Nanotechnology-Assisted Immunogenic Cell Death for Effective Cancer Immunotherapy
Abstract
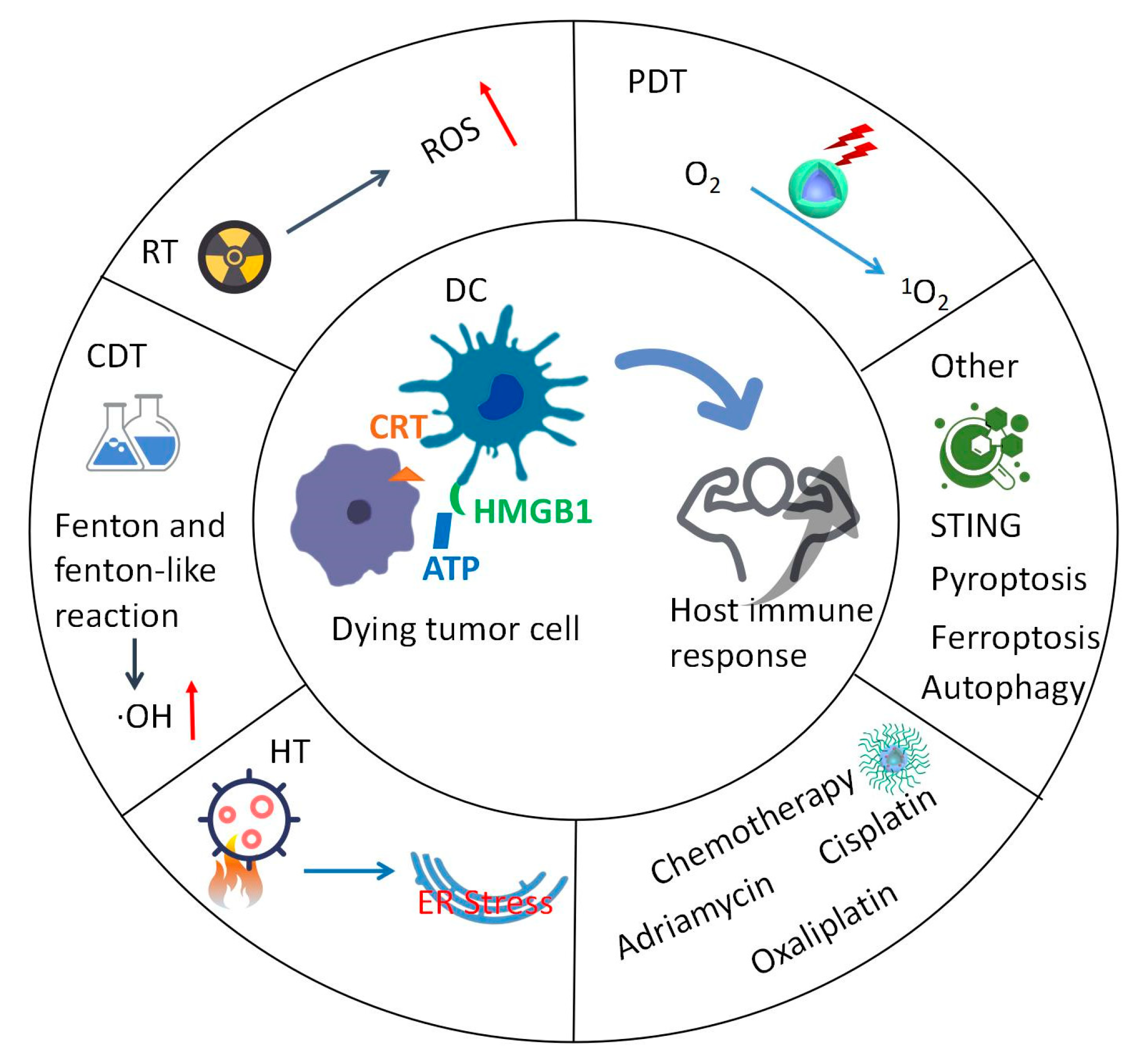
:1. Introduction
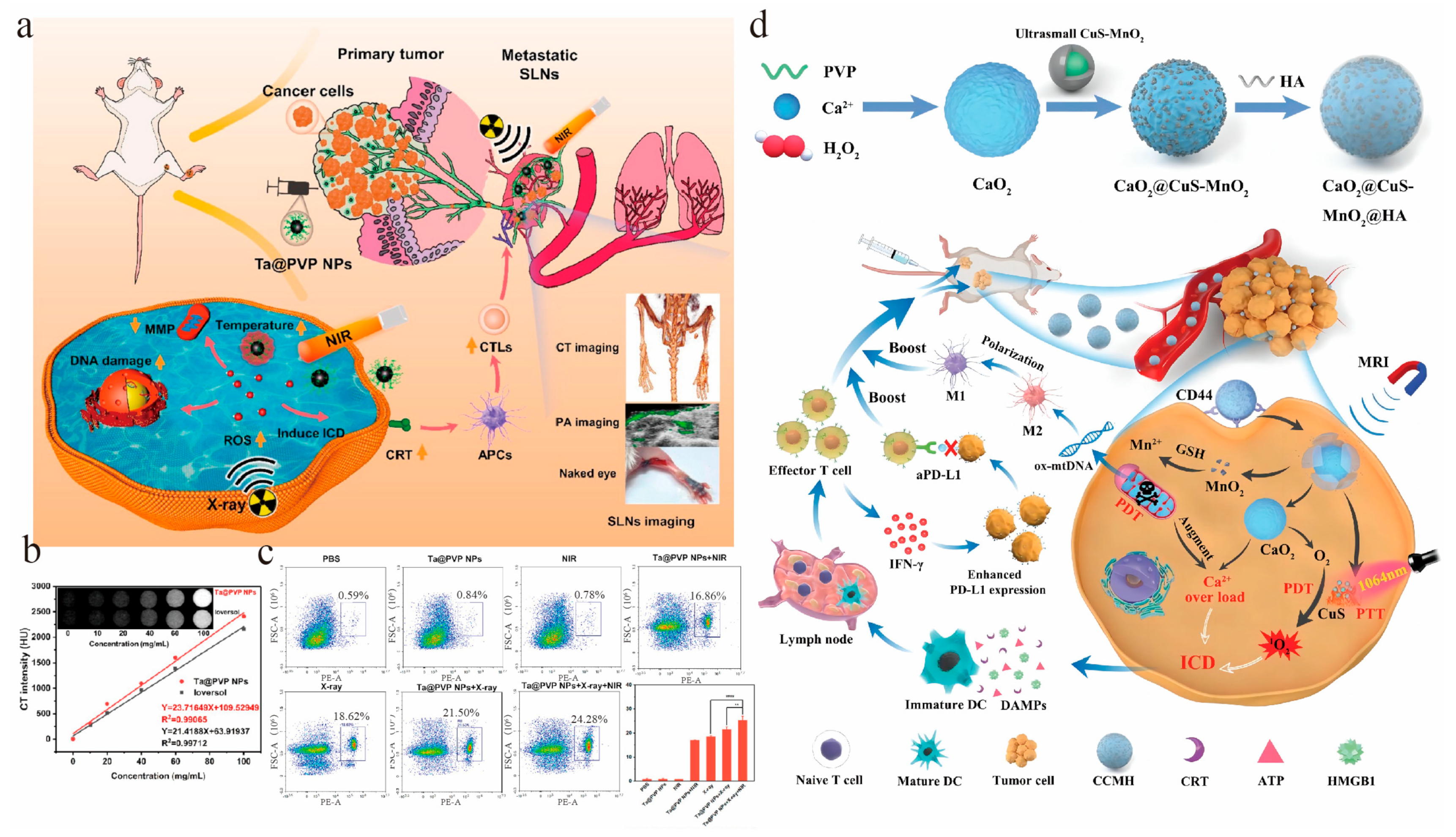
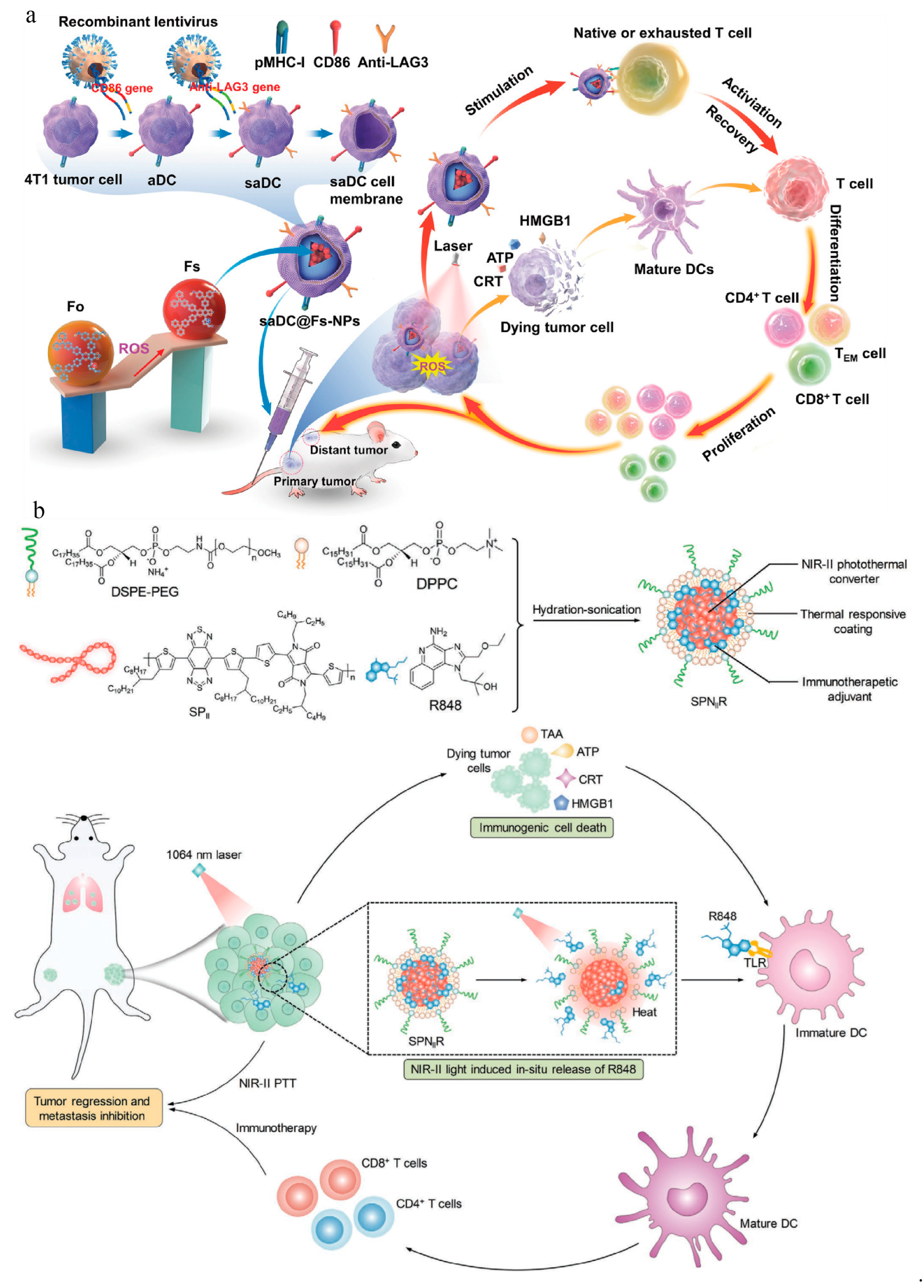
2. Radiotherapy
3. Photodynamic Therapy
| Formulation | Photosensitizer | Mechanism | NIR Light (nm) | Tumor Model | Ref. |
|---|---|---|---|---|---|
| Upconversion nanoparticle (UCNP)-based PDT system with an Fe-based CDT scaffold (UCS-PS-FeTA) | MC540Ce6 | UCNPs loaded with dual photosensitizers were irradiated with near-infrared (NIR) light to generate ROS to induce PDT. FeTA reacts with H2O2 in the tumor microenvironment to induce CDT. | 808 | Hepa1-6, MC38 | [62] |
| (Cytarabine, Ara-C)A-(Ce6)C/NPs | Ce6 | The controllable triggering of GSDME-mediated pyroptosis via ROS accumulation leads to immunogenic cell death. | 660 | 4T1, MDA-MB-231, MCF-7 | [63] |
| Gold nanobipyramids and copper sulfifide in a core/shell architecture (AuNBP@CuS) | Semiconducto-rs/plasmonic metal | The accumulated electrons from plasmonic metal nanocrystals can be easily transferred to surface-adsorbed oxygen to form superoxide anions. The accumulated holes favor the formation of 1O2. | 1064 | EMT-6 | [64] |
| Silk fibroin cRGDfk-Ce6 conjugate-based MnO2 nanocomposite (SRCM) | Ce6 | The cRGDfk sequence enables SRCM to target solid tumors with high expression of αvβ3. SRCM is reduced by the acidic environment of lysosomes and glutathione in the cytoplasm. Ce6 is released, triggering PDT. | 660 | 4T1 | [65] |
| Au–Pd heterostructures (Au Pd HSs) | Plasmonic | Under laser irradiation, Au-Pd-HSs can generate a large number of hot electrons. These highly efficient hot electrons can immediately promote heat release and ROS production, including 1O2, superoxide radicals, and hydroxyl radicals. | 808 | 4T1 | [66] |
| M-LDH/ICG@Ca3(PO4)2, MICaP | ICG | ICG produces 1O2 to induce ICD. | 808 | 4T1 | [67] |
| Iron tungsten oxide (FeWOx)-based nanosheets with surface PEGylation (FWO-PEG NA) | FWO-PEG NA | The irradiation of FWO-PEG NA with 1060 nm light produced heat and ROS to achieve the CDT/PDT/PTT combination and to induce further ICD. | 1060 | 4T1 | [68] |
| Perylene monoamide-based ROS supergenerator (PMIC-NC) | PDIs | A hypoxia-enhanced burst of typeⅠROS is induced with the help of a proton transient, while the generation of typeⅠ/ⅡROS is triggered by electron or energy transfer under NIR light irradiation and triggers a strong ICD effect. | 660 | B16 | [69] |
| RA-crosslinked supramolecular nanoassembly (CPR) | Ce6 | CPR produces large amounts of ROS to damage tumor cells and induce ICD. | 660 | 4T1 | [70] |
4. Hyperthermia Therapy
5. Chemodynamic Therapy
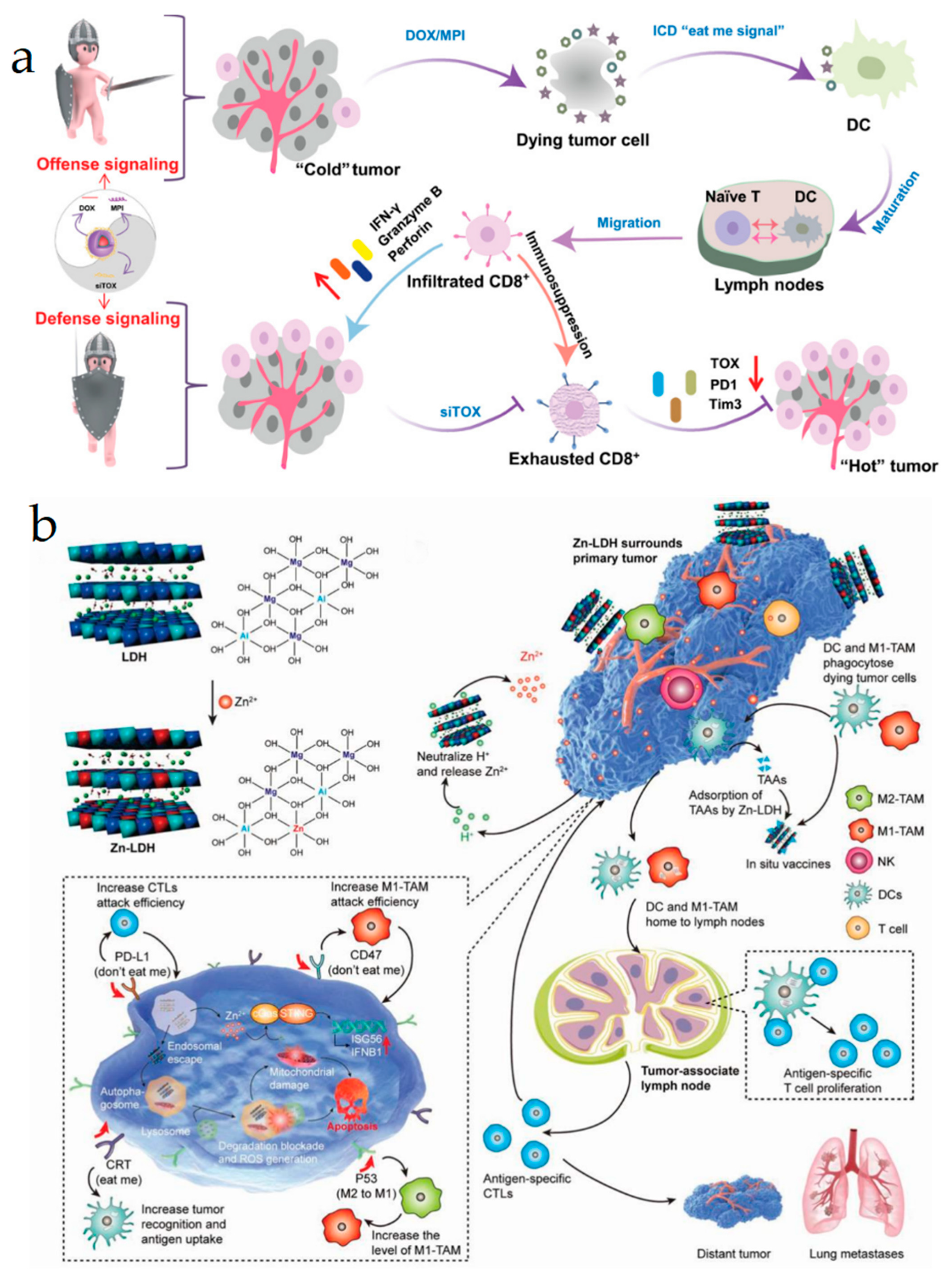
6. Chemotherapy
| Formulation | Cargo | Treatment Modalities | Tumor Model | Ref. |
|---|---|---|---|---|
| Metallacycle-loaded nanoparticles (MNPs) | Tetraphenylethylene-based di-Pt(II) organometallic precursor (TPE-Pt) perylene bisimide fluorophore (PPy) | Chemotherapy, RT | A2780CIS-derived multicellular tumor spheroid (MCS) | [106] |
| Mannose-targeted RBCD vesicle-coated PLB/DIH co-loaded nanoformulation (Comb-NP) | PLB, DIH | Chemotherapy | Huh7 HCC | [107] |
| iRGD-modified BTZ-based nanomedicine (i-NPBTZ) | BTZ | Chemotherapy | 4T1 | [108] |
| DOX/POEG-bPCro micelles | DOX, Cro | Chemotherapy | 4T1, LLC and HepG2 | [109] |
| α5β1 integrin-targeted micellar paclitaxel (ATN-MPTX) | PTX | Chemotherapy, STING agonist | 4T1 | [98] |
| ACD (A: Au nanoclusters, C: copper ions, D: DOX) | DOX, Au nanozymes | Chemotherapy, CDT | 4T1 | [110] |
7. STING, Pyroptosis, Ferroptosis, and Autophagy-Induced ICD
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Riley, R.S.; June, C.H.; Langer, R.; Mitchell, M.J. Delivery technologies for cancer immunotherapy. Nat. Rev. Drug Discov. 2019, 18, 175–196. [Google Scholar] [CrossRef] [PubMed]
