Abstract
Pregnant women are a highly vaccine-resistant population and face unique circumstances that complicate vaccine decision-making. Pregnant women are also at increased risk of adverse maternal and neonatal outcomes to many vaccine-preventable diseases. Several models have been proposed to describe factors informing vaccine hesitancy and acceptance. However, none of these existing models are applicable to the complex decision-making involved with vaccine acceptance during pregnancy. We propose a model for vaccine decision-making in pregnancy that incorporates the following key factors: (1) perceived information sufficiency regarding vaccination risks during pregnancy, (2) harm avoidance to protect the fetus, (3) relationship with a healthcare provider, (4) perceived benefits of vaccination, and (5) perceived disease susceptibility and severity during pregnancy. In addition to these factors, the availability of research on vaccine safety during pregnancy, social determinants of health, structural barriers to vaccine access, prior vaccine acceptance, and trust in the healthcare system play roles in decision-making. As a final step, the pregnant individual must balance the risks and benefits of vaccination for themselves and their fetus, which adds greater complexity to the decision. Our model represents a first step in synthesizing factors informing vaccine decision-making by pregnant women, who represent a highly vaccine-resistant population and who are also at high risk for adverse outcomes for many infectious diseases.
1. Introduction
Pregnant women and their fetuses are at greater risk for adverse outcomes of many infectious diseases compared to non-pregnant people, leading to an increased risk for hospitalization, maternal death, preterm birth, congenital anomalies, and stillbirth [1,2,3,4,5,6,7,8,9,10,11,12]. Vaccination can play a crucial role in protecting the health of pregnant women and fetuses due to maternal antibody transfer across the placenta and through breast milk after birth. The U.S. Centers for Disease Control recommend that women receive several vaccines during pregnancy, including vaccines for pertussis, tetanus, diphtheria, polio, influenza, and coronavirus disease of 2019 (COVID-19) [13]. Despite these recommendations, pregnant individuals are highly vaccine-hesitant. During the COVID-19 pandemic, vaccination rates for COVID-19 remained lower among pregnant versus non-pregnant women, even though contracting COVID-19 during pregnancy conferred a greater risk for adverse outcomes [14,15]. A significant knowledge gap exists regarding the factors influencing vaccine decision-making in pregnancy.
Barriers to vaccine uptake for pregnant individuals include safety concerns regarding the vaccine, lack of information on vaccines from care providers, perceived lack of data on the safety of vaccines, and low self-perceived risk of infection or severity of illness [16]. Despite the existence of many clinical practice guidelines regarding SARS-CoV-2 vaccination in pregnancy, there was an information gap between experts in pregnancy vaccination and the pregnant lay public [17]. Historically, pregnant women have also been excluded from clinical vaccine trials, which contributes to a lack of confidence as to the safety of vaccines for them or their fetuses [18,19]. Perceived insufficiency of data regarding vaccine safety for the fetus is a common reason for vaccine hesitancy among pregnant women [16,20]. An information gap and lack of research and public health messaging around vaccines and the concerns of pregnant or reproductive-aged women has led to disinformation linking vaccination to adverse fertility or pregnancy outcomes. To address these barriers, we launched a limited public health campaign and research program, called One Vax Two Lives, during the COVID-19 pandemic [21,22]. However, without a vaccine-decision-making model in pregnancy, a public health campaign is likely to miss key factors driving uptake.
Several health decision and health behavior models have been applied to vaccine hesitancy and acceptance, including the Health Belief Model [23,24,25], 3C [26], 4C [27], and the 5A models [28]. Pregnancy represents an intense information-seeking phase in life, in which pregnant women face heightened awareness of the impact of their health decisions on their fetuses; the sensitivity of this decision also increases vulnerability to disinformation. The unique complexity of pregnancy is not captured by any of the general models of health behavior or vaccine hesitancy. Our objective is to highlight the challenges of vaccine decision-making in pregnancy and to present a new vaccine-acceptance model that can be used to inform public health campaigns and provider–patient interactions targeting pregnant women. We begin by exploring barriers to vaccination in pregnancy. Secondly, we address current vaccine-acceptance models and the ways in which they can and cannot be applied to pregnant individuals as decision-makers. Finally, we propose a new 5-P model for vaccine decision-making in pregnancy and address how these factors influence vaccination and other health decisions of pregnant individuals.
2. Barriers to Vaccination in Pregnancy
The recent COVID-19 pandemic and rapid rollout of vaccines presented an opportunity to understand barriers to vaccination in pregnancy. Vaccine hesitancy can be generally divided into structural and attitudinal barriers, with the latter playing a larger role in why pregnant individuals have greater vaccine hesitancy [29]. Early reasons for COVID-19 vaccine hesitancy involved the concern about the lack of data regarding its safety during pregnancy [30,31,32,33]. For pregnant individuals, vaccine safety was initially unknown, as pregnant and lactating individuals were not included in the initial Phase 3 studies [18]. One study found that 98.7% of pregnant respondents were aware that there was a COVID-19 vaccine available but very few were knowledgeable about the vaccine [31]. Furthermore, the available information about vaccination in pregnancy was often contradictory, making it difficult to know what was accurate and further enhancing skepticism about the vaccine’s efficacy and safety [34]. The internet and social media were significant sources of misinformation, perpetuating confusion and vaccine hesitancy. Concern about the COVID-19 vaccine’s efficacy was also a reason for vaccine hesitancy in pregnant and breastfeeding individuals [31,33,34]. In addition to pregnancy-specific and other attitudinal barriers to vaccination in pregnancy, there are also many other structural barriers to vaccination (e.g., access, affordability, trust in science), which are addressed in many vaccine-acceptance models designed for the general population.
3. Models of Vaccine Acceptance
There are no specific models for vaccine acceptance in pregnancy, but several constructs that explain factors informing vaccine hesitancy and acceptance exist; many of these models build upon the Health Belief Model (HBM) [23,24,25], which was generally designed to describe factors informing health decision-making. The HBM is divided into several categories: perceived susceptibility to the disease, perceived severity of the disease, perceived benefits of the disease-prevention behavior, barriers to the disease-prevention behavior, a cue to action, and self-efficacy. The cue to action represents events, people, or things that help trigger a change in health behavior. Self-efficacy refers to one’s confidence in the health behavior, which could represent one’s trust and confidence that vaccination is a healthy choice.
In 2014, a new vaccine-decision-making model was proposed, called the 3C model. The 3C model describes three factors of vaccine hesitancy: confidence, complacency, and convenience [26]. Confidence can be described as a belief in the safety of vaccines, the reliability of the healthcare systems that deliver them, and the motivations of policymakers. Complacency can be described as belief (or lack thereof) in the necessity of the vaccine with respect to other life responsibilities. Convenience can be described as the access to and affordability of the vaccine for those who want it. This was expanded in 2015 in the 4C model to include a utility calculation, where the benefits of the vaccine play a larger role [27]. In 2016, the 5A model was developed, in which vaccine acceptance was described in terms of access, affordability, awareness, acceptance, and activation [28]. The factors, strengths, and limitations are described with respect to vaccination and vaccination in pregnancy in Table 1.

