COVID-19 Vaccines Status, Acceptance and Hesitancy among Maintenance Hemodialysis Patients: A Cross-Sectional Study and the Implications for Pakistan and Beyond
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design, Population and Location
2.2. Study Instrument
- Section-I: This section collected data on the demographics of the study population, hemodialysis-related details and the COVID-19 vaccination status.
- Section-II: This section consisted of nine questions relating to the factors associated with the acceptance of COVID-19 vaccines among the study population. Each question had a ‘yes’ and ‘no’ option, and participants were requested to select one option for each question.
- Section-III: This section collected information on the reasons for COVID-19 vaccine hesitancy among study participants. There were twelve questions in this section and, similar to Section II, two response options were available, ‘yes’ and ‘no’, of which respondents had to select one option.
2.3. Sample Size Calculation
2.4. Sampling and Data Collection Procedure
2.5. Statistical Analysis
2.6. Ethical Approval
3. Results
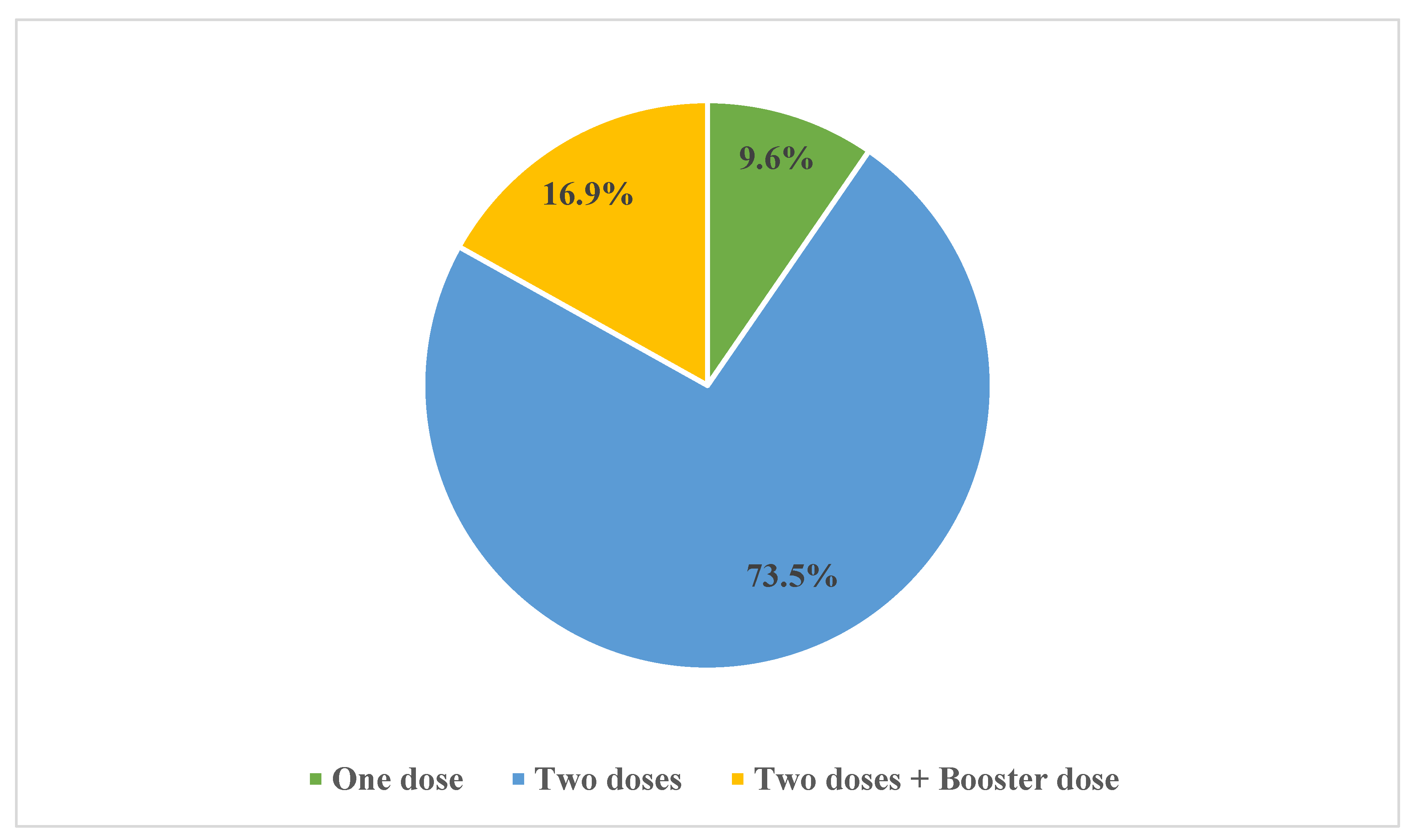
3.1. COVID-19 Vaccination Status among MHD Patients
3.2. Reasons for COVID-19 Vaccine Acceptance
3.3. Reasons for COVID-19 Vaccine Hesitancy
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Richards, F.; Kodjamanova, P.; Chen, X.; Li, N.; Atanasov, P.; Bennetts, L.; Patterson, B.J.; Yektashenas, B.; Mesa-Frias, M.; Tronczynski, K.; et al. Economic Burden of COVID-19: A Systematic Review. Clin. Outcomes Res. 2022, 14, 293–307. [Google Scholar] [CrossRef] [PubMed]
- Fatoye, F.; Gebrye, T.; Arije, O.; Fatoye, C.T.; Onigbinde, O.; Mbada, C.E. Economic Impact of COVID-19 Lockdown on households. Pan Afr. Med. J. 2021, 40, 225. [Google Scholar] [CrossRef] [PubMed]
- Bonotti, M.; Zech, S.T. The Human, Economic, Social, and Political Costs of COVID-19. Recover. Civ. Dur. COVID-19 2021, 1–36. [Google Scholar]
- WHO. WHO Coronavirus (COVID-19) Dashboard. 2022. Available online: https://covid19.who.int/ (accessed on 15 February 2023).