- Topalian, S.L.; Weiner, G.J.; Pardoll, D.M. Cancer immunotherapy comes of age. J. Clin. Oncol. 2011, 29, 4828–4836. [Google Scholar] [CrossRef] [PubMed]
- DeLucia, D.C.; Lee, J.K. Development of Cancer Immunotherapies. Cancer Treat. Res. 2022, 183, 1–48. [Google Scholar] [CrossRef] [PubMed]
- Fan, Y.; Moon, J.J. Nanoparticle Drug Delivery Systems Designed to Improve Cancer Vaccines and Immunotherapy. Vaccines 2015, 3, 662–685. [Google Scholar] [CrossRef]
- Yang, W.; Deng, H.; Zhu, S.; Lau, J.; Tian, R.; Wang, S.; Zhou, Z.; Yu, G.; Rao, L.; He, L.; et al. Size-transformable antigen-presenting cell-mimicking nanovesicles potentiate effective cancer immunotherapy. Sci. Adv. 2020, 6, eabd1631. [Google Scholar] [CrossRef]
- Duan, X.; Chan, C.; Lin, W. Nanoparticle-Mediated Immunogenic Cell Death Enables and Potentiates Cancer Immunotherapy. Angew. Chem. Int. Ed. 2019, 58, 670–680. [Google Scholar] [CrossRef]
- Krysko, D.V.; Garg, A.D.; Kaczmarek, A.; Krysko, O.; Agostinis, P.; Vandenabeele, P. Immunogenic cell death and DAMPs in cancer therapy. Nat. Rev. Cancer 2012, 12, 860–875. [Google Scholar] [CrossRef]
- Fu, L.; Ma, X.; Liu, Y.; Xu, Z.; Sun, Z. Applying nanotechnology to boost cancer immunotherapy by promoting immunogenic cell death. Chin. Chem. Lett. 2022, 33, 1718–1728. [Google Scholar] [CrossRef]
- Choi, M.; Shin, J.; Lee, C.-E.; Chung, J.-Y.; Kim, M.; Yan, X.; Yang, W.-H.; Cha, J.-H. Immunogenic cell death in cancer immunotherapy. BMB Rep. 2023, 56, 275–286. [Google Scholar] [CrossRef]
- Park, S.J.; Ye, W.; Xiao, R.; Silvin, C.; Padget, M.; Hodge, J.W.; Van Waes, C.; Schmitt, N.C. Cisplatin and oxaliplatin induce similar immunogenic changes in preclinical models of head and neck cancer. Oral Oncol. 2019, 95, 127–135. [Google Scholar] [CrossRef]
- Bai, S.; Zhang, Y.; Li, D.; Shi, X.; Lin, G.; Liu, G. Gain an advantage from both sides: Smart size-shrinkable drug delivery nanosystems for high accumulation and deep penetration. Nano Today 2021, 36, e101038. [Google Scholar] [CrossRef]
- Sahu, T.; Ratre, Y.K.; Chauhan, S.; Bhaskar, L.V.K.S.; Nair, M.P.; Verma, H.K. Nanotechnology based drug delivery system: Current strategies and emerging therapeutic potential for medical science. J. Drug Deliv. Sci. Tec. 2021, 63, e102487. [Google Scholar] [CrossRef]
- Fang, J.; Islam, W.; Maeda, H. Exploiting the dynamics of the EPR effect and strategies to improve the therapeutic effects of nanomedicines by using EPR effect enhancers. Adv. Drug Deliv. Rev. 2020, 157, 142–160. [Google Scholar] [CrossRef]
- Shi, Y.; van der Meel, R.; Chen, X.; Lammers, T. The EPR effect and beyond: Strategies to improve tumor targeting and cancer nanomedicine treatment efficacy. Theranostics 2020, 10, 7921–7924. [Google Scholar] [CrossRef]
- Ikeda-Imafuku, M.; Wang, L.L.; Rodrigues, D.; Shaha, S.; Zhao, Z.; Mitragotri, S. Strategies to improve the EPR effect: A mechanistic perspective and clinical translation. J. Control. Release 2022, 345, 512–536. [Google Scholar] [CrossRef]
- Patra, J.K.; Das, G.; Fraceto, L.F.; Campos, E.V.R.; Rodriguez-Torres, M.D.P.; Acosta-Torres, L.S.; Diaz-Torres, L.A.; Grillo, R.; Swamy, M.K.; Sharma, S.; et al. Nano based drug delivery systems: Recent developments and future prospects. J. Nanobiotechnol. 2018, 16, 71. [Google Scholar] [CrossRef]
- Guo, J.; Zou, Y.; Huang, L. Nano Delivery of Chemotherapeutic ICD Inducers for Tumor Immunotherapy. Small Methods 2023, 7, e2201307. [Google Scholar] [CrossRef]
- Dai, H.; Fan, Q.; Wang, C. Recent applications of immunomodulatory biomaterials for disease immunotherapy. Exploration 2022, 2, e20210157. [Google Scholar] [CrossRef]
- Chen, Q.; Li, C.; Wang, Q. Multifunctional Nano-Biomaterials for Cancer Therapy via Inducing Enhanced Immunogenic Cell Death. Small Methods 2023, 7, e2201457. [Google Scholar] [CrossRef]