Table 1.
Factors, strengths, and limitations of vaccine-hesitancy models.
These models operate on similar decision-making factors and principles: access, affordability, confidence or self-efficacy, complacency, and utility of intervention. Historic and continual research on the social determinants of health has demonstrated a vast number of factors that influence health outcomes outside of a healthcare setting. Therefore, decision-making frameworks should be heavily based on factors that are contextualized within an individual’s social environment. Access, affordability, and complacency are all factors whose primary effects occur before the patient even decides to make an appointment, and they are arguably the most important factors in determining whether a patient makes a positive healthcare decision. A provider has little power to instill confidence in and utility of healthcare preventions and interventions if a patient lacks access to the provider or does not think to go to the provider. While these factors are helpful and accurate for the general population of the United States, they are less applicable to pregnant individuals, who have more frequent interactions with their healthcare providers during the duration of their pregnancy than non-pregnant adults.
Although there are no specific models for vaccine acceptance in pregnancy, a model has been proposed to describe decision-making in pregnancy that may be applied to vaccine acceptance [35]. This model describes three themes in the decisions of pregnant people: uncertainty, bodily autonomy, and being a good mother. These three themes are interlinked with three actions: information gathering, balancing aspects of a choice, and aligning with a birth philosophy. This model is also inspired by the knowledge that choices during pregnancy cannot be simplified to weighing the pros and cons of medical actions. Instead, it is impacted by perceptions of birth as a natural process or a medical process, desires to maintain body autonomy and independent choice, and stressors of pregnancy [35]. Application of this model to vaccine decision-making addresses, in part, many of the limitations of more traditional decision-making models by describing specifically how safety and perceived worth impact health decisions in pregnancy. However, vaccine decision-making in pregnancy is even more complex, which we describe in a new model.
4. The 5-P Vaccine Acceptance Model in Pregnancy
Although the models in Table 1 are easily applied to the general population, pregnant women have a more complex decision-making process that generally involves balancing risks and benefits for themselves and the fetus [36,37]. We now propose a 5-P model of vaccine acceptance in pregnancy that combines our clinical experience, features of the HBM, and a pregnancy decision-making model [23,24,35,36,37]. By drawing on these models [25,35], literature review as a research methodology [38], as well as our experience from the One Vax Two Lives COVID-19 research and public health campaign [21,22], we can address key elements unique to pregnancy decision-making.
The basic tenets of the HBM certainly remain true in that health decisions are influenced by a combination of one’s perceptions of the benefits and barriers related to that health behavior as well as perceptions of disease susceptibility and severity. The pregnant population intersects with this model, but carries additional distinctive factors separate from the rest of the general population; therefore, we propose a new model of vaccine decision-making that is unique to the pregnant perspective.
However, additional elements should be considered that are unique to pregnancy, including the intense information-seeking nature of pregnancy, the frequent exposure to healthcare providers that can impart their knowledge of and opinions on vaccination during pregnancy, and a frequent stance of harm avoidance that is typical in pregnancy. Historically, there has been little scientific evidence regarding the safety and efficacy of new vaccines in pregnancy, as pregnant people were excluded. Furthermore, public health campaigns have not prioritized the dissemination of health information to pregnant people, as they represent a minority of the population. Consequently, at a time in life when information about health decisions is valued highly, there has been little to no information available on the safety and benefits of a new vaccine during pregnancy.
Many other modifying factors can also influence an individual’s perceptions and, ultimately, their health behavior. These factors include characteristics of an individual, such as their age, geographic location, income, or level of education. For example, rural areas in the United States are associated with lower vaccination uptake among pregnant people than non-rural areas [39]. Race and ethnicity are other modifying factors. Historically, Black and Latinx people have shown greater vaccine hesitancy and lower vaccine uptake. This can be accredited to barriers to health behavior created by racism and a history of harm perpetuated by the medical field on these communities. A 2020 Kaiser Family Foundation survey found that 45% of Black patients had experienced negative experiences with a healthcare provider [40]. Vaccine decision-making in pregnancy clearly exists on the background of a person’s socioeconomic, geographic, educational, and racial/ethnic identity.
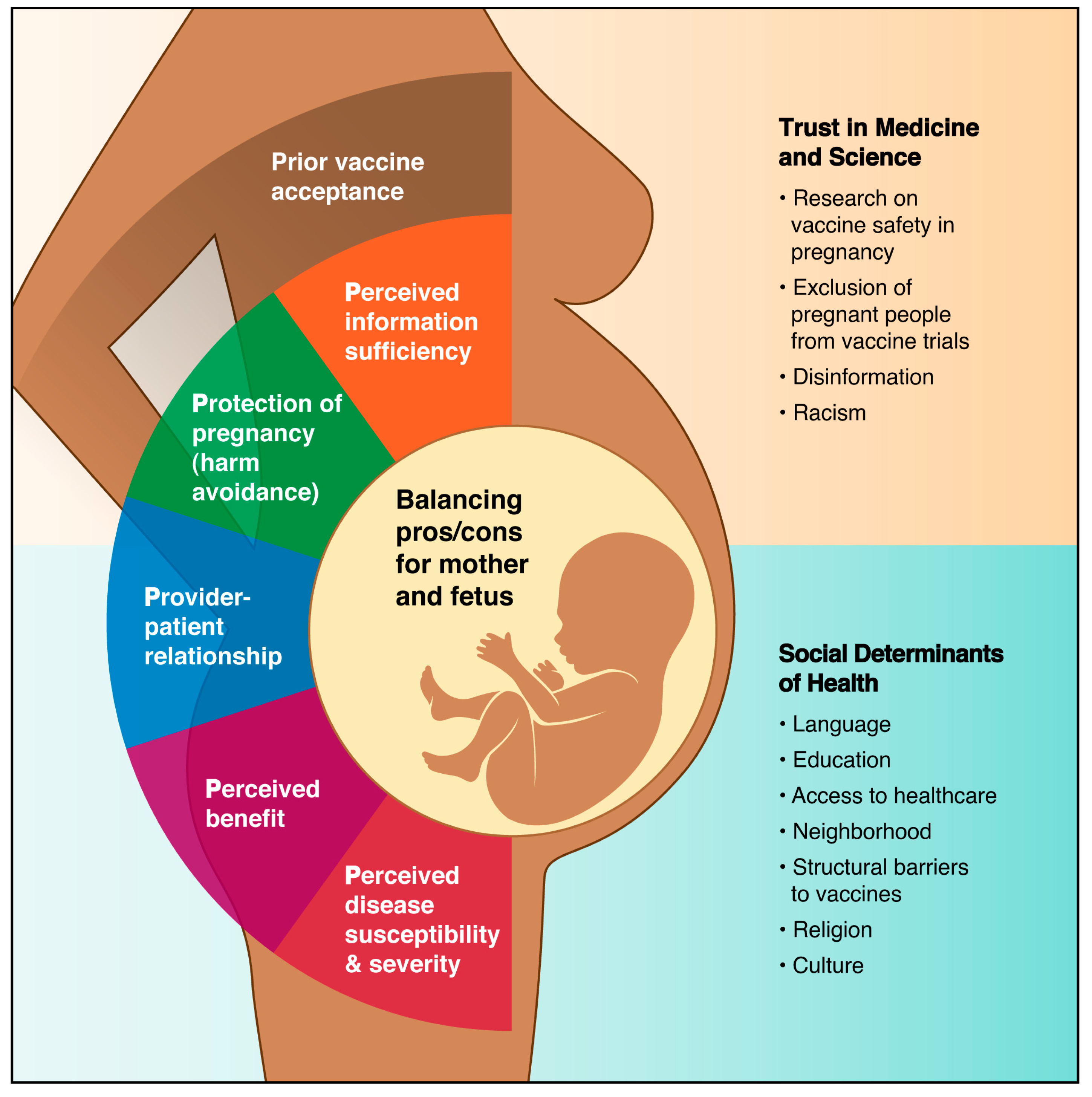
The key factors informing the 5-P model include: (1) perceived information sufficiency on vaccine safety in pregnancy, (2) protection of pregnancy (harm avoidance), (3) provider–patient relationship, (4) perceived vaccine benefits for mother and fetus, and (5) perceived disease susceptibility and severity in pregnancy (Figure 1, Table 2). Two themes regarding decision-making in the pregnancy model, uncertainty and bodily autonomy, ultimately play into the “perceived information sufficiency” and “balancing pros and cons for mother and fetus” elements of our model, respectively. Additional elements that are more universal in medical decision-making also contribute to vaccine decision-making in pregnancy and can be positive, negative, or neutral factors in the ultimate decision. The final step in the process requires a careful balancing of the risks and benefits for oneself and one’s fetus, which can be a taxing process given the many inputs into the decision, including, potentially, the partner’s opinion. Prior vaccine acceptance and trust can also be a determinant of vaccine decision-making but was not included as a key component of the 5-P model. Overall, vaccination during pregnancy is a complex decision. Unique pregnancy-specific factors must be considered in addition to other factors applicable to the general population in understanding the decision-making process.
