The Protective Efficacy of Single-Dose Nasal Immunization with Cold-Adapted Live-Attenuated MERS-CoV Vaccine against Lethal MERS-CoV Infections in Mice
Abstract
:1. Introduction
2. Materials and Methods
2.1. The Mouse and Virus
2.2. Generation of Cold-Adapted Live-Attenuated MERS-CoV Vaccine Virus
2.3. Sensitivity of Attenuated MERS-CoV Vaccine Virus to the Temperature
2.4. Quantification of Plaque-Forming Units (pfu)
2.5. Estimation of Viral Titers by log10TCID50/mL
2.6. Attenuation Confirmation of Live-Attenuated MERS-CoV Vaccine Virus in Animal
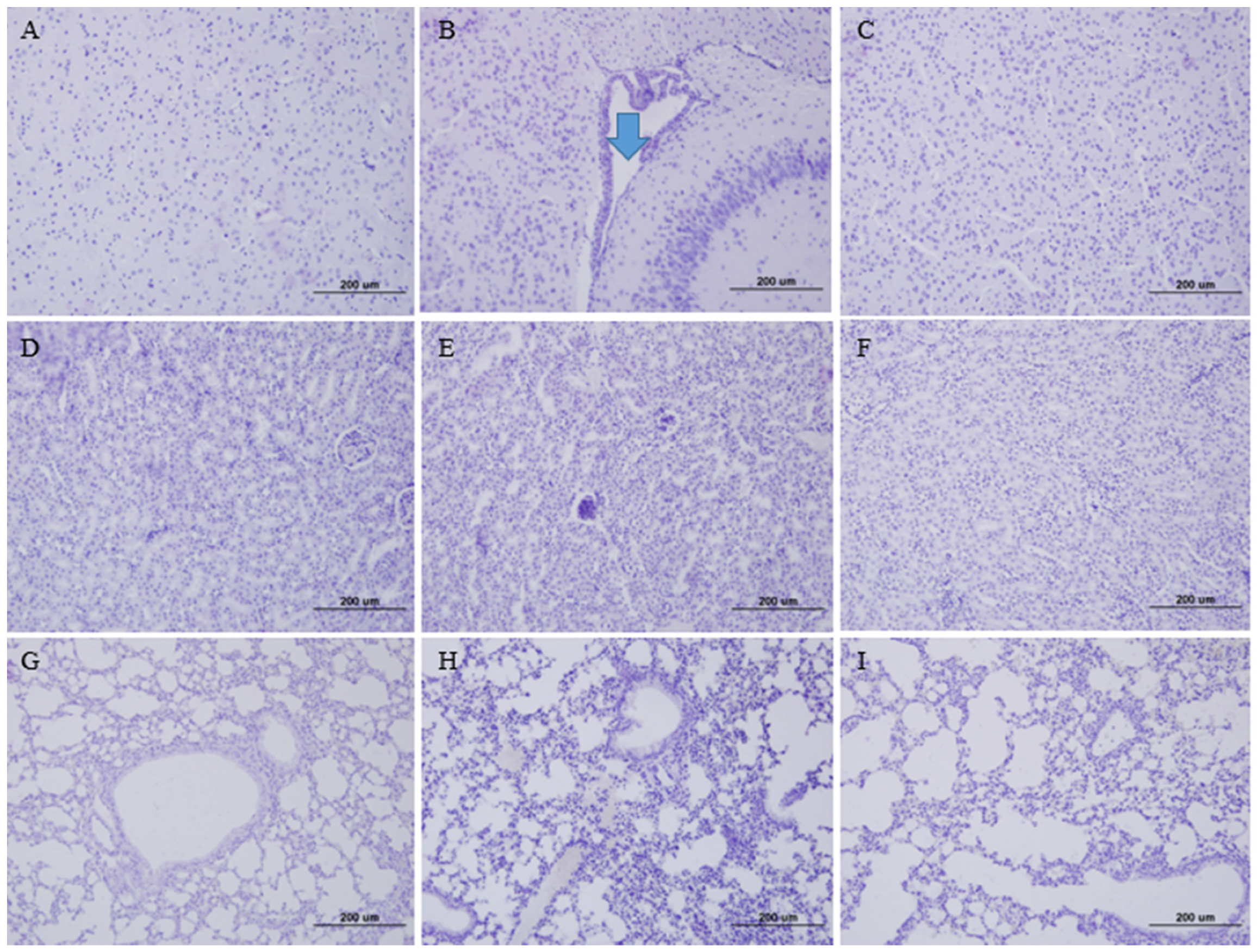
2.7. Tissue Staining with Hematoxylin and Eosin
2.8. Vaccine Efficacy in K18-hDPP4 Mice
2.9. Viral Neutralizing Antibody Titers
2.10. Determining Lymphocytes Expressing Mouse IFN–γ
2.11. Detection of Mouse Cytokines, TNF-α, IL-4, and IL-10, in Spleen Lymphocytes Using Enzyme-Linked Immunosorbent Assay
2.12. Measurement of MERS-CoV-Specific IgA Antibody in Tissues of Vaccinated Mice