- Zhao, X.; Yang, K.; Zhao, R.; Ji, T.; Wang, X.; Yang, X.; Zhang, Y.; Cheng, K.; Liu, S.; Hao, J.; et al. Inducing enhanced immunogenic cell death with nanocarrier-based drug delivery systems for pancreatic cancer therapy. Biomaterials 2016, 102, 187–197. [Google Scholar] [CrossRef]
- Ding, Y.; Wang, Y.; Hu, Q. Recent advances in overcoming barriers to cell-based delivery systems for cancer immunotherapy. Exploration 2022, 2, e20210106. [Google Scholar] [CrossRef]
- Jiang, M.; Zeng, J.; Zhao, L.; Zhang, M.; Ma, J.; Guan, X.; Zhang, W. Chemotherapeutic drug-induced immunogenic cell death for nanomedicine-based cancer chemo-immunotherapy. Nanoscale 2021, 13, 17218–17235. [Google Scholar] [CrossRef]
- Shang, T.; Yu, X.; Han, S.; Yang, B. Nanomedicine-based tumor photothermal therapy synergized immunotherapy. Biomater. Sci. 2020, 8, 5241–5259. [Google Scholar] [CrossRef]
- Yang, Y.; Huang, J.; Liu, M.; Qiu, Y.; Chen, Q.; Zhao, T.; Xiao, Z.; Yang, Y.; Jiang, Y.; Huang, Q.; et al. Emerging Sonodynamic Therapy-Based Nanomedicines for Cancer Immunotherapy. Sci. Adv. 2023, 10, e2204365. [Google Scholar] [CrossRef]
- Tian, H.; Zhang, M.; Jin, G.; Jiang, Y.; Luan, Y. Cu-MOF chemodynamic nanoplatform via modulating glutathione and H2O2 in tumor microenvironment for amplified cancer therapy. J. Colloid Interface Sci. 2021, 587, 358–366. [Google Scholar] [CrossRef]
- Sun, J.; Huangfu, Z.; Yang, J.; Wang, G.; Hu, K.; Gao, M.; Zhong, Z. Imaging-guided targeted radionuclide tumor therapy: From concept to clinical translation. Adv. Drug Deliv. Rev. 2022, 190, e114538. [Google Scholar] [CrossRef]
- Yu, X.; Ma, H.; Xu, G.; Liu, Z. Radiotherapy assisted with biomaterials to trigger antitumor immunity. Chin. Chem. Lett. 2022, 33, 4169–4174. [Google Scholar] [CrossRef]
- Huang, Z.; Yao, D.; Ye, Q.; Jiang, H.; Gu, R.; Ji, C.; Wu, J.; Hu, Y.; Yuan, A. Zoledronic Acid-Gadolinium Coordination Polymer Nanorods for Improved Tumor Radioimmunotherapy by Synergetically Inducing Immunogenic Cell Death and Reprogramming the Immunosuppressive Microenvironment. ACS Nano 2021, 15, 8450–8465. [Google Scholar] [CrossRef]
- Pan, P.; Dong, X.; Chen, Y.; Ye, J.J.; Sun, Y.X.; Zhang, X.Z. A heterogenic membrane-based biomimetic hybrid nanoplatform for combining radiotherapy and immunotherapy against breast cancer. Biomaterials 2022, 289, e121810. [Google Scholar] [CrossRef]
- Zhu, X.; Wang, X.; Li, B.; Zhang, Y.; Chen, Y.; Zhang, W.; Wang, Y.; Zhai, W.; Liu, Z.; Liu, S.; et al. A Three-In-One Assembled Nanoparticle Containing Peptide-Radio-Sensitizer Conjugate and TLR7/8 Agonist Can Initiate the Cancer-Immunity Cycle to Trigger Antitumor Immune Response. Small 2022, 18, e2107001. [Google Scholar] [CrossRef]
- Sun, Q.; Li, J.; Ding, Z.; Liu, Z. Radiopharmaceuticals heat anti-tumor immunity. Theranostics 2023, 13, 767–786. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Wang, Z.; Liu, X.; Song, N.; Song, Y.; Shi, X.; Liu, J.; Liu, J.; Yu, Z. Adaptable peptide-based therapeutics modulating tumor microenvironment for combinatorial radio-immunotherapy. J. Control. Release 2021, 340, 35–47. [Google Scholar] [CrossRef] [PubMed]
- Deng, Z.; Xi, M.; Zhang, C.; Wu, X.; Li, Q.; Wang, C.; Fang, H.; Sun, G.; Zhang, Y.; Yang, G.; et al. Biomineralized MnO2 Nanoplatforms Mediated Delivery of Immune Checkpoint Inhibitors with STING Pathway Activation to Potentiate Cancer Radio-Immunotherapy. ACS Nano 2023, 17, 4495–4506. [Google Scholar] [CrossRef]
- Huang, Z.; Wang, Y.; Yao, D.; Wu, J.; Hu, Y.; Yuan, A. Nanoscale coordination polymers induce immunogenic cell death by amplifying radiation therapy mediated oxidative stress. Nat. Commun. 2021, 12, 145. [Google Scholar] [CrossRef] [PubMed]
