID-19 Vaccine in Pregnant and Lactating Women: A Review of Existing Evidence and Practice Guidelines. Infect. Dis. Rep. 2021, 13, 685–699. [Google Scholar] [CrossRef] [PubMed]
- Mendoza, M.; Garcia-Ruiz, I.; Maiz, N.; Rodo, C.; Garcia-Manau, P.; Serrano, B.; Lopez-Martinez, R.; Balcells, J.; Fernandez-Hidalgo, N.; Carreras, E.; et al. Pre-eclampsia-like Syndrome Induced by Severe COVID-19: A Prospective Observational Study. BJOG Int. J. Obstet. Gynaecol. 2020, 127, 1374–1380. [Google Scholar] [CrossRef] [PubMed]
- Rawal, S.; Tackett, R.L.; Stone, R.H.; Young, H.N. COVID-19 Vaccination among Pregnant People in the U.S.: A Systematic Review. Am. J. Obstet. Gynecol. MFM 2022, 4, 100616. [Google Scholar] [CrossRef] [PubMed]
- American College of Obstetricians and Gynecologist. ACOG and SMFM Recommend COVID-19 Vaccination for Pregnant Individuals; American College of Obstetricians and Gynecologist: Washington, DC, USA, 2021. [Google Scholar]
- Centers for Disease Control and Prevention. COVID-19 Vaccines While Pregnant or Breastfeeding; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2021.
- Blakeway, H.; Prasad, S.; Kalafat, E.; Heath, P.T.; Ladhani, S.N.; Le Doare, K.; Magee, L.A.; O’Brien, P.; Rezvani, A.; von Dadelszen, P.; et al. COVID-19 Vaccination during Pregnancy: Coverage and Safety. Am. J. Obstet. Gynecol. 2022, 226, 236.e1–236.e14. [Google Scholar] [CrossRef]
- Cetin, I.; Mandalari, M.; Cesari, E.; Borriello, C.R.; Ercolanoni, M.; Preziosi, G. SARS-CoV-2 Vaccine Uptake during Pregnancy in Regione Lombardia, Italy: A Population-Based Study of 122,942 Pregnant Women. Vaccines 2022, 10, 1369. [Google Scholar] [CrossRef] [PubMed]
- Hosokawa, Y.; Okawa, S.; Hori, A.; Morisaki, N.; Takahashi, Y.; Fujiwara, T.; Nakayama, S.F.; Hamada, H.; Satoh, T.; Tabuchi, T. The Prevalence of COVID-19 Vaccination and Vaccine Hesitancy in Pregnant Women: An Internet-Based Cross-Sectional Study in Japan. J. Epidemiol. 2022, 32, JE20210458. [Google Scholar] [CrossRef] [PubMed]
- Janik, K.; Nietupska, K.; Iwanowicz-Palus, G.; Cybulski, M. Fear of COVID-19 and Vaccine Hesitancy among Pregnant Women in Poland: A Cross-Sectional Study. Vaccines 2022, 10, 1700. [Google Scholar] [CrossRef]
- Mustafa, Z.U.; Bashir, S.; Shahid, A.; Raees, I.; Salman, M.; Merchant, H.A.; Aldeyab, M.A.; Kow, C.S.; Hasan, S.S. COVID-19 Vaccine Hesitancy among Pregnant Women Attending Antenatal Clinics in Pakistan: A Multicentric, Prospective, Survey-Based Study. Viruses 2022, 14, 2344. [Google Scholar] [CrossRef]
- Nowacka, U.; Malarkiewicz, P.; Sierdzinski, J.; Januszaniec, A.; Kozłowski, S.; Issat, T. COVID-19 Vaccination Status among Pregnant and Postpartum Women—A Cross-Sectional Study on More Than 1000 Individuals. Vaccines 2022, 10, 1179. [Google Scholar] [CrossRef] [PubMed]
- Razzaghi, H.; Meghani, M.; Pingali, C.; Crane, B.; Naleway, A.; Weintraub, E.; Kenigsberg, T.A.; Lamias, M.J.; Irving, S.A.; Kauffman, T.L.; et al. COVID-19 Vaccination Coverage Among Pregnant Women During Pregnancy—Eight Integrated Health Care Organizations, United States, December 14, 2020–May 8, 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 895–899. [Google Scholar] [CrossRef] [PubMed]
- Siegel, M.R.; Lumbreras-Marquez, M.I.; James, K.; McBay, B.R.; Gray, K.J.; Schantz-Dunn, J.; Diouf, K.; Goldfarb, I.T. Perceptions and Attitudes toward COVID-19 Vaccination among Pregnant and Postpartum Individuals. Am. J. Perinatol. 2022, 29, 1489–1495. [Google Scholar] [CrossRef] [PubMed]
- UK Health Security Agency. COVID-19 Vaccine Surveillance Report Week 47; UK Health Security Agency: London, UK, 2021.