2.13. Genome Decoding of Live-Attenuated MERS-CoV Vaccine Virus
2.14. Ethical Approval
2.15. Statistical Analysis
3. Results
3.1. Development of Live-Attenuated MERS-CoV Vaccine Virus by Cold Adaptation
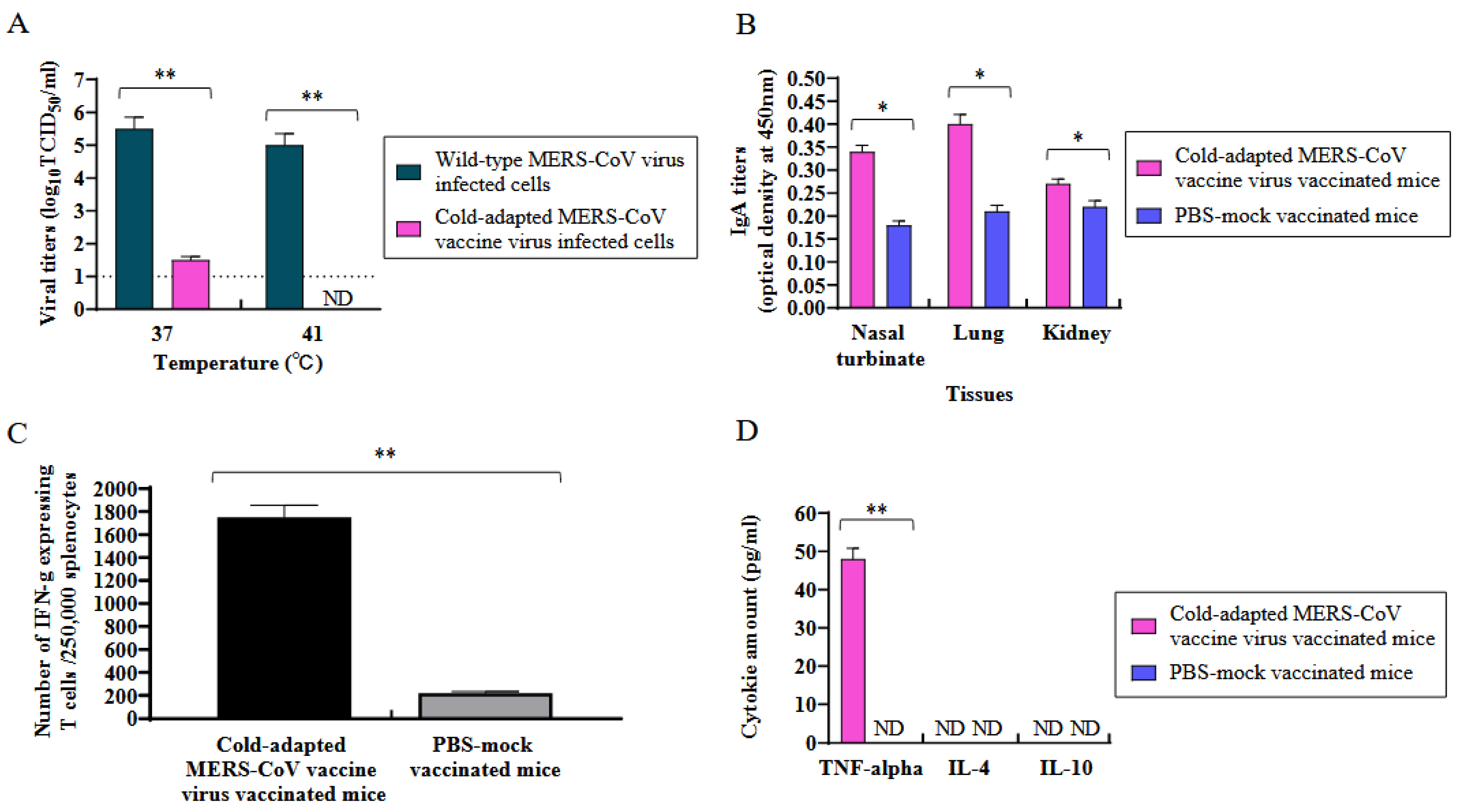
3.2. Temperature Sensitivity of Cold-Adapted MERS-CoV Vaccine Strain
3.3. Induction of Mucosal Antibody (IgA) in the Tissues of K18-hDPP4 Mice Immunized with Cold-Adapted MERS-CoV Vaccine Strain
3.4. Induction of Cellular Immunity and Th1-Type Specific Cytokines in Spleen Lymphocytes of K18-hDPP4 Mice Immunized with Cold-Adapted Attenuated MERS-CoV Vaccine Strain
3.5. Measurement of Th1 and Th2 Cytokines
3.6. Protection of K18-hDPP4 Mice Immunized by Cold-Adapted MERS-CoV Vaccine Strain
3.7. Decoding the Genome Sequence of the Cold-Adapted Live-Attenuated MERS-CoV Vaccine Strain
