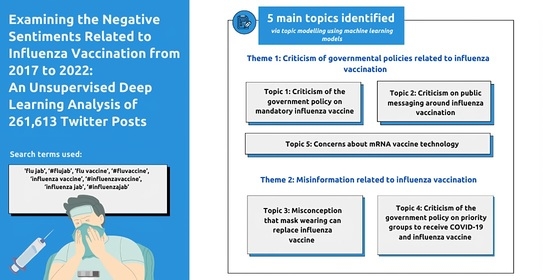
Examining the Negative Sentiments Related to Influenza Vaccination from 2017 to 2022: An Unsupervised Deep Learning Analysis of 261,613 Twitter Posts
Abstract
:1. Introduction
2. Methods
3. Results
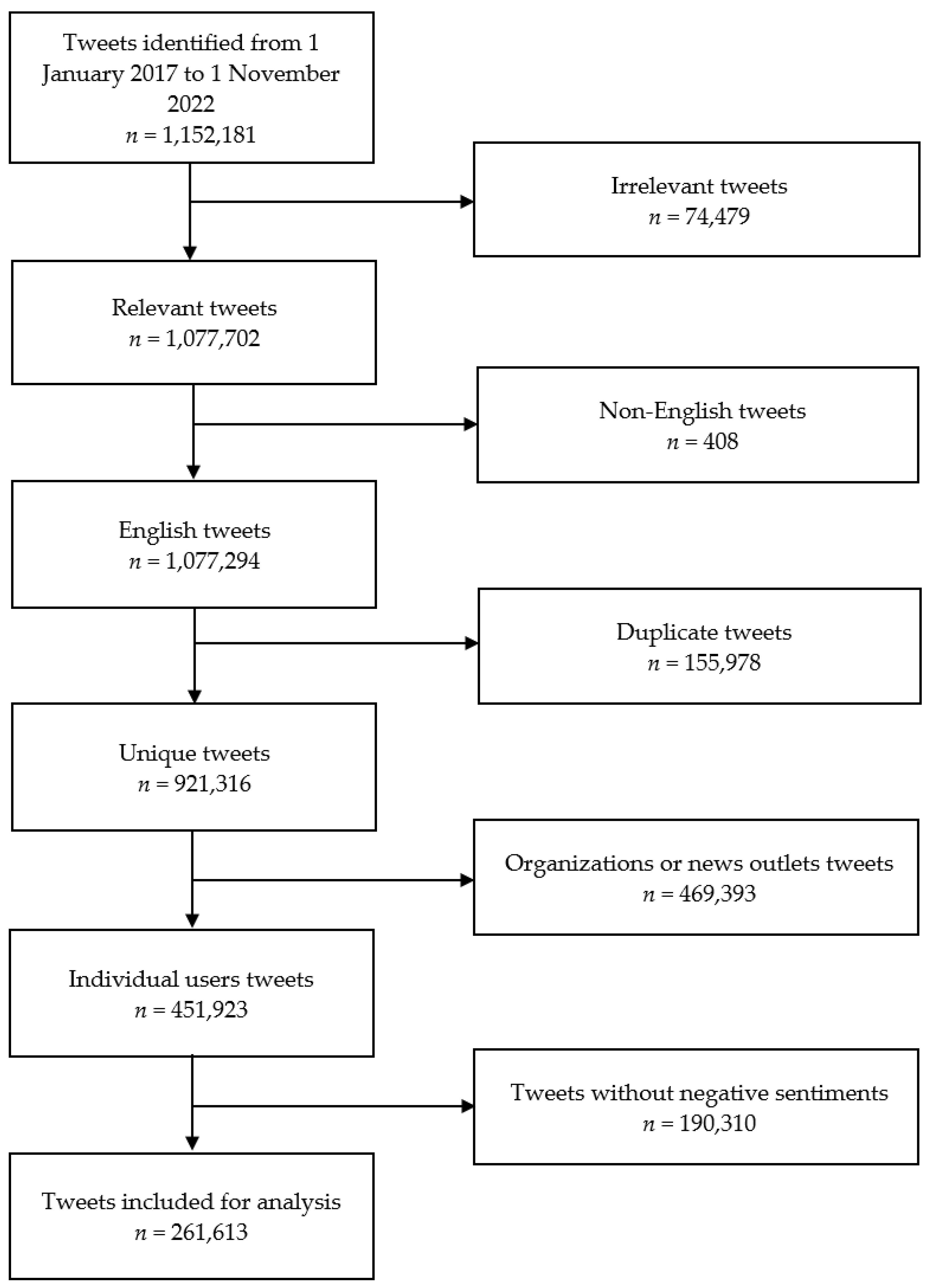
3.1. Search Results
3.2. Topic Modelling
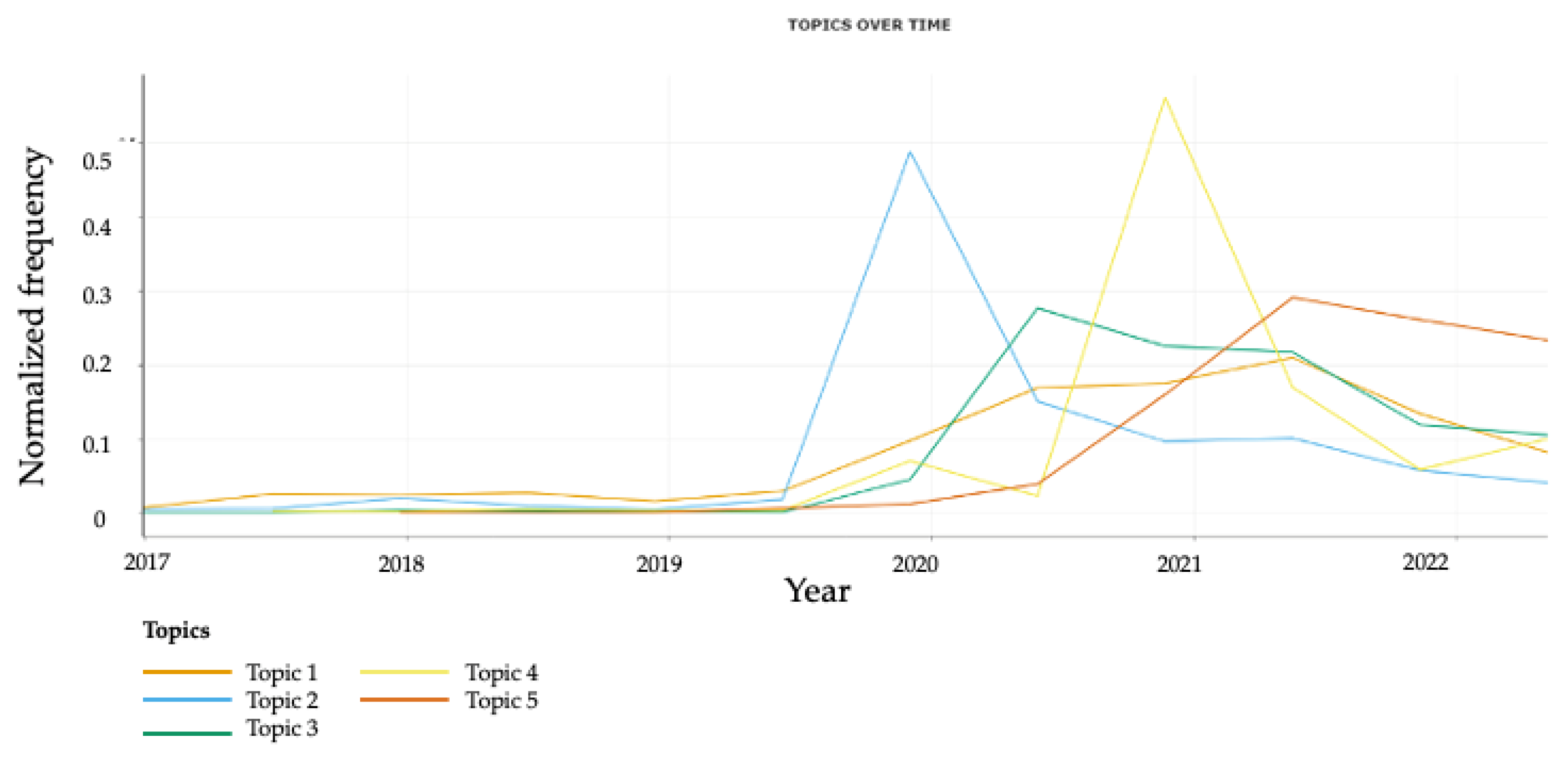
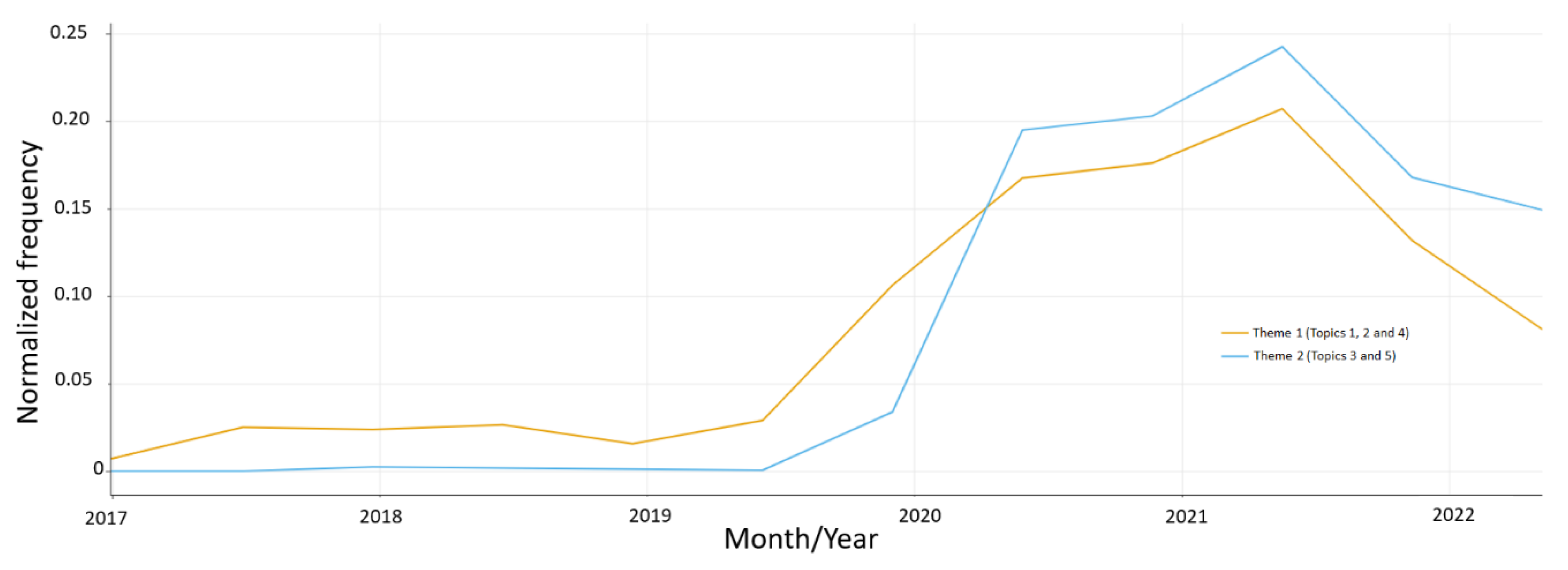
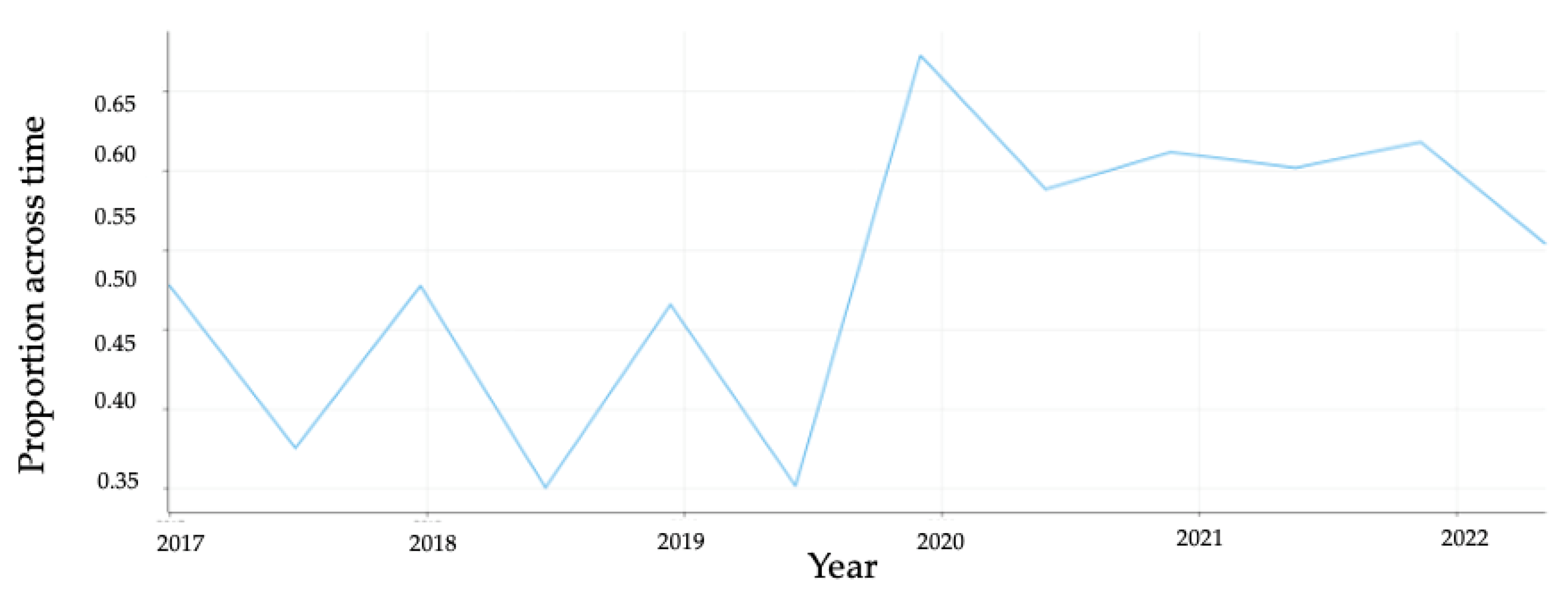
3.3. Analysis of Temporal Trends
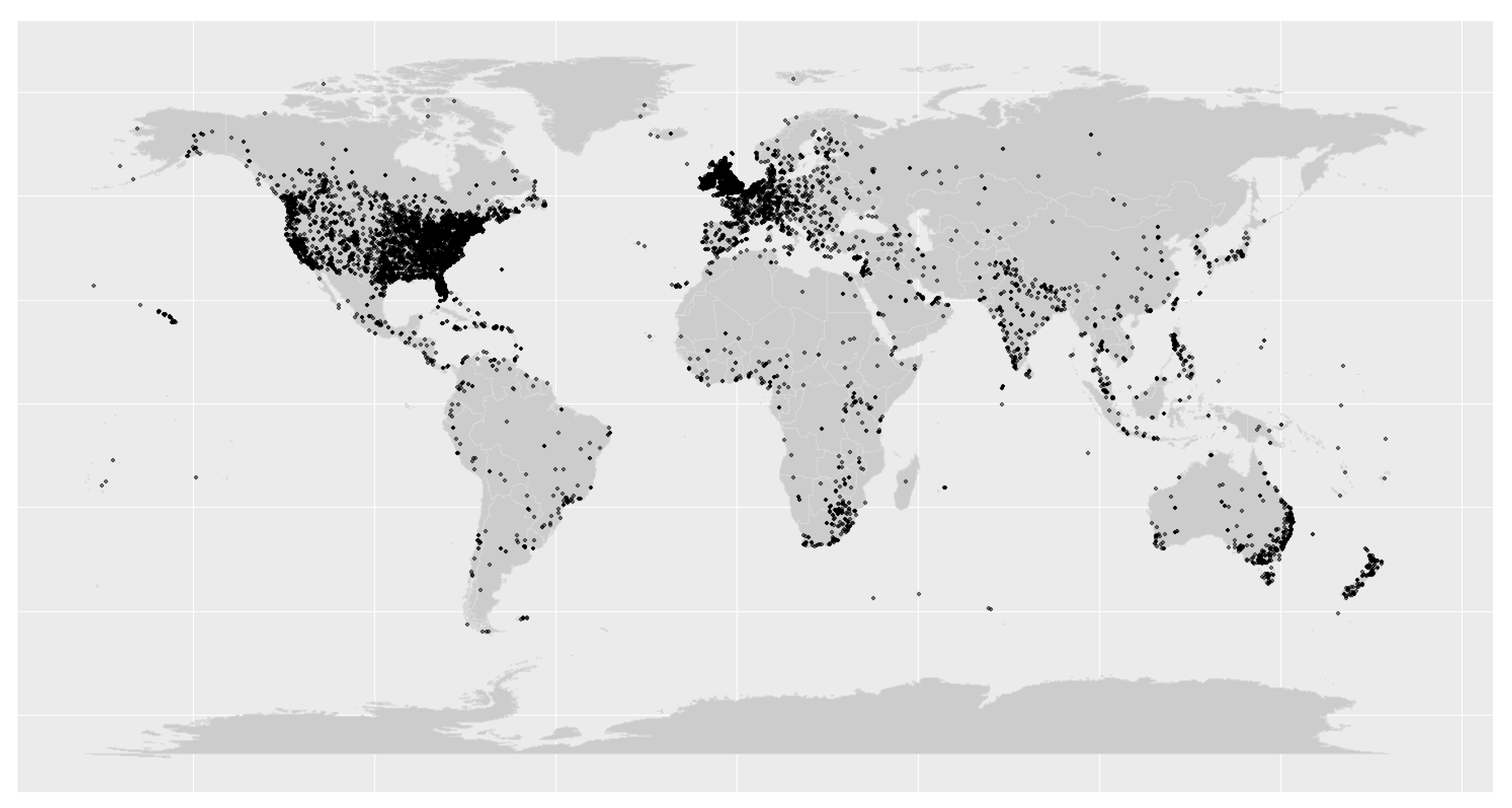
3.4. Analysis of Geolocational Data
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nicoll, A.; Ciancio, B.C.; Lopez Chavarrias, V.; Mølbak, K.; Pebody, R.; Pedzinski, B.; Penttinen, P.; van der Sande, M.; Snacken, R.; Van Kerkhove, M.D. Influenza-related deaths—Available methods for estimating numbers and detecting patterns for seasonal and pandemic influenza in Europe. Eurosurveillance 2012, 17, 20162. [Google Scholar] [CrossRef] [PubMed]
- Nunes, B.; Viboud, C.; Machado, A.; Ringholz, C.; Rebelo-de-Andrade, H.; Nogueira, P.; Miller, M. Excess mortality associated with influenza epidemics in Portugal, 1980 to 2004. PLoS ONE 2011, 6, e20661. [Google Scholar] [CrossRef] [PubMed]