- Ramlawi, S.; Muldoon, K.A.; Dunn, S.I.; Murphy, M.S.Q.; Dingwall-Harvey, A.L.J.; Rennicks White, R.; Fakhraei, R.; Wen, S.W.; Walker, M.C.; Fell, D.B.; et al. Worries, Beliefs and Factors Influencing Perinatal COVID-19 Vaccination: A Cross-Sectional Survey of Preconception, Pregnant and Lactating Individuals. BMC Public Health 2022, 22, 2418. [Google Scholar] [CrossRef] [PubMed]
- Skirrow, H.; Barnett, S.; Bell, S.; Riaposova, L.; Mounier-Jack, S.; Kampmann, B.; Holder, B. Women’s Views on Accepting COVID-19 Vaccination during and after Pregnancy, and for Their Babies: A Multi-Methods Study in the UK. BMC Pregnancy Childbirth 2022, 22, 33. [Google Scholar] [CrossRef] [PubMed]
- Tostrud, L.; Thelen, J.; Palatnik, A. Models of Determinants of COVID-19 Vaccine Hesitancy in Non-Pregnant and Pregnant Population: Review of Current Literature. Hum. Vaccines Immunother. 2022, 18, 2138047. [Google Scholar] [CrossRef] [PubMed]
- Lubrano, C.; Vilca, L.M.; Coco, C.; Schirripa, I.; Zuliani, P.L.; Corneo, R.; Pavone, G.; Pellegrino, A.; Vignali, M.; Savasi, V.; et al. Pregnant Women’s Acceptance and Views on COVID-19 Vaccine in Northern Italy. J. Obstet. Gynaecol. 2023, 43, 2139596. [Google Scholar] [CrossRef] [PubMed]
- Marbán-Castro, E.; Nedic, I.; Ferrari, M.; Crespo-Mirasol, E.; Ferrer, L.; Noya, B.; Marin, A.; Fumadó, V.; López, M.; Menéndez, C.; et al. Perceptions of COVID-19 Maternal Vaccination among Pregnant Women and Healthcare Workers and Factors That Influence Vaccine Acceptance: A Cross-Sectional Study in Barcelona, Spain. Vaccines 2022, 10, 1930. [Google Scholar] [CrossRef] [PubMed]
- Chekol Abebe, E.; Ayalew Tiruneh, G.; Asmare Adela, G.; Mengie Ayele, T.; Tilahun Muche, Z.; Behaile T/Mariam, A.; Tilahun Mulu, A.; Abebe Zewde, E.; Dagnaw Baye, N.; Asmamaw Dejenie, T. COVID-19 Vaccine Uptake and Associated Factors among Pregnant Women Attending Antenatal Care in Debre Tabor Public Health Institutions: A Cross-Sectional Study. Front. Public Health 2022, 10, 919494. [Google Scholar] [CrossRef] [PubMed]
- Greek Ministry of Health. COVID-19 Vaccination. Available online: https://emvolio.gov.gr/en (accessed on 23 January 2023).
- Taylor, S.; Landry, C.A.; Paluszek, M.M.; Fergus, T.A.; McKay, D.; Asmundson, G.J.G. Development and Initial Validation of the COVID Stress Scales. J. Anxiety Disord. 2020, 72, 102232. [Google Scholar] [CrossRef]
- Galanis, P.; Vraka, I.; Katsiroumpa, A.; Konstantakopoulou, O.; Siskou, O.; Zogaki, E.; Kaitelidou, D. Cross-Cultural Adaptation and Validation of the “COVID Stress Scales” in Greek. Int. J. Caring Sci. 2022, 15, 499–508. [Google Scholar]
- Efstathiou, G. Translation, Adaptation and Validation Process of Research Instruments. In Individualized Care; Suhonen, R., Stolt, M., Papastavrou, E., Eds.; Springer International Publishing: Cham, Switzerland, 2019; pp. 65–78. ISBN 978-3-319-89898-8. [Google Scholar]
- Bentler, P.; Bonett, M.; Douglas, G. Significance Tests and Goodness of Fit in the Analysis of Covariance Structures. Psychol. Bull. 1980, 88, 588–606. [Google Scholar] [CrossRef]
- Hooper, D.; Coughlan, J.; Mullen, M. Structural Equation Modelling: Guidelines for Determining Model Fit. Electron. J. Bus. Res. Methods 2008, 6, 141–146. [Google Scholar] [CrossRef]
- Hu, L.; Bentler, P.M. Fit Indices in Covariance Structure Modeling: Sensitivity to Underparameterized Model Misspecification. Psychol. Methods 1998, 3, 424–453. [Google Scholar] [CrossRef]
- Steiger, J.H. Understanding the Limitations of Global Fit Assessment in Structural Equation Modeling. Personal. Individ. Differ. 2007, 42, 893–898. [Google Scholar] [CrossRef]
- DeVellis, R. Scale Development: Theory and Applications, 3rd ed.; Sage Publications Inc.: Thousand Oaks, CA, USA, 2012. [Google Scholar]