- Chiesa, V.; Antony, G.; Wismar, M.; Rechel, B. COVID-19 pandemic: Health impact of staying at home, social distancing ‘and ‘lock ’own’ measures-a systematic review of systematic reviews. J. Public Health 2021, 43, e462–e481. [Google Scholar] [CrossRef] [PubMed]
- Shang, Y.; Li, H.; Zhang, R. Effects of Pandemic Outbreak on Economies: Evidence From Business History Context. Front. Public Health 2021, 9, 632043. [Google Scholar] [CrossRef] [PubMed]
- Naseer, S.; Khalid, S.; Parveen, S.; Abbass, K.; Song, H.; Achim, M.V. COVID-19 outbreak: Impact on global economy. Front. Public Health 2022, 10, 1009393. [Google Scholar] [CrossRef]
- Rasheed, R.; Rizwan, A.; Javed, H.; Sharif, F.; Zaidi, A. Socio-economic and environmental impacts of COVID-19 pandemic in Pakistan—An integrated analysis. Environ. Sci. Pollut. Res. 2021, 28, 19926–19943. [Google Scholar] [CrossRef]
- Cheema, A.; Rehman, M. COVID-19 Pandemic’s Economic Burden in Pakistan. 2021. Available online: https://mhrc.lums.edu.pk/covid-19-pandemics-economic-burden-in-pakistan/ (accessed on 15 April 2023).
- Panneer, S.; Kantamaneni, K.; Akkayasamy, V.S.; Susairaj, A.X.; Panda, P.K.; Acharya, S.S.; Rice, L.; Liyanage, C.; Pushparaj, R.R.B. The Great Lockdown in the Wake of COVID-19 and Its Implications: Lessons for Low and Middle-Income Countries. Int. J. Environ. Res. Public Health 2022, 19, 610. [Google Scholar] [CrossRef]
- Gebru, A.A.; Birhanu, T.; Wendimu, E.; Ayalew, A.F.; Mulat, S.; Abasimel, H.Z.; Kazemi, A.; Tadesse, B.A.; Gebru, B.A.; Deriba, B.S.; et al. Global burden of COVID-19: Situational analysis and review. Hum. Antibodies 2021, 29, 139–148. [Google Scholar] [CrossRef]
- Muller, A.E.; Hafstad, E.V.; Himmels, J.P.W.; Smedslund, G.; Flottorp, S.; Stensland, S.Ø.; Stroobants, S.; Van De Velde, S.; Vist, G.E. The mental health impact of the covid-19 pandemic on healthcare workers, and interventions to help them: A rapid systematic review. Psychiatr. Res. 2020, 293, 113441. [Google Scholar] [CrossRef]
- Salman, M.; Mustafa, Z.U.; Khan, T.M.; Shehzadi, N.; Hussain, K. How prepared was Pakistan for the COVID-19 outbreak? Disaster Med. Public Health Prep. 2020, 14, e44–e45. [Google Scholar] [CrossRef] [PubMed]
- Ramzan, K.; Shafiq, S.; Raees, I.; Mustafa, Z.U.; Salman, M.; Khan, A.H.; Meyer, J.C.; Godman, B. Co-Infections, Secondary Infections, and Antimicrobial Use in Patients Hospitalized with COVID-19 during the First Five Waves of the Pandemic in Pakistan; Findings and Implications. Antibiotics 2022, 11, 789. [Google Scholar] [CrossRef] [PubMed]
- Rahim, S.; Dhrolia, M.; Qureshi, R.; Nasir, K.; Ahmad, A. A Comparative Study of the First and Second Waves of COVID-19 in Hemodialysis Patients From Pakistan. Cureus 2022, 14, e21512. [Google Scholar] [CrossRef] [PubMed]
- Imran, M.; Khan, S.; Khan, S.; Uddin, A.; Khan, M.S.; Ambade, K.A. COVID-19 situation in Pakistan: A broad overview. Respirology 2021, 26, 891–892. [Google Scholar] [CrossRef]
- Godman, B.; Haque, M.; Islam, S.; Iqbal, S.; Urmi, U.L.; Kamal, Z.M.; Shuvo, S.A.; Rahman, A.; Kamal, M.; Haque, M.; et al. Rapid Assessment of Price Instability and Paucity of Medicines and Protection for COVID-19 Across Asia: Findings and Public Health Implications for the Future. Front. Public Health 2020, 8, 585832. [Google Scholar] [CrossRef]
- Ayouni, I.; Maatoug, J.; Dhouib, W.; Zammit, N.; Ben Fredj, S.; Ghammam, R.; Ghannem, H. Effective public health measures to mitigate the spread of COVID-19: A systematic review. BMC Public Health 2021, 21, 1015. [Google Scholar] [CrossRef] [PubMed]
- Talic, S.; Shah, S.; Wild, H.; Gasevic, D.; Maharaj, A.; Ademi, Z.; Li, X.; Xu, W.; Mesa-Eguiagaray, I.; Rostron, J.; et al. Effectiveness of public health measures in reducing the incidence of covid-19, SARS-CoV-2 transmission, and covid-19 mortality: Systematic review and meta-analysis. BMJ 2021, 375, e068302. [Google Scholar] [CrossRef]
- Looi, M.K. COVID-19: Is a second wave hitting Europe? BMJ 2020, 371, m4113. [Google Scholar] [CrossRef]
- Shahid, R.; Zeb, S. Second Wave of COVID-19 Pandemic: Its deleterious and mortal repercussion in Pakistan. J. Rawalpindi Med. Coll. 2020, 24, 288–289. [Google Scholar] [CrossRef]
- Basheer, A.; Zahoor, I. Genomic Epidemiology of SARS-CoV-2 Divulge B.1, B.1.36, and B.1.1.7 as the Most Dominant Lineages in First, Second, and Third Wave of SARS-CoV-2 Infections in Pakistan. Microorganisms 2021, 9, 2609. [Google Scholar] [CrossRef]
- Kamran, K.; Ali, A. Challenges and Strategies for Pakistan in the Third Wave of COVID-19: A Mini Review. Front. Public Health 2021, 9, 690820. [Google Scholar] [CrossRef] [PubMed]
- The United Nations Children’s Fund (UNICEF). Pakistan Humanitarian. Situation Report No. 28. 2021. Available online: https://www.unicef.org/media/107031/file/%20Pakistan-Humanitarian-sitRep-No28-31-August-2021.pdf (accessed on 21 March 2022).
