The Burden of Streptococcus pneumoniae-Related Admissions and In-Hospital Mortality: A Retrospective Observational Study between the Years 2015 and 2022 from a Southern Italian Province
Abstract
1. Introduction
2. Materials and Methods
2.1. Coding of Streptococcus pneumoniae—Hospital Admission
- Pneumococcal Specified Pneumonias:
- ○
- 481 (Pneumococcal pneumonia);
- ○
- 482.9 (Bacterial pneumonia, unspecified) and 041.2 (Pneumococcus infection in conditions classified elsewhere and of unspecified site);
- ○
- 485 (Bronchopneumonia, organism unspecified) and 041.2 (Pneumococcus infection in conditions classified elsewhere and of unspecified site);
- ○
- 486 (Pneumonia, organism unspecified) and 041.2 (Pneumococcus infection in conditions classified elsewhere and of unspecified site).
- Unspecified Pneumonias:
- ○
- 482.9 (Bacterial pneumonia, unspecified);
- ○
- 485 (Bronchopneumonia, organism unspecified);
- ○
- 486 (Pneumonia, organism unspecified).
- Pneumonia All-cause:
- ○
- 480.x, which includes the following diagnoses:
- ▪
- 480.1 (Pneumonia due to adenovirus);
- ▪
- 480.2 (Pneumonia due to respiratory syncytial virus);
- ▪
- 480.3 (Pneumonia due to parainfluenza virus);
- ▪
- 480.8 (Pneumonia due to SARS-associated coronavirus);
- ▪
- 480.9 (Pneumonia due to other virus not elsewhere classified).
- ○
- 481 (Pneumococcal pneumonia);
- ○
- 482.x which includes the following diagnoses:
- ▪
- 482.0 (Pneumonia due to Klebsiella pneumoniae);
- ▪
- 482.1 (Pneumonia due to Pseudomonas);
- ▪
- 482.2 (Pneumonia due to Hemophilus influenzae (H. influenzae));
- ▪
- 482.30 (Pneumonia due to Streptococcus, unspecified);
- ▪
- 482.31 (Pneumonia due to Streptococcus, group A);
- ▪
- 482.32 (Pneumonia due to Streptococcus, group B);
- ▪
- 482.39 (Pneumonia due to other Streptococcus);
- ▪
- 482.40 (Pneumonia due to Staphylococcus, unspecified);
- ▪
- 482.41 (Methicillin susceptible pneumonia due to Staphylococcus aureus);
- ▪
- 482.42 (Methicillin resistant pneumonia due to Staphylococcus aureus);
- ▪
- 482.49 (Other Staphylococcus pneumonia);
- ▪
- 482.81 (Pneumonia due to anaerobes);
- ▪
- 482.82 (Pneumonia due to escherichia coli (E. coli));
- ▪
- 482.83 (Pneumonia due to other Gram-negative bacteria);
- ▪
- 482.84 (Pneumonia due to Legionnaires’ disease);
- ▪
- 482.89 (Pneumonia due to other specified bacteria);
- ▪
- 482.9 (Bacterial pneumonia, unspecified).
- ○
- 483.x which includes the following diagnoses:
- ▪
- 483.0 (Pneumonia due to Mycoplasma pneumoniae);
- ▪
- 483.1 (Pneumonia due to chlamydia);
- ▪
- 483.8 (Pneumonia due to other specified organism).
- ○
- 484.x which includes the following diagnoses:
- ▪
- 484.1 (Pneumonia in cytomegalic inclusion disease,);
- ▪
- 484.3 (Pneumonia in whooping cough);
- ▪
- 484.5 (Pneumonia in anthrax);
- ▪
- 484.6 (Pneumonia in aspergillosis);
- ▪
- 484.7 (Pneumonia in other systemic mycoses);
- ▪
- 484.8 (Pneumonia in other infectious diseases classified elsewhere).
- ○
- 485 (Bronchopneumonia, organism unspecified);
- ○
- 486 (Pneumonia, organism unspecified);
- ○
- 487.0 (Influenza with pneumonia).