Figure 1.
The 5-P model for vaccine decision-making in pregnancy.

Table 2.
Examples of factors impacting vaccine acceptance in pregnancy in the 5-P Model.
The figure illustrates the key components of the 5-P model (colored wedges) and how the information (pros/cons) arising from these components must be weighed for the mother and fetus. Other factors informing the decision to vaccinate in pregnancy are also shown that are not included in the 5-P model but may be important determinants in some populations.
The factors defining the 5-P model exist within a background of social determinants of health, including proficiency in the native language, geographic location (country, state, neighborhood), education, healthcare access, structural barriers to vaccination, religion, and culture. Historical events also play a role in determining an individual’s underlying trust in medicine, including medical racism and the exclusion of pregnant individuals from vaccine trials. Finally, the pregnant individual must weigh the pros and cons of all these factors for herself and the fetus, resulting in a complex decision-making process. Maternal vaccine decision-making is influenced by these determinants of health, and the factors themselves may change based on the setting. For example, a woman in a low-resource setting may face barriers to accessing adequate healthcare or vaccines and may experience a provider–patient relationship with a community health worker rather than a doctor or nurse.
4.1. Perceived Information Sufficiency
Pregnancy is an intense information-seeking phase [52]. Information trusted by pregnant women influences health decisions, behavior, and vaccine acceptance [53]. Information sufficiency is also shown to positively influence pregnancy satisfaction [54]. It has also been shown that for many women, vaccine decision-making for the infant commences during their pregnancy [52]. Given the heightened risk to pregnant women that COVID-19 presents, numerous studies have shown that pregnant women are highly engaged in information-seeking behavior related to COVID-19 infection and vaccines [53]. Conversely, in a study of COVID-19 vaccine uptake during pregnancy, the most cited reason for hesitancy was a lack of knowledge about the vaccine [31]. Lack of data on the safety and efficacy of the vaccine for pregnant women, combined with inconsistent messaging in government advice and guidelines, contributed to vaccine hesitancy and lower vaccine uptake among pregnant women [55]. Exclusion of pregnant individuals from vaccine trials and misinformation about the vaccine’s effects on the fetus and fertility are further barriers to obtaining information regarding pregnancy (Table 2). Pregnant and breastfeeding individuals have lacked the same assurances from clinical research as the general population, leaving them to make vaccination choices without reliable data on the associated risks to themselves and their fetus or child due to the absence of evidence-based data [56].
4.2. Pregnancy Protection of the Mother and Fetus (Harm Avoidance)
During pregnancy, there is a philosophical shift in which the pregnant individual prioritizes avoidance of harm to the fetus. This can be beneficial, such as using pregnancy and the responsibility for reducing harm to the fetus as the impetus to stop smoking and other substance use (Table 2) [42]. It can also be potentially detrimental, such as in the case of self-discontinuation of important medications without the advice or supervision of a physician. The desire to avoid potential teratogenic effects has been the motivating factor for people when discontinuing medications like anti-epilepsy medication and psychotropic medications (Table 2) [43,57].
Harm avoidance for the fetus is also directly related to vaccine hesitancy. In a study of pregnancy in France, researchers found that the main reason for not vaccinating was a greater fear of potential deleterious effects of the vaccine on the fetus than of the COVID-19 disease itself [58]. In a Canadian study, perceived personal risk of COVID-19 was not a predictor of a pregnant person’s vaccine acceptance, indicating that for those who were vaccine-hesitant, perceived risk of the vaccine outweighed perceived risk of the illness [59]. Here, the avoidance of risk trumped any possible vaccine benefit. Understanding the hierarchy of priorities is helpful for understanding vaccine uptake during pregnancy. If there is a question about the potential for the vaccine to harm the fetus, the pregnant individual may simply avoid vaccination.
4.3. Provider–Patient Relationship
Recommendations from healthcare providers are commonly cited as a reason for vaccine uptake among pregnant people. The term healthcare provider encompasses a vast definition, which may include physicians, nurses, midwives, or community health workers, depending on the setting and resources available. Studies of influenza and Tdap vaccination show that vaccine uptake among pregnant women is higher for those who receive vaccine recommendations from their care providers [60,61]. Pregnant people indicate that they are more willing to receive vaccines if they received a recommendation from their provider to do so [62]. In one study, participants who were ranked as highly likely to receive the COVID-19 vaccine identified physicians to be their main source of COVID-19 vaccine information, and 37% indicated that a physician recommendation would reduce their vaccine hesitancy [63].
