Geographic and Socioeconomic Determinants of Full Coverage COVID-19 Vaccination in Peru: Findings from a National Population-Based Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Variables and Measurements
2.2.1. Dependent Variable
2.2.2. Independent Variables
2.3. Statistical Analysis
2.4. Ethical Considerations
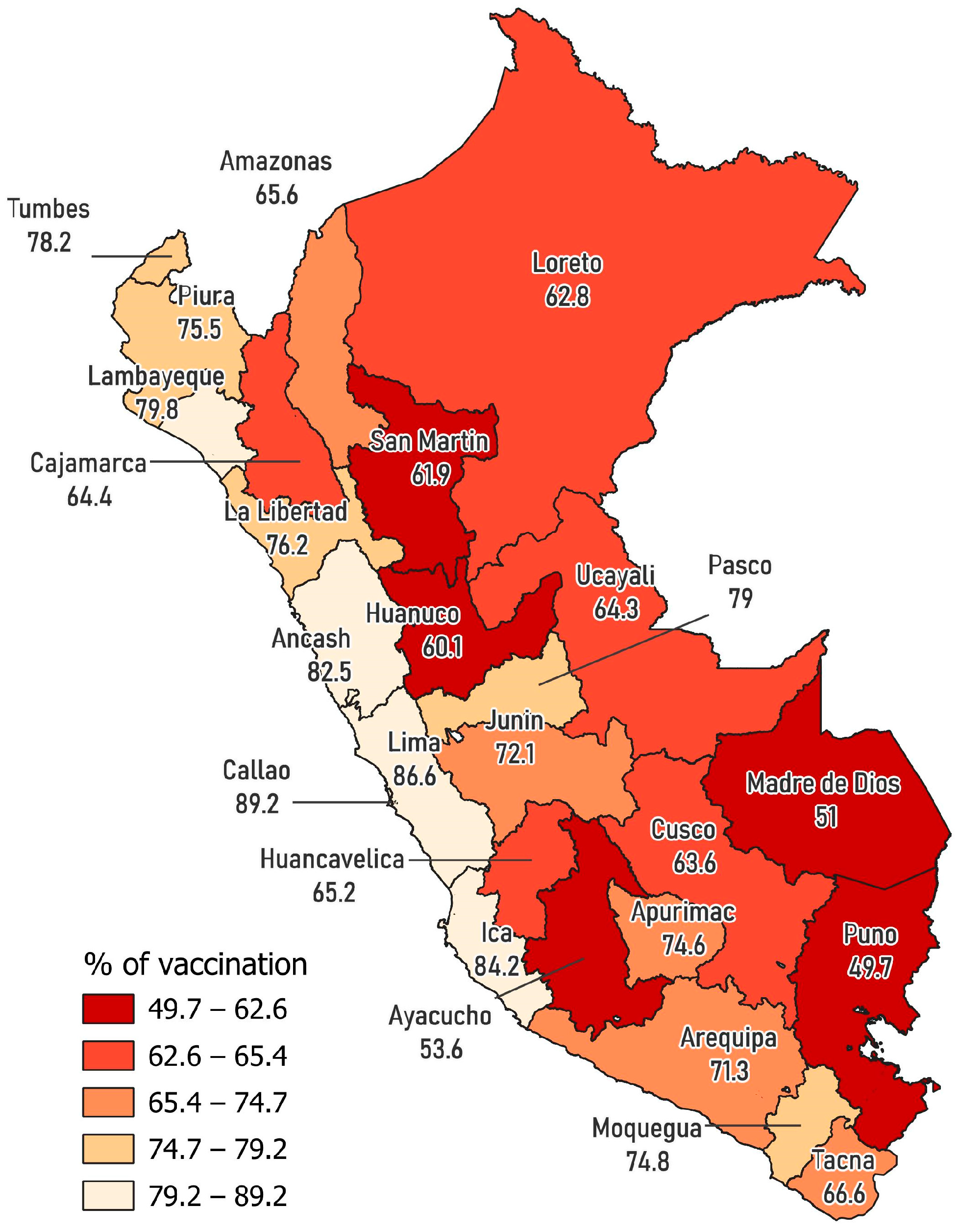
3. Results
4. Discussion
4.1. Main Findings
4.2. Comparison with Previous Studies
4.3. Public Health Implications
4.4. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chang, D.; Chang, X.; He, Y.; Tan, K.J.K. The Determinants of COVID-19 Morbidity and Mortality across Countries. Sci. Rep. 2022, 12, 5888. [Google Scholar] [CrossRef] [PubMed]
- Girum, T.; Lentiro, K.; Geremew, M.; Migora, B.; Shewamare, S.; Shimbre, M.S. Optimal Strategies for COVID-19 Prevention from Global Evidence Achieved through Social Distancing, Stay at Home, Travel Restriction and Lockdown: A Systematic Review. Arch. Public Health 2021, 79, 150. [Google Scholar] [CrossRef]
- Christie, A.; Brooks, J.T.; Hicks, L.A.; Sauber-Schatz, E.K.; Yoder, J.S.; Honein, M.A.; CDC COVID-19 Response Team. Guidance for Implementing COVID-19 Prevention Strategies in the Context of Varying Community Transmission Levels and Vaccination Coverage. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 1044–1047. [Google Scholar] [CrossRef]
- World Health Organization. Global COVID-19 Vaccination Strategy in a Changing World: July 2022 Update. Available online: https://www.who.int/publications/m/item/global-covid-19-vaccination-strategy-in-a-changing-world--july-2022-update (accessed on 22 May 2023).