- Geo News. COVID-19 Situation Continues to Worsen in Pakistan Amid Fifth Wave. 2021. Available online: https://www.geo.tv/latest/394761-covid-19-situation-continues-to-worsen-in-pakistan-amid-fifth-wavepdf (accessed on 21 March 2022).
- National Disaster Management Authority (NDMA). 2022. Available online: http://cms.ndma.gov.pk/ (accessed on 16 April 2023).
- National Command and Operation Center (NCOC); Government of Islamic Government of Pakistan. 2022. Available online: https://ncoc.gov.pk/ (accessed on 17 April 2023).
- Sarfaraz, S.; Shaikh, Q.; Saleem, S.G.; Rahim, A.; Herekar, F.F.; Junejo, S.; Hussain, A. Determinants of in-hospital mortality in COVID-19; a prospective cohort study from Pakistan. PLoS ONE 2021, 16, e0251754. [Google Scholar] [CrossRef] [PubMed]
- Kamran, S.H.; Ul Mustafa, Z.; Rao, A.Z.; Hasan, S.S.; Zahoor, F.; Sarwar, M.U.; Khan, S.; Butt, S.; Rameez, M.; Abbas, M.A. SARS-CoV-2 infection pattern, transmission and treatment: Multicenter study in low to middle-income districts hospitals in Punjab, Pakistan. Pak. J. Pharm. Sci. 2021, 34, 1135–1142. [Google Scholar] [PubMed]
- Mustafa, Z.U.; Kow, C.S.; Salman, M.; Kanwal, M.; Riaz, M.B.; Parveen, S.; Hasan, S.S. Pattern of medication utilization in hospitalized patients with COVID-19 in three District Headquarters Hospitals in the Punjab province of Pakistan. Explor. Res. Clin. Soc. Pharm. 2022, 5, 100101. [Google Scholar] [CrossRef]
- Khattak, S.; Khan, M.; Usman, T.; Ali, J.; Wu, D.-X.; Jahangir, M.; Haleem, K.; Muhammad, P.; Rauf, M.A.; Saddique, K.; et al. Assessment of General Populations Knowledge, Attitude, and Perceptions Toward the Coronavirus Disease (COVID-19): A Cross-Sectional Study From Pakistan. Front. Med. 2021, 8, 747819. [Google Scholar] [CrossRef]
- Ladiwala, Z.F.R.; Dhillon, R.A.; Zahid, I.; Irfan, O.; Khan, M.S.; Awan, S.; Khan, J.A. Knowledge, attitude and perception of Pakistanis towards COVID-19; a large cross-sectional survey. BMC Public Health 2021, 21, 21. [Google Scholar] [CrossRef]
- Salman, M.; Mustafa, Z.U.; Asif, N.; Zaidi, H.A.; Hussain, K.; Shehzadi, N.; Khan, T.M.; Saleem, Z. Knowledge, attitude and preventive practices related to COVID-19: A cross-sectional study in two Pakistani university populations. Drugs Ther. Perspect. 2020, 36, 319–325. [Google Scholar] [CrossRef]
- Salman, M.; Mustafa, Z.; Asif, N.; Zaidi, H.A.; Shehzadi, N.; Khan, T.M.; Saleem, Z.; Hussain, K. Knowledge, attitude and preventive practices related to COVID-19 among health professionals of Punjab province of Pakistan. J. Infect. Dev. Ctries. 2020, 14, 707–712. [Google Scholar] [CrossRef]
- Mustafa, Z.U.; Majeed, H.K.; Latif, S.; Salman, M.; Hayat, K.; Mallhi, T.H.; Khan, Y.H.; Khan, A.H.; Abubakar, U.; Sultana, K.; et al. Adherence to Infection Prevention and Control Measures Among Health-Care Workers Serving in COVID-19 Treatment Centers in Punjab, Pakistan. Disaster Med. Public Health Prep. 2023, 17, e298. [Google Scholar] [CrossRef]
- Horby, P.; Mafham, M.; Linsell, L.; Bell, J.L.; Staplin, N.; Emberson, J.R.; Wiselka, M.; Ustianowski, A.; Elmahi, E. Effect of Hydroxychloroquine in Hospitalized Patients with COVID-19. N. Engl. J. Med. 2020, 383, 2030–2040. [Google Scholar]
- Horby, P.W.; Mafham, M.; Bell, J.L.; Linsell, L.; Staplin, N.; Emberson, J.; Palfreeman, A.; Raw, J.; Elmahi, E.; Prudon, B.; et al. Lopinavir-ritonavir in patients admitted to hospital with COVID-19 (RECOVERY): A randomised, controlled, open-label, platform trial. Lancet 2020, 396, 1345–1352. [Google Scholar] [CrossRef] [PubMed]
- Dyer, O. COVID-19: Remdesivir has little or no impact on survival, WHO trial shows. BMJ 2020, 371, m4057. [Google Scholar] [CrossRef] [PubMed]
- Schellack, N.; Strydom, M.; Pepper, M.S.; Herd, C.L.; Hendricks, C.L.; Bronkhorst, E.; Meyer, J.C.; Padayachee, N.; Bangalee, V.; Truter, I.; et al. Social Media and COVID-19: Perceptions and Public Deceptions of Ivermectin, Colchicine and Hydroxychloroquine: Lessons for Future Pandemics. Antibiotics 2022, 11, 445. [Google Scholar] [CrossRef] [PubMed]
- Mohammed, I.; Nauman, A.; Paul, P.; Ganesan, S.; Chen, K.-H.; Jalil, S.M.S.; Jaouni, S.H.; Kawas, H.; Khan, W.A.; Vattoth, A.L.; et al. The efficacy and effectiveness of the COVID-19 vaccines in reducing infection, severity, hospitalization, and mortality: A systematic review. Hum. Vaccines Immunother. 2022, 18, 2027160. [Google Scholar] [CrossRef]
- Korang, S.K.; von Rohden, E.; Veroniki, A.A.; Ong, G.; Ngalamika, O.; Siddiqui, F.; Juul, S.; Nielsen, E.E.; Feinberg, J.B.; Petersen, J.J.; et al. Vaccines to prevent COVID-19: A living systematic review with Trial Sequential Analysis and network meta-analysis of randomized clinical trials. PLoS ONE 2022, 17, e0260733. [Google Scholar] [CrossRef]
- Khandker, S.S.; Godman, B.; Jawad, I.; Meghla, B.A.; Tisha, T.A.; Khondoker, M.U.; Haq, A.; Charan, J.; Talukder, A.A.; Azmuda, N.; et al. A Systematic Review on COVID-19 Vaccine Strategies, Their Effectiveness, and Issues. Vaccines 2021, 9, 1387. [Google Scholar] [CrossRef]
- Martínez-Baz, I.; Miqueleiz, A.; Casado, I.; Navascués, A.; Trobajo-Sanmartín, C.; Burgui, C.; Guevara, M.; Ezpeleta, C.; Castilla, J. Effectiveness of COVID-19 vaccines in preventing SARS-CoV-2 infection and hospitalisation, Navarre, Spain, January to April 2021. Euro. Surveill. 2021, 26, 2100438. [Google Scholar] [CrossRef]
- Rodrigues, C.; Plotkin, S.A. Impact of Vaccines; Health, Economic and Social Perspectives. Front. Microbiol. 2020, 11, 1526. [Google Scholar] [CrossRef]
- Tribune. Govt to Start COVID-19 Vaccination Drive in Ap–il-Parliamentary Secretary Says Vaccines will be Provided Free of charge. Available online: https://tribune.com.pk/story/2274372/pti-govt-to-provide-coronavirus-vaccine-for-free (accessed on 15 April 2023).