- Sousa, V.D.; Rojjanasrirat, W. Translation, Adaptation and Validation of Instruments or Scales for Use in Cross-Cultural Health Care Research: A Clear and User-Friendly Guideline. J. Eval. Clin. Pract. 2011, 17, 268–274. [Google Scholar] [CrossRef]
- Papazachariou, A.; Tsioutis, C.; Lytras, T.; Malikides, O.; Stamatelatou, M.; Vasilaki, N.; Milioni, A.; Dasenaki, M.; Spernovasilis, N. The Impact of Seasonal Influenza Vaccination Uptake on COVID-19 Vaccination Attitudes in a Rural Area in Greece. Vaccine 2023, 41, 821–825. [Google Scholar] [CrossRef]
- Galanis, P.; Vraka, I.; Siskou, O.; Konstantakopoulou, O.; Katsiroumpa, A.; Kaitelidou, D. Uptake of COVID-19 Vaccines among Pregnant Women: A Systematic Review and Meta-Analysis. Vaccines 2022, 10, 766. [Google Scholar] [CrossRef]
- Mhereeg, M.; Jones, H.; Kennedy, J.; Seaborne, M.; Parker, M.; Kennedy, N.; Beeson, S.; Akbari, A.; Zuccolo, L.; Davies, A.; et al. COVID-19 Vaccination in Pregnancy: Views and Vaccination Uptake Rates in Pregnancy, a Mixed Methods Analysis from SAIL and the Born-In-Wales Birth Cohort. BMC Infect. Dis. 2022, 22, 932. [Google Scholar] [CrossRef] [PubMed]
- Kapinos, K.A.; DeYoreo, M.; Lawrence, R.; Waymouth, M.; Uscher-Pines, L. COVID-19 Vaccine Uptake and Attitudes among Pregnant and Postpartum Parents. Am. J. Obstet. Gynecol. MFM 2022, 4, 100735. [Google Scholar] [CrossRef]
- Nguyen, L.H.; Joshi, A.D.; Drew, D.A.; Merino, J.; Ma, W.; Lo, C.-H.; Kwon, S.; Wang, K.; Graham, M.S.; Polidori, L.; et al. Racial and Ethnic Differences in COVID-19 Vaccine Hesitancy and Uptake. MedRxiv 2021. [Google Scholar]
- Schrading, W.A.; Trent, S.A.; Paxton, J.H.; Rodriguez, R.M.; Swanson, M.B.; Mohr, N.M.; Talan, D.A.; Project COVERED Emergency Department Network; Bahamon, M.; Carlson, J.N.; et al. Vaccination Rates and Acceptance of SARS-CoV-2 Vaccination among U.S. Emergency Department Health Care Personnel. Acad. Emerg. Med. 2021, 28, 455–458. [Google Scholar] [CrossRef]
- Xu, B.; Gao, X.; Zhang, X.; Hu, Y.; Yang, H.; Zhou, Y.-H. Real-World Acceptance of COVID-19 Vaccines among Healthcare Workers in Perinatal Medicine in China. Vaccines 2021, 9, 704. [Google Scholar] [CrossRef] [PubMed]
- Skjefte, M.; Ngirbabul, M.; Akeju, O.; Escudero, D.; Hernandez-Diaz, S.; Wyszynski, D.F.; Wu, J.W. COVID-19 Vaccine Acceptance among Pregnant Women and Mothers of Young Children: Results of a Survey in 16 Countries. Eur. J. Epidemiol. 2021, 36, 197–211. [Google Scholar] [CrossRef]
- Freeman, D.; Loe, B.S.; Chadwick, A.; Vaccari, C.; Waite, F.; Rosebrock, L.; Jenner, L.; Petit, A.; Lewandowsky, S.; Vanderslott, S.; et al. COVID-19 Vaccine Hesitancy in the UK: The Oxford Coronavirus Explanations, Attitudes, and Narratives Survey (Oceans) II. Psychol. Med. 2020, 52, 3127–3141. [Google Scholar] [CrossRef] [PubMed]
- Ahorsu, D.K.; Imani, V.; Lin, C.-Y.; Timpka, T.; Broström, A.; Updegraff, J.A.; Årestedt, K.; Griffiths, M.D.; Pakpour, A.H. Associations Between Fear of COVID-19, Mental Health, and Preventive Behaviours Across Pregnant Women and Husbands: An Actor-Partner Interdependence Modelling. Int. J. Ment. Health Addict. 2022, 20, 68–82. [Google Scholar] [CrossRef]
- Masjoudi, M.; Aslani, A.; Seifi, M.; Khazaeian, S.; Fathnezhad-Kazemi, A. Association between Perceived Stress, Fear and Anxiety of COVID 19 with Self-Care in Pregnant Women: A Cross-Sectional Study. Psychol. Health Med. 2022, 27, 289–300. [Google Scholar] [CrossRef]
- W/Mariam, T.G.; Kassie, B.A.; Asratie, M.H.; Abate, A.T. The Effects of Fear and Knowledge of COVID-19 on Preventive Practice Among Pregnant Women Who Attend Antenatal Care in Northwest Ethiopia, 2020: Institution-Based Cross-Sectional Study. Int. J. Womens Health 2021, 13, 95–100. [Google Scholar] [CrossRef]