- Rotshild, V.; Hirsh-Raccah, B.; Miskin, I.; Muszkat, M.; Matok, I. Comparing the Clinical Efficacy of COVID-19 Vaccines: A Systematic Review and Network Meta-Analysis. Sci. Rep. 2021, 11, 22777. [Google Scholar] [CrossRef]
- Rudan, I.; Adeloye, D.; Sheikh, A. COVID-19: Vaccines, Efficacy and Effects on Variants. Curr. Opin. Pulm. Med. 2022, 28, 180–191. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 18 May 2023).
- Tagoe, E.T.; Sheikh, N.; Morton, A.; Nonvignon, J.; Sarker, A.R.; Williams, L.; Megiddo, I. COVID-19 Vaccination in Lower-Middle Income Countries: National Stakeholder Views on Challenges, Barriers, and Potential Solutions. Front. Public Health 2021, 9, 709127. [Google Scholar] [CrossRef]
- Duroseau, B.; Kipshidze, N.; Limaye, R.J. The Impact of Delayed Access to COVID-19 Vaccines in Low- and Lower-Middle-Income Countries. Front. Public Health 2023, 10, 1087138. [Google Scholar] [CrossRef] [PubMed]
- PAHO/WHO. COVID-19 Vaccine Doses Administered in the Americas. Available online: https://ais.paho.org/imm/IM_DosisAdmin-Vacunacion.asp (accessed on 22 May 2023).
- Ministerio de Salud Documento Técnico: Plan Nacional Actualizado de Vacunación Contra La COVID-19 2021. Available online: https://cdn.www.gob.pe/uploads/document/file/1805113/Plan%20Nacional%20Actualizado%20contra%20la%20COVID-19.pdf (accessed on 18 May 2023).
- Diario El Peruano. COVID-19: Conoce Aquí El Cronograma de Vacunación Para Personas de 12 años a Más. Available online: https://elperuano.pe/noticia/124671-covid-19-conoce-aqui-el-cronograma-de-vacunacion-para-personas-de-12-anos-a-mas (accessed on 22 May 2023).
- Ministerio de Salud Protocolo de Aplicación de Dosis de Refuerzo de la Vacuna Contra la COVID-19. Available online: https://cdn.www.gob.pe/uploads/document/file/2517918/Protocolo%20.pdf?v=1637973703 (accessed on 22 May 2023).