- Putri, W.; Muscatello, D.J.; Stockwell, M.S.; Newall, A.T. Economic burden of seasonal influenza in the United States. Vaccine 2018, 36, 3960–3966. [Google Scholar] [CrossRef] [PubMed]
- Nichols, M.K.; Andrew, M.K.; Hatchette, T.F.; Ambrose, A.; Boivin, G.; Bowie, W.; Chit, A.; Dos Santos, G.; ElSherif, M.; Green, K.; et al. Influenza vaccine effectiveness to prevent influenza-related hospitalizations and serious outcomes in Canadian adults over the 2011/12 through 2013/14 influenza seasons: A pooled analysis from the Canadian Immunization Research Network (CIRN) Serious Outcomes Surveillance (SOS Network). Vaccine 2018, 36, 2166–2175. [Google Scholar] [CrossRef] [PubMed]
- Mohd Nordin, N.R.; Arsad, F.S.; Megat Kamaruddin, P.S.N.; Hilmi, M.; Madrim, M.F.; Hassan, M.R.; Syed Abdul Rahim, S.S.; Jeffree, M.S.; Ramdzan, A.R.; Atil, A.; et al. Impact of social distancing on COVID-19 and other related infectious disease transmission: A systematic review. Open Access Maced. J. Med. Sci. 2021, 9, 601–607. [Google Scholar] [CrossRef]
- Ali, S.; Lau, Y.; Shan, S.; Ryu, S.; Du, Z.; Wang, L.; Xu, X.-K.; Chen, D.; Xiong, J.; Tae, J.; et al. Prediction of upcoming global infection burden of influenza seasons after relaxation of public health and social measures during the COVID-19 pandemic: A modelling study. Lancet Glob. Health 2022, 10, e1612–e1622. [Google Scholar] [CrossRef]