In a study on how mothers’ perceptions of vaccines evolved over time, those who experienced increased confidence in vaccines did so in part due to positive relationships and experiences with care providers. Participants described having conversations with trusted doctors, physicians, and public health nurses about the safety and importance of vaccines. Participants reported that convincing techniques used by these care providers included listening to the mothers’ specific concerns, communicating shared values, sharing their (the provider’s) own personal experiences with vaccines, and addressing specific concerns about the ingredients of vaccines or their side effects [64]. We propose that the relationship between a pregnant woman and her obstetric or primary care provider is a critical piece in the decision to vaccinate during pregnancy and enables the pregnant woman to feel empowered to make a decision.
In contrast to the data on the importance of care providers in the pregnant woman’s decision to vaccinate, there are mixed results on the influence of partners and family. A systematic review of studies conducted in low- and middle-income countries representing a vast geographical region found that family members and husbands influenced the decision-making process, with husbands being the most influential individuals [65]. However, a study conducted with pregnant women from Latin America found many women received vaccinations without consulting family or friends, and only a few considered the opinions of family members or male partners [66]. Although the influence of partners and family is important, the opinion of healthcare providers, whether that be physicians or community health workers, appears to supersede that of family and partner as a key determinant for vaccine uptake.
4.4. Perceived Benefits
Studies and research have shown that the COVID-19 vaccine provides numerous benefits to pregnant women, including a reduced risk of hospitalization and death for the mother, and transmission of neutralizing antibodies to the fetus that confers disease protection after birth [60,67]. Pregnant individuals with beliefs that the COVID-19 vaccine carried benefits were less vaccine-hesitant and more likely to be vaccinated against COVID-19 or report an intent to vaccinate [36,68,69]. In a Canadian study, self-protection was identified by 65% of respondents as their primary reason for receiving the COVID-19 vaccine [59]. A cross-sectional survey among pregnant women in three U.S. cities found that protection of the fetus/newborn was the most common reason for vaccine acceptance among those who reported intent to receive the COVID-19 vaccine [70]. A study on messaging for the seasonal influenza vaccine directed toward pregnant women found that an emphasis on vaccine benefits for the fetus had a positive impact on maternal vaccine confidence [71]. Researchers have called for research on vaccines for pregnant and breastfeeding women to be prioritized, as data on the safety and efficacy of the vaccine during both pregnancy and breastfeeding would likely contribute to the perceived benefits of the vaccine and, ultimately, vaccine uptake [72].
4.5. Perceived Susceptibility and Severity of Disease in Pregnancy
The perception of contracting COVID-19 has fluctuated over time and was greater early in the pandemic. The perception of contracting the disease plays an important role in the decision to get vaccinated and is further complicated by whether they believe a vaccine will provide effective protection [34]. The perceived severity of COVID-19 disease for a pregnant individual is two-pronged, as it involves how both the mother and the infant will be affected. In both cases, a combined perception of the consequences of disease on both individuals plays into the decision on whether contracting the disease will be more or less harmful than getting the vaccine. For COVID-19, the perceived threat of infection was not a direct indicator of willingness to receive the vaccine, as those who believed COVID-19 to be a serious threat were not always willing to receive the vaccine [59]. Multiple studies have shown statistically significant differences in perceived severity of disease between those who get vaccinated and those who do not [30,73]. Interestingly, in one study, perceived threat was not a significant indicator of COVID-19 vaccination hesitancy, suggesting that a potential lack of education, awareness, or perhaps even lack of belief in the consequences of COVID-19 disease may contribute to vaccine resistance [36]. One study found that unvaccinated participants were less likely to agree with the statement that COVID-19 infection is more severe during pregnancy versus their vaccinated counterparts (47% vs. 78%) [30]. These studies suggest that some individuals may be complacent or misinformed about how COVID-19 infection presents differently and more dangerously during pregnancy [30,36]. There are many factors at play that may be contributing to the lack of understanding or belief around the severity of COVID-19 in pregnancy. Two core contributors appear to be a lack of evidence-based communication and disparity in education. A large amount of anecdotal information can be found on social media and TV ads, and individuals who rely on social media platforms such as Twitter or Facebook for health-related information are less likely to receive the influenza vaccine. Furthermore, social media platforms appear to disseminate information regarding vaccine hesitance more successfully than vaccine uptake [74], whereas exposure to direct conversations between healthcare providers and patients has been shown to reduce vaccine hesitancy overall [74]. A wider lens of educational disparities across regions can be used to understand the lack of understanding around the severity of COVID-19 disease for pregnant people. Rates of vaccination in 2021 were found to be lower in rural counties than in urban counties, in part explained by lower education rates [75]. Rural residents have less access to specialty doctors or scientific literature, and their health literacy is generally more limited in these communities [76].
4.6. Balancing Risks and Benefits for Oneself and Fetus
The ultimate decision to vaccinate is the assessment by the pregnant individual that there is a greater benefit of vaccination for herself and/or her fetus than harm associated with vaccination. Key factors informing this decision include perceived information sufficiency, harm-avoidance philosophy in pregnancy, relationship with a healthcare provider, and perceived susceptibility and severity of disease. Pregnant individuals who were concerned about the perceived potential risks of the COVID-19 vaccine reported that they were less likely to accept the COVID-19 vaccine [36,68,69]. However, in one study conducted outside of the United States, perceived benefits about the COVID-19 vaccine contributed positively to vaccine acceptance and vaccination rates [77]. “Positive perceptions” included evaluations of trust and mistrust in the benefits of the vaccine, beliefs regarding the vaccine causing infertility, and future risks of the vaccine, among others. Studies have, in turn, hypothesized that the type of information that may contribute to an individual’s understanding of the benefits of the COVID-19 vaccine and/or the potential risks of the COVID-19 disease, such as level of education and access to healthcare, may influence a pregnant individual’s acceptance of the COVID-19 vaccine [77,78]. For many women, this means weighing the perceived risks associated with the vaccine with the risks associated with acquiring COVID-19 [52].
The determinants of vaccine decision-making highlighted in the 5-P model also intersect with one another to influence vaccine decision-making. For example, a trusting relationship with a healthcare provider can facilitate conversations that focus on the benefits of vaccination as well as call attention to the susceptibility and severity of diseases such as COVID-19. A patient–provider relationship built on trust will also influence a pregnant individual’s perception of information sufficiency to encourage them to be vaccinated. This, in turn, impacts an individual’s perception of harm avoidance, as pregnant individuals will be able to determine whether vaccination or taking the risk of not vaccinating (and acquiring the disease) is best for pregnancy protection.