- Ministerio de Salud Vacuna COVID-19 en el Perú. Available online: https://public.tableau.com/views/TableroVacunaCovid/VacunacionCOVID?:embed=y&:showVizHome=no&:host_url=https%3A%2F%2Fpublic.tableau.com%2F&:embed_code_version=3&:tabs=no&:toolbar=yes&:animate_transition=yes&:display_static_image=no&:display_spinner=no&:display_overlay=yes&:display_count=yes&:language=es-ES&publish=yes&:loadOrderID=0 (accessed on 22 May 2023).
- Terry, E.; Cartledge, S.; Damery, S.; Greenfield, S. Factors Associated with COVID-19 Vaccine Intentions during the COVID-19 Pandemic; a Systematic Review and Meta-Analysis of Cross-Sectional Studies. BMC Public Health 2022, 22, 1667. [Google Scholar] [CrossRef] [PubMed]
- Vizcardo, D.; Salvador, L.F.; Nole-Vara, A.; Dávila, K.P.; Alvarez-Risco, A.; Yáñez, J.A.; Mejia, C.R. Sociodemographic Predictors Associated with the Willingness to Get Vaccinated against COVID-19 in Peru: A Cross-Sectional Survey. Vaccines 2021, 10, 48. [Google Scholar] [CrossRef]
- Bendezu-Quispe, G.; Caira-Chuquineyra, B.; Fernandez-Guzman, D.; Urrunaga-Pastor, D.; Herrera-Añazco, P.; Benites-Zapata, V.A. Factors Associated with Not Receiving a Booster Dose of COVID-19 Vaccine in Peru. Vaccines 2022, 10, 1183. [Google Scholar] [CrossRef]
- Al-kassab-Córdova, A.; Mendez-Guerra, C.; Silva-Perez, C.; Herrera-Añazco, P.; Benites-Zapata, V.A. Inequalities in COVID-19 Vaccination Coverage in Peru: An Ecological Study. Public Health Pract. 2023, 5, 100384. [Google Scholar] [CrossRef] [PubMed]
- Instituto Nacional de Estadística e Informática Ficha Técnica: Encuesta Nacional de Hogares 2022. Available online: https://www.inei.gob.pe/media/encuestas/documentos/enaho/2022/Ficha_tecnica2022.pdf (accessed on 18 May 2023).
- Instituto Nacional de Estadística e Informática Perú: Evolución de La Pobreza Monetaria. Informe Técnico. Available online: https://www.inei.gob.pe/media/MenuRecursivo/publicaciones_digitales/Est/pobreza2022/Pobreza2022.pdf (accessed on 18 May 2023).
- Diario El Peruano COVID-19: Dosis de Refuerzo se Aplicará Desde Este Viernes 26 a Personas de 18 años o Más. Available online: https://elperuano.pe/noticia/134142-covid-19-dosis-de-refuerzo-se-aplicara-desde-este-viernes-26-a-personas-de-18-anos-o-mas (accessed on 22 May 2023).
- Ministerio de Salud Protocolo Actualizado Para la Aplicación de Tercera y Cuarta Dosis Para la Vacunación Contra la COVID-19. Available online: https://cdn.www.gob.pe/uploads/document/file/3452341/Protocolo%20.pdf?v=1658868919 (accessed on 22 May 2023).