- Hambidge, S.J.; Glanz, J.M.; France, E.K.; McClure, D.; Xu, S.; Yamasaki, K.; Jackson, L.; Mullooly, J.P.; Zangwill, K.M.; Marcy, S.M.; et al. Safety of trivalent inactivated influenza vaccine in children 6 to 23 months old. JAMA 2006, 296, 1990–1997. [Google Scholar] [CrossRef]
- Woo, E.J.; Moro, P.L. Postmarketing safety surveillance of quadrivalent recombinant influenza vaccine: Reports to the vaccine adverse event reporting system. Vaccine 2021, 39, 1812–1817. [Google Scholar] [CrossRef]
- Fan, J.; Cong, S.; Wang, N.; Bao, H.; Wang, B.; Feng, Y.; Lv, X.; Zhang, Y.; Zha, Z.; Yu, L.; et al. Influenza vaccination rate and its association with chronic diseases in China: Results of a national cross-sectional study. Vaccine 2020, 38, 2503–2511. [Google Scholar] [CrossRef]
- Wang, Q.; Yue, N.; Zheng, M.; Wang, D.; Duan, C.; Yu, X.; Zhang, X.; Bao, C.; Jin, H. Influenza vaccination coverage of population and the factors influencing influenza vaccination in mainland China: A meta-analysis. Vaccine 2018, 36, 7262–7269. [Google Scholar] [CrossRef]
- Lee, H.; Choi, H.; Jo, Y.S. Trends in influenza vaccination rates in participants with airflow limitation: The Korea National Health and Nutrition Examination Survey 2007–2018. Front. Med. 2022, 9, 870617. [Google Scholar] [CrossRef] [PubMed]