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zaki, A.M.; Boheemen, S.V.; Bestebroer, T.M.; Osterhaus, A.D.M.E.; Fouchier, R.A.M. Isolation of a Novel Coronavirus from a Man with Pneumonia in Saudi Arabia. N. Engl. J. Med. 2012, 367, 1814–1820. [Google Scholar] [CrossRef]
- Memish, Z.A.; Perlman, S.; Kerkhove, M.D.V.; Zumla, A. Middle East respiratory syndrome. Lancet 2020, 395, 1063–1077. [Google Scholar] [CrossRef] [PubMed]
- Drosten, C.; Seilmaier, M.; Corman, V.M.; Hartmann, W.; Scheible, G.; Sack, S.; Guggemos, W.; Kallies, R.; Muth, D.; Junglen, S.; et al. Clinical features and virological analysis of a case of Middle East respiratory syndrome coronavirus infection. Lancet Infect. Dis. 2013, 13, 745–751. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Middle East Respiratory Syndrome Coronavirus (MERS-CoV). Available online: https://www.who.int/news-room/fact-sheets/detail/middle-east-respiratory-syndrome-coronavirus-(mers-cov)?gclid=CjwKCAiAnZCdBhBmEiwA8nDQxaji4hmfA9dt-Wxc-JENLvYiCJqqew82QMxRCo2A8LaczJZderBaWBoCg4YQAvD_BwE (accessed on 22 December 2022).