- Pneumococcal Specified Meningitis:
- ○
- 320.1 (Pneumococcal meningitis);
- ○
- 320.2 (Streptococcal meningitis) and 041.2 (Pneumococcus infection in conditions classified elsewhere and of unspecified site);
- ○
- 320.82 (Meningitis due to Gram-negative bacteria, not elsewhere classified) and 041.2 (Pneumococcus infection in conditions classified elsewhere and of unspecified site);
- ○
- 320.9 (Meningitis due to unspecified bacterium) and 041.2 (Pneumococcus infection in conditions classified elsewhere and of unspecified site);
- ○
- 322.9 (Meningitis, unspecified) and 041.2 (Pneumococcus infection in conditions classified elsewhere and of unspecified site).
- Unspecified Meningitis:
- ○
- 320.2 (Streptococcal meningitis);
- ○
- 320.82 (Meningitis due to Gram-negative bacteria, not elsewhere classified);
- ○
- 320.9 (Meningitis due to unspecified bacterium).
- Pneumococcal Specified Bacteriemia:
- ○
- 038.2 (Pneumococcal septicemia (Streptococcus pneumoniae septicemia));
- ○
- 038.0 (Streptococcal septicemia) and 041.2 (Pneumococcus infection in conditions classified elsewhere and of unspecified site);
- ○
- 038.9 (Unspecified septicemia) and 041.2 (Pneumococcus infection in conditions classified elsewhere and of unspecified site);
- ○
- 790.7 (Bacteremia) and 041.2 (Pneumococcus infection in conditions classified elsewhere and of unspecified site).
- Unspecified Bacteriemia:
- ○
- 038.0 (Streptococcal septicemia);
- ○
- 038.9 (Unspecified septicemia);
- ○
- 790.7 (Bacteremia).
2.2. Comorbidity Coding
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- File, T.M., Jr.; Marrie, T.J. Burden of community-acquired pneumonia in North American adults. Postgrad. Med. 2010, 122, 130–141. [Google Scholar] [CrossRef] [PubMed]
- WHO. Pneumococcal Disease. Available online: https://www.who.int/teams/health-product-policy-and-standards/standards-and-specifications/vaccine-standardization/pneumococcal-disease (accessed on 31 May 2023).
- EpiCentro. Epidemiological Data in Italy. Available online: https://www.epicentro.iss.it/en/invasive-bacterial-diseases/epidemiology-italy (accessed on 31 May 2023).
- Asner, S.A.; Agyeman, P.K.A.; Gradoux, E.; Posfay-Barbe, K.M.; Heininger, U.; Giannoni, E.; Crisinel, P.A.; Stocker, M.; Bernhard-Stirnemann, S.; Niederer-Loher, A.; et al. Burden of Streptococcus Pneumoniae Sepsis in Children After Introduction of Pneumococcal Conjugate Vaccines: A Prospective Population-Based Cohort Study. Clin. Infect. Dis. 2019, 69, 1574–1580. [Google Scholar] [CrossRef] [PubMed]