- Alotaibi, F.Y.; Alhetheel, A.F.; Alluhaymid, Y.M.; Alshibani, M.G.; Almuhaydili, A.O.; Alhuqayl, T.A.; Alfayez, F.M.; Almasabi, A.A. Influenza vaccine coverage, awareness, and beliefs regarding seasonal influenza vaccination among people aged 65 years and older in Central Saudi Arabia. Saudi Med. J. 2019, 40, 1013–1018. [Google Scholar] [CrossRef] [PubMed]
- Alshahrani, S.M.; Zahrani, Y. Prevalence and predictors of seasonal influenza vaccine uptake in Saudi Arabia post COVID-19: A web-based online cross-sectional study. Vaccines 2023, 11, 353. [Google Scholar] [CrossRef] [PubMed]
- Flu Vaccination Coverage, United States, 2021–2022 Influenza Season. Available online: https://www.cdc.gov/flu/fluvaxview/coverage-2022estimates.htm (accessed on 27 March 2023).
- Ng, Q.X.; Lim, S.R.; Yau, C.E.; Liew, T.M. Examining the prevailing negative sentiments related to COVID-19 vaccination: Unsupervised deep learning of Twitter posts over a 16 month period. Vaccines 2022, 10, 1457. [Google Scholar] [CrossRef]
- Qunaibi, E.A.; Helmy, M.; Basheti, I.; Sultan, I. A high rate of COVID-19 vaccine hesitancy in a large-scale survey on Arabs. eLife 2021, 10, e68038. [Google Scholar] [CrossRef]