- Li, T.; Gao, M.; Wu, Z.; Yang, J.; Mo, B.; Yu, S.; Gong, X.; Liu, J.; Wang, W.; Luo, S.; et al. Tantalum-Zirconium Co-Doped Metal-Organic Frameworks Sequentially Sensitize Radio-Radiodynamic-Immunotherapy for Metastatic Osteosarcoma. Adv. Sci. 2023, 10, e2206779. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Ding, Y.; Yao, D.; Dong, H.; Ji, C.; Wu, J.; Hu, Y.; Yuan, A. Copper-Based Nanoscale Coordination Polymers Augmented Tumor Radioimmunotherapy for Immunogenic Cell Death Induction and T-Cell Infiltration. Small 2021, 17, e2006231. [Google Scholar] [CrossRef] [PubMed]
- Zheng, D.; Li, Y.; Song, L.; Xu, T.; Jiang, X.; Yin, X.; He, Y.; Xu, J.; Ma, X.; Chai, L.; et al. Improvement of radiotherapy with an ozone-carried liposome nano-system for synergizing cancer immune checkpoint blockade. Nano Today 2022, 47, e101675. [Google Scholar] [CrossRef]
- Zhu, C.; Guo, X.; Luo, L.; Wu, Z.; Luo, Z.; Jiang, M.; Zhang, J.; Qin, B.; Shi, Y.; Lou, Y.; et al. Extremely Effective Chemoradiotherapy by Inducing Immunogenic Cell Death and Radio-Triggered Drug Release under Hypoxia Alleviation. ACS Appl. Mater. Interfaces 2019, 11, 46536–46547. [Google Scholar] [CrossRef]
- Choi, B.; Choi, H.; Yu, B.; Kim, D.H. Synergistic Local Combination of Radiation and Anti-Programmed Death Ligand 1 Immunotherapy Using Radiation-Responsive Splintery Metallic Nanocarriers. ACS Nano 2020, 14, 13115–13126. [Google Scholar] [CrossRef]
- Qin, X.; Liu, J.; Xu, Y.; Li, B.; Cheng, J.; Wu, X.; Zhang, J.; Liu, Z.; Ning, R.; Li, Y.; et al. Mesoporous Bi-Containing Radiosensitizer Loading with DOX to Repolarize Tumor-Associated Macrophages and Elicit Immunogenic Tumor Cell Death to Inhibit Tumor Progression. ACS Appl. Mater. Interfaces 2020, 12, 31225–31234. [Google Scholar] [CrossRef]
- Shao, D.; Zhang, F.; Chen, F.; Zheng, X.; Hu, H.; Yang, C.; Tu, Z.; Wang, Z.; Chang, Z.; Lu, J.; et al. Biomimetic Diselenide-Bridged Mesoporous Organosilica Nanoparticles as an X-ray-Responsive Biodegradable Carrier for Chemo-Immunotherapy. Adv. Mater. 2020, 32, e2004385. [Google Scholar] [CrossRef]
- Ji, C.; Zhao, M.; Wang, C.; Liu, R.; Zhu, S.; Dong, X.; Su, C.; Gu, Z. Biocompatible Tantalum Nanoparticles as Radiosensitizers for Enhancing Therapy Efficacy in Primary Tumor and Metastatic Sentinel Lymph Nodes. ACS Nano 2022, 16, 9428–9441. [Google Scholar] [CrossRef]
- Chen, Q.; Chen, J.; Yang, Z.; Xu, J.; Xu, L.; Liang, C.; Han, X.; Liu, Z. Nanoparticle-Enhanced Radiotherapy to Trigger Robust Cancer Immunotherapy. Adv. Mater. 2019, 31, e1802228. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Wang, M.; Huang, B.; Zhu, S.-W.; Zhou, J.-J.; Chen, D.-R.; Cui, R.; Zhang, M.; Sun, Z.-J. Theranostic near-infrared-IIb emitting nanoprobes for promoting immunogenic radiotherapy and abscopal effects against cancer metastasis. Nat. Commun. 2021, 12, 7149. [Google Scholar] [CrossRef] [PubMed]
- Kashyap, B.K.; Singh, V.V.; Solanki, M.K.; Kumar, A.; Ruokolainen, J.; Kesari, K.K. Smart Nanomaterials in Cancer Theranostics: Challenges and Opportunities. ACS Omega 2023, 8, 14290–14320. [Google Scholar] [CrossRef] [PubMed]
- Son, S.; Kim, J.; Kim, J.; Kim, B.; Lee, J.; Kim, Y.; Li, M.; Kang, H.; Kim, J.S. Cancer therapeutics based on diverse energy sources. Chem. Soc. Rev. 2022, 51, 8201–8215. [Google Scholar] [CrossRef]
- Xu, R.; Chi, W.; Zhao, Y.; Tang, Y.; Jing, X.; Wang, Z.; Zhou, Y.; Shen, Q.; Zhang, J.; Yang, Z.; et al. All-in-One Theranostic Platforms: Deep-Red AIE Nanocrystals to Target Dual-Organelles for Efficient Photodynamic Therapy. ACS Nano 2022, 16, 20151–20162. [Google Scholar] [CrossRef]
- Yang, W.; Zhu, G.; Wang, S.; Yu, G.; Yang, Z.; Lin, L.; Zhou, Z.; Liu, Y.; Dai, Y.; Zhang, F.; et al. In Situ Dendritic Cell Vaccine for Effective Cancer Immunotherapy. ACS Nano 2019, 13, 3083–3094. [Google Scholar] [CrossRef]