- Fletcher, M.; Laufer, D.; McIntosh, E.; Cimino, C.; Malinoski, F. Controlling Invasive Pneumococcal Disease: Is Vaccination of at-Risk Groups Sufficient? Int. J. Clin. Pract. 2006, 60, 450–456. [Google Scholar] [CrossRef] [PubMed][Green Version]
- McIntosh, E.D.G.; Fritzell, B.; Fletcher, M.A. Burden of Paediatric Invasive Pneumococcal Disease in Europe, 2005. Epidemiol. Infect. 2007, 135, 644–656. [Google Scholar] [CrossRef]
- Hausdorff, W.P.; Bryant, J.; Paradiso, P.R.; Siber, G.R. Which Pneumococcal Serogroups Cause the Most Invasive Disease: Implications for Conjugate Vaccine Formulation and Use, Part I. Clin. Infect. Dis. 2000, 30, 100–121. [Google Scholar] [CrossRef]
- Isaacman, D.J.; McIntosh, E.D.; Reinert, R.R. Burden of Invasive Pneumococcal Disease and Serotype Distribution among Streptococcus Pneumoniae Isolates in Young Children in Europe: Impact of the 7-Valent Pneumococcal Conjugate Vaccine and Considerations for Future Conjugate Vaccines. Int. J. Infect. Dis. 2010, 14, e197–e209. [Google Scholar] [CrossRef]
- Amodio, E.; Costantino, C.; Boccalini, S.; Tramuto, F.; Maida, C.M.; Vitale, F. Estimating the Burden of Hospitalization for Pneumococcal Pneumonia in a General Population Aged 50 Years or Older and Implications for Vaccination Strategies. Hum. Vaccines Immunother. 2014, 10, 1337–1342. [Google Scholar] [CrossRef][Green Version]
- Welte, T.; Torres, A.; Nathwani, D. Clinical and Economic Burden of Community-Acquired Pneumonia among Adults in Europe. Thorax 2012, 67, 71–79. [Google Scholar] [CrossRef]
- Weycker, D.; Strutton, D.; Edelsberg, J.; Sato, R.; Jackson, L.A. Clinical and Economic Burden of Pneumococcal Disease in Older US Adults. Vaccine 2010, 28, 4955–4960. [Google Scholar] [CrossRef]
- Di Martino, G.; Di Giovanni, P.; Cedrone, F.; D’Addezio, M.; Meo, F.; Scampoli, P.; Romano, F.; Staniscia, T. The Burden of Diabetes-Related Preventable Hospitalization: 11-Year Trend and Associated Factors in a Region of Southern Italy. Healthcare 2021, 9, 997. [Google Scholar] [CrossRef]
- Di Martino, G.; Cedrone, F.; Di Giovanni, P.; Tognaccini, L.; Trebbi, E.; Romano, F.; Staniscia, T. The Burden of HPV-Related Hospitalizations: Analysis of Hospital Discharge Records from the Years 2015-2021 from a Southern Italian Region. Pathogens 2023, 12, 725. [Google Scholar] [CrossRef] [PubMed]
- Baldo, V.; Cocchio, S.; Lazzari, R.; Furlan, P.; Bertoncello, C.; Russo, F.; Saia, M.; Baldovin, T. Estimated Hospitalization Rate for Diseases Attributable to Streptococcus Pneumoniae in the Veneto Region of North-East Italy. Prev. Med. Rep. 2015, 2, 27–31. [Google Scholar] [CrossRef]
