Multivariate Assessment of Vaccine Equity in Cambodia: A Longitudinal VERSE Tool Case Study Using Demographic and Health Survey 2004, 2010, and 2014
Abstract
1. Introduction
2. Materials and Methods
3. Results
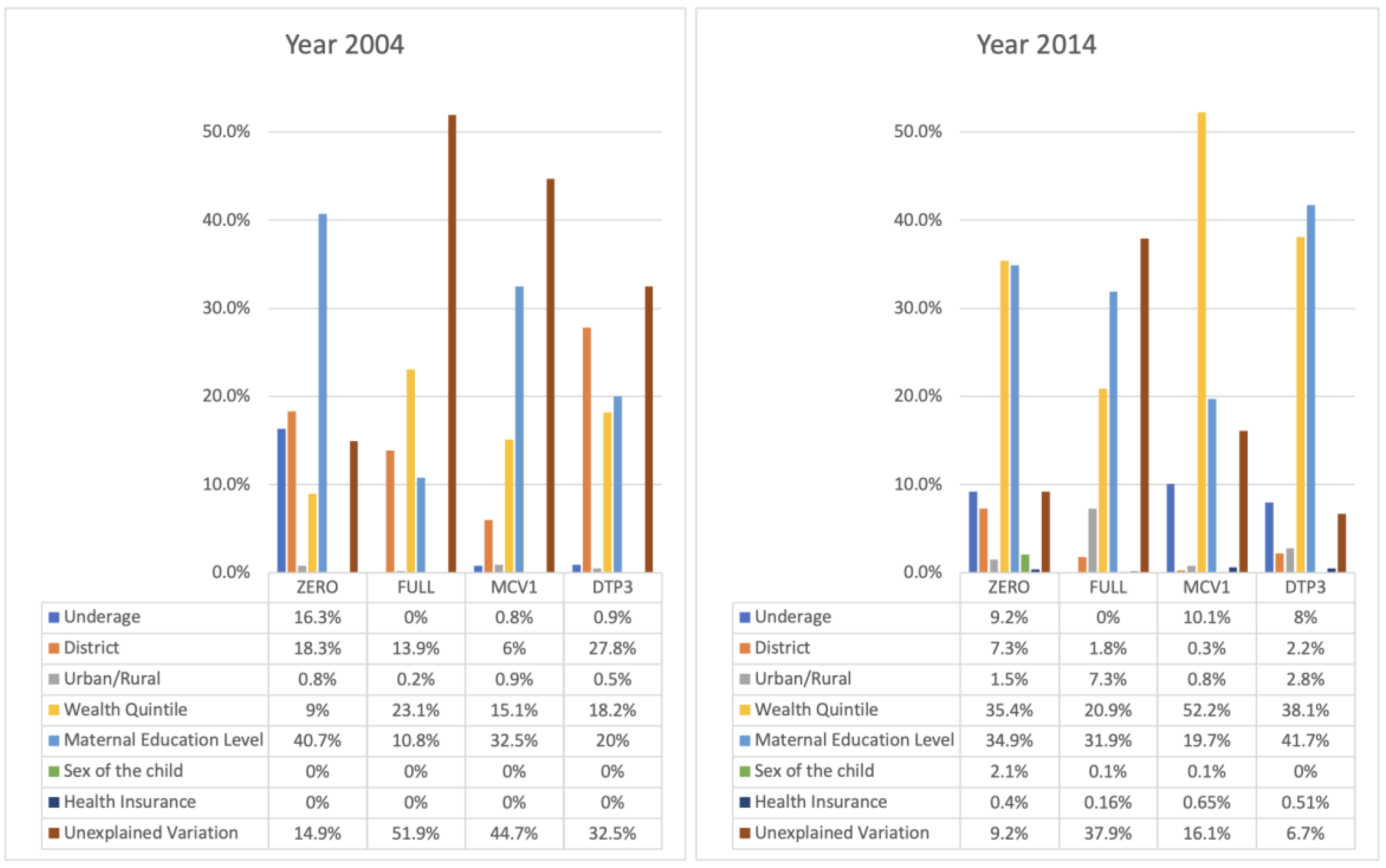
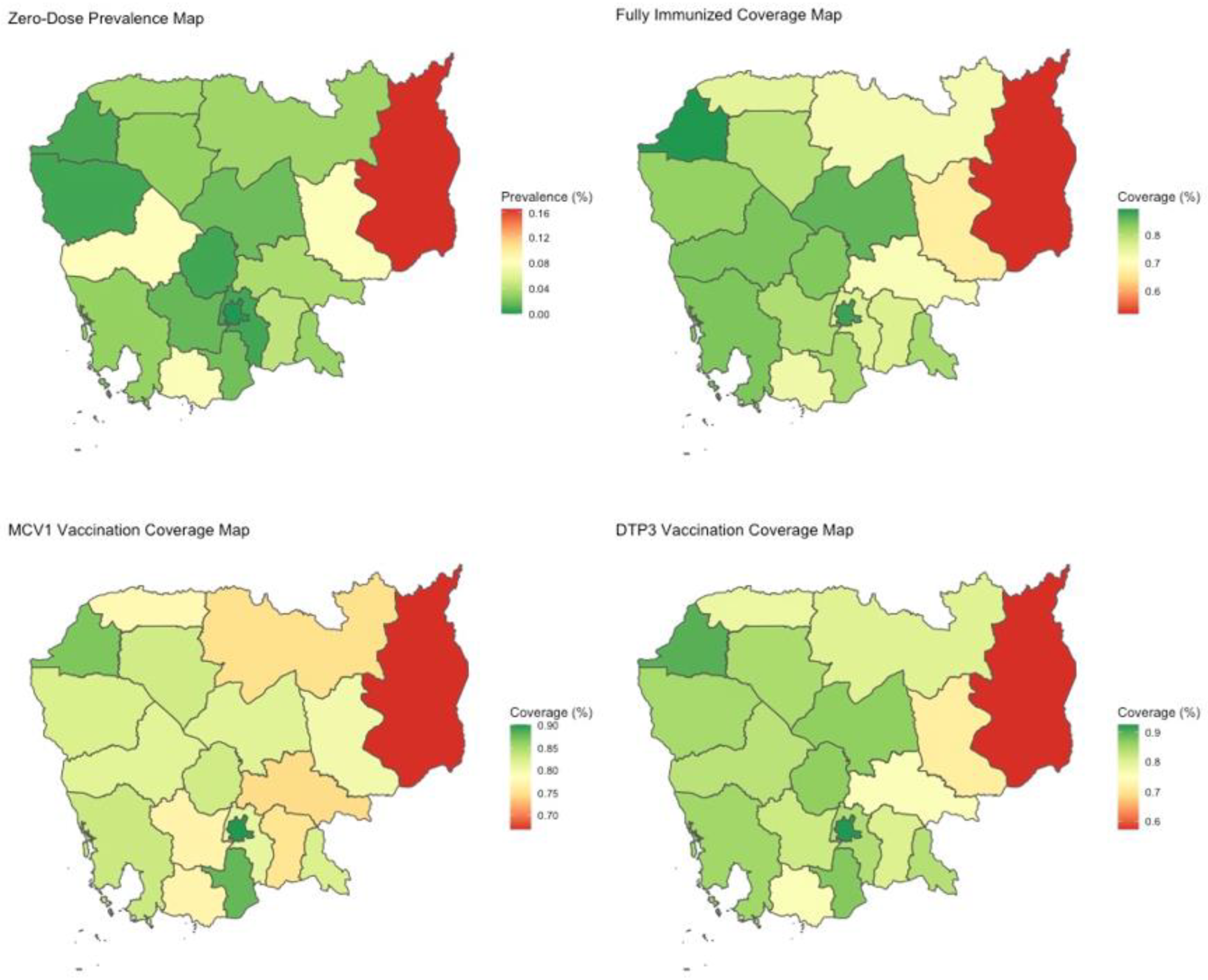
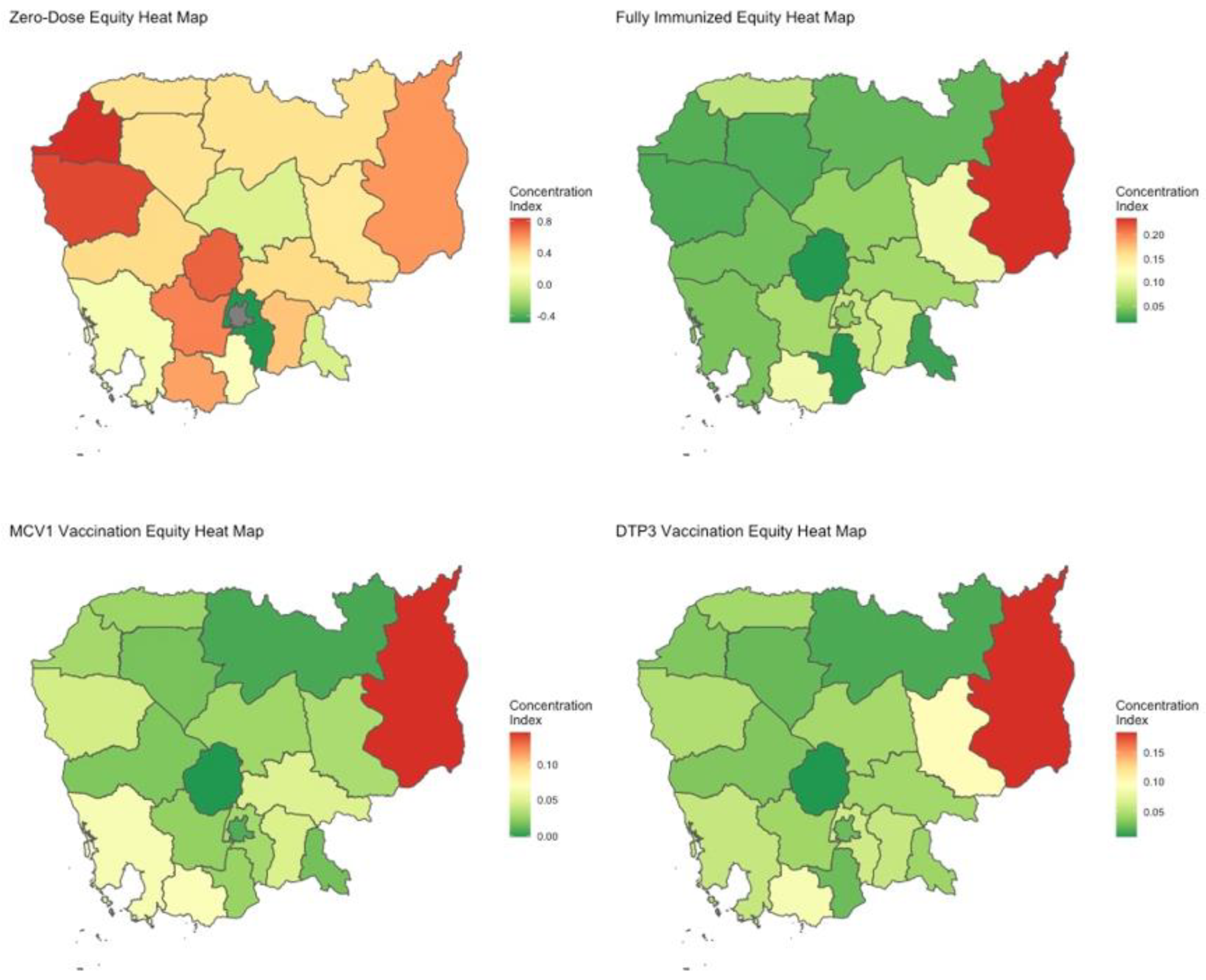
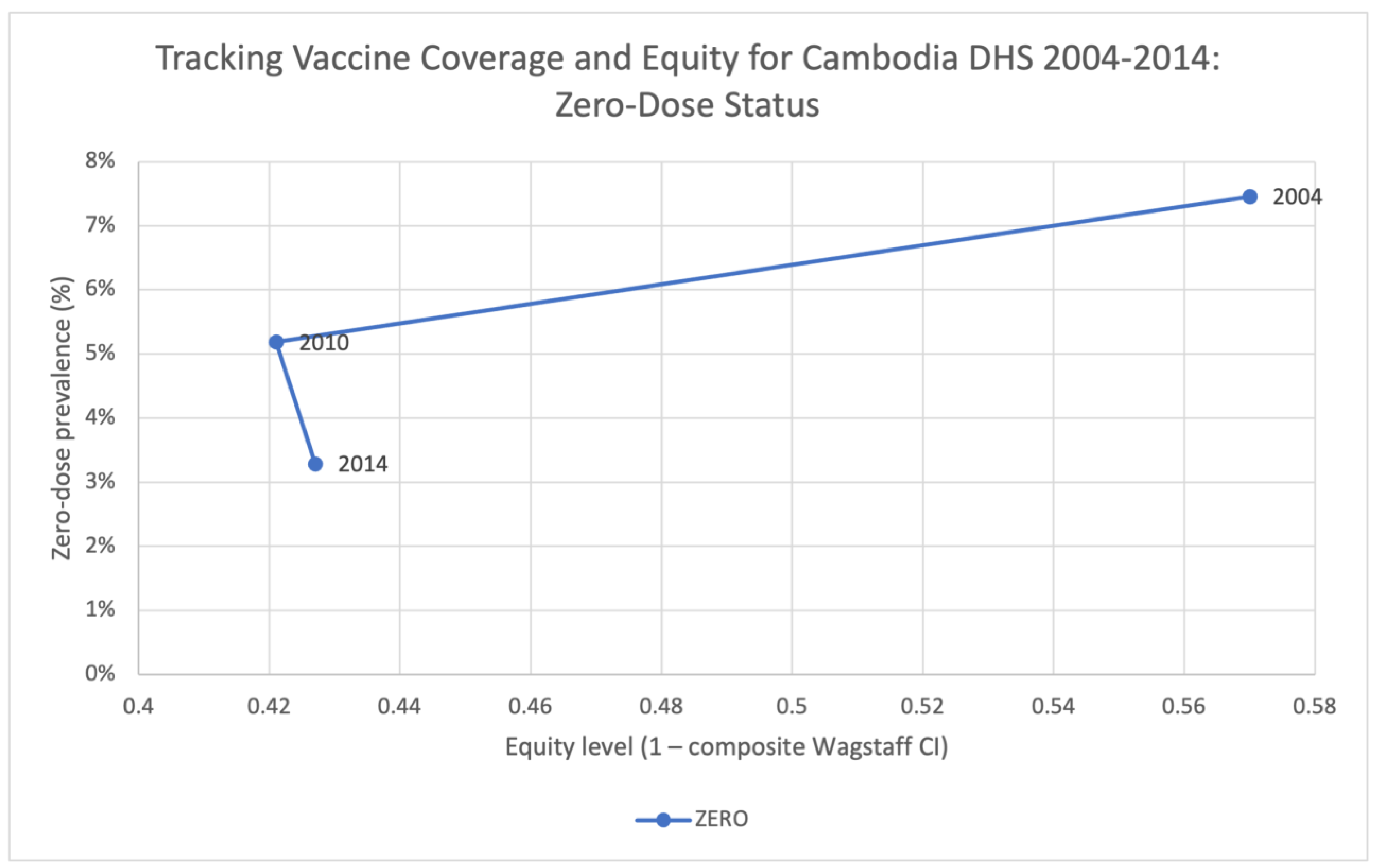
3.1. Zero-Dose
3.2. Fully-Immunized for Age
3.3. MCV1
3.4. DTP3
3.5. Trends over Time
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Vaccines and Immunization. Available online: https://www.who.int/health-topics/vaccines-and-immunization#tab=tab_1 (accessed on 14 July 2022).
- Over 13 Million Cchildren Did Not Receive Any Vaccines at All Even before COVID-19 Disrupted Global Immunization–UNICEF. Available online: https://www.unicef.org/eap/press-releases/over-13-million-children-did-not-receive-any-vaccines-all-even-covid-19-disrupted (accessed on 27 March 2023).