- Shen, L.; Zhou, T.; Fan, Y.; Chang, X.; Wang, Y.; Sun, J.; Xing, L.; Jiang, H. Recent progress in tumor photodynamic immunotherapy. Chin. Chem. Lett. 2020, 31, 1709–1716. [Google Scholar] [CrossRef]
- Li, M.; Zhao, M.; Zhang, Y.; Ding, M.; Yu, N.; Peng, S.; Shi, X.; Li, J. Second near-infrared light-activated semiconducting polymer nanomediators enable three-in-one tumor microenvironment modulation for combination immunotherapy. Nano Today 2023, 50, e101833. [Google Scholar] [CrossRef]
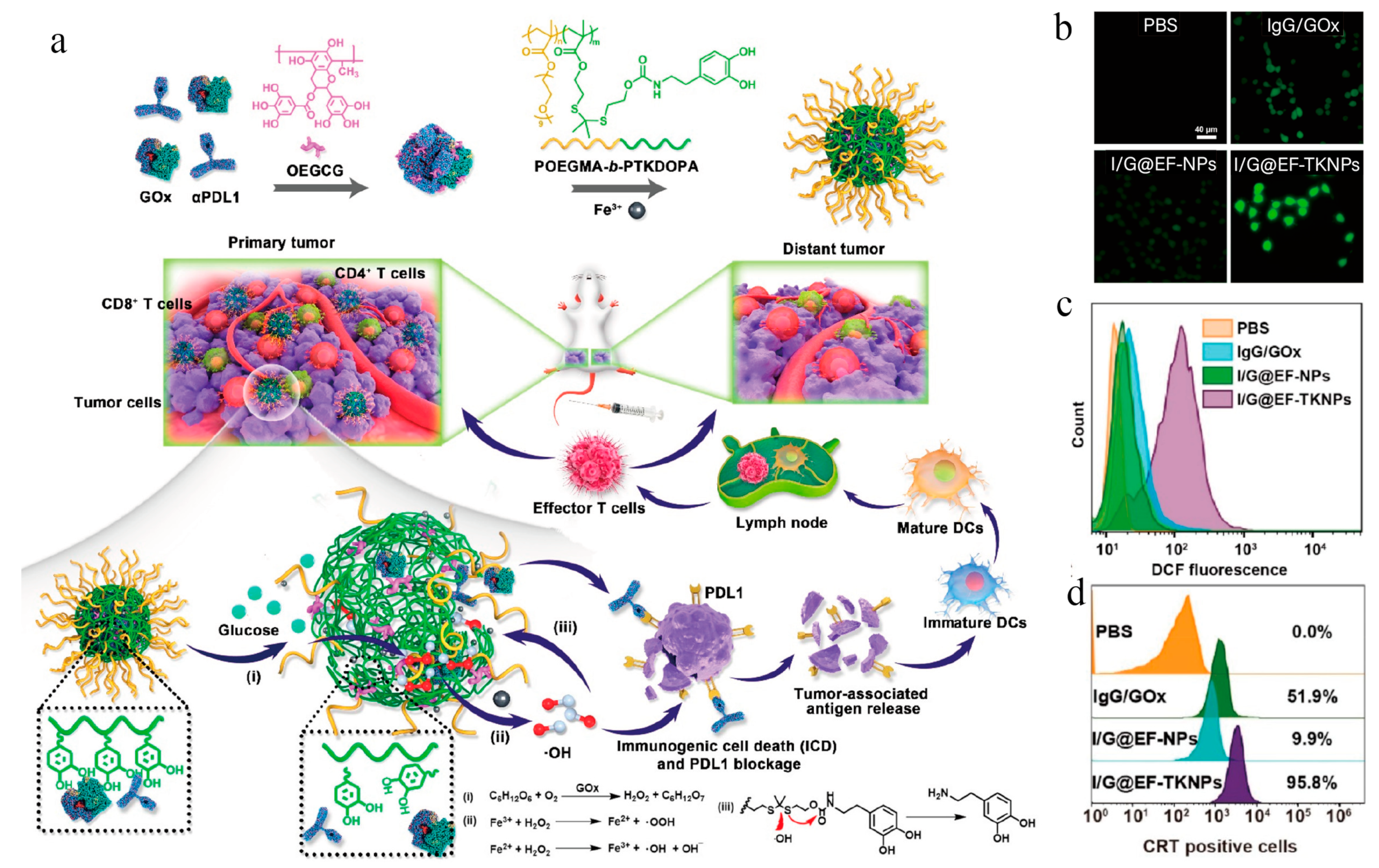
- Huang, C.; Lin, B.; Chen, C.; Wang, H.; Lin, X.; Liu, J.; Ren, Q.; Tao, J.; Zhao, P.; Xu, Y. Synergistic Reinforcing of Immunogenic Cell Death and Transforming Tumor-Associated Macrophages Via a Multifunctional Cascade Bioreactor for Optimizing Cancer Immunotherapy. Adv. Mater. 2022, 34, e2207593. [Google Scholar] [CrossRef] [PubMed]
- Zhao, L.; Rao, X.; Huang, C.; Zheng, R.; Kong, R.; Chen, Z.; Yu, X.; Cheng, H.; Li, S. Epigenetic reprogramming of carrier free photodynamic modulator to activate tumor immunotherapy by EZH2 inhibition. Biomaterials 2022, 293, e121952. [Google Scholar] [CrossRef]
- Zheng, R.R.; Zhao, L.P.; Yang, N.; Chen, Z.X.; Kong, R.J.; Huang, C.Y.; Rao, X.N.; Chen, X.; Cheng, H.; Li, S.Y. Cascade Immune Activation of Self-Delivery Biomedicine for Photodynamic Immunotherapy Against Metastatic Tumor. Small 2023, 19, e2205694. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Xiong, T.; Zhao, X.; Du, J.; Sun, W.; Fan, J.; Peng, X. Tumor Cell-Responsive Photodynamic Immunoagent for Immunogenicity-Enhanced Orthotopic and Remote Tumor Therapy. Adv. Healthc. Mater. 2023, 12, e2202085. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Ai, X.; Cabral, H.; Liu, J.; Huang, Y.; Mi, P. Tumor hypoxia-activated combinatorial nanomedicine triggers systemic antitumor immunity to effectively eradicate advanced breast cancer. Biomaterials 2021, 273, e120847. [Google Scholar] [CrossRef]
- Jin, F.; Liu, D.; Xu, X.; Ji, J.; Du, Y. Nanomaterials-Based Photodynamic Therapy with Combined Treatment Improves Antitumor Efficacy Through Boosting Immunogenic Cell Death. Int. J. Nanomed. 2021, 16, 4693–4712. [Google Scholar] [CrossRef]
- Mai, Z.; Zhong, J.; Zhang, J.; Chen, G.; Tang, Y.; Ma, W.; Li, G.; Feng, Z.; Li, F.; Liang, X.J.; et al. Carrier-Free Immunotherapeutic Nano-Booster with Dual Synergistic Effects Based on Glutaminase Inhibition Combined with Photodynamic Therapy. ACS Nano 2023, 17, 1583–1596. [Google Scholar] [CrossRef]
- Choi, J.; Shim, M.K.; Yang, S.; Hwang, H.S.; Cho, H.; Kim, J.; Yun, W.S.; Moon, Y.; Kim, J.; Yoon, H.Y.; et al. Visible-Light-Triggered Prodrug Nanoparticles Combine Chemotherapy and Photodynamic Therapy to Potentiate Checkpoint Blockade Cancer Immunotherapy. ACS Nano 2021, 15, 12086–12098. [Google Scholar] [CrossRef]
- Sun, Z.; Liu, J.; Li, Y.; Lin, X.; Chu, Y.; Wang, W.; Huang, S.; Li, W.; Peng, J.; Liu, C.; et al. Aggregation-Induced-Emission Photosensitizer-Loaded Nano-superartificial Dendritic Cells with Directly Presenting Tumor Antigens and Reversed Immunosuppression for Photodynamically Boosted Immunotherapy. Adv. Mater. 2022, 35, e2208555. [Google Scholar] [CrossRef]
- Xu, X.; Deng, G.; Sun, Z.; Luo, Y.; Liu, J.; Yu, X.; Zhao, Y.; Gong, P.; Liu, G.; Zhang, P.; et al. A Biomimetic Aggregation-Induced Emission Photosensitizer with Antigen-Presenting and Hitchhiking Function for Lipid Droplet Targeted Photodynamic Immunotherapy. Adv. Mater. 2021, 33, e2102322. [Google Scholar] [CrossRef]
- Li, J.; Yu, X.; Jiang, Y.; He, S.; Zhang, Y.; Luo, Y.; Pu, K. Second Near-Infrared Photothermal Semiconducting Polymer Nanoadjuvant for Enhanced Cancer Immunotherapy. Adv. Mater. 2021, 33, e2003458. [Google Scholar] [CrossRef] [PubMed]