- Guo, J.; Zhang, H.; Zhang, H.; Lai, X.; Wang, J.; Feng, H.; Fang, H. Cost-Effectiveness of Pneumococcal Vaccines among Adults Aged 65 Years and Older in China: A Comparative Study. Vaccine 2023, 41, 716–723. [Google Scholar] [CrossRef]
- Syeed, M.S.; Ghule, P.; Le, L.M.; Veettil, S.K.; Horn, E.K.; Perdrizet, J.; Wasserman, M.; Thakkinstian, A.; Chaiyakunapruk, N. Pneumococcal Vaccination in Children: A Systematic Review and Meta-Analysis of Cost-Effectiveness Studies. Value Health 2023, 26, 598–611. [Google Scholar] [CrossRef]
- Cedrone, F.; Di Martino, G.; Di Giovanni, P.; Greco, E.; Trebbi, E.; Romano, F.; Staniscia, T. Reduction in Hospital Admissions for Cardiovascular Diseases (CVDs) during the Coronavirus Disease 2019 (COVID-19) Pandemic: A Retrospective Study from a Southern Italian Region in the Year 2020. Healthcare 2022, 10, 871. [Google Scholar] [CrossRef] [PubMed]
- Di Martino, G.; Cedrone, F.; Di Giovanni, P.; Romano, F.; Staniscia, T. Impact of COVID-19 Pandemic on Oncological Surgery Activities: A Retrospective Study from a Southern Italian Region. Healthcare 2022, 10, 2329. [Google Scholar] [CrossRef]
- Ferreira-Coimbra, J.; Sarda, C.; Rello, J. Burden of Community-Acquired Pneumonia and Unmet Clinical Needs. Adv. Ther. 2020, 37, 1302–1318. [Google Scholar] [CrossRef] [PubMed]
- Hespanhol, V.; Bárbara, C. Pneumonia Mortality, Comorbidities Matter? Pulmonology 2020, 26, 123–129. [Google Scholar] [CrossRef]
- Barmanray, R.D.; Cheuk, N.; Fourlanos, S.; Greenberg, P.B.; Colman, P.G.; Worth, L.J. In-Hospital Hyperglycemia but Not Diabetes Mellitus Alone Is Associated with Increased in-Hospital Mortality in Community-Acquired Pneumonia (CAP): A Systematic Review and Meta-Analysis of Observational Studies Prior to COVID-19. BMJ Open Diabetes Res. Care 2022, 10, e002880. [Google Scholar] [CrossRef]
- Di Giovanni, P.; Di Martino, G.; Cedrone, F.; Meo, F.; Scampoli, P.; Romano, F.; Staniscia, T. Total Parenteral Nutrition Is Associated with Worse Hospital Outcomes among Elderly Diabetic Patients: A Propensity Score Matched Analysis on Discharge Records. Clin. Ther. 2022, 173, 115–120. [Google Scholar] [CrossRef]
- Di Giovanni, P.; Di Martino, G.; Zecca, I.A.L.; Porfilio, I.; Romano, F.; Staniscia, T. Predictors of Prolonged Hospitalization and In-Hospital Mortality After Hip Fracture: A Retrospective Study on Discharge Registry. Ann. Ig. 2022, 34, 467–477. [Google Scholar] [CrossRef]
- Ko, F.C. Preoperative Frailty Evaluation: A Promising Risk-stratification Tool in Older Adults Undergoing General Surgery. Clin Ther. 2019, 41, 387–399. [Google Scholar] [CrossRef]
- Jacob, B.; Stock, D.; Chan, V.; Colantonio, A.; Cullen, N. Predictors of in-hospital mortality following hypoxic-ischemic brain injury: A population-based study. Brain Inj. 2020, 34, 178–186. [Google Scholar] [CrossRef]