4.7. Limitations of Models of Vaccine Acceptance in Pregnancy and Research Gaps
While the HBM includes modifying factors as a core part of the likelihood of action, the assessment of intersectionality among pregnant and recently pregnant individuals is crucial to develop strategies that address COVID-19 vaccine hesitancy. Previous research has demonstrated the need for gender-based approaches to improving vaccine confidence and uptake that also intersect with socioeconomic status [79]. Specifically, more attention and resources toward increasing vaccine uptake should be directed to women living in low-income households and/or working women. Further, culturally competent approaches should be prioritized among African American populations who face higher rates of maternal mortality. Research on vaccine hesitancy should be conducted broadly among minority and non-English speaking groups, who have been historically harmed or marginalized by medicine and science. Research should also be conducted to learn about the reaction of pregnant individuals to social media ads and other public health materials to determine the best method of addressing pregnant women’s unique sources of vaccine hesitancy.
5. Conclusions
Increasing vaccine uptake in populations vulnerable to disease is an important goal of public health, but a framework for vaccine decision-making in pregnancy has been lacking and is complex. Pregnant women face unique health concerns, and addressing vaccine hesitancy requires a different approach in public health campaigns to increase vaccine uptake in this unique population. Our 5-P model draws on the HBM [23,24,25], features of decision-making in pregnancy [35], clinical practice, and our research from the One Vax Two Lives social media campaign [21,22] to incorporate factors unique to pregnancy that may be helpful in designing research studies or public health communication campaigns. The 5-P model is an important beginning for further research into the factors that lead to vaccine hesitancy or acceptance in pregnancy.
Author Contributions
Conceptualization, E.C., M.S., K.T. and K.M.A.W.; methodology, E.C., M.S. and K.M.A.W.; writing—original draft preparation, E.C., M.S., K.T., C.B., I.C., E.E., B.F. and K.M.A.W.; writing—review and editing, E.C., M.S., K.T., C.B., I.C., E.E., B.F. and K.M.A.W.; supervision, E.C., M.S. and K.M.A.W.; funding acquisition, K.M.A.W. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by funding by the University of Washington Population Health Initiative and the Department of Obstetrics and Gynecology, the Washington State Obstetrical Association, and the Washington State Department of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of any of these organizations.
Data Availability Statement
No data are associated with this manuscript.
Conflicts of Interest
The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results. Kristina Adams Waldorf reported receiving consultant fees from GlaxoSmithKline. Cox, Sanchez, Taylor, Baxter, Crary, Every and Futa reported no biomedical financial interests or potential conflicts of interests.
References
- Singer, D.B.; Rudolph, A.J.; Rosenberg, H.S.; Rawls, W.E.; Boniuk, M. Pathology of the congenital rubella syndrome. J. Pediatr. 1967, 71, 665–675. [Google Scholar] [CrossRef]
- Gabrielli, L.; Bonasoni, M.P.; Santini, D.; Piccirilli, G.; Chiereghin, A.; Petrisli, E.; Dolcetti, R.; Guerra, B.; Piccioli, M.; Lanari, M.; et al. Congenital cytomegalovirus infection: Patterns of fetal brain damage. Clin. Microbiol. Infect. 2012, 18, E419–E427. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Maternal and infant outcomes among severely ill pregnant and postpartum women with 2009 pandemic influenza A (H1N1)—United States, April 2009–August 2010. MMWR Morb. Mortal. Wkly. Rep. 2011, 60, 1193–1196. [Google Scholar]
- Ellington, S.; Strid, P.; Tong, V.T.; Woodworth, K.; Galang, R.R.; Zambrano, L.D.; Nahabedian, J.; Anderson, K.; Gilboa, S.M. Characteristics of Women of Reproductive Age with Laboratory-Confirmed SARS-CoV-2 Infection by Pregnancy Status—United States, January 22–June 7, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 769–775. [Google Scholar] [CrossRef] [PubMed]
- DeSisto, C.L.; Wallace, B.; Simeone, R.M.; Polen, K.; Ko, J.Y.; Meaney-Delman, D.; Ellington, S.R. Risk for Stillbirth Among Women with and Without COVID-19 at Delivery Hospitalization—United States, March 2020–September 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 1640–1645. [Google Scholar] [CrossRef]
- Lokken, E.M.; Huebner, E.M.; Taylor, G.G.; Hendrickson, S.; Vanderhoeven, J.; Kachikis, A.; Coler, B.; Walker, C.L.; Sheng, J.S.; Al-Haddad, B.J.S.; et al. Disease Severity, Pregnancy Outcomes and Maternal Deaths among Pregnant Patients with SARS-CoV-2 Infection in Washington State. Am. J. Obstet. Gynecol. 2021, 225, 77.e1–14. [Google Scholar] [CrossRef] [PubMed]
- Lokken, E.M.; Taylor, G.G.; Huebner, E.M.; Vanderhoeven, J.; Hendrickson, S.; Coler, B.; Sheng, J.S.; Walker, C.L.; McCartney, S.A.; Kretzer, N.M.; et al. Higher severe acute respiratory syndrome coronavirus 2 infection rate in pregnant patients. Am. J. Obstet. Gynecol. 2021, 225, 75.e1–16. [Google Scholar] [CrossRef]
- Cervantes, O.; Cruz Talavera, I.; Every, E.; Coler, B.; Li, M.; Li, A.; Li, H.; Adams Waldorf, K. Role of hormones in the pregnancy and sex-specific outcomes to infections with respiratory viruses. Immunol. Rev. 2022, 308, 123–148. [Google Scholar] [CrossRef]
- Brasil, P.; Pereira, J.P., Jr.; Moreira, M.E.; Ribeiro Nogueira, R.M.; Damasceno, L.; Wakimoto, M.; Rabello, R.S.; Valderramos, S.G.; Halai, U.A.; Salles, T.S.; et al. Zika Virus Infection in Pregnant Women in Rio de Janeiro. N. Engl. J. Med. 2016, 375, 2321–2334. [Google Scholar] [CrossRef]
- Adams Waldorf, K.M.; McAdams, R.M. Influence of infection during pregnancy on fetal development. Reproduction 2013, 146, R151–R162. [Google Scholar] [CrossRef]
- Coler, B.; Cervantes, O.; Li, M.; Coler, C.; Li, A.; Shivakumar, M.; Every, E.; Schwartz, D.; Adams Waldorf, K.M. Common pathways targeted by viral hemorrhagic fever viruses to infect the placenta and increase the risk of stillbirth. Placenta 2022, S0143-4004(22)00427-1. [Google Scholar] [CrossRef]
- Schwartz, D.A.; Ha, S.; Dashraath, P.; Baud, D.; Pittman, P.R.; Waldorf, K.A. Monkeypox Virus in Pregnancy, the Placenta and Newborn: An Emerging Poxvirus with Similarities to Smallpox and Other Orthopoxvirus Agents Causing Maternal and Fetal Disease. Arch. Pathol. Lab. Med. 2023, 147, 746–757. [Google Scholar] [CrossRef]
- Prevention, U.S.C.f.D.C.a. Pregnancy and Vaccination. Available online: https://www.cdc.gov/vaccines/pregnancy/index.html (accessed on 14 May 2023).