- Wong, L.P.; Hung, C.-C.; Alias, H.; Lee, T.S.-H. Anxiety Symptoms and Preventive Measures during the COVID-19 Outbreak in Taiwan. BMC Psychiatry 2020, 20, 376. [Google Scholar] [CrossRef] [PubMed]
- Yıldırım, M.; Geçer, E.; Akgül, Ö. The Impacts of Vulnerability, Perceived Risk, and Fear on Preventive Behaviours against COVID-19. Psychol. Health Med. 2021, 26, 35–43. [Google Scholar] [CrossRef]
- Ayaz, R.; Hocaoğlu, M.; Günay, T.; devrim Yardımcı, O.; Turgut, A.; Karateke, A. Anxiety and Depression Symptoms in the Same Pregnant Women before and during the COVID-19 Pandemic. J. Perinat. Med. 2020, 48, 965–970. [Google Scholar] [CrossRef] [PubMed]
- Mappa, I.; Distefano, F.A.; Rizzo, G. Effects of Coronavirus 19 Pandemic on Maternal Anxiety during Pregnancy: A Prospectic Observational Study. J. Perinat. Med. 2020, 48, 545–550. [Google Scholar] [CrossRef]
- Stepowicz, A.; Wencka, B.; Bieńkiewicz, J.; Horzelski, W.; Grzesiak, M. Stress and Anxiety Levels in Pregnant and Post-Partum Women during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2020, 17, 9450. [Google Scholar] [CrossRef]
- King, L.S.; Feddoes, D.E.; Kirshenbaum, J.S.; Humphreys, K.L.; Gotlib, I.H. Pregnancy during the Pandemic: The Impact of COVID-19-Related Stress on Risk for Prenatal Depression. Psychol. Med. 2021, 53, 170–180. [Google Scholar] [CrossRef] [PubMed]
- Edvinsson, Å.; Bränn, E.; Hellgren, C.; Freyhult, E.; White, R.; Kamali-Moghaddam, M.; Olivier, J.; Bergquist, J.; Boström, A.E.; Schiöth, H.B.; et al. Lower Inflammatory Markers in Women with Antenatal Depression Brings the M1/M2 Balance into Focus from a New Direction. Psychoneuroendocrinology 2017, 80, 15–25. [Google Scholar] [CrossRef]
- Figueiredo, B.; Canário, C.; Field, T. Breastfeeding Is Negatively Affected by Prenatal Depression and Reduces Postpartum Depression. Psychol. Med. 2014, 44, 927–936. [Google Scholar] [CrossRef] [PubMed]
- Gustafsson, H.C.; Sullivan, E.L.; Nousen, E.K.; Sullivan, C.A.; Huang, E.; Rincon, M.; Nigg, J.T.; Loftis, J.M. Maternal Prenatal Depression Predicts Infant Negative Affect via Maternal Inflammatory Cytokine Levels. Brain Behav. Immun. 2018, 73, 470–481. [Google Scholar] [CrossRef] [PubMed]
- Osborne, S.; Biaggi, A.; Chua, T.E.; Du Preez, A.; Hazelgrove, K.; Nikkheslat, N.; Previti, G.; Zunszain, P.A.; Conroy, S.; Pariante, C.M. Antenatal Depression Programs Cortisol Stress Reactivity in Offspring through Increased Maternal Inflammation and Cortisol in Pregnancy: The Psychiatry Research and Motherhood—Depression (PRAM-D) Study. Psychoneuroendocrinology 2018, 98, 211–221. [Google Scholar] [CrossRef]
- Rossen, L.; Hutchinson, D.; Wilson, J.; Burns, L.; Olsson, C.A.; Allsop, S.; Elliott, E.J.; Jacobs, S.; Macdonald, J.A.; Mattick, R.P. Predictors of Postnatal Mother-Infant Bonding: The Role of Antenatal Bonding, Maternal Substance Use and Mental Health. Arch. Womens Ment. Health 2016, 19, 609–622. [Google Scholar] [CrossRef]
- Masjoudi, M.; Aslani, A.; Khazaeian, S.; Fathnezhad-Kazemi, A. Explaining the Experience of Prenatal Care and Investigating the Association between Psychological Factors with Self-Care in Pregnant Women during COVID-19 Pandemic: A Mixed Method Study Protocol. Reprod. Health 2020, 17, 98. [Google Scholar] [CrossRef]
- Stearns, S.; Bernard, S.; Fasick, S.; Schwartz, R.; Konrad, T.; Ory, M.; DeFriese, G. The Economic Implications of Self-Care: The Effect of Lifestyle, Functional Adaptations, and Medical Self-Care among a National Sample of Medicare Beneficiaries. Am. J. Public Health 2000, 90, 1608–1612. [Google Scholar] [CrossRef]