- Spetz, M.; Lundberg, L.; Nwaru, C.; Li, H.; Santosa, A.; Ng, N.; Leach, S.; Gisslén, M.; Hammar, N.; Nyberg, F.; et al. An Intersectional Analysis of Sociodemographic Disparities in COVID-19 Vaccination: A Nationwide Register-Based Study in Sweden. Vaccine 2022, 40, 6640–6648. [Google Scholar] [CrossRef] [PubMed]
- Getachew, T.; Negash, A.; Degefa, M.; Lami, M.; Balis, B.; Debela, A.; Gemechu, K.; Shiferaw, K.; Nigussie, K.; Bekele, H.; et al. COVID-19 Vaccine Acceptance and Associated Factors among Adult Clients at Public Hospitals in Eastern Ethiopia Using the Health Belief Model: Multicentre Cross-Sectional Study. BMJ Open 2023, 13, e070551. [Google Scholar] [CrossRef]
- Farah, W.; Breeher, L.E.; Hainy, C.M.; Tommaso, C.P.; Swift, M.D. Who Is Getting Boosted? Disparities in COVID-19 Vaccine Booster Uptake among Health Care Workers. Vaccine X 2023, 13, 100269. [Google Scholar] [CrossRef]
- Guay, M.; Maquiling, A.; Chen, R.; Lavergne, V.; Baysac, D.-J.; Racine, A.; Dubé, E.; MacDonald, S.E.; Gilbert, N.L. Measuring Inequalities in COVID-19 Vaccination Uptake and Intent: Results from the Canadian Community Health Survey 2021. BMC Public Health 2022, 22, 1708. [Google Scholar] [CrossRef] [PubMed]
- Duan, Y.; Shi, J.; Wang, Z.; Zhou, S.; Jin, Y.; Zheng, Z.-J. Disparities in COVID-19 Vaccination among Low-, Middle-, and High-Income Countries: The Mediating Role of Vaccination Policy. Vaccines 2021, 9, 905. [Google Scholar] [CrossRef]
- Lazarus, J.V.; Wyka, K.; White, T.M.; Picchio, C.A.; Gostin, L.O.; Larson, H.J.; Rabin, K.; Ratzan, S.C.; Kamarulzaman, A.; El-Mohandes, A. A Survey of COVID-19 Vaccine Acceptance across 23 Countries in 2022. Nat. Med. 2023, 29, 366–375. [Google Scholar] [CrossRef] [PubMed]
- Zintel, S.; Flock, C.; Arbogast, A.L.; Forster, A.; Von Wagner, C.; Sieverding, M. Gender Differences in the Intention to Get Vaccinated against COVID-19: A Systematic Review and Meta-Analysis. J. Public Health 2022. [Google Scholar] [CrossRef]
- Wingert, A.; Pillay, J.; Gates, M.; Guitard, S.; Rahman, S.; Beck, A.; Vandermeer, B.; Hartling, L. Risk Factors for Severity of COVID-19: A Rapid Review to Inform Vaccine Prioritisation in Canada. BMJ Open 2021, 11, e044684. [Google Scholar] [CrossRef]
- Dubé, È.; Dionne, M.; Pelletier, C.; Hamel, D.; Gadio, S. COVID-19 Vaccination Attitudes and Intention among Quebecers during the First and Second Waves of the Pandemic: Findings from Repeated Cross-Sectional Surveys. Hum. Vaccines Immunother. 2021, 17, 3922–3932. [Google Scholar] [CrossRef]
- Loomba, S.; De Figueiredo, A.; Piatek, S.J.; De Graaf, K.; Larson, H.J. Measuring the Impact of COVID-19 Vaccine Misinformation on Vaccination Intent in the UK and USA. Nat. Hum. Behav. 2021, 5, 337–348. [Google Scholar] [CrossRef] [PubMed]