- Voice of America. Pakistan Starts COVID-19 Inoculation Drive. 24 October 2021. Available online: https://www.voanews.com/covid-19-pandemic/pakistan-starts-covid-19-inoculation-drive (accessed on 15 April 2023).
- Aljazeera. Pakistan Kicks off COVID Vaccination Drive for Senior Citizens. Available online: https://www.aljazeera.com/news/2021/3/10/pakistan-kicks-off-senior-citizen-coronavirus-vaccinations (accessed on 15 April 2023).
- National Command and Operation Center (NCOC). Get Vaccinated-Save Lives. Available online: https://ncoc.gov.pk/ (accessed on 15 April 2023).
- Siddiqui, A.; Ahmed, A.; Tanveer, M.; Saqlain, M.; Kow, C.S.; Hasan, S.S. An overview of procurement, pricing, and uptake of COVID-19 vaccines in Pakistan. Vaccine 2021, 39, 5251–5253. [Google Scholar] [CrossRef]
- NDMA. Available online: https://bing.com/covid/local/pakistan (accessed on 16 April 2023).
- Shrestha, N.; Gautam, S.; Mishra, S.R.; Virani, S.S.; Dhungana, R.R. Burden of chronic kidney disease in the general population and high-risk groups in South Asia: A systematic review and meta-analysis. PLoS ONE 2021, 16, e0258494. [Google Scholar] [CrossRef]
- Hasan, M.; Sutradhar, I.; Das Gupta, R.; Sarker, M. Prevalence of chronic kidney disease in South Asia: A systematic review. BMC Nephrol. 2018, 19, 291. [Google Scholar] [CrossRef] [PubMed]
- Alam, A.; Amanullah, F.; Baig-Ansari, N.; Lotia-Farrukh, I.; Khan, F.S. Prevalence and risk factors of kidney disease in urban Karachi: Baseline findings from a community cohort study. BMC Res. Notes 2014, 7, 179. [Google Scholar] [CrossRef] [PubMed]
- Yeung, E.; Bello, A.; Levin, A.; Lunney, M.; Osman, A.M.; Ye, F.; Ashuntantang, G.; Bellorin-Font, E.; Gharbi, M.B.; Davison, S.; et al. Current status of health systems financing and oversight for end-stage kidney disease care: A cross-sectional global survey. BMJ Open 2021, 11, e047245. [Google Scholar] [CrossRef]
- Bello, A.K.; Levin, A.; Lunney, M.; Osman, A.M.; Ye, F.; E Ashuntantang, G.E.; Bellorin-Font, E.; Gharbi, M.B.; Davison, S.N.; Ghnaimat, M.; et al. Status of care for end stage kidney disease in countries and regions worldwide: International cross sectional survey. BMJ 2019, 367, l5873. [Google Scholar] [CrossRef] [PubMed]
- United States Renal Data System. 2020 USRDS Annual Data Report: Epidemiology of Kidney Disease in the United States; National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases: Bethesda, MD, USA, 2020. [Google Scholar]
- Sharif, M.R.; Chitsazian, Z.; Moosavian, M.; Raygan, F.; Nikoueinejad, H.; Sharif, A.R.; Einollahi, B. Immune disorders in hemodialysis patients. Iran. J. Kidney Dis. 2015, 9, 84–96. [Google Scholar] [PubMed]
- Hsu, C.M.; Weiner, D.E.; Aweh, G.; Miskulin, D.C.; Manley, H.J.; Stewart, C.; Ladik, V.; Hosford, J.; Lacson, E.C.; Johnson, D.S.; et al. COVID-19 Among US Dialysis Patients: Risk Factors and Outcomes From a National Dialysis Provider. Am. J. Kidney Dis. 2021, 77, 748–756.e1. [Google Scholar] [CrossRef]
- De Meester, J.; De Bacquer, D.; Naesens, M.; Meijers, B.; Couttenye, M.M.; De Vriese, A.S.; NBVN Kidney Registry Group. Incidence, Characteristics, and Outcome of COVID-19 in Adults on Kidney Replacement Therapy: A Regionwide Registry Study. J. Am. Soc. Nephrol. 2021, 32, 385–396. [Google Scholar] [CrossRef]
- Clarke, C.; Prendecki, M.; Dhutia, A.; Ali, M.A.; Sajjad, H.; Shivakumar, O.; Lightstone, L.; Kelleher, P.; Pickering, M.C.; Thomas, D.; et al. High Prevalence of Asymptomatic COVID-19 Infection in Hemodialysis Patients Detected Using Serologic Screening. J. Am. Soc. Nephrol. 2020, 31, 1969–1975. [Google Scholar] [CrossRef]
- Creput, C.; Fumeron, C.; Toledano, D.; Diaconita, M.; Izzedine, H. COVID-19 in Patients Undergoing Hemodialysis: Prevalence and Asymptomatic Screening During a Period of High Community Prevalence in a Large Paris Center. Kidney Med. 2020, 2, 716–723.e711. [Google Scholar] [CrossRef]
- Saleem, Z.; Hassali, M.A.; Hashmi, F.K. Pakistan’s national action plan for antimicrobial resistance: Translating ideas into reality. Lancet Infect. Dis. 2018, 18, 1066–1067. [Google Scholar] [CrossRef]