- SeyedAlinaghi, S.; Karimi, A.; Mojdeganlou, H.; Alilou, S.; Mirghaderi, S.P.; Noori, T.; Shamsabadi, A.; Dadras, O.; Vahedi, F.; Mohammadi, P.; et al. Impact of COVID-19 pandemic on routine vaccination coverage of children and adolescents: A systematic review. Health Sci. Rep. 2022, 5, e00516. [Google Scholar] [CrossRef] [PubMed]
- WHO TEAM Immunization, Vaccines and Biologicals. Immunization Agenda 2030: A Global Strategy to Leave No One Behind. Available online: https://www.who.int/publications/m/item/immunization-agenda-2030-a-global-strategy-to-leave-no-one-behind (accessed on 27 March 2023).
- Ministry of Health, National Maternal and Child Health Center, National Immunization Program. CAMBODIA National Immunization Program Strategic Plan 2008–2015; Ministry of Health: Phnom Penh, Cambodia, 2008. [Google Scholar]
- Miyazaki, A.; Tung, R.; Taing, B.; Matsui, M.; Iwamoto, A.; Cox, S.E. Frequent unregulated use of antibiotics in rural Cambodian infants. Trans. R. Soc. Trop. Med. Hyg. 2020, 114, 401–407. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Regional Office for the Western Pacific. Cambodia-WHO Country Cooperation Strategy 2016–2020. Available online: https://apps.who.int/iris/handle/10665/246102 (accessed on 27 March 2023).
- Ministry of Health, National Maternal and Child Health Center, National Immunization Program. CAMBODIA National Immunization Program Strategic Plan 2016–2020; Ministry of Health: Phnom Penh, Cambodia, 2016. [Google Scholar]
- WHO. Health Inequities and Their Causes. Available online: https://www.who.int/news-room/facts-in-pictures/detail/health-inequities-and-their-causes (accessed on 26 December 2022).
- Satcher, D. Include a Social Determinants of Health Approach to Reduce Health Inequities. Public Health Rep. 2010, 125 (Suppl. S4), 6–7. [Google Scholar] [CrossRef] [PubMed]
- Reid, P.; Robson, B. Understanding Health Inequities. Hauora: Māori Standards of Health IV. A Study of the Years: 2000–2005; Te Rōpū Rangahau Hauora a Eru Pōmare: Wellington, New Zealand, 2007. [Google Scholar]
- Commission on Social Determinants of Health. Closing the Gap in a Generation: Health Equity through Action on the Social Determinants of Health—Final Report of the Commission on Social Determinants of Health. Available online: https://www.who.int/publications/i/item/WHO-IER-CSDH-08.1 (accessed on 14 July 2022).