- Cen, D.; Zheng, Q.; Zheng, B.; Zhou, R.; Xiao, X.; Zhang, T.; Huang, Z.; Yan, T.; Yu, J.; Li, X.; et al. A Near-Infrared Light-Responsive ROS Cascade Nanoplatform for Synergistic Therapy Potentiating Antitumor Immune Responses. Adv. Funct. Mater. 2023, 33, e2211402. [Google Scholar] [CrossRef]
- Li, L.; Tian, H.; Zhang, Z.; Ding, N.; He, K.; Lu, S.; Liu, R.; Wu, P.; Wang, Y.; He, B.; et al. Carrier-Free Nanoplatform via Evoking Pyroptosis and Immune Response against Breast Cancer. ACS Appl. Mater. Interfaces 2023, 15, 452–468. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Liu, P.; Zhou, C.; Zhang, T.; Zhou, T.; Men, D.; Jiang, G.; Hang, L. Gold nanobipyramid@copper sulfide nanotheranostics for image-guided NIR-II photo/chemodynamic cancer therapy with enhanced immune response. Acta Biomater. 2023, 158, 649–659. [Google Scholar] [CrossRef]
- He, L.; Wang, J.; Zhu, P.; Chen, J.; Zhao, S.; Liu, X.; Li, Y.; Guo, X.; Yan, Z.; Shen, X.; et al. Intelligent manganese dioxide nanocomposites induce tumor immunogenic cell death and remould tumor microenvironment. Chem. Eng. J. 2023, 461, e141369. [Google Scholar] [CrossRef]
- Feng, Y.; Ning, X.; Wang, J.; Wen, Z.; Cao, F.; You, Q.; Zou, J.; Zhou, X.; Sun, T.; Cao, J.; et al. Mace-Like Plasmonic Au-Pd Heterostructures Boost Near-Infrared Photoimmunotherapy. Sci. Adv. 2023, 10, e2204842. [Google Scholar] [CrossRef]
- Zhu, B.; Qu, F.; Bi, D.; Geng, R.; Chen, S.; Zhu, J. Monolayer LDH Nanosheets with Ultrahigh ICG Loading for Phototherapy and Ca2+-Induced Mitochondrial Membrane Potential Damage to Co-Enhance Cancer Immunotherapy. ACS Appl. Mater. Interfaces 2023, 15, 9135–9149. [Google Scholar] [CrossRef]
- Xiang, Q.; Yang, C.; Luo, Y.; Liu, F.; Zheng, J.; Liu, W.; Ran, H.; Sun, Y.; Ren, J.; Wang, Z. Near-Infrared II Nanoadjuvant-Mediated Chemodynamic, Photodynamic, and Photothermal Therapy Combines Immunogenic Cell Death with PD-L1 Blockade to Enhance Antitumor Immunity. Small 2022, 18, e2107809. [Google Scholar] [CrossRef]
- Lou, X.; Wang, H.; Liu, Y.; Huang, Y.; Liu, Z.; Zhang, W.; Wang, T. Perylene-Based Reactive Oxygen Species Supergenerator for Immunogenic Photochemotherapy against Hypoxic Tumors. Angew. Chem. Int. Ed. 2023, 62, e202214586. [Google Scholar] [CrossRef]
- Zhou, Y.; Zhang, Y.; Jiang, C.; Chen, Y.; Tong, F.; Yang, X.; Wang, Y.; Xia, X.; Gao, H. Rosmarinic Acid-Crosslinked Supramolecular Nanoassembly with Self-Regulated Photodynamic and Anti-Metastasis Properties for Synergistic Photoimmunotherapy. Small 2023, 19, e2300594. [Google Scholar] [CrossRef]
- Ge, J.; Yang, N.; Yang, Y.; Yu, H.; Yang, X.; Wang, Y.; Wang, T.; Cheng, S.; Wang, Y.; Han, Z.; et al. The combination of eddy thermal effect of biodegradable magnesium with immune checkpoint blockade shows enhanced efficacy against osteosarcoma. Bioact. Mater. 2023, 25, 73–85. [Google Scholar] [CrossRef] [PubMed]
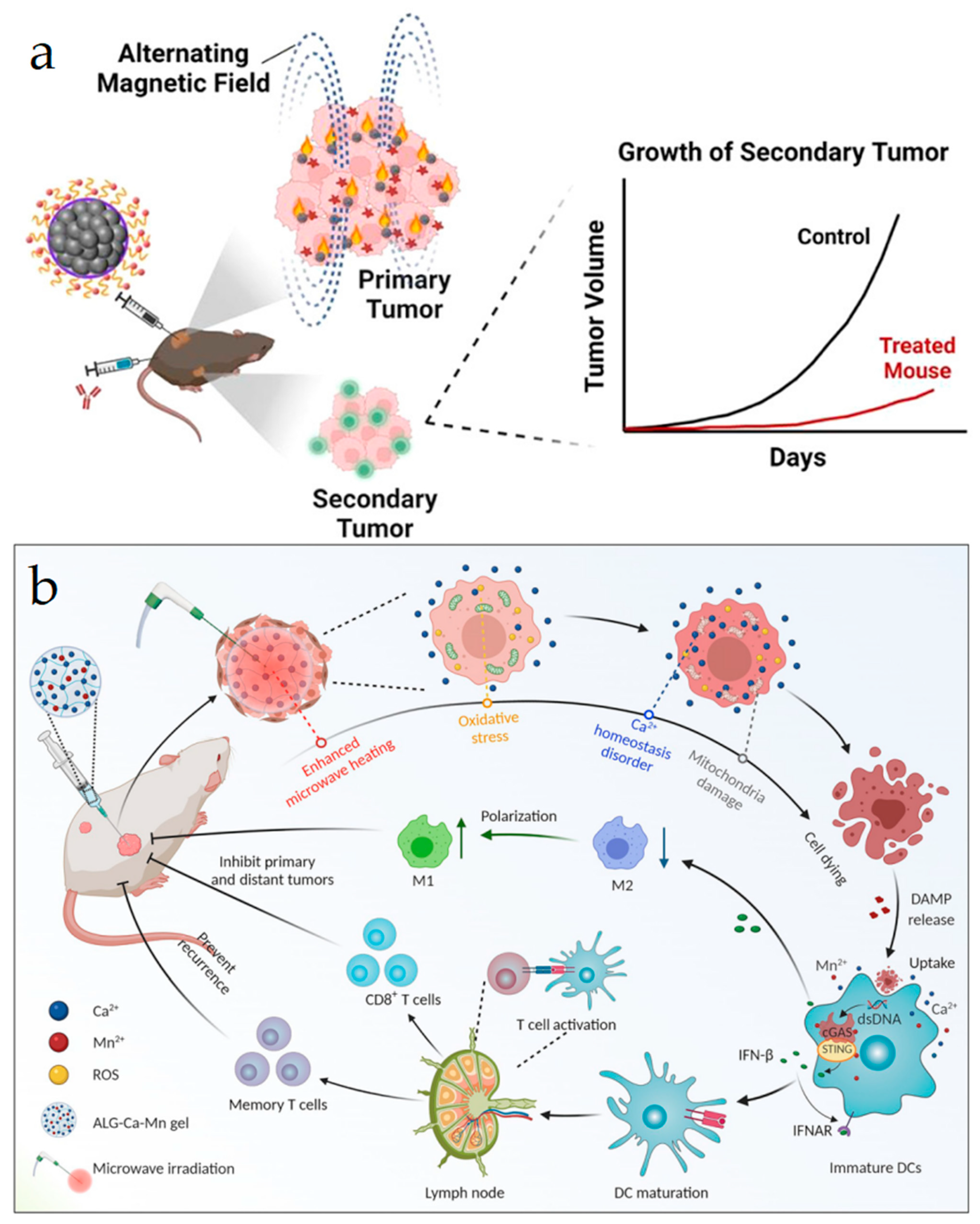
- Jiang, H.; Fu, H.; Guo, Y.; Hu, P.; Shi, J. Evoking tumor associated macrophages by mitochondria-targeted magnetothermal immunogenic cell death for cancer immunotherapy. Biomaterials 2022, 289, e121799. [Google Scholar] [CrossRef] [PubMed]
- Chang, M.; Hou, Z.; Wang, M.; Li, C.; Lin, J. Recent Advances in Hyperthermia Therapy-Based Synergistic Immunotherapy. Adv. Mater. 2021, 33, e2004788. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Fan, H.; Xu, Y.; Liu, M.; Liu, J.; Xu, L.; Zou, M.; Cheng, Q.; Zhang, Y.; Liang, T.; et al. NIR-responsive hollow germanium nanospheres mediate photothermal/photodynamic therapy and restrain immunosuppression to cooperatively eradicate primary and metastatic tumors. Chem. Eng. J. 2023, 458, e141314. [Google Scholar] [CrossRef]
- Zhao, Q.; Liang, G.; Guo, B.; Wang, W.; Yang, C.; Chen, D.; Yang, F.; Xiao, H.; Xing, N. Polyphotosensitizer-Based Nanoparticles with Michael Addition Acceptors Inhibiting GST Activity and Cisplatin Deactivation for Enhanced Chemotherapy and Photodynamic Immunotherapy. Sci. Adv. 2023, 10, e2300175. [Google Scholar] [CrossRef] [PubMed]