- Mustafa, Z.U.; Saleem, M.S.; Ikram, M.N.; Salman, M.; Butt, S.A.; Khan, S.; Godman, B.; Seaton, R.A. Co-infections and antimicrobial use among hospitalized COVID-19 patients in Punjab, Pakistan: Findings from a multicenter, point prevalence survey. Pathog. Glob. Health 2022, 116, 421–427. [Google Scholar] [CrossRef] [PubMed]
- Amjad, A.; Kumar, J.; Chaudary, N.; Kumar, K.; Nazar, C.M.; Khan, K.; Karmani, S.J.K.; Hepatitis, B. Vaccination status in chronic kidney disease: Experience at Pakistan institute of medical sciences. Cureus 2019, 11, e5282. [Google Scholar] [CrossRef] [PubMed]
- Khan, Y.H.; Mallhi, T.H.; Alotaibi, N.H.; Alzarea, A.I.; Alanazi, A.S.; Tanveer, N.; Hashmi, F.K. Threat of COVID-19 Vaccine Hesitancy in Pakistan: The Need for Measures to Neutralize Misleading Narratives. Am. J. Trop. Med. Hyg. 2020, 103, 603–604. [Google Scholar] [CrossRef] [PubMed]
- Tahir, M.J.; Saqlain, M.; Tariq, W.; Waheed, S.; Tan, S.H.S.; Nasir, S.I.; Ullah, I.; Ahmed, A. Population preferences and attitudes towards COVID-19 vaccination: A cross-sectional study from Pakistan. BMC Public Health 2021, 21, 1759. [Google Scholar] [CrossRef]
- Kashif, M.; Fatima, I.; Ahmed, A.M.; Ali, S.A.; Memon, R.S.; Afzal, M.; Saeed, U.; Gul, S.; Ahmad, J.; Malik, F.; et al. Perception, willingness, barriers, and hesitancy towards COVID-19 vaccine in Pakistan: Comparison between healthcare workers and general population. Cureus 2021, 13, e19106. [Google Scholar] [CrossRef]
- Malik, A.; Malik, J.; Ishaq, U. Acceptance of COVID-19 vaccine in Pakistan among health care workers. PLoS ONE 2021, 16, e0257237. [Google Scholar] [CrossRef]
- Ogunleye, O.O.; Godman, B.; Fadare, J.O.; Mudenda, S.; Adeoti, A.O.; Yinka-Ogunleye, A.F.; Ogundele, S.O.; Oyawole, M.R.; Schönfeldt, M.; Rashed, W.M.; et al. Coronavirus Disease 2019 (COVID-19) Pandemic across Africa: Current Status of Vaccinations and Implications for the Future. Vaccines 2022, 10, 1553. [Google Scholar] [CrossRef]
- Ennab, F.; Qabsa, R.K.; Uday, U.; Priya, P.; Qamar, K.; Nawaz, F.A.; Islam, Z.; Zary, N. COVID-19 vaccine hesitancy: A narrative review of four South Asian countries. Front. Public Health 2022, 10, 997884. [Google Scholar] [CrossRef]
- Perveen, S.; Akram, M.; Nasar, A.; Arshad-Ayaz, A.; Naseem, A. Vaccination-hesitancy and vaccination-inequality as challenges in Pakistan’s COVID-19 response. J. Community Psychol. 2022, 50, 666–683. [Google Scholar] [CrossRef]
- Zakar, R.; Momina, A.U.; Shahzad, S.; Hayee, M.; Shahzad, R.; Zakar, M.Z. COVID-19 Vaccination Hesitancy or Acceptance and Its Associated Factors: Findings from Post-Vaccination Cross-Sectional Survey from Punjab Pakistan. Int. J. Environ. Res. Public Health 2022, 19, 1305. [Google Scholar] [CrossRef]
- Mustafa, Z.U.; Salman, M.; Yasir, M.; Godman, B.; Majeed, H.A.; Kanwal, M.; Iqbal, M.; Riaz, M.B.; Hayat, K.; Hasan, S.S. Antibiotic consumption among hospitalized neonates and children in Punjab province, Pakistan. Expert Rev. Anti-Infect. Ther. 2020, 20, 931–939. [Google Scholar] [CrossRef] [PubMed]
- Patel, P.R.; Tanz, L.J.; Hamilton, E.; Swanzy, K.; Hymes, J.L.; Giullian, J.; Novosad, S.A. Assessment of Provision of COVID-19 Vaccination in Dialysis Clinics and Patient Vaccination Coverage. JAMA Intern. Med. 2022, 182, 676. [Google Scholar] [CrossRef] [PubMed]
- Mosconi, G.; Fantini, M.; Righini, M.; Flachi, M.; Semprini, S.; Hu, L.; Chiappo, F.; Veterani, B.; Ambri, K.; Ferrini, F.; et al. Efficacy of SARS-CoV-2 Vaccination in Dialysis Patients: Epidemiological Analysis and Evaluation of the Clinical Progress. J. Clin. Med. 2022, 11, 4723. [Google Scholar] [CrossRef] [PubMed]
- Moore, L.R.; Al-Jaddou, N.; Wodeyar, H.; Sharma, A.; Schulz, M.; Rao, A.; Abraham, K. SARS-CoV-2 in dialysis patients and the impact of vaccination. BMC Nephrol. 2022, 23, 317. [Google Scholar] [CrossRef]
- Tharwat, S.; Khairallah, M.K.; Nassar, M.K.; Nassar, D.K.; Nagy, E. Acceptance of COVID-19 vaccination among maintenance hemodialysis patients: An Egyptian survey study. Trop. Med. Health 2022, 50, 42. [Google Scholar] [CrossRef] [PubMed]
- Hasan, S.S.; Rashid, A.; Osama, S.; Mustafa, Z.U.; Merchant, H.A. COVID-19 Vaccine safety and adverse event analysis from Pakistan. Clin. Immunol. Commun. 2022, 2, 91–97. [Google Scholar] [CrossRef]