- Larson, H.J.; Gakidou, E.; Murray, C.J.L. The vaccine-hesitant moment. N. Engl. J. Med. 2022, 387, 58–65. [Google Scholar] [CrossRef]
- Yang, K.-C.; Pierri, F.; Hui, P.-M.; Axelrod, D.; Torres-Lugo, C.; Bryden, J.; Menczer, F. The COVID-19 infodemic: Twitter versus Facebook. Big Data Soc. 2021, 8, 20539517211013861. [Google Scholar] [CrossRef]
- Pierri, F.; Perry, B.L.; DeVerna, M.R.; Yang, K.-C.; Flammini, A.; Menczer, F.; Bryden, J. Online misinformation is linked to early COVID-19 vaccination hesitancy and refusal. Sci. Rep. 2022, 12, 5966. [Google Scholar] [CrossRef]
- Cervi, L.; García, F.; Marín-Lladó, C. Populism, Twitter, and COVID-19: Narrative, fantasies, and desires. Soc. Sci. 2021, 10, 294. [Google Scholar] [CrossRef]
- Rufai, S.R.; Bunce, C. World leaders’ usage of Twitter in response to the COVID-19 pandemic: A content analysis. J. Public Health 2020, 42, 510–516. [Google Scholar] [CrossRef]
- Twitter: Number of Monetizable Daily Active Users Worldwide 2017–2022. Available online: https://www.globaldata.com/data-insights/technology--media-and-telecom/twitter-monetizable-daily-active-users/#:~:text=Monetizable%20Daily%20Active%20Users%20of,2017%20%2D%20Q4%202021%2C%20Million)&text=Twitter%2C%20the%20microblogging%20platform%2C%20reported,the%20same%20period%20last%20year (accessed on 2 May 2023).