- Hosseinpoor, A.R.; Victora, C.; Bergen, N.; Barros, A.; Boerma, T. Towards universal health coverage: The role of within-country wealth-related inequality in 28 countries in sub-Saharan Africa. Bull. World Health Organ. 2011, 89, 881–890. [Google Scholar] [CrossRef]
- Houweling, A.; Ronsmans, C.; Campbell, O.; Kunst, A. Huge poor–rich inequalities in maternity care: An international comparative study of maternity and child care in developing countries. Bull. World Health Organ. 2007, 85, 745–754. [Google Scholar] [CrossRef]
- Home. Equity Tool. 2021. Available online: https://www.equitytool.org/ (accessed on 3 October 2022).
- Hosseinpoor, A.R.; Nambiar, D.; Schlotheuber, A.; Reidpath, D.; Ross, Z. Health Equity Assessment Toolkit (HEAT): Software for exploring and comparing health inequalities in countries. BMC Med. Res. Methodol. 2016, 16, 141. [Google Scholar] [CrossRef]
- Arsenault, C.; Harper, S.; Nandi, A.; Rodríguez, J.M.M.; Hansen, P.M.; Johri, M. Monitoring equity in vaccination coverage: A systematic analysis of demographic and health surveys from 45 Gavi-supported countries. Vaccine 2017, 35, 951–959. [Google Scholar] [CrossRef] [PubMed]
- Patenaude, B.; Odihi, D.; Sriudomporn, S.; Mak, J.; Watts, E.; de Broucker, G. A standardized approach for measuring multivariate equity in vaccination coverage, cost-of-illness, and health outcomes: Evidence from the Vaccine Economics Research for Sustainability & Equity (VERSE) project. Soc. Sci. Med. 2022, 302, 114979. [Google Scholar] [CrossRef] [PubMed]
- The Zero-Dose Child: Explained. Gavi.Org. 2021. Available online: https://www.gavi.org/vaccineswork/zero-dose-child-explained (accessed on 12 January 2023).
- Wagstaff, A. The concentration index of a binary outcome revisited: The Concentration Index of a Binary Outcome Revisited. Health Econ. 2011, 20, 1155–1160. Available online: https://openknowledge.worldbank.org/handle/10986/5148 (accessed on 14 July 2022). [CrossRef]
- Barbosa, E.C.; Cookson, R. Multiple inequity in health care: An example from Brazil. Soc. Sci. Med. 2019, 228, 1–8. [Google Scholar] [CrossRef]
- Williams, A.H.; Cookson, R.A. Equity–efficiency trade-offs in health technology assessment. Int. J. Technol. Assess. Health Care 2006, 22, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Fleurbaey, M.; Schokkaert, E. Equity in Health and Health Care11This Chapter was Written When Marc Fleurbaey was Research Associate at CORE. We Thank Chiara Canta, Tom McGuire, Tom Van Ourti and Fred Schrogen for Their Useful Comments. In Handbook of Health Economics; Pauly, M.V., Mcguire, T.G., Barros, P.P., Eds.; Elsevier: Amsterdam, The Netherlands, 2011; pp. 1003–1092. [Google Scholar]
- Fleurbaey, M.; Schokkaert, E. Unfair inequalities in health and health care. J. Health Econ. 2009, 28, 73–90. [Google Scholar] [CrossRef] [PubMed]
- O’Donnell, O. Analyzing Health Equity Using Household Survey Data: A Guide to Techniques and Their Implementation; World Bank Publications: Washington, DC, USA, 2008; Available online: https://openknowledge.worldbank.org/handle/10986/6896 (accessed on 14 July 2022).
- Alonge, O.; Peters, D.H. Utility and limitations of measures of health inequities: A theoretical perspective. Glob. Health Action 2015, 8, 27591. [Google Scholar] [CrossRef] [PubMed]
- McRae, J.; Onukwugha, E. Why the Gap in Evaluating the Social Constructs and the Value of Medicines? Pharmacoeconomics 2021, 39, 1365–1372. [Google Scholar] [CrossRef]
- Joe, W. Intersectional inequalities in immunization in India, 1992–1993 to 2005–06: A progress assessment. Health Policy Plan. 2015, 30, 407–422. [Google Scholar] [CrossRef]
- Heckley, G.; Gerdtham, U.-G.; Kjellsson, G. A general method for decomposing the causes of socioeconomic in-equality in health. J. Health Econ. 2016, 48, 89–106. Available online: https://www.sciencedirect.com/science/article/pii/S0167629616300066 (accessed on 14 July 2022). [CrossRef]
- The DHS Program. Dhsprogram.com. Available online: https://dhsprogram.com/Countries/Country-Main.cfm?ctry_id=63&c=Cambodia (accessed on 14 July 2022).