- Baraka, M.A.; Manzoor, M.N.; Ayoub, U.; Aljowaie, R.M.; Mustafa, Z.U.; Zaidi, S.T.R.; Salman, M.; Kow, C.S.; Aldeyab, M.A.; Hasan, S.S. Vaccine Acceptance and Hesitancy among Hospitalized COVID-19 Patients in Punjab, Pakistan. Vaccines 2022, 10, 1640. [Google Scholar] [CrossRef]
- Mustafa, Z.U.; Bashir, S.; Shahid, A.; Raees, I.; Salman, M.; Merchant, H.A.; Aldeyab, M.A.; Kow, C.S.; Hasan, S.S. COVID-19 Vaccine Hesitancy among Pregnant Women Attending Antenatal Clinics in Pakistan: A Multicentric, Prospective, Survey-Based Study. Viruses 2022, 14, 2344. [Google Scholar] [CrossRef]
- Hayat, K.; Mustafa, Z.U.; Godman, B.; Arshed, M.; Zhang, J.; Khan, F.U.; Saleem, F.; Lambojon, K.; Li, P.; Feng, Z.; et al. Perceptions, Expectations, and Experience of Physicians About Pharmacists and Pharmaceutical Care Services in Pakistan: Findings and Implications. Front. Pharmacol. 2021, 12, 650137. [Google Scholar] [CrossRef]
- Mudenda, S.; Mukosha, M.; Godman, B.; Fadare, J.; Malama, S.; Munyeme, M.; Hikaambo, C.N.; Kalungia, A.C.; Hamachila, A.; Kainga, H.; et al. Knowledge, Attitudes, and Practices of Community Pharmacy Professionals on Poultry Antibiotic Dispensing, Use, and Bacterial Antimicrobial Resistance in Zambia: Implications on Antibiotic Stewardship and WHO AWaRe Classification of Antibiotics. Antibiotics 2022, 11, 1210. [Google Scholar] [CrossRef]
- Guma, S.P.; Godman, B.; Campbell, S.M.; Mahomed, O. Determinants of the Empiric Use of Antibiotics by General Practitioners in South Africa: Observational, Analytic, Cross-Sectional Study. Antibiotics 2022, 11, 1423. [Google Scholar] [CrossRef] [PubMed]
- Jairoun, A.A.; Al-Hemyari, S.S.; Shahwan, M.; Saeed, B.Q.; Godman, B.; Kurdi, A.; Zyoud, S.H.; Ibrahim, B. Risk Awareness and Demographic Characteristics Associated With the Use of Sexual Enhancement Supplements Among University Staff: A Cross-Sectional Study in the United Arab Emirates. Am. J. Men’s Health 2023, 17, 15579883231158531. [Google Scholar] [CrossRef] [PubMed]
- Mustafa, Z.U.; Nazir, M.; Majeed, H.K.; Salman, M.; Hayat, K.; Khan, A.H.; Meyer, J.C.; Godman, B. Exploring Knowledge of Antibiotic Use, Resistance, and Stewardship Programs among Pharmacy Technicians Serving in Ambulatory Care Settings in Pakistan and the Implications. Antibiotics 2022, 11, 921. [Google Scholar] [CrossRef] [PubMed]
- Raosoft Inc. 2004. Available online: http://www.raosoft.com/samplesize.html (accessed on 1 June 2020).
- Wang, P.-W.; Ahorsu, D.K.; Lin, C.-Y.; Chen, I.-H.; Yen, C.-F.; Kuo, Y.-J.; Griffiths, M.D.; Pakpour, A.H. Motivation to Have COVID-19 Vaccination Explained Using an Extended Protection Motivation Theory among University Students in China: The Role of Information Sources. Vaccines 2021, 9, 380. [Google Scholar] [CrossRef] [PubMed]
- Larson, H.J.; Sahinovic, I.; Balakrishnan, M.R.; Simas, C. Vaccine safety in the next decade: Why we need new modes of trust building. BMJ Glob. Health 2021, 6 (Suppl. S2), e003908. [Google Scholar] [CrossRef]
- Lazarus, J.V.; Wyka, K.; White, T.M.; Picchio, C.A.; Rabin, K.; Ratzan, S.C.; Leigh, J.P.; Hu, J.; El-Mohandes, A. Revisiting COVID-19 vaccine hesitancy around the world using data from 23 countries in 2021. Nat. Commun. 2022, 13, 3801. [Google Scholar] [CrossRef]
- Lazarus, J.V.; Romero, D.; Kopka, C.J.; Karim, S.A.; Abu-Raddad, L.J.; Almeida, G.; Baptista-Leite, R.; Barocas, J.A.; Barreto, M.L.; Bar-Yam, Y.; et al. A multinational Delphi consensus to end the COVID-19 public health threat. Nature 2022, 611, 332–345. [Google Scholar] [CrossRef]
- Marzo, R.R.; Sami, W.; Alam, Z.; Acharya, S.; Jermsittiparsert, K.; Songwathana, K.; Pham, N.T.; Respati, T.; Faller, E.M.; Baldonado, A.M.; et al. Hesitancy in COVID-19 vaccine uptake and its associated factors among the general adult population: A cross-sectional study in six Southeast Asian countries. Trop. Med. Health 2022, 50, 4. [Google Scholar] [CrossRef]
- Wonodi, C.; Obi-Jeff, C.; Adewumi, F.; Keluo-Udeke, S.C.; Gur-Arie, R.; Krubiner, C.; Jaffe, E.F.; Bamiduro, T.; Karron, R.; Faden, R. Conspiracy theories and misinformation about COVID-19 in Nigeria: Implications for vaccine demand generation communications. Vaccine 2022, 40, 2114–2121. [Google Scholar] [CrossRef]