- Green, M.S.; Abdullah, R.; Vered, S.; Nitzan, D. A Study of Ethnic, Gender and Educational Differences in Attitudes toward COVID-19 Vaccines in Israel—Implications for Vaccination Implementation Policies. Isr. J. Health Policy Res. 2021, 10, 26. [Google Scholar] [CrossRef]
- Paul, E.; Steptoe, A.; Fancourt, D. Attitudes towards Vaccines and Intention to Vaccinate against COVID-19: Implications for Public Health Communications. Lancet Reg. Health Eur. 2021, 1, 100012. [Google Scholar] [CrossRef] [PubMed]
- Taubman-Ben-Ari, O.; Weiss, E.; Abu-Sharkia, S.; Khalaf, E. A Comparison of COVID-19 Vaccination Status among Pregnant Israeli Jewish and Arab Women and Psychological Distress among the Arab Women. Nurs. Health Sci. 2022, 24, 360–367. [Google Scholar] [CrossRef] [PubMed]
- Galanis, P.; Vraka, I.; Siskou, O.; Konstantakopoulou, O.; Katsiroumpa, A.; Kaitelidou, D. Willingness, Refusal and Influential Factors of Parents to Vaccinate Their Children against the COVID-19: A Systematic Review and Meta-Analysis. Prev. Med. 2022, 157, 106994. [Google Scholar] [CrossRef]
- Yılmaz, M.; Sahin, M.K. Parents’ Willingness and Attitudes Concerning the COVID-19 Vaccine: A Cross-sectional Study. Int. J. Clin. Pract. 2021, 75, e14364. [Google Scholar] [CrossRef] [PubMed]
- Zhang, K.C.; Fang, Y.; Cao, H.; Chen, H.; Hu, T.; Chen, Y.Q.; Zhou, X.; Wang, Z. Parental Acceptability of COVID-19 Vaccination for Children Under the Age of 18 Years: Cross-Sectional Online Survey. JMIR Pediatr. Parent. 2020, 3, e24827. [Google Scholar] [CrossRef] [PubMed]
- Galanis, P.; Vraka, I.; Fragkou, D.; Bilali, A.; Kaitelidou, D. Intention of Healthcare Workers to Accept COVID-19 Vaccination and Related Factors: A Systematic Review and Meta-Analysis. Asian Pac. J. Trop. Med. 2021, 14, 543. [Google Scholar] [CrossRef]
- Li, M.; Luo, Y.; Watson, R.; Zheng, Y.; Ren, J.; Tang, J.; Chen, Y. Healthcare Workers’ (HCWs) Attitudes and Related Factors towards COVID-19 Vaccination: A Rapid Systematic Review. Postgrad. Med. J. 2021, postgradmedj-2021-140195. [Google Scholar] [CrossRef] [PubMed]
- Luo, C.; Yang, Y.; Liu, Y.; Zheng, D.; Shao, L.; Jin, J.; He, Q. Intention to COVID-19 Vaccination and Associated Factors among Health Care Workers: A Systematic Review and Meta-Analysis of Cross-Sectional Studies. Am. J. Infect. Control 2021, 49, 1295–1304. [Google Scholar] [CrossRef] [PubMed]
- Shamshirsaz, A.A.; Hessami, K.; Morain, S.; Afshar, Y.; Nassr, A.A.; Arian, S.E.; Asl, N.M.; Aagaard, K. Intention to Receive COVID-19 Vaccine during Pregnancy: A Systematic Review and Meta-Analysis. Am. J. Perinatol. 2021, 39, 492–500. [Google Scholar] [CrossRef] [PubMed]
- Doran, J.; Seyidov, N.; Mehdiyev, S.; Gon, G.; Kissling, E.; Herdman, T.; Suleymanova, J.; Rehse, A.P.C.; Pebody, R.; Katz, M.A.; et al. Factors Associated with Early Uptake of COVID-19 Vaccination among Healthcare Workers in Azerbaijan, 2021. Influenza Other Respir. Viruses 2022, 16, 626–631. [Google Scholar] [CrossRef] [PubMed]
- Galanis, P.; Vraka, I.; Siskou, O.; Konstantakopoulou, O.; Katsiroumpa, A.; Moisoglou, I.; Kaitelidou, D. Predictors of Real-World Parents’ Acceptance to Vaccinate Their Children Against the COVID-19. Acta Med. Litu. 2022, 29, 4. [Google Scholar] [CrossRef]
- Gilboa, M.; Tal, I.; Levin, E.G.; Segal, S.; Belkin, A.; Zilberman-Daniels, T.; Biber, A.; Rubin, C.; Rahav, G.; Regev-Yochay, G. Coronavirus Disease 2019 (COVID-19) Vaccination Uptake among Healthcare Workers. Infect. Control Hosp. Epidemiol. 2021, 43, 1433–1438. [Google Scholar] [CrossRef]
- Shariff, S.Z.; Richard, L.; Hwang, S.W.; Kwong, J.C.; Forchuk, C.; Dosani, N.; Booth, R. COVID-19 Vaccine Coverage and Factors Associated with Vaccine Uptake among 23 247 Adults with a Recent History of Homelessness in Ontario, Canada: A Population-Based Cohort Study. Lancet Public Health 2022, 7, e366–e377. [Google Scholar] [CrossRef]