- Ahmed, W.; Bath, P.A.; Sbaffi, L.; Demartini, G. Novel insights into views towards H1N1 during the 2009 Pandemic: A thematic analysis of Twitter data. Health Inf. Libr. J. 2019, 36, 60–72. [Google Scholar] [CrossRef] [PubMed]
- Tang, L.; Bie, B.; Park, S.-E.; Zhi, D. Social media and outbreaks of emerging infectious diseases: A systematic review of literature. Am. J. Infect. Control 2018, 46, 962–972. [Google Scholar] [CrossRef] [PubMed]
- Bari, A.; Heymann, M.; Cohen, R.J.; Zhao, R.; Szabo, L.; Apas Vasandani, S.; Khubchandani, A.; DiLorenzo, M.; Coffee, M. Exploring Coronavirus Disease 2019 vaccine hesitancy on Twitter using sentiment analysis and natural language processing algorithms. Clin. Infect. Dis. 2022, 74, e4–e9. [Google Scholar] [CrossRef] [PubMed]
- Gerts, D.; Shelley, C.D.; Parikh, N.; Pitts, T.; Watson Ross, C.; Fairchild, G.; Vaquera Chavez, N.Y.; Daughton, A.R. “Thought I’d share first” and other conspiracy theory tweets from the COVID-19 infodemic: Exploratory study. JMIR Public Health Surveill. 2021, 7, e26527. [Google Scholar] [CrossRef]
- Damstra, A.; Boomgaarden, H.G.; Broda, E.; Lindgren, E.; Strömbäck, J.; Tsfati, Y.; Vliegenthart, R. What does fake look like? A review of the literature on intentional deception in the news and on social media. J. Stud. 2021, 22, 1947–1963. [Google Scholar] [CrossRef]
- Jamison, A.M.; Broniatowski, D.A.; Dredze, M.; Sangraula, A.; Smith, M.C.; Quinn, S.C. Not just conspiracy theories: Vaccine opponents and proponents add to the COVID-19 infodemic’ on Twitter. Harv. Kennedy Sch. Misinformation Rev. 2020, 1. [Google Scholar] [CrossRef]
- Nehal, K.R.; Steendam, L.M.; Campos Ponce, M.; van der Hoeven, M.; Smit, G.S.A. Worldwide vaccination willingness for COVID-19: A systematic review and meta-analysis. Vaccines 2021, 9, 1071. [Google Scholar] [CrossRef]
- Jang, H.; Rempel, E.; Roth, D.; Carenini, G.; Janjua, N.Z. Tracking COVID-19 Discourse on Twitter in North America: Infodemiology study using topic modeling and aspect-based sentiment analysis. J. Med. Internet Res. 2021, 23, e25431. [Google Scholar] [CrossRef]
- Devlin, J.; Chang, M.-W.; Lee, K.; Toutanova, K. BERT: Pre-training of Deep Bidirectional Transformers for Language Understanding. arXiv 2019, arXiv:1810.04805. [Google Scholar]
- Huggingface.co. Available online: https://huggingface.co/dslim/bert-base-NER (accessed on 8 November 2022).
- Hartmann, J.; Heitmann, M.; Siebert, C.; Schamp, C. More than a feeling: Accuracy and application of sentiment analysis. Int. J. Res. Mark. 2023, 40, 75–87. [Google Scholar] [CrossRef]
- Schöne, J.P.; Parkinson, B.; Goldenberg, A. Negativity spreads more than positivity on Twitter after both positive and negative political situations. Affect. Sci. 2021, 2, 379–390. [Google Scholar] [CrossRef] [PubMed]
- Grootendorst, M.R. BERTopic: Neural topic modeling with a class-based TF-IDF procedure. arXiv 2022, arXiv:2203.05794. [Google Scholar]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Leuchter, R.K.; Jackson, N.J.; Mafi, J.N.; Sarkisian, C.A. Association between COVID-19 vaccination and influenza Vaccination rates. N. Engl. J. Med. 2022, 386, 2531–2532. [Google Scholar] [CrossRef] [PubMed]
- Zhang, V.; Zhu, P.; Wagner, A.L. Spillover of vaccine hesitancy into adult COVID-19 and influenza: The role of race, religion, and political affiliation in the United States. Int. J. Environ. Res. Public Health 2023, 20, 3376. [Google Scholar] [CrossRef]
- Bruine de Bruin, W.; Carman, K.G.; Parker, A.M. Mental associations with COVID-19 and how they relate with self-reported protective behaviors: A national survey in the United States. Soc. Sci. Med. 2021, 275, 113825. [Google Scholar] [CrossRef]
- Larsen, J.R.; Martin, M.R.; Martin, J.D.; Kuhn, P.; Hicks, J.B. Modeling the onset of symptoms of COVID-19. Front. Public Health 2020, 8, 473. [Google Scholar] [CrossRef]
- Katsiroumpa, A.; Sourtzi, P.; Kaitelidou, D.; Siskou, O.; Konstantakopoulou, O.; Galanis, P. Predictors of seasonal influenza vaccination willingness among high-risk populations three years after the onset of the COVID-19 pandemic. Vaccines 2023, 11, 331. [Google Scholar] [CrossRef]
- Parker, A.M.; Atshan, S.; Walsh, M.M.; Gidengil, C.A.; Vardavas, R. Association of COVID-19 vaccination with influenza vaccine history and changes in influenza vaccination. JAMA Netw. Open 2022, 5, e2241888. [Google Scholar] [CrossRef]