- Wang, Q.; Qi, J.; Yuan, Y.; Xuan, Y.; Han, P.; Wan, Y.; Ji, W.; Li, Y.; Wu, Y.; Wang, J.; et al. Bat origins of MERS-CoV supported by bat coronavirus HKU4 usage of human receptor CD26. Cell Host Microbe 2014, 16, 328–337. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, Y.; Du, L.; Liu, C.; Li, F. Receptor usage and cell entry of bat coronavirus HKU4 provide insight into bat-to-human transmission of MERS coronavirus. Proc. Natl. Acad. Sci. USA 2014, 111, 12516–12521. [Google Scholar] [CrossRef]
- Azhar, E.I.; El-Kafrawy, S.A.; Farraj, S.A.; Hassan, A.M.; Al-Saeed, M.S.; Hashem, A.M.; Madani, T.A. Evidence for camel-to-human transmission of MERS coronavirus. N. Engl. J. Med. 2014, 370, 2499–2505. [Google Scholar] [CrossRef]
- Conzade, R.; Grant, R.; Malik, M.R.; Elkholy, A.; Elhakim, M.; Samhouri, D.; Embarek, P.K.B.; Kerkhove, M.D.V. Reported Direct and Indirect Contact with Dromedary Camels among Laboratory-Confirmed MERS-CoV Cases. Viruses 2018, 10, 425. [Google Scholar] [CrossRef] [Green Version]
- Paden, C.R.; Yusof, M.F.B.M.; Al Hammadi, Z.M.; Queen, K.; Tao, Y.; Eltahir, Y.M.; Elsayed, E.A.; Marzoug, B.A.; Bensalah, O.K.A.; Khalafalla, A.I.; et al. Zoonotic origin and transmission of Middle East respiratory syndrome coronavirus in the UAE. Zoonoses Public Health 2018, 65, 322–333. [Google Scholar] [CrossRef]
- Alfaraj, S.H.; Al-Tawfiq, J.A.; Altuwaijri, T.A.; Alanazi, M.; Alzahrani, N.; Memish, Z.A. Middle East respiratory syndrome coronavirus transmission among health care workers: Implication for infection control. Am. J. Infect. Control 2018, 46, 165–168. [Google Scholar] [CrossRef]
- Bailey-Elkin, B.A.; Knaap, R.C.M.; Johnson, G.G.; Dalebout, T.J.; Ninaber, D.K.; Kasteren, P.B.V.; Bredenbeek, P.J.; Snijder, E.J.; Kikkert, M.; Mark, B.L. Crystal structure of the Middle East respiratory syndrome coronavirus (MERS-CoV) papain-like protease bound to ubiquitin facilitates targeted disruption of deubiquitinating activity to demonstrate its role in innate immune suppression. J. Biol. Chem. 2014, 289, 34667–34682. [Google Scholar] [CrossRef] [Green Version]
- Fehr, A.R.; Perlman, S. Coronaviruses: An overview of their replication and pathogenesis. Methods Mol. Biol. 2015, 1282, 1–23. [Google Scholar] [PubMed] [Green Version]
- Snijder, E.J.; Decroly, E.; Ziebuhr, J. The Nonstructural Proteins Directing Coronavirus RNA Synthesis and Processing. Adv. Virus Res. 2016, 96, 59–126. [Google Scholar] [PubMed]
- Chena, Y.; Rajashankarb, K.R.; Yanga, Y.; Agnihothramc, S.S.; Liua, C.; Lina, Y.L.; Baricc, R.S.; Lia, F. Crystal Structure of the Receptor-Binding Domain from Newly Emerged Middle East Respiratory Syndrome Coronavirus. J. Virol. 2013, 87, 10777–10783. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Raj, V.S.; Mou, H.; Smits, S.L.; Dekkers, D.H.; Müller, M.A.; Dijkman, R.; Muth, D.; Demmers, J.A.; Zaki, A.; Fouchier, R.A.; et al. Dipeptidyl peptidase 4 is a functional receptor for the emerging human coronavirus-EMC. Nature 2013, 495, 251–254. [Google Scholar] [CrossRef] [Green Version]