- Wang, R.; Liu, M.; Liu, J. The Association between Influenza Vaccination and COVID-19 and Its Outcomes: A Systematic Review and Meta-Analysis of Observational Studies. Vaccines 2021, 9, 529. [Google Scholar] [CrossRef] [PubMed]
- Zeynali Bujani, M.; Behnampour, M.; Rahimi, N.; Safari, T.; Khazaei Feizabad, A.; Hossein Sarbazi, A.; Baniasadi, M.; Rezaei, N.; Ansari Moghaddam, A. The Effect of Influenza Vaccination on COVID-19 Morbidity, Severity and Mortality: Systematic Review and Meta-Analysis. Malays. J. Med. Sci. 2021, 28, 20–31. [Google Scholar] [CrossRef] [PubMed]
- Stuckelberger, S.; Favre, G.; Ceulemans, M.; Nordeng, H.; Gerbier, E.; Lambelet, V.; Stojanov, M.; Winterfeld, U.; Baud, D.; Panchaud, A.; et al. SARS-CoV-2 Vaccine Willingness among Pregnant and Breastfeeding Women during the First Pandemic Wave: A Cross-Sectional Study in Switzerland. Viruses 2021, 13, 1199. [Google Scholar] [CrossRef]
- Glick, I.; Kadish, E.; Rottenstreich, M. Management of Pregnancy in Women of Advanced Maternal Age: Improving Outcomes for Mother and Baby. Int. J. Womens Health 2021, 13, 751–759. [Google Scholar] [CrossRef] [PubMed]
- Pinheiro, R.L.; Areia, A.L.; Mota Pinto, A.; Donato, H. Advanced Maternal Age: Adverse Outcomes of Pregnancy, A Meta-Analysis. Acta Med. Port. 2019, 32, 219. [Google Scholar] [CrossRef]
- Mehraeen, E.; Karimi, A.; Barzegary, A.; Vahedi, F.; Afsahi, A.M.; Dadras, O.; Moradmand-Badie, B.; Seyed Alinaghi, S.A.; Jahanfar, S. Predictors of Mortality in Patients with COVID-19–a Systematic Review. Eur. J. Integr. Med. 2020, 40, 101226. [Google Scholar] [CrossRef]
- Sepandi, M.; Taghdir, M.; Alimohamadi, Y.; Afrashteh, S.; Hosamirudsari, H. Factors Associated with Mortality in COVID-19 Patients: A Systematic Review and Meta-Analysis. Iran. J. Public Health 2020, 49, 1211–1221. [Google Scholar] [CrossRef] [PubMed]
- Yanez, N.D.; Weiss, N.S.; Romand, J.-A.; Treggiari, M.M. COVID-19 Mortality Risk for Older Men and Women. BMC Public Health 2020, 20, 1742. [Google Scholar] [CrossRef]
- Caserotti, M.; Girardi, P.; Rubaltelli, E.; Tasso, A.; Lotto, L.; Gavaruzzi, T. Associations of COVID-19 Risk Perception with Vaccine Hesitancy over Time for Italian Residents. Soc. Sci. Med. 2021, 272, 113688. [Google Scholar] [CrossRef]
- Ward, J.K.; Alleaume, C.; Peretti-Watel, P.; Peretti-Watel, P.; Seror, V.; Cortaredona, S.; Launay, O.; Raude, J.; Verger, P.; Beck, F.; et al. The French Public’s Attitudes to a Future COVID-19 Vaccine: The Politicization of a Public Health Issue. Soc. Sci. Med. 2020, 265, 113414. [Google Scholar] [CrossRef] [PubMed]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The Psychological Impact of Quarantine and How to Reduce It: Rapid Review of the Evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef]
- Moccia, L.; Janiri, D.; Pepe, M.; Dattoli, L.; Molinaro, M.; De Martin, V.; Chieffo, D.; Janiri, L.; Fiorillo, A.; Sani, G.; et al. Affective Temperament, Attachment Style, and the Psychological Impact of the COVID-19 Outbreak: An Early Report on the Italian General Population. Brain Behav. Immun. 2020, 87, 75–79. [Google Scholar] [CrossRef]
- Pacella-LaBarbara, M.L.; Park, Y.L.; Patterson, P.D.; Doshi, A.; Guyette, M.K.; Wong, A.H.; Chang, B.P.; Suffoletto, B.P. COVID-19 Vaccine Uptake and Intent Among Emergency Healthcare Workers: A Cross-Sectional Survey. J. Occup. Environ. Med. 2021, 63, 852–856. [Google Scholar] [CrossRef]
- Skalis, G.; Archontakis, S.; Thomopoulos, C.; Andrianopoulou, I.; Papazachou, O.; Vamvakou, G.; Aznaouridis, K.; Katsi, V.; Makris, T. A Single-Center, Prospective, Observational Study on Maternal Smoking during Pregnancy in Greece: The HELENA Study. Tob. Prev. Cessat. 2021, 7, 16. [Google Scholar] [CrossRef] [PubMed]