- Sun, Q.; Yang, Z.; Lin, M.; Peng, Y.; Wang, R.; Du, Y.; Zhou, Y.; Li, J.; Qi, X. Phototherapy and anti-GITR antibody-based therapy synergistically reinvigorate immunogenic cell death and reject established cancers. Biomaterials 2021, 269, e120648. [Google Scholar] [CrossRef]
- Liu, X.; Zheng, C.; Kong, Y.; Wang, H.; Wang, L. An in situ nanoparticle recombinant strategy for the enhancement of photothermal therapy. Chin. Chem. Lett. 2022, 33, 328–333. [Google Scholar] [CrossRef]
- Li, X.; Lovell, J.F.; Yoon, J.; Chen, X. Clinical development and potential of photothermal and photodynamic therapies for cancer. Nat. Rev. Clin. Oncol. 2020, 17, 657–674. [Google Scholar] [CrossRef]
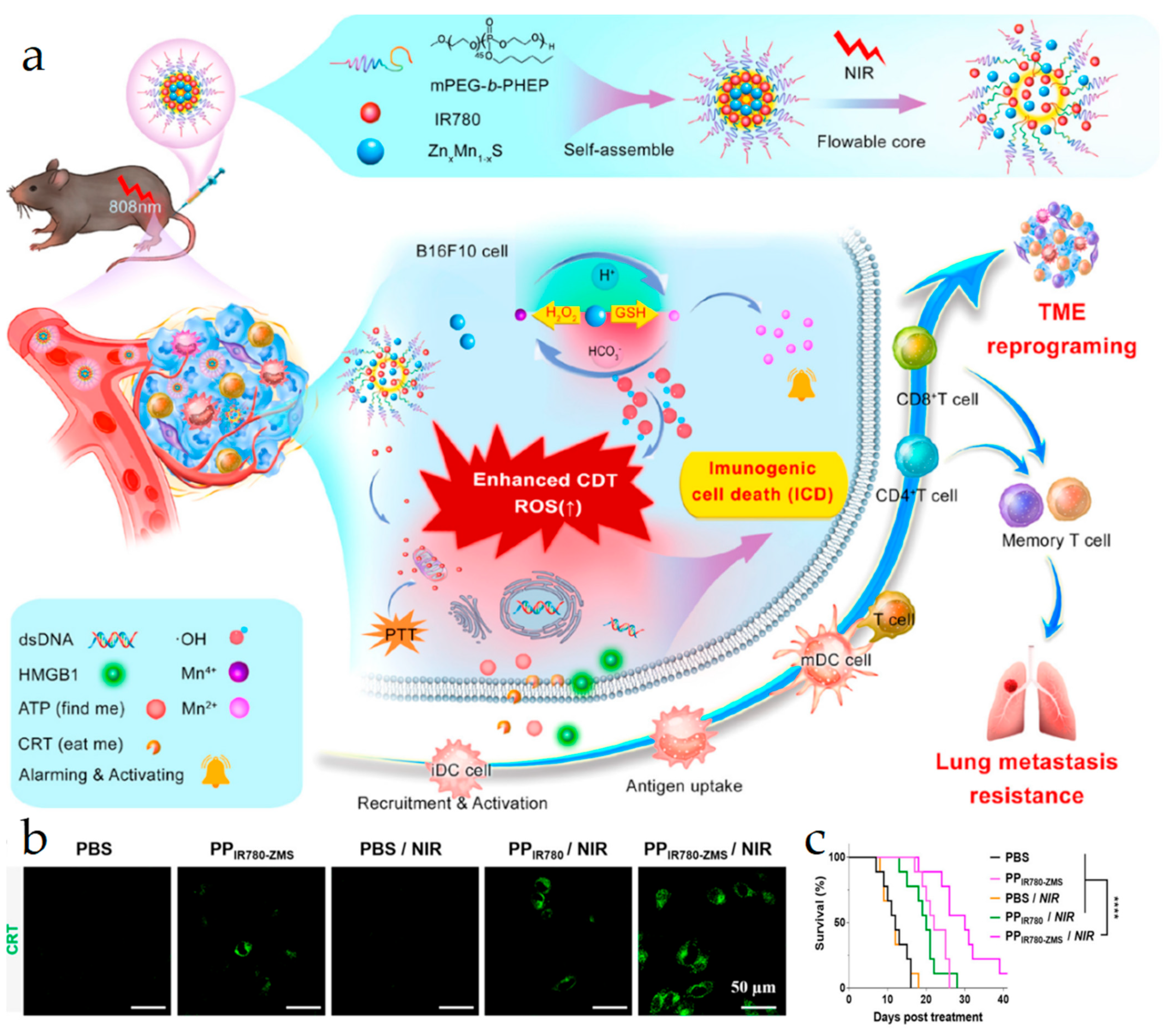
- Li, Z.; Chu, Z.; Yang, J.; Qian, H.; Xu, J.; Chen, B.; Tian, T.; Chen, H.; Xu, Y.; Wang, F. Immunogenic Cell Death Augmented by Manganese Zinc Sulfide Nanoparticles for Metastatic Melanoma Immunotherapy. ACS Nano 2022, 16, 15471–15483. [Google Scholar] [CrossRef]
- Li, J.; Lu, W.; Yang, Y.; Xiang, R.; Ling, Y.; Yu, C.; Zhou, Y. Hybrid Nanomaterials for Cancer Immunotherapy. Adv. Sci. 2022, 10, e2204932. [Google Scholar] [CrossRef]
- Zhang, L.; Zhang, Q.; Hinojosa, D.T.; Jiang, K.; Pham, Q.K.; Xiao, Z.; Colvin, V.L.; Bao, G. Multifunctional Magnetic Nanoclusters Can Induce Immunogenic Cell Death and Suppress Tumor Recurrence and Metastasis. ACS Nano 2022, 16, 18538–18554. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Yang, Z.; Pan, Z.; Hao, Y.; Wang, C.; Dong, Z.; Li, Q.; Han, Y.; Tian, L.; Feng, L.; et al. Metallo-alginate hydrogel can potentiate microwave tumor ablation for synergistic cancer treatment. Sci. Adv. 2022, 8, eabo5285. [Google Scholar] [CrossRef] [PubMed]
- Qi, J.; Jin, F.; You, Y.; Du, Y.; Liu, D.; Xu, X.; Wang, J.; Zhu, L.; Chen, M.; Shu, G.; et al. Synergistic effect of tumor chemo-immunotherapy induced by leukocyte-hitchhiking thermal-sensitive micelles. Nat. Commun. 2021, 12, 4755. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Zhou, Q.; Japir, A.; Dutta, D.; Lu, N.; Ge, Z. Protein-Delivering Nanocomplexes with Fenton Reaction-Triggered Cargo Release to Boost Cancer Immunotherapy. ACS Nano 2022, 16, 14982–14999. [Google Scholar] [CrossRef]
- Ding, F.; Li, F.; Tang, D.; Wang, B.; Liu, J.; Mao, X.; Yin, J.; Xiao, H.; Wang, J.; Liu, Z. Restoration of the Immunogenicity of Tumor Cells for Enhanced Cancer Therapy via Nanoparticle-Mediated Copper Chaperone Inhibition. Angew. Chem. Int. Ed. 2022, 61, e202203546. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.; Yang, J.; Zhou, L.; Hu, X.; Wang, C.; Chai, K.; Li, R.; Feng, L.; Sun, Y.; Dong, C.; et al. Dual-Responsive and ROS-Augmented Nanoplatform for Chemo/Photodynamic/Chemodynamic Combination Therapy of Triple Negative Breast Cancer. ACS Appl. Mater. Interfaces 2022, 14, 57–68. [Google Scholar] [CrossRef]
- Feng, X.; Lin, T.; Chen, D.; Li, Z.; Yang, Q.; Tian, H.; Xiao, Y.; Lin, M.; Liang, M.; Guo, W.; et al. Mitochondria-associated ER stress evokes immunogenic cell death through the ROS-PERK-eIF2α pathway under PTT/CDT combined therapy. Acta Biomater. 2023, 160, 211–224. [Google Scholar] [CrossRef]
- Fu, Z.; Zhang, Y.; Chen, X.; Wang, N.; Ma, R.; Luo, X.; Pan, X.; Yang, Y.; Xue, W. A Versatile Nanoplatform Based on Metal-Phenolic Networks Inhibiting Tumor Growth and Metastasis by Combined Starvation/Chemodynamic/Immunotherapy. Adv. Funct. Mater. 2022, 33, e2211869. [Google Scholar] [CrossRef]
- Huang, Y.; Wu, S.; Zhang, L.; Deng, Q.; Ren, J.; Qu, X. A Metabolic Multistage Glutathione Depletion Used for Tumor-Specific Chemodynamic Therapy. ACS Nano 2022, 16, 4228–4238. [Google Scholar] [CrossRef]