- Razzaghi, H.; Meghani, M.; Pingali, C.; Crane, B.; Naleway, A.; Weintraub, E.; Kenigsberg, T.A.; Lamias, M.J.; Irving, S.A.; Kauffman, T.L.; et al. COVID-19 Vaccination Coverage Among Pregnant Women During Pregnancy—Eight Integrated Health Care Organizations, United States, December 14, 2020–May 8, 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 895–899. [Google Scholar] [CrossRef]
- Wainstock, T.; Yoles, I.; Sergienko, R.; Sheiner, E. Prenatal maternal COVID-19 vaccination and pregnancy outcomes. Vaccine 2021, 39, 6037–6040. [Google Scholar] [CrossRef]
- Qiu, X.; Bailey, H.; Thorne, C. Barriers and Facilitators Associated with Vaccine Acceptance and Uptake Among Pregnant Women in High Income Countries: A Mini-Review. Front. Immunol. 2021, 12, 626717. [Google Scholar] [CrossRef] [PubMed]
- Di Girolamo, R.; Khalil, A.; Rizzo, G.; Capannolo, G.; Buca, D.; Liberati, M.; Acharya, G.; Odibo, A.O.; D’Antonio, F. Systematic review and critical evaluation of quality of clinical practice guidelines on the management of SARS-CoV-2 infection in pregnancy. Am. J. Obstet. Gynecol. MFM 2022, 4, 100654. [Google Scholar] [CrossRef]
- LaCourse, S.; John-Stewart, G.; Adams Waldorf, K.M. Importance of Inclusion of Pregnant and Breastfeeding Women in COVID-19 Therapeutic Trials. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2020, 71, 879–881. [Google Scholar] [CrossRef] [PubMed]
- Rubin, R. Pregnant People’s Paradox-Excluded from Vaccine Trials Despite Having a Higher Risk of COVID-19 Complications. JAMA J. Am. Med. Assoc. 2021, 325, 1027–1028. [Google Scholar] [CrossRef] [PubMed]
- Goncu Ayhan, S.; Oluklu, D.; Atalay, A.; Menekse Beser, D.; Tanacan, A.; Moraloglu Tekin, O.; Sahin, D. COVID-19 vaccine acceptance in pregnant women. Int. J. Gynaecol. Obstet. 2021, 154, 291–296. [Google Scholar] [CrossRef] [PubMed]
- Marcell, L.; Dokania, E.; Navia, I.; Baxter, C.; Crary, I.; Rutz, S.; Soto Monteverde, M.J.; Simlai, S.; Hernandez, C.; Huebner, E.M.; et al. One Vax Two Lives: A Social Media Campaign and Research Program to Address COVID-19 Vaccine Hesitancy in Pregnancy. Am. J. Obstet. Gynecol. 2022, 227, 685–695. [Google Scholar] [CrossRef]
- Cox, E.; Sanchez, M.; Baxter, C.; Crary, I.; Every, E.; Munson, J.; Stapley, S.; Stonehill, A.; Taylor, K.; Widmann, W.; et al. COVID-19 Vaccine Hesitancy among English-Speaking Pregnant Women Living in Rural Western United States. Vaccines 2023, 11, 1108. [Google Scholar] [CrossRef] [PubMed]
- Kegeles, S.S. The Health Belief Model and Personal Health Behavior—Becker, Mh. Soc. Sci. Med. Med. Econ. 1980, 14, 227–229. [Google Scholar] [CrossRef]
- Champion, V.L.; Skinner, C.S. The health belief model. In Health Behavior: Theory, Research, and Practice; Jossey-Bass: Hoboken, NJ, USA, 2008; pp. 45–65. [Google Scholar]
- Limbu, Y.B.; Gautam, R.K.; Pham, L. The Health Belief Model Applied to COVID-19 Vaccine Hesitancy: A Systematic Review. Vaccines 2022, 10, 973. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, N.E. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef]
- Betsch, C.; Böhm, R.; Chapman, G.B. Using Behavioral Insights to Increase Vaccination Policy Effectiveness. Policy Insights Behav. Brain Sci. 2015, 2, 61–73. [Google Scholar] [CrossRef]
- Thomson, A.; Robinson, K.; Vallee-Tourangeau, G. The 5As: A practical taxonomy for the determinants of vaccine uptake. Vaccine 2016, 34, 1018–1024. [Google Scholar] [CrossRef]
- Zhang, Y.; Fisk, R.J. Barriers to vaccination for coronavirus disease 2019 (COVID-19) control: Experience from the United States. Glob. Health J. 2021, 5, 51–55. [Google Scholar] [CrossRef] [PubMed]
- Cui, Y.; Binger, K.; Palatnik, A. Attitudes and Beliefs Associated With COVID-19 Vaccination During Pregnancy. JAMA Netw. Open 2022, 5, e227430. [Google Scholar] [CrossRef]
- Simmons, L.A.; Whipps, M.D.M.; Phipps, J.E.; Satish, N.S.; Swamy, G.K. Understanding COVID-19 vaccine uptake during pregnancy: ‘Hesitance’, knowledge, and evidence-based decision-making. Vaccine 2022, 40, 2755–2760. [Google Scholar] [CrossRef]
- Rawal, S.; Tackett, R.L.; Stone, R.H.; Young, H.N. COVID-19 vaccination among pregnant people in the United States: A systematic review. Am. J. Obstet. Gynecol. MFM 2022, 4, 100616. [Google Scholar] [CrossRef]
- Bateman, L.B.; Hall, A.G.; Anderson, W.A.; Cherrington, A.L.; Helova, A.; Judd, S.; Kimberly, R.; Oates, G.R.; Osborne, T.; Ott, C.; et al. Exploring COVID-19 Vaccine Hesitancy Among Stakeholders in African American and Latinx Communities in the Deep South Through the Lens of the Health Belief Model. Am. J. Health Promot. 2022, 36, 288–295. [Google Scholar] [CrossRef] [PubMed]
- Walker, K.K.; Head, K.J.; Owens, H.; Zimet, G.D. A qualitative study exploring the relationship between mothers’ vaccine hesitancy and health beliefs with COVID-19 vaccination intention and prevention during the early pandemic months. Hum. Vaccin. Immunother. 2021, 17, 3355–3364. [Google Scholar] [CrossRef]
- Yuill, C.; McCourt, C.; Cheyne, H.; Leister, N. Women’s experiences of decision-making and informed choice about pregnancy and birth care: A systematic review and meta-synthesis of qualitative research. BMC Pregnancy Childbirth 2020, 20, 343. [Google Scholar] [CrossRef] [PubMed]
- Firouzbakht, M.; Sharif Nia, H.; Kazeminavaei, F.; Rashidian, P. Hesitancy about COVID-19 vaccination among pregnant women: A cross-sectional study based on the health belief model. BMC Pregnancy Childbirth 2022, 22, 611. [Google Scholar] [CrossRef]
- Mercadante, A.R.; Law, A.V. Will they, or Won’t they? Examining patients’ vaccine intention for flu and COVID-19 using the Health Belief Model. Res. Social. Adm. Pharm. 2021, 17, 1596–1605. [Google Scholar] [CrossRef]
- Snyder, H. Literature review as a research methodology: An overview and guidelines. J. Bus. Res. 2019, 104, 333–339. [Google Scholar] [CrossRef]
- Razzaghi, H.; Kahn, K.E.; Masalovich, S.; Black, C.L.; Nguyen, K.H.; Barfield, W.D.; Galang, R.R.; Singleton, J.A. COVID-19 Vaccination and Intent Among Pregnant Women, United States, April 2021. Public Health Rep. 2022, 137, 988–999. [Google Scholar] [CrossRef]
- KFF. Latest Data on COVID-19 Vaccinations by Race/Ethnicity. Available online: https://www.kff.org/coronavirus-covid-19/issue-brief/latest-data-on-covid-19-vaccinations-by-race-ethnicity/ (accessed on 16 July 2023).