- Hosseinpoor, A.R.; Bergen, N.; Schlotheuber, A.; Gacic-Dobo, M.; Hansen, P.M.; Senouci, K.; Boerma, T.; Barros, A.J.D. State of inequality in diphtheria-tetanus-pertussis immunisation coverage in low-income and middle-income countries: A multicountry study of household health surveys. Lancet Glob. Health 2016, 4, e617–e626. [Google Scholar] [CrossRef]
- Utazi, C.E.; Thorley, J.; Alegana, V.A.; Ferrari, M.J.; Takahashi, S.; Metcalf, C.J.E.; Lessler, J.; Cutts, F.T.; Tatem, A.J. Mapping vaccination coverage to explore the effects of delivery mechanisms and inform vaccination strategies. Nat. Commun. 2019, 10, 1633. [Google Scholar] [CrossRef]
- National Institute of Statistics, Directorate General for Health, The DHS Program. Cambodia: Demographic and Health Survey 2014; National Institute of Statistics (NIS), Directorate General for Health (DGH), and ICF International: Phnom Penh, Cambodia; Rockville, MD, USA, 2015. [Google Scholar]
- USAID/Cambodia Gender Assessment. 2016 Sep. Available online: https://banyanglobal.com/resource/usaidcambodia-gender-assessment/ (accessed on 27 March 2023).
- National Institute of Public Health/Cambodia, National Institute of Statistics/Cambodia, Macro ORC. Cambodia Demographic and Health Survey 2005. 2006. Available online: https://dhsprogram.com/publications/publication-fr185-dhs-final-reports.cfm (accessed on 27 December 2022).
- National Institute of Statistics/Cambodia, Directorate General for Health/Cambodia, Macro ICF. Cambodia 2010: Results from the demographic and health survey. Stud. Fam. Plann. 2012, 43, 63–68. Available online: https://dhsprogram.com/publications/publication-fr249-dhs-final-reports.cfm (accessed on 14 July 2022). [CrossRef]
- Ngy, M.-H.; Nakamura, K.; Ohnishi, M.; Kizuki, M.; Suyama, S.; Seino, K.; Inose, T.; Umezaki, M.; Watanabe, M.; Takano, T. Improved perinatal health through qualified antenatal care in urban Phnom Penh, Cambodia. Environ. Health Prev. Med. 2007, 12, 193–201. [Google Scholar] [CrossRef]
- Ricchi, A.; La Corte, S.; Molinazzi, M.T.; Messina, M.P.; Banchelli, F.; Neri, I. Study of childbirth education classes and evaluation of their effectiveness. Clin. Ter. 2020, 170, e78–e86. [Google Scholar] [CrossRef] [PubMed]
- Bureau-Point, E.; Baxerres, C.; Chheang, S. Self-Medication and the Pharmaceutical System in Cambodia. Med. Anthr. 2020, 39, 765–781. [Google Scholar] [CrossRef] [PubMed]
- Bhuiy, I.; Bhuiya, A.; Chowdhury, M. Factors affecting acceptance of immunization among children in rural Bangladesh. Health Policy Plan. 1995, 10, 304–311. [Google Scholar] [CrossRef] [PubMed]
- Rainey, J.J.; Watkins, M.; Ryman, T.K.; Sandhu, P.; Bo, A.; Banerjee, K. Reasons related to non-vaccination and under-vaccination of children in low and middle income countries: Findings from a systematic review of the published literature, 1999–2009. Vaccine 2011, 29, 8215–8221. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, C.T.T.; Grappasonni, I.; Scuri, S.; Nguyen, B.T.; Nguyen, T.T.T.; Petrelli, F. Immunization in Vietnam. Ann. Di Ig. Med. Prev. E Di Comunità 2019, 31, 291–305. [Google Scholar] [CrossRef]