- Amodio, E.; Vitale, F.; d’Angela, D.; Carrieri, C.; Polistena, B.; Spandonaro, F.; Pagliaro, A.; Montuori, E.A. Increased Risk of Hospitalization for Pneumonia in Italian Adults from 2010 to 2019: Scientific Evidence for a Call to Action. Vaccines 2023, 11, 187. [Google Scholar] [CrossRef] [PubMed]
- Yamana, H.; Ono, S.; Michihata, N.; Uemura, K.; Jo, T.; Yasunaga, H. Effect of the 23-Valent Pneumococcal Polysaccharide Vaccine on the Incidence of Hospitalization with Pneumonia in Adults Aged ≥65 Years: Retrospective Cohort Study Using a Population-Based Database in Japan. Clin. Microbiol. Infect. 2023, 29, 904–910. [Google Scholar] [CrossRef] [PubMed]
- Paynter, J.; Howe, A.S.; Best, E.; Petousis-Harris, H. A Retrospective Cohort Study Investigating the Comparative Effectiveness of Pneumococcal Vaccines against Hospitalisation with Otitis Media and Pneumonia in New Zealand. Vaccine 2023, 41, 4121–4128. [Google Scholar] [CrossRef] [PubMed]

| (a) | Overall | % | All Pneumonia | % | S.P. Pneumonia | % | Unspecified Pneumonia | % |
|---|---|---|---|---|---|---|---|---|
| 288,110 | 14,506 | 5.035 | 7906 | 2.744 | 1673 | 0.581 | ||
| M | 140,699 | 49 | 8234 | 57 | 4351 | 55 | 1058 | 63 |
| F | 147,411 | 51 | 6272 | 43 | 3555 | 45 | 615 | 37 |
| 0–4 | 46,954 | 16 | 2508 | 17 | 1791 | 23 | 335 | 20 |
| 5–14 | 13,963 | 5 | 268 | 2 | 216 | 3 | 9 | 1 |
| 15–64 | 121,582 | 42 | 3651 | 25 | 1444 | 18 | 348 | 21 |
| 65–79 | 68,508 | 24 | 4157 | 29 | 2184 | 28 | 485 | 29 |
| 80+ | 37,103 | 13 | 3922 | 27 | 2271 | 29 | 496 | 30 |
| 2015 | 39,225 | 14 | 1205 | 8 | 842 | 11 | 268 | 16 |
| 2016 | 38,804 | 13 | 1230 | 8 | 990 | 13 | 143 | 9 |
| 2017 | 37,255 | 13 | 1468 | 10 | 1185 | 15 | 184 | 11 |
| 2018 | 36,961 | 13 | 1537 | 11 | 1158 | 15 | 230 | 14 |
| 2019 | 37,119 | 13 | 1570 | 11 | 1226 | 16 | 183 | 11 |
| 2020 | 30,166 | 10 | 2561 | 18 | 1056 | 13 | 172 | 10 |
| 2021 | 33,240 | 12 | 2619 | 18 | 779 | 10 | 144 | 9 |
| 2022 | 35,340 | 12 | 2316 | 16 | 670 | 8 | 349 | 21 |
| 0 | 192,088 | 67 | 7432 | 51 | 3539 | 45 | 898 | 54 |
| 1 | 59,573 | 21 | 4787 | 33 | 2809 | 36 | 549 | 33 |
| 2+ | 36,449 | 13 | 2287 | 16 | 1558 | 20 | 226 | 14 |
| Y | 13,434 | 5 | 3060 | 21 | 1686 | 21 | 457 | 27 |
| N | 274,676 | 95 | 11,446 | 79 | 6220 | 79 | 1216 | 73 |
| (b) | S.P. Mening. | % | S.P. Bacteremia | % | Unspecified Bacteremia | % | ||
| 33 | 0.011 | 88 | 0.031 | 5 | 0.002 | |||
| M | 16 | 48 | 57 | 65 | 4 | 80 | ||
| F | 17 | 52 | 31 | 35 | 1 | 20 | ||
| 0–4 | 3 | 9 | 13 | 15 | 0 | 0 | ||
| 5–14 | 1 | 3 | 5 | 6 | 1 | 20 | ||