- Syan, S.K.; Gohari, M.R.; Levitt, E.E.; Belisario, K.; Gillard, J.; DeJesus, J.; MacKillop, J. COVID-19 Vaccine Perceptions and Differences by Sex, Age, and Education in 1,367 Community Adults in Ontario. Front. Public Health 2021, 9, 719665. [Google Scholar] [CrossRef] [PubMed]
- Smith, B.A.; Ricotta, E.E.; Kwan, J.L.; Evans, N.G. COVID-19 Risk Perception and Vaccine Acceptance in Individuals with Self-Reported Chronic Respiratory or Autoimmune Conditions. Allergy Asthma Clin. Immunol. 2023, 19, 37. [Google Scholar] [CrossRef]
- Ajebli, M.; Amssayef, A.; Akdad, M.; Algharrass, Y.; Babakhouya, A.; Ghanimi, D.; Eddouks, M. Chronic Diseases and COVID-19: A Review. Endocr. Metab. Immune Disord.-Drug Targets 2021, 21, 1781–1803. [Google Scholar] [CrossRef]
- Wang, Q.; Yang, L.; Jin, H.; Lin, L. Vaccination against COVID-19: A Systematic Review and Meta-Analysis of Acceptability and Its Predictors. Prev. Med. 2021, 150, 106694. [Google Scholar] [CrossRef] [PubMed]
- Yabar, C.A. Extreme Poverty First: An Argument on the Equitable Distribution of the COVID-19 Vaccine in Peru. Dev. World Bioeth. 2023, dewb.12391. [Google Scholar] [CrossRef]
- Aguilar, A.; Pinto, J.A.; Araujo, J.; Fajardo, W.; Bravo, L.; Pinillos, L.; Vallejos, C. Control of Cervical Cancer in Peru: Current Barriers and Challenges for the Future. Mol. Clin. Oncol. 2016, 5, 241–245. [Google Scholar] [CrossRef]
- Hernández-Vásquez, A.; Bendezu-Quispe, G.; Turpo Cayo, E.Y. Indigenous Communities of Peru: Level of Accessibility to Health Facilities. J. Taibah Univ. Med. Sci. 2022, 17, 810–817. [Google Scholar] [CrossRef]
- Di Mauro, A.; Di Mauro, F.; De Nitto, S.; Rizzo, L.; Greco, C.; Stefanizzi, P.; Tafuri, S.; Baldassarre, M.E.; Laforgia, N. Social Media Interventions Strengthened COVID-19 Immunization Campaign. Front. Pediatr. 2022, 10, 869893. [Google Scholar] [CrossRef]
- Ministerio de Salud Minsa Lanzó Campaña Para Promover la Vacunación Contra la COVID-19 en Todo El País. Available online: https://www.gob.pe/institucion/minsa/noticias/500970-minsa-lanzo-campana-para-promover-la-vacunacion-contra-la-covid-19-en-todo-el-pais (accessed on 22 May 2023).
| Characteristics | n (n = 58,471) | % |
|---|---|---|
| Gender | ||
| Male | 27,782 | 47.4 |
| Female | 30,689 | 52.6 |
| Age group (years) | ||
| 18–29 | 13,792 | 24.6 |
| 30–59 | 30,964 | 52.8 |
| 60 or more | 13,715 | 22.5 |
| Educational level | ||
| None or elementary school | 3429 | 5.2 |
| Primary education | 15,314 | 23.0 |
| Secondary education | 22,148 | 41.3 |
| Higher education | 17,580 | 30.5 |
| Ethnicity | ||
| Non-native | 40,903 | 72.9 |
| Native | 17,568 | 27.1 |
| Chronic disease | ||
| No | 26,820 | 46.5 |
| Yes | 31,651 | 53.5 |
| Physical or psychological limitation | ||
| No | 54,727 | 94.2 |
| Yes | 3744 | 5.8 |
| Type of main occupation | ||
| Non-health-related activities | 44,696 | 73.8 |
| Health-related activities | 1026 | 1.7 |
| No main occupation | 12,749 | 24.5 |
| Poverty status | ||