- Corsi, D.J.; Neuman, M.; Finlay, J.E.; Subramanian, S.V. Demographic and health surveys: A profile. Int. J. Epidemiol. 2012, 41, 1602–1613. [Google Scholar] [CrossRef]
- Boerma, J.T.; Sommerfelt, A.E. Demographic and health surveys (DHS): Contributions and limitations. World Health Stat. Q. 1993, 46, 222–226. [Google Scholar]

| Wagstaff Concentration Index | ||||
|---|---|---|---|---|
| Vaccine or Outcome 1 | Proportion Covered | Wealth Only 2 | Composite | Absolute Equity Gap |
| BCG | 94.0% | 0.013 | 0.031 | 0.146 |
| DTP1 | 91.8% | 0.016 | 0.033 | 0.155 |
| DTP2 | 87.4% | 0.026 | 0.05 | 0.206 |
| DTP3 | 82.0% | 0.031 | 0.062 | 0.235 |
| OPV1 | 92.5% | 0.014 | 0.029 | 0.122 |
| OPV2 | 87.6% | 0.024 | 0.048 | 0.197 |
| OPV3 | 81.6% | 0.03 | 0.063 | 0.239 |
| MCV1 | 80.3% | 0.024 | 0.047 | 0.195 |
| ZERO | 3.3% | −0.014 | 0.573 | 0.091 |
| FULL | 78.4% | 0.031 | 0.077 | 0.303 |
| COMPLETE | 84.5% | 0.028 | 0.067 | 0.28 |
| District | Vaccine or Health Outcome Coverage | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| BCG | DTP1 | DTP2 | DTP3 | OPV1 | OPV2 | OPV3 | MCV1 | ZERO | FULL | COMPLETE | |
| Banteay Meanchey | 96.8% | 94.9% | 91.8% | 90.0% | 95.7% | 92.6% | 90.2% | 86.9% | 0.8% | 89.3% | 97.2% |
| Battambang & Pailin | 99.5% | 95.2% | 89.0% | 85.0% | 95.3% | 89.3% | 83.4% | 82.1% | 0.7% | 82.7% | 87.2% |
| Kampong Cham | 92.0% | 85.1% | 81.6% | 75.0% | 88.6% | 82.9% | 76.1% | 74.4% | 3.8% | 71.7% | 76.8% |
| Kampong Chhnang | 98.9% | 95.5% | 90.6% | 87.0% | 95.5% | 90.6% | 86.5% | 82.8% | 0.7% | 83.9% | 92.7% |
| Kampong Speu | 95.7% | 92.7% | 89.5% | 82.0% | 93.0% | 88.8% | 81.7% | 77.0% | 1.6% | 80.5% | 86.9% |
| Kampong Thom | 96.3% | 93.2% | 90.0% | 87.0% | 94.1% | 90.9% | 86.6% | 81.5% | 1.8% | 86.0% | 96.4% |
| Kampot & Kep | 87.8% | 86.4% | 80.0% | 76.0% | 87.4% | 80.6% | 75.2% | 77.1% | 7.8% | 73.2% | 78.3% |
| Kandal | 96.3% | 96.6% | 92.0% | 84.0% | 95.6% | 90.5% | 81.9% | 81.0% | 0.7% | 76.0% | 85.1% |
| Kratie | 84.4% | 87.8% | 78.8% | 71.0% | 87.7% | 79.4% | 71.3% | 79.9% | 8.0% | 67.0% | 75.3% |
| Mondulkiri & Ratanakiri | 79.1% | 76.7% | 67.4% | 57.0% | 78.8% | 67.2% | 56.8% | 66.8% | 16.5% | 51.9% | 59.6% |
| Oddar Meanchey | 93.8% | 88.8% | 81.8% | 78.0% | 89.5% | 81.6% | 77.4% | 77.6% | 3.5% | 75.0% | 79.6% |
| Phnom Penh | 97.6% | 98.3% | 95.5% | 92.0% | 97.6% | 95.7% | 91.2% | 90.1% | 0.0% | 88.1% | 93.2% |
| Preah Sihanouk & Koh Kong | 94.6% | 92.6% | 88.8% | 85.0% | 92.4% | 88.6% | 85.4% | 83.1% | 2.9% | 84.2% | 89.8% |
| Preah Vihear & Stung Treng | 90.1% | 92.3% | 87.8% | 80.0% | 92.8% | 87.7% | 79.0% | 74.7% | 3.3% | 72.4% | 80.4% |
| Prey Veng | 92.7% | 91.5% | 86.4% | 80.0% | 91.8% | 86.4% | 80.3% | 75.2% | 4.5% | 76.1% | 87.6% |
| Pursat | 92.8% | 91.8% | 88.0% | 83.0% | 92.5% | 88.8% | 83.4% | 81.4% | 8.1% | 84.3% | 86.6% |
| Siem Reap | 95.0% | 95.9% | 92.0% | 84.0% | 95.2% | 92.5% | 84.9% | 82.8% | 2.9% | 79.8% | 80.2% |
| Svay Rieng | 93.5% | 90.2% | 86.9% | 84.0% | 90.1% | 86.9% | 83.6% | 82.2% | 3.1% | 81.0% | 88.1% |
| Takeo | 95.5% | 92.8% | 88.9% | 87.0% | 94.4% | 88.9% | 85.7% | 87.9% | 1.9% | 80.9% | 87.0% |
| District | Vaccine or Health Outcome Wagstaff Composite Concentration Index | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| BCG | DTP1 | DTP2 | DTP3 | OPV1 | OPV2 | OPV3 | MCV1 | ZERO | FULL | COMPLETE | |