- Modjarrad, K.; Roberts, C.C.; Mills, K.T.; Castellano, A.R.; Paolino, K.; Muthumani, K.; Reuschel, E.L.; Robb, M.L.; Racine, T.; Oh, M.D.; et al. Safety and immunogenicity of an anti-Middle East respiratory syndrome coronavirus DNA vaccine: A phase 1, open-label, single-arm, dose-escalation trial. Lancet Infect. Dis. 2019, 9, 1013–1022. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bosaeed, M.; Balkhy, H.H.; Almaziad, S.; Aljami, H.A.; Alhatmi, H.; Alanazi, H.; Alahmadi, M.; Jawhary, A.; Alenazi, M.W.; Almasoud, A.; et al. Safety and immunogenicity of ChAdOx1 MERS vaccine candidate in healthy Middle Eastern adults (MERS002): An open-label, non-randomised, dose-escalation, phase 1b trial. Lancet Microbe 2022, 3, e11–e20. [Google Scholar] [CrossRef] [PubMed]
- Koch, T.; Dahlke, C.; Fathi, A.; Kupke, A.; Krähling, V.; Okba, N.M.A.; Halwe, S.; Rohde, C.; Eickmann, M.; Volz, A.; et al. Safety and immunogenicity of a modified vaccinia virus Ankara vector vaccine candidate for Middle East respiratory syndrome: An open-label, phase 1 trial. Lancet Infect. Dis. 2020, 20, 827–838. [Google Scholar] [CrossRef]
- Li, K.; Wohlford-Lenane, C.; Perlman, S.; Zhao, J.; Jewell, A.K.; Reznikov, L.R.; Gibson-Corley, K.N.; Meyerholz, D.K.; McCray, P.B., Jr. Middle East Respiratory Syndrome Coronavirus Causes Multiple Organ Damage and Lethal Disease in Mice Transgenic for Human Dipeptidyl Peptidase 4. J. Infect. Dis. 2016, 213, 712–722. [Google Scholar] [CrossRef] [Green Version]
- Seo, S.H.; Jang, Y. Cold-Adapted Live Attenuated SARS-CoV-2 Vaccine Completely Protects Human ACE2 Transgenic Mice from SARS-CoV-2 Infection. Vaccines 2020, 8, 584. [Google Scholar] [CrossRef]
- Reed, L.J.; Muench, H. A simple method of estimating fifty percent endpoints. Am. J. Hyg. 1938, 27, 493–497. [Google Scholar]
- Corthésy, B. Multi-faceted functions of secretory IgA at mucosal surfaces. Front. Immunol. 2013, 4, 185. [Google Scholar] [CrossRef] [Green Version]
- Wang, N.; Shi, X.; Jiang, L.; Zhang, S.; Wang, D.; Tong, P.; Guo, D.; Fu, L.; Cui, Y.; Liu, X.; et al. Structure of MERS-CoV spike receptor-binding domain complexed with human receptor DPP4. Cell Res. 2013, 23, 986–993. [Google Scholar] [CrossRef] [Green Version]
- Yuan, S.; Balaji, S.; Lomakin, I.B.; Yong, X. Coronavirus Nsp1: Immune Response Suppression and Protein Expression Inhibition. Front. Microbiol. 2021, 12, 752214. [Google Scholar] [CrossRef] [PubMed]
- Lei, J.; Kusov, Y.; Hilgenfeld, R. Nsp3 of coronaviruses: Structures and functions of a large multi-domain protein. Antivir. Res. 2018, 149, 58–74. [Google Scholar] [CrossRef] [PubMed]
- Wu, A.; Wang, Y.; Zeng, C.; Huang, X.; Xu, S.; Su, C.; Wang, M.; Chen, Y.; Guo, D. Prediction and biochemical analysis of putative cleavage sites of the 3C-like protease of Middle East respiratory syndrome coronavirus. Virus Res. 2015, 208, 56–65. [Google Scholar] [CrossRef]
- Xia, H.; Cao, Z.; Xie, X.; Zhang, X.; Chen, J.Y.; Wang, H.; Menachery, V.D.; Rajsbaum, R.; Shi, P.Y. Evasion of Type I Interferon by SARS-CoV-2. Cell Rep. 2020, 33, 108234. [Google Scholar] [CrossRef]
- Littler, D.R.; Liu, M.; McAuley, J.L.; Lowery, S.A.; Illing, P.T.; Gully, B.S.; Purcell, A.W.; Chandrashekaran, I.R.; Perlman, S.; Purcell, D.F.J.; et al. A natural product compound inhibits coronaviral replication in vitro by binding to the conserved Nsp9 SARS-CoV-2 protein. J. Biol. Chem. 2021, 297, 101362. [Google Scholar] [CrossRef] [PubMed]
- Rona, G.; Zeke, A.; Miwatani-Minter, B.; de Vries, M.; Kaur, R.; Schinlever, A.; Garcia, S.F.; Goldberg, H.V.; Wang, H.; Hinds, T.R.; et al. The NSP14/NSP10 RNA repair complex as a Pan-coronavirus therapeutic target. Cell Death Differ. 2022, 29, 285–292. [Google Scholar] [CrossRef]