| Extreme poverty | 2606 | 3.9 |
| Non-extreme poverty | 9927 | 19.5 |
| Non-poor | 45,938 | 76.6 |
| Home without media | ||
| No | 56,112 | 97.2 |
| Yes | 2359 | 2.8 |
| Natural region of residence | ||
| Jungle | 12,199 | 11.3 |
| Highlands | 20,058 | 30.7 |
| Coast | 26,214 | 58.0 |
| Area of residence | ||
| Rural | 19,054 | 19.0 |
| Urban | 39,417 | 81.0 |
| Characteristics | Three or More Doses of Vaccine Against COVID-19 | ||
|---|---|---|---|
| No (n = 15,721) | Yes (n = 42,750) | ||
| % (95% CI) | % (95% CI) | p-Value * | |
| Overall | 24.2 (23.4–25.0) | 75.8 (75.0–76.6) | |
| Gender | |||
| Male | 25.7 (24.7–26.6) | 74.3 (73.4–75.3) | <0.001 |
| Female | 22.9 (22.0–23.8) | 77.1 (76.2–78.0) | |
| Age group (years) | |||
| 18–29 | 29.1 (27.7–30.5) | 70.9 (69.5–72.3) | <0.001 |
| 30–59 | 25.0 (24.1–25.9) | 75.0 (74.1–75.9) | |
| 60 or more | 17.1 (16.0–18.2) | 82.9 (81.8–84.0) | |
| Educational level | |||
| None or elementary school | 36.5 (34.2–39.0) | 63.5 (61.0–65.8) | <0.001 |
| Primary education | 32.9 (31.5–34.3) | 67.1 (65.7–68.5) | |
| Secondary education | 26.2 (25.1–27.3) | 73.8 (72.7–74.9) | |
| Higher education | 12.9 (12.0–13.8) | 87.1 (86.2–88.0) | |
| Ethnicity | |||
| Non-native | 20.1 (19.3–21.0) | 79.9 (79.0–80.7) | <0.001 |
| Native | 35.2 (33.7–36.8) | 64.8 (63.2–66.3) | |
| Chronic disease | |||
| No | 27.7 (26.7–28.8) | 72.3 (71.2–73.3) | <0.001 |
| Yes | 21.2 (20.3–22.1) | 78.8 (77.9–79.7) | |
| Physical or psychological limitation | |||
| No | 24.1 (23.3–25.0) | 75.9 (75.0–76.7) | 0.202 |
| Yes | 25.5 (23.4–27.7) | 74.5 (72.3–76.6) | |
| Type of main occupation | |||
| Non-health-related activities | 26.1 (25.2–27.1) | 73.9 (72.9–74.8) | <0.001 |
| Health-related activities | 8.0 (5.8–10.9) | 92.0 (89.1–94.2) | |
| No main occupation | 19.5 (18.3–20.7) | 80.5 (79.3–81.7) | |
| Poverty status | |||
| Extreme poverty | 46.3 (42.1–50.5) | 53.7 (49.5–57.9) | <0.001 |
| Non-extreme poverty | 32.4 (30.6–34.3) | 67.6 (65.7–69.4) | |
| Non-poor | 21.0 (20.2–21.8) | 79.0 (78.2–79.8) | |
| Home without media | |||
| No | 23.7 (22.9–24.6) | 76.3 (75.4–77.1) | <0.001 |
| Yes | 40.8 (37.5–44.3) | 59.2 (55.7–62.5) | |
| Natural region of residence | |||
| Jungle | 40.1 (38.1–42.2) | 59.9 (57.8–61.9) | <0.001 |
| Highlands | 33.8 (32.2–35.4) | 66.2 (64.6–67.8) | |
| Coast | 16.0 (15.1–17.0) | 84.0 (83.0–84.9) | |
| Area of residence | <0.001 | ||
| Rural | 40.9 (39.3–42.6) | 59.1 (57.4–60.7) | |
| Urban | 20.3 (19.4–21.2) | 79.7 (78.8–80.6) | |
| Variable | Crude Model | Adjusted Model | ||
|---|---|---|---|---|
| PR (95% CI) | p-Value | aPR (95% CI) | p-Value | |
| Gender | ||||
| Male | Reference | Reference | ||
| Female | 1.04 (1.03–1.05) | <0.001 | 1.04 (1.03–1.06) | <0.001 |
| Age group (years) | ||||
| 18–29 | Reference | Reference | ||
| 30–59 | 1.06 (1.04–1.08) | <0.001 | 1.10 (1.08–1.12) | <0.001 |