- Katoto, P.D.M.C.; Parker, S.; Coulson, N.; Pillay, N.; Cooper, S.; Jaca, A.; Mavundza, E.; Houston, G.; Groenewald, C.; Essack, Z.; et al. Predictors of COVID-19 Vaccine Hesitancy in South African Local Communities: The VaxScenes Study. Vaccines 2022, 10, 353. [Google Scholar] [CrossRef]
- Bhandari, S. Reasons for COVID-19 vaccination hesitancy in hemodialysis patients. Kidney Int. 2021, 100, 702. [Google Scholar] [CrossRef] [PubMed]
- Syed Alwi, S.A.; Rafidah, E.; Zurraini, A.; Juslina, O.; Brohi, I.B.; Lukas, S. A survey on COVID-19 vaccine acceptance and concern among Malaysians. BMC Public Health 2021, 21, 1129. [Google Scholar] [CrossRef] [PubMed]
- Rotolo, B.; Dubé, E.; Vivion, M.; MacDonald, S.E.; Meyer, S.B. Hesitancy towards COVID-19 vaccines on social media in Canada. Vaccine 2022, 40, 2790–2796. [Google Scholar] [CrossRef] [PubMed]
- Islam, S.; Kamal, A.-H.M.; Kabir, A.; Southern, D.L.; Khan, S.H.; Hasan, S.M.M.; Sarkar, T.; Sharmin, S.; Das, S.; Roy, T.; et al. COVID-19 vaccine rumors and conspiracy theories: The need for cognitive inoculation against misinformation to improve vaccine adherence. PLoS ONE 2021, 16, e0251605. [Google Scholar] [CrossRef]
- Tsai, R.; Hervey, J.; Hoffman, K.; Wood, J.; Johnson, J.; Deighton, D.; Clermont, D.; Loew, B.; Goldberg, S.L. COVID-19 Vaccine Hesitancy and Acceptance Among Individuals With Cancer, Autoimmune Diseases, or Other Serious Comorbid Conditions: Cross-sectional, Internet-Based Survey. JMIR Public Health Surveill. 2022, 8, e29872. [Google Scholar] [CrossRef]
- Ehde, D.M.; Roberts, M.K.; Humbert, A.T.; Herring, T.E.; Alschuler, K.N. COVID-19 vaccine hesitancy in adults with multiple sclerosis in the United States: A follow up survey during the initial vaccine rollout in 2021. Mult. Scler. Relat. Disord. 2021, 54, 103163. [Google Scholar] [CrossRef]
- Tuckerman, J.M.; Kaufman, J.; Danchin, M.M. Effective Approaches to Combat Vaccine Hesitancy. Pediatr. Infect. Dis. J. 2022, 41, e243–e245. [Google Scholar] [CrossRef]
- Jose, S.; Cyriac, M.C.; Dhandapani, M.; Joseph, J. COVID-19 vaccination intention and hesitancy: Mistrust on COVID-19 vaccine benefit a major driver for vaccine hesitancy among healthcare workers; a cross-sectional study in North India. J. Prev. Med. Hyg. 2022, 63, E219–E230. [Google Scholar]
- Peters, M.D. Addressing vaccine hesitancy and resistance for COVID-19 vaccines. Int. J. Nurs. Stud. 2022, 131, 104241. [Google Scholar] [CrossRef]
- Muric, G.; Wu, Y.; Ferrara, E. COVID-19 Vaccine Hesitancy on Social Media: Building a Public Twitter Data Set of Antivaccine Content, Vaccine Misinformation, and Conspiracies. JMIR Public Health Surveill. 2021, 7, e30642. [Google Scholar] [CrossRef]
- Ngai, C.S.B.; Singh, R.G.; Yao, L. Impact of COVID-19 Vaccine Misinformation on Social Media Virality: Content Analysis of Message Themes and Writing Strategies. J. Med. Internet Res. 2022, 24, e37806. [Google Scholar] [CrossRef] [PubMed]
- Greyling, T.; Rossouw, S. Positive attitudes towards COVID-19 vaccines: A cross-country analysis. PLoS ONE 2022, 17, e0264994. [Google Scholar] [CrossRef] [PubMed]
- Vilar-Lluch, S.; McClaughlin, E.; Knight, D.; Adolphs, S.; Nichele, E. The language of vaccination campaigns during COVID-19. Med. Humanit. 2023. [Google Scholar] [CrossRef] [PubMed]
- Weeks, R.; Cooper, L.; Sangha, P.; Sedoc, J.; White, S.; Toledo, A.; Gretz, S.; Lahav, D.; Martin, N.; Michel, A.; et al. Chatbot-Delivered COVID-19 Vaccine Communication Message Preferences of Young Adults and Public Health Workers in Urban American Communities: Qualitative Study. J. Med. Internet Res. 2022, 24, e38418. [Google Scholar] [CrossRef]
- Singh, P.; Dhalaria, P.; Kashyap, S.; Soni, G.K.; Nandi, P.; Ghosh, S.; Mohapatra, M.K.; Rastogi, A.; Prakash, D. Strategies to overcome vaccine hesitancy: A systematic review. Syst. Rev. 2022, 11, 78. [Google Scholar] [CrossRef]
- Capalbo, C.; Aceti, A.; Simmaco, M.; Bonfini, R.; Rocco, M.; Ricci, A.; Napoli, C.; Rocco, M.; Alfonsi, V.; Teggi, A.; et al. The Exponential Phase of the COVID-19 Pandemic in Central Italy: An Integrated Care Pathway. Int. J. Environ. Res. Public Health 2020, 17, 3792. [Google Scholar] [CrossRef]


| Variable | Sub-Groups | N (%) | p-Value | ||
|---|---|---|---|---|---|
| Overall (n = 399) | Vaccinated (n = 249) | Unvaccinated (n = 150) | |||