| 15–64 | 17 | 52 | 38 | 43 | 4 | 80 | ||
| 65–79 | 10 | 30 | 23 | 26 | 0 | 0 | ||
| 80+ | 2 | 6 | 9 | 10 | 0 | 0 | ||
| 2015 | 4 | 12 | 5 | 6 | 0 | 0 | ||
| 2016 | 2 | 6 | 6 | 7 | 0 | 0 | ||
| 2017 | 10 | 30 | 6 | 7 | 0 | 0 | ||
| 2018 | 3 | 9 | 1 | 1 | 1 | 20 | ||
| 2019 | 3 | 9 | 24 | 27 | 2 | 40 | ||
| 2020 | 3 | 9 | 13 | 15 | 0 | 0 | ||
| 2021 | 1 | 3 | 16 | 18 | 1 | 20 | ||
| 2022 | 7 | 21 | 17 | 19 | 1 | 20 | ||
| 0 | 20 | 61 | 64 | 73 | 0 | 0 | ||
| 1 | 12 | 36 | 17 | 19 | 2 | 40 | ||
| 2+ | 1 | 3 | 7 | 8 | 3 | 60 | ||
| Y | 3 | 9 | 8 | 9 | 1 | 20 | ||
| N | 30 | 91 | 80 | 91 | 4 | 80 |
| Odds Ratio | IC 95% | p | ||
|---|---|---|---|---|
| AGE | 0–4 | 4.786 | 4.494–5.098 | <0.001 |
| 5–14 | 0.153 | 0.101–0.234 | <0.001 | |
| 65–79 | 2.868 | 2.698–3.049 | <0.001 | |
| 80+ | 6.599 | 6.207–7.015 | <0.001 | |
| SEX | 0.987 | 0.951–1.024 | 0.480 | |
| Invasive Bacterial Disease | SP Pneumonia | 4.528 | 4.257–4.816 | <0.001 |
| Unspecified Pneumonia | 7.098 | 6.304–7.991 | <0.001 | |
| SP meningitidis | 3.443 | 1.012–11.716 | 0.048 | |
| Unspecified meningitidis | (omitted) | |||
| SP Bacteraemia | 2.201 | 1.001–4.837 | 0.050 | |
| Unspecified Bacteraemia | 4.052 | 0.418–39.245 | 0.227 | |
| Comorbidity (Charlson) | Myocardial Infarction | 1.140 | 1.024–1.269 | 0.017 |
| Chronic Heart Failure | 2.333 | 2.221–2.451 | <0.001 | |
| Periferal Vascular Disease | 1.217 | 1.083–1.367 | 0.001 | |
| Cerebro-vascular Disease | 2.483 | 2.360–2.611 | <0.001 | |
| Dementia | 2.302 | 2.096–2.529 | <0.001 | |
| CPD | 0.931 | 0.866–1.001 | 0.054 | |
| Rheumatologic disease | 0.567 | 0.433–0.741 | <0.001 | |
| Peptic Ulcer | 1.520 | 1.187–1.947 | 0.001 | |
| Mild Liver Disease | 1.990 | 1.787–2.217 | <0.001 | |
| Diabetes without complication | 1.104 | 1.039–1.172 | 0.001 | |
| Diabetes complicated | 1.113 | 0.921–1.344 | 0.267 | |
| Plegia | 1.234 | 0.920–1.654 | 0.160 | |
| Renal Disease | 2.051 | 1.933–2.176 | <0.001 | |
| Any malignancy | 2.040 | 1.914–2.175 | <0.001 | |
| Liver Disease | 3.666 | 3.394–3.959 | <0.001 | |
| HIV | (omitted) | |||
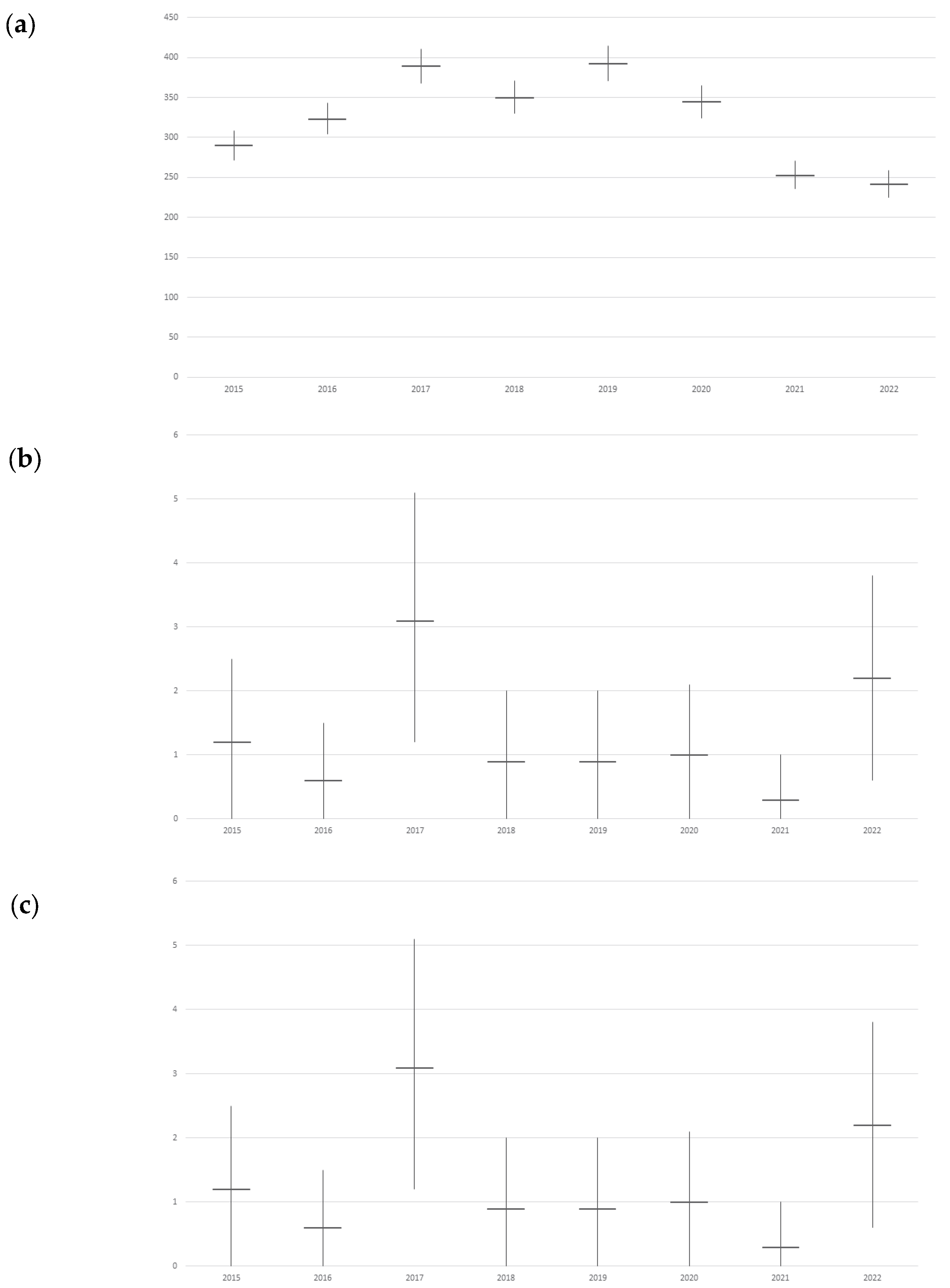
| (a) | Streptococcus pneumoniae Admission Rate | |||||||
|---|---|---|---|---|---|---|---|---|
| All | IC 95% | Pneumonia | IC 95% | Meningitis | IC 95% | Bacteremia | IC 95% | |
| 2015 | 343.3 | 323.2–363.4 | 290.3 | 271.8–308.8 | 1.2 | 0–2.5 | 1.5 | 0.4–2.5 |
| 2016 | 388.4 | 366.9–409.8 | 323.6 | 304.0–343.1 | 0.6 | 0–1.5 | 1.9 | 0.4–3.4 |
| 2017 | 469.5 | 446–493.1 | 389.3 | 367.9–410.8 | 3.1 | 1.2–5.1 | 1.9 | 0.4–3.4 |
| 2018 | 443.9 | 421–466.8 | 350.5 | 330.2–370.8 | 0.9 | 0–2.0 | 0.3 | 0–0.8 |