| 60 or more | 1.17 (1.15–1.19) | <0.001 | 1.28 (1.25–1.31) | <0.001 |
| Educational level | ||||
| None or elementary school | Reference | Reference | ||
| Primary education | 1.06 (1.02–1.10) | 0.004 | 1.07 (1.03–1.11) | 0.001 |
| Secondary education | 1.16 (1.12–1.21) | <0.001 | 1.16 (1.12–1.21) | <0.001 |
| Higher education | 1.37 (1.32–1.43) | <0.001 | 1.33 (1.28–1.39) | <0.001 |
| Ethnicity | ||||
| Non-native | Reference | Reference | ||
| Native | 0.81 (0.79–0.83) | <0.001 | 0.89 (0.87–0.92) | <0.001 |
| Chronic disease | ||||
| No | Reference | Reference | ||
| Yes | 1.09 (1.07–1.11) | <0.001 | 1.04 (1.03–1.06) | <0.001 |
| Physical or psychological limitation | ||||
| No | Reference | Not included | ||
| Yes | 0.98 (0.95–1.01) | 0.213 | ||
| Type of main occupation | ||||
| Non-health-related activities | Reference | Reference | ||
| Health-related activities | 1.25 (1.21–1.28) | <0.001 | 1.05 (1.02–1.08) | 0.001 |
| No main occupation | 1.09 (1.07–1.11) | <0.001 | 1.00 (0.99–1.02) | 0.868 |
| Poverty status | ||||
| Extreme poverty | Reference | Reference | ||
| Non-extreme poverty | 1.26 (1.16–1.36) | <0.001 | 1.12 (1.04–1.20) | 0.001 |
| Non-poor | 1.47 (1.36–1.59) | <0.001 | 1.21 (1.13–1.30) | <0.001 |
| Home without media | ||||
| No | Reference | Reference | ||
| Yes | 0.78 (0.73–0.82) | <0.001 | 0.93 (0.88–0.98) | 0.006 |
| Natural region of residence | ||||
| Jungle | Reference | Reference | ||
| Highlands | 1.11 (1.06–1.15) | <0.001 | 1.14 (1.10–1.18) | <0.001 |
| Coast | 1.40 (1.35–1.45) | <0.001 | 1.27 (1.23–1.32) | <0.001 |
| Area of residence | ||||
| Rural | Reference | Reference | ||
| Urban | 1.35 (1.31–1.39) | <0.001 | 1.11 (1.07–1.14) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hernández-Vásquez, A.; Vargas-Fernández, R.; Rojas-Roque, C. Geographic and Socioeconomic Determinants of Full Coverage COVID-19 Vaccination in Peru: Findings from a National Population-Based Study. Vaccines 2023, 11, 1195. https://doi.org/10.3390/vaccines11071195
Hernández-Vásquez A, Vargas-Fernández R, Rojas-Roque C. Geographic and Socioeconomic Determinants of Full Coverage COVID-19 Vaccination in Peru: Findings from a National Population-Based Study. Vaccines. 2023; 11(7):1195. https://doi.org/10.3390/vaccines11071195
Chicago/Turabian StyleHernández-Vásquez, Akram, Rodrigo Vargas-Fernández, and Carlos Rojas-Roque. 2023. "Geographic and Socioeconomic Determinants of Full Coverage COVID-19 Vaccination in Peru: Findings from a National Population-Based Study" Vaccines 11, no. 7: 1195. https://doi.org/10.3390/vaccines11071195
APA StyleHernández-Vásquez, A., Vargas-Fernández, R., & Rojas-Roque, C. (2023). Geographic and Socioeconomic Determinants of Full Coverage COVID-19 Vaccination in Peru: Findings from a National Population-Based Study. Vaccines, 11(7), 1195. https://doi.org/10.3390/vaccines11071195