| Banteay Meanchey | 0.019 | 0.017 | 0.037 | 0.031 | 0.017 | 0.038 | 0.032 | 0.03 | 0.839 | 0.029 | 0.013 |
| Battambang & Pailin | −0.003 | 0.019 | 0.043 | 0.049 | 0.015 | 0.031 | 0.046 | 0.045 | 0.789 | 0.027 | 0.049 |
| Kampong Cham | 0.022 | 0.035 | 0.032 | 0.043 | 0.022 | 0.032 | 0.045 | 0.05 | 0.406 | 0.06 | 0.033 |
| Kampong Chhnang | −0.004 | −0.001 | 0 | 0.006 | 0.004 | 0.002 | 0.014 | −0.001 | 0.727 | 0.015 | 0.011 |
| Kampong Speu | 0.016 | 0.02 | 0.029 | 0.042 | 0.019 | 0.028 | 0.042 | 0.024 | 0.646 | 0.062 | 0.046 |
| Kampong Thom | 0.015 | 0.022 | 0.031 | 0.044 | 0.02 | 0.027 | 0.04 | 0.028 | −0.032 | 0.053 | 0.013 |
| Kampot & Kep | 0.032 | 0.059 | 0.067 | 0.088 | 0.052 | 0.065 | 0.093 | 0.068 | 0.563 | 0.11 | 0.094 |
| Kandal | 0.002 | 0.014 | 0.03 | 0.061 | 0.014 | 0.029 | 0.065 | 0.03 | −0.492 | 0.08 | 0.065 |
| Kratie | 0.049 | 0.034 | 0.064 | 0.099 | 0.037 | 0.067 | 0.095 | 0.032 | 0.334 | 0.109 | 0.089 |
| Mondulkiri & Ratanakiri | 0.111 | 0.1 | 0.148 | 0.184 | 0.099 | 0.159 | 0.191 | 0.143 | 0.592 | 0.235 | 0.221 |
| Oddar Meanchey | 0.018 | 0.023 | 0.037 | 0.043 | 0.022 | 0.04 | 0.046 | 0.027 | 0.363 | 0.074 | 0.064 |
| Phnom Penh | 0.001 | 0 | 0.012 | 0.025 | 0.003 | 0.014 | 0.023 | 0.008 | NA | 0.053 | 0.031 |
| Preah Sihanouk & Koh Kong | 0.02 | 0.031 | 0.05 | 0.057 | 0.032 | 0.048 | 0.057 | 0.065 | 0.114 | 0.042 | 0.032 |
| Preah Vihear & Stung Treng | 0.015 | 0.01 | 0.011 | 0.016 | 0.007 | 0.004 | 0.018 | 0.006 | 0.367 | 0.034 | 0.019 |
| Prey Veng | 0.005 | 0.015 | 0.035 | 0.057 | 0.016 | 0.04 | 0.059 | 0.048 | 0.471 | 0.085 | 0.05 |
| Pursat | 0.016 | 0.005 | 0.019 | 0.031 | 0.007 | 0.016 | 0.029 | 0.019 | 0.407 | 0.04 | 0.039 |
| Siem Reap | −0.002 | 0.004 | 0.015 | 0.024 | 0.004 | 0.017 | 0.012 | 0.017 | 0.363 | 0.027 | 0.045 |
| Svay Rieng | 0.003 | 0.02 | 0.037 | 0.041 | 0.021 | 0.035 | 0.035 | 0.016 | −0.042 | 0.021 | 0.019 |
| Takeo | 0.019 | 0.031 | 0.028 | 0.025 | 0.01 | 0.013 | 0.026 | 0.026 | 0.163 | 0.014 | −0.013 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhao, Y.; Mak, J.; de Broucker, G.; Patenaude, B. Multivariate Assessment of Vaccine Equity in Cambodia: A Longitudinal VERSE Tool Case Study Using Demographic and Health Survey 2004, 2010, and 2014. Vaccines 2023, 11, 795. https://doi.org/10.3390/vaccines11040795
Zhao Y, Mak J, de Broucker G, Patenaude B. Multivariate Assessment of Vaccine Equity in Cambodia: A Longitudinal VERSE Tool Case Study Using Demographic and Health Survey 2004, 2010, and 2014. Vaccines. 2023; 11(4):795. https://doi.org/10.3390/vaccines11040795
Chicago/Turabian StyleZhao, Yijin, Joshua Mak, Gatien de Broucker, and Bryan Patenaude. 2023. "Multivariate Assessment of Vaccine Equity in Cambodia: A Longitudinal VERSE Tool Case Study Using Demographic and Health Survey 2004, 2010, and 2014" Vaccines 11, no. 4: 795. https://doi.org/10.3390/vaccines11040795
APA StyleZhao, Y., Mak, J., de Broucker, G., & Patenaude, B. (2023). Multivariate Assessment of Vaccine Equity in Cambodia: A Longitudinal VERSE Tool Case Study Using Demographic and Health Survey 2004, 2010, and 2014. Vaccines, 11(4), 795. https://doi.org/10.3390/vaccines11040795