- Abbasi, J. Widespread Misinformation About Infertility Continues to Create COVID-19 Vaccine Hesitancy. JAMA J. Am. Med. Assoc. 2022, 327, 1013–1015. [Google Scholar] [CrossRef]
- Orleans, C.T.; Johnson, R.W.; Barker, D.C.; Kaufman, N.J.; Marx, J.F. Helping pregnant smokers quit: Meeting the challenge in the next decade. West. J. Med. 2001, 174, 276–281. [Google Scholar] [CrossRef]
- Williams, J.; Myson, V.; Steward, S.; Jones, G.; Wilson, J.F.; Kerr, M.P.; Smith, P.E. Self-discontinuation of antiepileptic medication in pregnancy: Detection by hair analysis. Epilepsia 2002, 43, 824–831. [Google Scholar] [CrossRef]
- Kilpatrick, S.J.; Papile, L.-A.; Macones, G.A. (Eds.) Guidelines for Perinatal Care, 8th ed.; American Academy of Pediatrics: Elk Gove Village, IL, USA, 2017. [Google Scholar]
- Santo, L.; Kang, K. National Ambulatory Medical Care Survey: 2019 National Summary Tables. Available online: https://stacks.cdc.gov/view/cdc/123251. (accessed on 5 November 2022).
- Collins, J.; Alona, I.; Tooher, R.; Marshall, H. Increased awareness and health care provider endorsement is required to encourage pregnant women to be vaccinated. Human Vaccines Immunother. 2014, 10, 2922–2929. [Google Scholar] [CrossRef] [PubMed]
- Fleming, J.A.; Baltrons, R.; Rowley, E.; Quintanilla, I.; Crespin, E.; Ropero, A.-M.; Ortiz, J.R.; Lambach, P.; Neuzil, K.M.; Stepanchak, M.; et al. Implementation of maternal influenza immunization in El Salvador: Experiences and lessons learned from a mixed-methods study. Vaccine 2018, 36, 4054–4061. [Google Scholar] [CrossRef] [PubMed]
- Geoghegan, S.; Shuster, S.; Butler, K.M.; Feemster, K.A. Understanding Barriers and Facilitators to Maternal Immunization: A Systematic Narrative Synthesis of the Published Literature. Matern. Child. Health J. 2022, 26, 2198–2209. [Google Scholar] [CrossRef]
- Joshi, A.; Kaur, M.; Kaur, R.; Grover, A.; Nash, D.; El-Mohandes, A. Predictors of COVID-19 Vaccine Acceptance, Intention, and Hesitancy: A Scoping Review. Front. Public. Health 2021, 9, 698111. [Google Scholar] [CrossRef]
- Maness, S.B.; Buhi, E.R. Associations Between Social Determinants of Health and Pregnancy Among Young People: A Systematic Review of Research Published During the Past 25 Years. Public. Health Rep. 2016, 131, 86–99. [Google Scholar] [CrossRef]
- Backes, E.P.; Scrimshaw, S.C. (Eds.) Birth Settings in America: Outcomes, Quality, Access, and Choice; The National Academies Collection: Reports funded by National Institutes of Health; National Academies Press: Washington, DC, USA, 2020. [Google Scholar]
- Smith, S.E.; Sivertsen, N.; Lines, L.; De Bellis, A. Weighing up the risks—Vaccine decision-making in pregnancy and parenting. Women Birth 2022, 35, 547–552. [Google Scholar] [CrossRef] [PubMed]
- Bohnhoff, J.; Davis, A.; Bruine de Bruin, W.; Krishnamurti, T. COVID-19 Information Sources and Health Behaviors During Pregnancy: Results from a Prenatal App-Embedded Survey. JMIR Infodemiol. 2021, 1, e31774. [Google Scholar] [CrossRef]
- Renner, R.M.; Eden, K.B.; Osterweil, P.; Chan, B.K.; Guise, J.M. Informational factors influencing patient’s childbirth preferences after prior cesarean. Am. J. Obstet. Gynecol. 2007, 196, e14–e16. [Google Scholar] [CrossRef]
- Blakeway, H.; Prasad, S.; Kalafat, E.; Heath, P.T.; Ladhani, S.N.; Le Doare, K.; Magee, L.A.; O’Brien, P.; Rezvani, A.; von Dadelszen, P.; et al. COVID-19 vaccination during pregnancy: Coverage and safety. Am. J. Obstet. Gynecol. 2022, 226, 236.E1–236.E14. [Google Scholar] [CrossRef]
- Scendoni, R.; Fedeli, P.; Cingolani, M. The State of Play on COVID-19 Vaccination in Pregnant and Breastfeeding Women: Recommendations, Legal Protection, Ethical Issues and Controversies in Italy. Healthcare 2023, 11, 328. [Google Scholar] [CrossRef]
- Einarson, A.; Selby, P.; Koren, G. Abrupt discontinuation of psychotropic drugs during pregnancy: Fear of teratogenic risk and impact of counselling. J. Psychiatry Neurosci. 2001, 26, 44–48. [Google Scholar] [PubMed]
- Egloff, C.; Couffignal, C.; Cordier, A.G.; Deruelle, P.; Sibiude, J.; Anselem, O.; Benachi, A.; Luton, D.; Mandelbrot, L.; Vauloup-Fellous, C.; et al. Pregnant women’s perceptions of the COVID-19 vaccine: A French survey. PLoS ONE 2022, 17, e0263512. [Google Scholar] [CrossRef] [PubMed]
- Reifferscheid, L.; Marfo, E.; Assi, A.; Dube, E.; MacDonald, N.E.; Meyer, S.B.; Bettinger, J.A.; Driedger, S.M.; Robinson, J.; Sadarangani, M.; et al. COVID-19 vaccine uptake and intention during pregnancy in Canada. Can. J. Public. Health 2022, 113, 547–558. [Google Scholar] [CrossRef] [PubMed]
- Badell, M.L.; Dude, C.M.; Rasmussen, S.A.; Jamieson, D.J. COVID-19 vaccination in pregnancy. BMJ 2022, 378, e069741. [Google Scholar] [CrossRef] [PubMed]