| 2019 | 501.1 | 476.6–525.6 | 392.4 | 370.7–414.0 | 0.9 | 0–2.0 | 7.6 | 4.5–10.6 |
| 2020 | 446.1 | 423.1–469.1 | 344.8 | 324.6–365.1 | 1.0 | 0–2.1 | 4.1 | 1.9–6.3 |
| 2021 | 381.7 | 360.5–402.9 | 253.1 | 235.9–270.4 | 0.3 | 0–1.0 | 5.0 | 2.6–7.5 |
| 2022 | 361.4 | 340.7–382 | 241.9 | 225.0–258.7 | 2.2 | 0.6–3.8 | 5.3 | 2.8–7.9 |
| (b) | Streptococcus pneumoniae In-Hospital Death Rate | |||||||
| All | IC 95% | Pneumonia | IC 95% | Meningitis | IC 95% | Bacteremia | IC 95% | |
| 2015 | 61.3 | 52.8–69.9 | 45.9 | 38.5–53.2 | 0 | - | 0 | - |
| 2016 | 61.6 | 53.0–70.1 | 54.5 | 46.4–62.6 | 0 | - | 0 | - |
| 2017 | 77.2 | 67.6–86.8 | 73.1 | 63.7–82.4 | 0 | - | 0 | - |
| 2018 | 71.1 | 61.9–80.4 | 67.8 | 58.8–76.9 | 0.6 | 0–1.4 | 0.3 | 0–0.8 |
| 2019 | 76.6 | 65.7–84.7 | 76.4 | 66.9–86.0 | 0 | - | 0.6 | 0–1.4 |
| 2020 | 150.9 | 137.6–164.2 | 79.2 | 69.5–88.9 | 0 | - | 0.3 | 0–0.9 |
| 2021 | 127.5 | 115.4–139.7 | 63.7 | 55.1–72.2 | 0 | - | 0.6 | 0–1.5 |
| 2022 | 111.9 | 100.4–123.3 | 57.9 | 49.7–66.2 | 0 | - | 0.6 | 0–1.5 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cedrone, F.; Montagna, V.; Del Duca, L.; Camplone, L.; Mazzocca, R.; Carfagnini, F.; Fortunato, V.; Di Martino, G. The Burden of Streptococcus pneumoniae-Related Admissions and In-Hospital Mortality: A Retrospective Observational Study between the Years 2015 and 2022 from a Southern Italian Province. Vaccines 2023, 11, 1324. https://doi.org/10.3390/vaccines11081324
Cedrone F, Montagna V, Del Duca L, Camplone L, Mazzocca R, Carfagnini F, Fortunato V, Di Martino G. The Burden of Streptococcus pneumoniae-Related Admissions and In-Hospital Mortality: A Retrospective Observational Study between the Years 2015 and 2022 from a Southern Italian Province. Vaccines. 2023; 11(8):1324. https://doi.org/10.3390/vaccines11081324
Chicago/Turabian StyleCedrone, Fabrizio, Vincenzo Montagna, Livio Del Duca, Laura Camplone, Riccardo Mazzocca, Federica Carfagnini, Valterio Fortunato, and Giuseppe Di Martino. 2023. "The Burden of Streptococcus pneumoniae-Related Admissions and In-Hospital Mortality: A Retrospective Observational Study between the Years 2015 and 2022 from a Southern Italian Province" Vaccines 11, no. 8: 1324. https://doi.org/10.3390/vaccines11081324
APA StyleCedrone, F., Montagna, V., Del Duca, L., Camplone, L., Mazzocca, R., Carfagnini, F., Fortunato, V., & Di Martino, G. (2023). The Burden of Streptococcus pneumoniae-Related Admissions and In-Hospital Mortality: A Retrospective Observational Study between the Years 2015 and 2022 from a Southern Italian Province. Vaccines, 11(8), 1324. https://doi.org/10.3390/vaccines11081324