| Age (years) | 18–44 | 57 (14.3) | 32 (12.9) | 25 (16.7) | 0.563 |
| 45–64 | 202 (50.6) | 129 (51.8) | 73 (48.7) | ||
| ≥65 | 140 (35.1) | 88 (35.3) | 52 (34.7) | ||
| Gender | Male | 225 (56.4) | 138 (55.4) | 87 (58.0) | 0.677 * |
| Female | 174 (43.6) | 111 (44.6) | 63 (42.0) | ||
| Residence | Urban | 151 (37.8) | 94 (37.8) | 57 (38.0) | 1.000 |
| Rural | 248 (62.2) | 155 (62.2) | 93 (62.0) | ||
| Marital status | Single | 111 (27.8) | 61 (24.5) | 50 (33.3) | 0.065 |
| Married | 288 (72.2) | 188 (75.5) | 100 (66.7) | ||
| Occupation | Employed | 82 (20.6) | 55 (22.1) | 27 (18.0) | 0.501 |
| Unemployed | 258 (64.7) | 159 (63.9) | 99 (66.0) | ||
| Retired | 42 (10.5) | 23 (9.2) | 19 (12.7) | ||
| Cannot work due to disability | 17 (4.3) | 12 (4.8) | 5 (3.3) | ||
| Family income (PKR) | <30,000 | 182 (45.6) | 108 (43.4) | 74 (49.3) | 0.498 |
| 31,000–60,000 | 129 (32.3) | 83 (33.3) | 46 (30.7) | ||
| >60,000 | 88 (22.1) | 58 (23.3) | 30 (20.0) | ||
| Education | Illiterate | 104 (26.1) | 63 (25.3) | 41 (27.3) | 0.290 |
| Religious education only | 33 (8.3) | 24 (9.6) | 9 (6.0) | ||
| Primary | 88 (22.1) | 55 (22.1) | 33 (22.0) | ||
| Secondary | 105 (26.3) | 65 (26.1) | 40 (26.7) | ||
| High secondary | 46 (11.5) | 24 (9.6) | 22 (14.7) | ||
| Diploma/Bachelor/Master | 23 (5.8) | 18 (7.2) | 5 (3.3) | ||
| Smoking status | Current smoker | 79 (19.8) | 51 (20.5) | 28 (18.7) | 0.907 |
| Non-smoker | 233 (58.4) | 144 (57.8) | 89 (59.3) | ||
| Former smoker | 87 (21.8) | 54 (21.7) | 33 (22.0) | ||
| Years on hemodialysis | <1 | 59 (14.8) | 37 (14.9) | 22 (14.7) | 0.915 |
| >1 to 3 | 181 (45.4) | 111 (44.6) | 70 (46.7) | ||
| >3 | 159 (39.8) | 101 (40.6) | 58 (38.7) | ||
| Frequency of hemodialysis | Once a week | 8 (2.0) | 4 (1.6) | 4 (2.7) | 0.539 |
| Two times a week | 310 (77.7) | 191 (76.7) | 119 (79.3) | ||
| Three times a week | 81 (20.3) | 54 (21.7) | 27 (18.0) | ||
| Influenza vaccine | Vaccinated | 89 (22.3) | 57 (22.9) | 32 (21.3) | 0.804 * |
| Not vaccinated | 310 (77.7) | 192 (77.1) | 118 (78.7) | ||
| Hepatitis B vaccine | Vaccinated | 293 (73.4) | 184 (73.9) | 109 (72.7) | 0.815 * |
| Not vaccinated | 106 (26.6) | 65 (26.1) | 41 (27.3) | ||
| Hepatitis C | Positive | 106 (26.6) | 64 (25.7) | 42 (28.0) | 0.641 * |
| Negative | 293 (73.4) | 185 (74.3) | 108 (72.0) | ||
| Family member or relative infected with COVID-19 | Yes | 162 (40.6) | 106 (42.6) | 56 (37.7) | 0.344 * |
| No | 237 (59.4) | 143 (57.4) | 94 (62.7) | ||
| Family member or relative died due to COVID-19 | Yes | 22 (5.5) | 15 (6.0) | 7 (4.7) | 0.655 * |
| No | 377 (94.5) | 234 (94.0) | 143 (95.3) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Amjad, Z.; Maryam, I.; Munir, M.; Salman, M.; Baraka, M.A.; Mustafa, Z.U.; Khan, Y.H.; Mallhi, T.H.; Hasan, S.S.; Meyer, J.C.; et al. COVID-19 Vaccines Status, Acceptance and Hesitancy among Maintenance Hemodialysis Patients: A Cross-Sectional Study and the Implications for Pakistan and Beyond. Vaccines 2023, 11, 904. https://doi.org/10.3390/vaccines11050904
Amjad Z, Maryam I, Munir M, Salman M, Baraka MA, Mustafa ZU, Khan YH, Mallhi TH, Hasan SS, Meyer JC, et al. COVID-19 Vaccines Status, Acceptance and Hesitancy among Maintenance Hemodialysis Patients: A Cross-Sectional Study and the Implications for Pakistan and Beyond. Vaccines. 2023; 11(5):904. https://doi.org/10.3390/vaccines11050904
Chicago/Turabian StyleAmjad, Zara, Iqra Maryam, Maria Munir, Muhammad Salman, Mohamed A. Baraka, Zia Ul Mustafa, Yusra Habib Khan, Tauqeer Hussain Mallhi, Syed Shahzad Hasan, Johanna C. Meyer, and et al. 2023. "COVID-19 Vaccines Status, Acceptance and Hesitancy among Maintenance Hemodialysis Patients: A Cross-Sectional Study and the Implications for Pakistan and Beyond" Vaccines 11, no. 5: 904. https://doi.org/10.3390/vaccines11050904
APA StyleAmjad, Z., Maryam, I., Munir, M., Salman, M., Baraka, M. A., Mustafa, Z. U., Khan, Y. H., Mallhi, T. H., Hasan, S. S., Meyer, J. C., & Godman, B. (2023). COVID-19 Vaccines Status, Acceptance and Hesitancy among Maintenance Hemodialysis Patients: A Cross-Sectional Study and the Implications for Pakistan and Beyond. Vaccines, 11(5), 904. https://doi.org/10.3390/vaccines11050904