- Papandreou, D.; Mantzorou, M.; Tyrovolas, S.; Pavlidou, E.; Antasouras, G.; Psara, E.; Poulios, E.; Vasios, G.K.; Giaginis, C. Pre-Pregnancy Excess Weight Association with Maternal Sociodemographic, Anthropometric and Lifestyle Factors and Maternal Perinatal Outcomes. Nutrients 2022, 14, 3810. [Google Scholar] [CrossRef] [PubMed]
- Koukkou, E.G.; Ilias, I.; Mamalis, I.; Markou, K.B. Pregnant Greek Women May Have a Higher Prevalence of Iodine Deficiency than the General Greek Population. Eur. Thyroid J. 2017, 6, 26–30. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Ten Threats to Global Health in 2019; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Zakiyah, N.; Insani, W.N.; Suwantika, A.A.; van der Schans, J.; Postma, M.J. Pneumococcal Vaccination for Children in Asian Countries: A Systematic Review of Economic Evaluation Studies. Vaccines 2020, 8, 426. [Google Scholar] [CrossRef]
- Pawaskar, M.; Méroc, E.; Samant, S.; Flem, E.; Bencina, G.; Riera-Montes, M.; Heininger, U. Economic Burden of Varicella in Europe in the Absence of Universal Varicella Vaccination. BMC Public Health 2021, 21, 2312. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.C.; Chaiyakunapruk, N.; Zhu, S.; Babigumira, J.B.; Furnback, W.; Chitale, R.; Gamil, A.; Zhao, K.; Wasserman, M. A Systematic Literature Review of Economic Evaluations of Pneumococcal Conjugate Vaccines in East and Southeast Asia (2006–2019). Expert Rev. Vaccines 2022, 21, 885–898. [Google Scholar] [CrossRef]
- Machlaurin, A.; van der Pol, S.; Setiawan, D.; van der Werf, T.S.; Postma, M.J. Health Economic Evaluation of Current Vaccination Strategies and New Vaccines against Tuberculosis: A Systematic Review. Expert Rev. Vaccines 2019, 18, 897–911. [Google Scholar] [CrossRef]
- Utami, A.M.; Rendrayani, F.; Khoiry, Q.A.; Noviyanti, D.; Suwantika, A.A.; Postma, M.J.; Zakiyah, N. Economic Evaluation of COVID-19 Vaccination: A Systematic Review. J. Glob. Health 2023, 13, 06001. [Google Scholar] [CrossRef]
| Variable | N | % |
|---|---|---|
| Marital status | ||
| Singles | 84 | 10.3 |
| Married or in a couple relationship without marriage | 728 | 89.7 |
| Divorced | 0 | 0 |
| Age (years), mean, standard deviation | 31.6 | 4.6 |
| Children < 18 years old | ||
| No | 525 | 64.7 |
| Yes | 287 | 35.3 |
| Educational level | ||
| Elementary school | 7 | 0.9 |
| High school | 210 | 25.9 |
| University degree | 595 | 73.3 |
| Self-perceived financial status | ||
| Very poor | 7 | 0.9 |
| Poor | 28 | 3.4 |
| Moderate | 385 | 47.4 |
| Good | 336 | 41.4 |
| Very good | 56 | 6.9 |
| Self-perceived health status | ||
| Very poor | 0 | 0 |
| Poor | 0 | 0 |
| Moderate | 77 | 9.5 |
| Good | 462 | 56.9 |
| Very good | 273 | 33.6 |
| Chronic disease | ||
| No | 693 | 85.3 |
| Yes | 119 | 14.7 |
| Previous COVID-19 diagnosis | ||
| No | 616 | 75.9 |
| Yes | 196 | 24.1 |
| Family members/friends with previous COVID-19 diagnosis | ||
| No | 168 | 20.7 |
| Yes | 644 | 79.3 |
| Variable | N | % |
|---|---|---|
| COVID-19 vaccination uptake | ||
| No | 336 | 41.4 |
| Yes | 476 | 58.6 |
| COVID-19 vaccination uptake before pregnancy | ||
| No | 217 | 45.6 |
| Yes | 259 | 54.4 |
| Seasonal influenza vaccination in 2021 | ||
| No | 616 | 75.9 |
| Yes | 196 | 24.1 |
| Reasons for decline of pregnant women to receive a COVID-19 vaccine | ||
| I have doubts about the safety and effectiveness of COVID-19 vaccines | 112 | 31.4 |
| I am afraid of adverse side effects of COVID-19 vaccines | 105 | 29.4 |
| I believe that even I get infected with COVID-19, nothing bad will happen to me | 14 | 3.9 |
| I have already been diagnosed with COVID-19 and the vaccine will not be beneficial for me | 14 | 3.9 |