- Bartolo, S.; Deliege, E.; Mancel, O.; Dufour, P.; Vanderstichele, S.; Roumilhac, M.; Hammou, Y.; Carpentier, S.; Dessein, R.; Subtil, D.; et al. Determinants of influenza vaccination uptake in pregnancy: A large single-Centre cohort study. BMC Pregnancy Childbirth 2019, 19, 510. [Google Scholar] [CrossRef] [PubMed]
- Redmond, M.L.; Mayes, P.; Morris, K.; Ramaswamy, M.; Ault, K.A.; Smith, S.A. Learning from maternal voices on COVID-19 vaccine uptake: Perspectives from pregnant women living in the Midwest on the COVID-19 pandemic and vaccine. J. Community Psychol. 2022, 50, 2630–2643. [Google Scholar] [CrossRef]
- Cui, Y.; Binger, K.S.; Tsaih, S.W.; Palatnik, A. Factors of COVID-19 vaccine hesitancy during pregnancy: A cross-sectional study. Am. J. Obstet. Gynecol. 2022, 226, S306. [Google Scholar] [CrossRef]
- Greyson, D.; Bettinger, J.A. How do mothers’ vaccine attitudes change over time? SSM Qual. Res. Health 2022, 2, 100060. [Google Scholar] [CrossRef]
- Raut, S.; Apte, A.; Srinivasan, M.; Dudeja, N.; Dayma, G.; Sinha, B.; Bavdekar, A. Determinants of maternal influenza vaccination in the context of low- and middle-income countries: A systematic review. PLoS ONE 2022, 17, e0262871. [Google Scholar] [CrossRef]
- Fauzia Malik, A.; Belizan, M.; Gutierrez, M.; Vilajeliu, A.; Sanclemente, L.N.; Gonzalez Casanova, I.; Jones, D.; Omer, S.; Maria Ropero, A.; Pedro Alonso, J. Pregnant women’s perspectives about maternal immunization in Latin America. Vaccine 2021, 39 (Suppl. S2), B44–B49. [Google Scholar] [CrossRef]
- Konje, J.C.; Al Beloushi, M.; Ahmed, B. Immunisation against COVID-19 in Pregnancy and of Women Planning Pregnancy. Viruses 2023, 15, 621. [Google Scholar] [CrossRef]
- Jones, A.; Wallis, D. Using the Health Belief Model to Identify Predictors of COVID-19 Vaccine Acceptance among a Sample of Pregnant Women in the U.S.: A Cross-Sectional Survey. Vaccines 2022, 10, 842. [Google Scholar] [CrossRef] [PubMed]
- Kiefer, M.K.; Mehl, R.; Costantine, M.M.; Johnson, A.; Cohen, J.; Summerfield, T.L.; Landon, M.B.; Rood, K.M.; Venkatesh, K.K. Characteristics and perceptions associated with COVID-19 vaccination hesitancy among pregnant and postpartum individuals: A cross-sectional study. BJOG 2022, 129, 1342–1351. [Google Scholar] [CrossRef] [PubMed]
- Battarbee, A.N.; Stockwell, M.S.; Varner, M.; Newes-Adeyi, G.; Daugherty, M.; Gyamfi-Bannerman, C.; Tita, A.T.; Vorwaller, K.; Vargas, C.; Subramaniam, A.; et al. Attitudes Toward COVID-19 Illness and COVID-19 Vaccination among Pregnant Women: A Cross-Sectional Multicenter Study during August–December 2020. Am. J. Perinatol. 2022, 39, 75–83. [Google Scholar] [CrossRef]
- Yudin, M.H.; Salripour, M.; Sgro, M.D. Impact of patient education on knowledge of influenza and vaccine recommendations among pregnant women. J. Obstet. Gynaecol. Can. 2010, 32, 232–237. [Google Scholar] [CrossRef]
- Manca, T.; Baylis, F.; Munoz, F.M.; Top, K.A. Prioritise research on vaccines for pregnant and breastfeeding women. Lancet 2022, 399, 890–893. [Google Scholar] [CrossRef] [PubMed]
- Kansal, N.; Weaver, K.; Vasudevan, L.; Hughes, B. Evaluating Influenza and COVID-19 Vaccine Hesitancy Among Pregnant Women Using the Health Belief Model. Am. J. Obstet. Gynecol. 2022, 226, 314. [Google Scholar] [CrossRef]
- Puri, N.; Coomes, E.A.; Haghbayan, H.; Gunaratne, K. Social media and vaccine hesitancy: New updates for the era of COVID-19 and globalized infectious diseases. Hum. Vaccines Immunother. 2020, 16, 2586–2593. [Google Scholar] [CrossRef]
- Sun, Y.; Monnat, S.M. Rural-urban and within-rural differences in COVID-19 vaccination rates. J. Rural Health 2022, 38, 916–922. [Google Scholar] [CrossRef]
- Chen, X.; Orom, H.; Hay, J.L.; Waters, E.A.; Schofield, E.; Li, Y.; Kiviniemi, M.T. Differences in Rural and Urban Health Information Access and Use. J. Rural Health 2019, 35, 405–417. [Google Scholar] [CrossRef]
- Hailemariam, S.; Mekonnen, B.; Shifera, N.; Endalkachew, B.; Asnake, M.; Assefa, A.; Qanche, Q. Predictors of pregnant women’s intention to vaccinate against coronavirus disease 2019: A facility-based cross-sectional study in southwest Ethiopia. SAGE Open Med. 2021, 9, 20503121211038454. [Google Scholar] [CrossRef] [PubMed]
- Nindrea, R.D.; Djanas, D.; Warsiti; Darma, I.Y.; Hendriyani, H.; Sari, N.P. The risk factors and pregnant women’s willingness toward the SARS-CoV-2 vaccination in various countries: A systematic review and meta-analysis. Clin. Epidemiol. Glob. Health 2022, 14, 100982. [Google Scholar] [CrossRef] [PubMed]
- Morales, D.X.; Beltran, T.F.; Morales, S.A. Gender, socioeconomic status, and COVID-19 vaccine hesitancy in the US: An intersectionality approach. Sociol. Health Illn. 2022, 44, 953–971. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).