- Chan, M.S.; Jones, C.R.; Hall Jamieson, K.; Albarracín, D. Debunking: A meta-analysis of the psychological efficacy of messages countering misinformation. Psychol. Sci. 2017, 28, 1531–1546. [Google Scholar] [CrossRef]
- Walter, N.; Tukachinsky, R. A meta-analytic examination of the continued influence of misinformation in the face of correction: How powerful is it, why does it happen, and how to stop it? Commun. Res. 2019, 47, 155–177. [Google Scholar] [CrossRef]
- Vraga, E.K.; Bode, L. I do not believe you: How providing a source corrects health misperceptions across social media platforms. Inf. Commun. Soc. 2018, 21, 1337–1353. [Google Scholar] [CrossRef]
- Hagen, L.; Fox, A.; O’Leary, H.; Dyson, D.; Walker, K.; Lengacher, C.A.; Hernandez, R. The role of influential actors in fostering the polarized COVID-19 vaccine discourse on Twitter: Mixed methods of machine learning and inductive coding. JMIR Infodemiol. 2022, 2, e34231. [Google Scholar] [CrossRef]
- Zollo, F.; Bessi, A.; Del Vicario, M.; Scala, A.; Caldarelli, G.; Shekhtman, L.; Havlin, S.; Quattrociocchi, W. Debunking in a world of tribes. PLoS ONE 2017, 12, e0181821. [Google Scholar] [CrossRef]
- Bertolotti, M.; Catellani, P. Counterfactual thinking as a prebunking strategy to contrast misinformation on COVID-19. J. Exp. Soc. Psychol. 2023, 104, 104404. [Google Scholar] [CrossRef]
- Bode, L.; Vraga, E.K. See something, say something: Correction of global health misinformation on social media. Health Commun. 2018, 33, 1131–1140. [Google Scholar] [CrossRef] [PubMed]
- Fernández-García, B.; Salgado, S. Discourses about fake news, conspiracies and counterknowledge in Spain. West. J. Commun. 2022, 86, 561–580. [Google Scholar] [CrossRef]
- Lewandowsky, S.; Ecker, U.K.H.; Cook, J. Beyond misinformation: Understanding and coping with the “post-truth” era. J. Appl. Res. Mem. Cogn. 2017, 6, 353–369. [Google Scholar] [CrossRef]
- Roozenbeek, J.; van der Linden, S.; Goldberg, B.; Rathje, S.; Lewandowsky, S. Psychological inoculation improves resilience against misinformation on social media. Sci. Adv. 2022, 8, eabo6254. [Google Scholar] [CrossRef]
- Van der Linden, S.; Roozenbeek, J.; Compton, J. Inoculating against fake news about COVID-19. Front. Psychol. 2020, 11, 566790. [Google Scholar] [CrossRef]
- Dwoskin, E.T.; Timberg, C. Misinformation Dropped Dramatically the Week after Twitter Banned Trump and Some Allies. Available online: https://www.washingtonpost.com/technology/2021/01/16/misinformation-trump-twitter/ (accessed on 5 May 2023).
- Singh, K. Many Places Drop COVID-19 Mask Mandates but Issue Recommendations. Available online: https://str.sg/wRdK (accessed on 7 May 2023).
- Schmid, P.; Rauber, D.; Betsch, C.; Lidolt, G.; Denker, M.-L. Barriers of influenza vaccination intention and behavior—A Systematic Review of Influenza Vaccine Hesitancy, 2005–2016. PLoS ONE 2017, 12, e0170550. [Google Scholar] [CrossRef] [PubMed]
- Nyhan, B.; Reifler, J. Does correcting myths about the flu vaccine work? An experimental evaluation of the effects of corrective information. Vaccine 2015, 33, 459–464. [Google Scholar] [CrossRef] [PubMed]
- Grohskopf, L.A.; Alyanak, E.; Ferdinands, J.M.; Broder, K.R.; Blanton, L.H.; Talbot, H.K.; Fry, A.M. Prevention and control of seasonal influenza with vaccines: Recommendations of the advisory committee on immunization practices, United States, 2021–2022 Influenza Season. MMWR Recomm. Rep. 2021, 70, 1–28. [Google Scholar] [CrossRef] [PubMed]
- Paget, J.; Spreeuwenberg, P.; Charu, V.; Taylor, R.J.; Iuliano, A.D.; Bresee, J.; Simonsen, L.; Viboud, C. Global mortality associated with seasonal influenza epidemics: New burden estimates and predictors from the GLaMOR Project. J. Glob. Health 2019, 9, 020421. [Google Scholar] [CrossRef]
- Zimmerman, T.; Shiroma, K.; Fleischmann, K.R.; Xie, B.; Jia, C.; Verma, N.; Lee, M.K. Misinformation and COVID-19 vaccine hesitancy. Vaccine 2023, 41, 136–144. [Google Scholar] [CrossRef] [PubMed]
- Romer, D.; Jamieson, K.H. Conspiratorial thinking, selective exposure to conservative media, and response to COVID-19 in the US. Soc. Sci. Med. 2021, 291, 114480. [Google Scholar] [CrossRef] [PubMed]
- Leading Countries Based on Number of Twitter Users as of January 2022 (In Millions). Available online: https://www.statista.com/statistics/242606/number-of-active-twitter-users-in-selected-countries (accessed on 31 March 2023).
- Barry, B. These are the Countries Where Twitter, Facebook and TikTok are Banned. Available online: https://time.com/6139988/countries-where-twitter-facebook-tiktok-banned/ (accessed on 2 May 2023).