| I am afraid because I suffer from a chronic disease | 7 | 2.0 |
| I am afraid that COVID-19 vaccines could be harmful to my fetus | 105 | 29.4 |
| Scale | Mean | Standard Deviation | p-Value a |
|---|---|---|---|
| Danger and contamination fears | <0.001 | ||
| Unvaccinated | 2.01 | 1.06 | |
| Vaccinated | 2.34 | 1.02 | |
| Fears about economic consequences | 0.042 | ||
| Unvaccinated | 0.51 | 0.82 | |
| Vaccinated | 0.65 | 1.05 | |
| Xenophobia | 0.471 | ||
| Unvaccinated | 0.97 | 1.24 | |
| Vaccinated | 1.04 | 1.27 | |
| Compulsive checking and reassurance seeking | 0.401 | ||
| Unvaccinated | 0.87 | 0.84 | |
| Vaccinated | 0.92 | 0.97 | |
| Traumatic stress symptoms about COVID-19 | 0.384 | ||
| Unvaccinated | 0.40 | 0.74 | |
| Vaccinated | 0.45 | 0.74 |
| Variable | Unadjusted OR (95% CI) | p-Value | Adjusted OR (95% CI) a | p-Value b |
|---|---|---|---|---|
| Marital status (singles vs. married) | 1.45 (0.91–2.36) | 0.12 | 2.18 (1.01–4.70) | 0.046 |
| Age (years) | 1.07 (1.04–1.10) | <0.001 | 1.09 (1.04–1.14) | <0.001 |
| Children aged <18 years old (yes vs. no) | 1.36 (1.01–1.83) | 0.04 | 1.88 (1.23–2.89) | 0.004 |
| Educational level (University degree vs. high school) | 2.75 (1.99–3.79) | <0.001 | NS | |
| Self-perceived financial status (very good/good vs. moderate/poor/very poor) | 1.18 (0.89–1.56) | 0.24 | NS | |
| Self-perceived health status (very poor/poor/moderate vs. good/very good) | 1.26 (0.78–2.05) | 0.35 | 3.44 (1.69–7.00) | 0.001 |
| Chronic disease (yes vs. no) | 1.35 (0.90–2.03) | 0.15 | NS | |
| Previous COVID-19 diagnosis (no vs. yes) | 1.31 (0.95–1.81) | 0.10 | 1.63 (1.01–2.64) | 0.047 |
| Family members/friends with previous COVID-19 diagnosis (yes vs. no) | 2.39 (1.69–3.38) | <0.001 | 1.79 (1.08–2.96) | 0.025 |
| Seasonal influenza vaccination in 2021 (yes vs. no) | 8.72 (5.40–14.09) | <0.001 | 17.64 (8.63–36.17) | <0.001 |
| Danger and contamination fears | 1.35 (1.18–1.54) | <0.001 | 1.43 (1.13–1.79) | 0.003 |
| Fears about economic consequences | 1.16 (0.99–1.35) | 0.05 | 1.58 (1.24–2.03) | <0.001 |
| Xenophobia | 1.04 (0.93–1.17) | 0.47 | NS | |
| Compulsive checking and reassurance seeking | 1.07 (0.91–1.24) | 0.41 | 0.50 (0.39–0.64) | <0.001 |
| Traumatic stress symptoms about COVID-19 | 1.09 (0.89–1.32) | 0.38 | NS | |
| Worry about the side effects of COVID-19 vaccines | 0.84 (0.81–0.88) | <0.001 | 0.73 (0.68–0.79) | <0.001 |
| Trust in COVID-19 vaccines | 1.36 (1.29–1.44) | <0.001 | 1.53 (1.41–1.65) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Galanis, P.; Vraka, I.; Katsiroumpa, A.; Siskou, O.; Konstantakopoulou, O.; Zogaki, E.; Kaitelidou, D. Psychosocial Predictors of COVID-19 Vaccine Uptake among Pregnant Women: A Cross-Sectional Study in Greece. Vaccines 2023, 11, 269. https://doi.org/10.3390/vaccines11020269
Galanis P, Vraka I, Katsiroumpa A, Siskou O, Konstantakopoulou O, Zogaki E, Kaitelidou D. Psychosocial Predictors of COVID-19 Vaccine Uptake among Pregnant Women: A Cross-Sectional Study in Greece. Vaccines. 2023; 11(2):269. https://doi.org/10.3390/vaccines11020269
Chicago/Turabian StyleGalanis, Petros, Irene Vraka, Aglaia Katsiroumpa, Olga Siskou, Olympia Konstantakopoulou, Eleftheria Zogaki, and Daphne Kaitelidou. 2023. "Psychosocial Predictors of COVID-19 Vaccine Uptake among Pregnant Women: A Cross-Sectional Study in Greece" Vaccines 11, no. 2: 269. https://doi.org/10.3390/vaccines11020269
APA StyleGalanis, P., Vraka, I., Katsiroumpa, A., Siskou, O., Konstantakopoulou, O., Zogaki, E., & Kaitelidou, D. (2023). Psychosocial Predictors of COVID-19 Vaccine Uptake among Pregnant Women: A Cross-Sectional Study in Greece. Vaccines, 11(2), 269. https://doi.org/10.3390/vaccines11020269