- Subbarao, K. Live Attenuated Cold-Adapted Influenza Vaccines. Cold Spring Harb. Perspect. Med. 2021, 11, a038653. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maassab, H.F. Adaptation and growth characteristics of influenza virus at 25 degrees c. Nature 1967, 213, 612–614. [Google Scholar] [CrossRef]
- Wang, L.; Shi, W.; Joyce, M.G.; Modjarrad, K.; Zhang, Y.; Leung, K.; Lees, C.R.; Zhou, T.; Yassine, H.M.; Kanekiyo, M.; et al. Evaluation of candidate vaccine approaches for MERS-CoV. Nat. Commun. 2015, 6, 7712. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Malczyk, A.H.; Kupke, A.; Prüfer, S.; Scheuplein, V.A.; Hutzler, S.; Kreuz, D.; Beissert, T.; Bauer, S.; Hubich-Rau, S.; Tondera, C.; et al. A Highly Immunogenic and Protective Middle East Respiratory Syndrome Coronavirus Vaccine Based on a Recombinant Measles Virus Vaccine Platform. J. Virol. 2015, 89, 11654–11667. [Google Scholar] [CrossRef] [PubMed]
- Patel, A.; Reuschel, E.L.; Xu, Z.; Zaidi, F.I.; Kim, K.Y.; Scott, D.P.; Mendoza, J.; Ramos, S.; Stoltz, R.; Feldmann, F.; et al. Intradermal delivery of a synthetic DNA vaccine protects macaques from Middle East respiratory syndrome coronavirus. JCI Insight 2021, 6, e146082. [Google Scholar] [CrossRef] [PubMed]
- Li, K.; Li, Z.; Wohlford-Lenane, C.; Meyerholz, D.K.; Channappanavar, R.; An, D.; Perlman, S.; McCray, P.B., Jr.; He, B. Single-Dose, Intranasal Immunization with Recombinant Parainfluenza Virus 5 Expressing Middle East Respiratory Syndrome Coronavirus (MERS-CoV) Spike Protein Protects Mice from Fatal MERS-CoV Infection. mBio 2020, 11, e00554-20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Javier Gutiérrez-Álvarez, J.; Honrubia, J.M.; Fernández-Delgado, R.; Wang, L.; Castaño-Rodríguez, C.; Zúñiga, S.; Sola, I.; Enjuanes, L. Genetically Engineered Live-Attenuated Middle East Respiratory Syndrome Coronavirus Viruses Confer Full Protection against Lethal Infection. mBio 2021, 12, e00103-21. [Google Scholar] [CrossRef] [PubMed]
- Boyaka, P.N. Inducing Mucosal IgA: A Challenge for Vaccine Adjuvants and Delivery Systems. J. Immunol. 2017, 199, 9–16. [Google Scholar] [CrossRef] [Green Version]



| Protein Name | Changed Amino Acid Sequences | The Number of Changed Sequence | |
|---|---|---|---|
| ORF1a polyprotein | nsp1 | H79R | 1/193 |
| nsp3 | H1616L, T2088P, and A2210V | 3/1887 | |
| nsp5 | Q3295R | 1/306 | |
| nsp6 | F3735I and E3822G | 2/292 | |
| nsp9 | P4195S | 1/110 | |
| nsp10 | N4247S | 1/140 | |
| S protein | T38P, N66Y, S305R, T872A, I879T, and S1251F | 6/1354 | |
| M protein | T5M | 1/220 | |
| Total amino acids | 16/12, 987 (including non-changed ORFs) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seo, H.; Jang, Y.; Kwak, D. The Protective Efficacy of Single-Dose Nasal Immunization with Cold-Adapted Live-Attenuated MERS-CoV Vaccine against Lethal MERS-CoV Infections in Mice. Vaccines 2023, 11, 1353. https://doi.org/10.3390/vaccines11081353
Seo H, Jang Y, Kwak D. The Protective Efficacy of Single-Dose Nasal Immunization with Cold-Adapted Live-Attenuated MERS-CoV Vaccine against Lethal MERS-CoV Infections in Mice. Vaccines. 2023; 11(8):1353. https://doi.org/10.3390/vaccines11081353
Chicago/Turabian StyleSeo, Heejeong, Yunyueng Jang, and Dongmi Kwak. 2023. "The Protective Efficacy of Single-Dose Nasal Immunization with Cold-Adapted Live-Attenuated MERS-CoV Vaccine against Lethal MERS-CoV Infections in Mice" Vaccines 11, no. 8: 1353. https://doi.org/10.3390/vaccines11081353