- Kruspe, A.; Häberle, M.; Hoffmann, E.J.; Rode-Hasinger, S.; Abdulahhad, K.; Zhu, X.X. Changes in Twitter geolocations: Insights and suggestions for future usage. arXiv 2021. [Google Scholar] [CrossRef]
- Sloan, L.; Morgan, J. Who tweets with their location? Understanding the relationship between demographic characteristics and the use of geoservices and geotagging on Twitter. PLoS ONE 2015, 10, e0142209. [Google Scholar] [CrossRef]
- Yi, J.; Gina Qu, J.; Zhang, W.J. Depicting the emotion flow: Super-spreaders of emotional messages on Weibo during the COVID-19 pandemic. Soc. Media + Soc. 2022, 8, 20563051221084950. [Google Scholar] [CrossRef]
- Zhang, M.; Qi, X.; Chen, Z.; Liu, J. Social bots’ involvement in the COVID-19 vaccine discussions on Twitter. Int. J. Environ. Res. Public Health 2022, 19, 1651. [Google Scholar] [CrossRef]
| Theme and Topic (Keywords) | Sample Tweets | Number of Tweets, n (%) |
|---|---|---|
| Theme 1: Criticism of governmental policies related to influenza vaccination | ||
| Topic 1: Criticism of the government policy on mandatory influenza vaccine (effective, such as flu vaccine, arm, GP, day, NHS, strain, flu, flu shot) | “What is your problem, what happened to free will? If some people don t want it then why should we force them? Not everyone gets the flu jab every year” “Just had breaking news here in my state where ALL children are going to be required to have the ‘flu vaccine’ before heading back to school. People are pissed as they should be. NO ONE is going to make me get any flu shot if I don’t want one ever. I’ll move to another country | 221,732 (84.8) |
| Topic 2: Criticism on public messaging around influenza vaccination (trump, vaccine work, flu vaccine work, president, guy, thinks, solid, solid flu vaccine, solid flu, corona) | “Heard him say that at the rally, but heard a radio interview from last week where he said he didn’t. Never takes flu vaccine either.” “My shock is from when he says he never had flu vaccine, hence I ask if as a politician he never traveled to countries where they are mandatory. I was not focused on this one when I made comment” | 5272 (2.0) |
| Topic 4: Criticism of the government policy on priority groups to receive COVID-19 and influenza vaccine (asthma, asthmatics, group, asthmatics at risk, jab list, flu jab list, priority, JCVI, eligible, asthmatic) | “On BBC breakfast this morning they’ve said everyone who has an annual flu jab will get a COVID-19 booster, and these people are clinically extremely vulnerable. Except many asthmatics who get an annual flu jab, including myself, don’t qualify for a COVID-19 vaccine yet….” “What you say is not happening in reality. My husband is asthmatic, a key worker and at 46 has been told he cannot have COVID-19 vaccination as not in priority group. Why is he offered a flu jab annually but not a COVID-19 vaccination as a dangerous respiratory virus?” | 1636 (0.6) |
| Theme 2: Misinformation related to influenza vaccination | ||
| Topic 3: Misconception that mask wearing can replace influenza vaccine (mask, masks, wear, wearing, wear mask, wearing masks, wearing mask, mask flu, wear masks, flu season) | “If masks can save us from COVID-19, they should be able to save us from flu. So why would anyone want a flu jab considering masks are mandatory??” “I am not bothering with the flu vaccine the masks killed it last year.” | 2618 (1.0) |
| Topic 5: Concerns about mRNA vaccine technology (MRNA, MRNA flu, MRNA flu vaccine, vaccine MRNA, MRNA vaccines, technology, MRNA vaccine, flu vaccine MRNA, RNA, Moderna) | “MRNA flu vaccine in the works now as well. Roll on sudden deaths” “So sad…. and criminal! Apparently, the flu jab is now mRNA.” | 1374 (0.5) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ng, Q.X.; Lee, D.Y.X.; Ng, C.X.; Yau, C.E.; Lim, Y.L.; Liew, T.M. Examining the Negative Sentiments Related to Influenza Vaccination from 2017 to 2022: An Unsupervised Deep Learning Analysis of 261,613 Twitter Posts. Vaccines 2023, 11, 1018. https://doi.org/10.3390/vaccines11061018
Ng QX, Lee DYX, Ng CX, Yau CE, Lim YL, Liew TM. Examining the Negative Sentiments Related to Influenza Vaccination from 2017 to 2022: An Unsupervised Deep Learning Analysis of 261,613 Twitter Posts. Vaccines. 2023; 11(6):1018. https://doi.org/10.3390/vaccines11061018
Chicago/Turabian StyleNg, Qin Xiang, Dawn Yi Xin Lee, Clara Xinyi Ng, Chun En Yau, Yu Liang Lim, and Tau Ming Liew. 2023. "Examining the Negative Sentiments Related to Influenza Vaccination from 2017 to 2022: An Unsupervised Deep Learning Analysis of 261,613 Twitter Posts" Vaccines 11, no. 6: 1018. https://doi.org/10.3390/vaccines11061018
APA StyleNg, Q. X., Lee, D. Y. X., Ng, C. X., Yau, C. E., Lim, Y. L., & Liew, T. M. (2023). Examining the Negative Sentiments Related to Influenza Vaccination from 2017 to 2022: An Unsupervised Deep Learning Analysis of 261,613 Twitter Posts. Vaccines, 11(6), 1018. https://doi.org/10.3390/vaccines11061018