- Kuai, X.; Zhu, Y.; Yuan, Z.; Wang, S.; Lin, L.; Ye, X.; Lu, Y.; Luo, Y.; Pang, Z.; Geng, D.; et al. Perfluorooctyl bromide nanoemulsions holding MnO2 nanoparticles with dual-modality imaging and glutathione depletion enhanced HIFU-eliciting tumor immunogenic cell death. Acta Pharm. Sin. B 2022, 12, 967–981. [Google Scholar] [CrossRef]
- Liu, Y.; Zhai, S.; Jiang, X.; Liu, Y.; Wang, K.; Wang, C.; Zhang, M.; Liu, X.; Bu, W. Intracellular Mutual Promotion of Redox Homeostasis Regulation and Iron Metabolism Disruption for Enduring Chemodynamic Therapy. Adv. Funct. Mater. 2021, 31, e2010390. [Google Scholar] [CrossRef]
- Yan, J.; Yu, H.; Tang, X.; Li, F.; Li, Z.; Liang, Y.; He, B.; Wang, X.; Sun, Y. Highly triple-effective synergy based on tetrahedral DNA nanostructure-induced tumor vaccines for cancer therapy. Mater. Design 2023, 226, e111584. [Google Scholar] [CrossRef]
- Zhou, Y.; Fan, S.; Feng, L.; Huang, X.; Chen, X. Manipulating Intratumoral Fenton Chemistry for Enhanced Chemodynamic and Chemodynamic-Synergized Multimodal Therapy. Adv. Mater. 2021, 33, e2104223. [Google Scholar] [CrossRef] [PubMed]
- Bai, Y.; Pan, Y.; An, N.; Zhang, H.; Wang, C.; Tian, W.; Huang, T. Host-guest interactions based supramolecular complexes self-assemblies for amplified chemodynamic therapy with H2O2 elevation and GSH consumption properties. Chin. Chem. Lett. 2023, 34, 107552. [Google Scholar] [CrossRef]
- Sun, K.; Hu, J.; Meng, X.; Lei, Y.; Zhang, X.; Lu, Z.; Zhang, L.; Wang, Z. Reinforcing the Induction of Immunogenic Cell Death Via Artificial Engineered Cascade Bioreactor-Enhanced Chemo-Immunotherapy for Optimizing Cancer Immunotherapy. Small 2021, 17, e2101897. [Google Scholar] [CrossRef]
- Zhang, L.; Yang, L.L.; Wan, S.C.; Yang, Q.C.; Xiao, Y.; Deng, H.; Sun, Z.J. Three-Dimensional Covalent Organic Frameworks with Cross-Linked Pores for Efficient Cancer Immunotherapy. Nano Lett. 2021, 21, 7979–7988. [Google Scholar] [CrossRef] [PubMed]
- Guo, B.; Qu, Y.; Sun, Y.; Zhao, S.; Yuan, J.; Zhang, P.; Zhong, Z.; Meng, F. Co-delivery of gemcitabine and paclitaxel plus NanoCpG empowers chemoimmunotherapy of postoperative “cold” triple-negative breast cancer. Bioact. Mater. 2023, 25, 61–72. [Google Scholar] [CrossRef]
- Qiu, X.; Qu, Y.; Guo, B.; Zheng, H.; Meng, F.; Zhong, Z. Micellar paclitaxel boosts ICD and chemo-immunotherapy of metastatic triple negative breast cancer. J. Control. Release 2022, 341, 498–510. [Google Scholar] [CrossRef]
- Yang, J.; Ma, S.; Xu, R.; Wei, Y.; Zhang, J.; Zuo, T.; Wang, Z.; Deng, H.; Yang, N.; Shen, Q. Smart biomimetic metal organic frameworks based on ROS-ferroptosis-glycolysis regulation for enhanced tumor chemo-immunotherapy. J. Control. Release 2021, 334, 21–33. [Google Scholar] [CrossRef]
- Zhang, X.; Wang, S.; Cheng, G.; Yu, P.; Chang, J.; Chen, X. Cascade Drug-Release Strategy for Enhanced Anticancer Therapy. Matter 2021, 4, 26–53. [Google Scholar] [CrossRef]
- Xiang, J.; Zhang, Y.; Liu, X.; Zhou, Q.; Piao, Y.; Shao, S.; Tang, J.; Zhou, Z.; Xie, T.; Shen, Y. Natural Polyphenols-Platinum Nanocomplexes Stimulate Immune System for Combination Cancer Therapy. Nano Lett. 2022, 22, 5615–5625. [Google Scholar] [CrossRef]
- Wu, P.; Zhang, H.; Sun, M.; Mao, S.; He, Q.; Shi, Y.; Deng, Y.; Dong, Z.; Xu, Q.; Zhao, C.; et al. Manipulating Offense and Defense Signaling to Fight Cold Tumors with Carrier-Free Nanoassembly of Fluorinated Prodrug and siRNA. Adv. Mater. 2022, 34, e2203019. [Google Scholar] [CrossRef]
- Li, C.W.; Lim, S.O.; Hsu, J.L.; Hung, M.C. Rational combination of immunotherapy for triple negative breast cancer treatment. Chin. Clin. Oncol. 2017, 6, 54. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Shi, D.; Guo, M.; Zhao, H.; Zhao, Y.; Yang, X. Radiofrequency-Activated Pyroptosis of Bi-Valent Gold Nanocluster for Cancer Immunotherapy. ACS Nano 2023, 17, 515–529. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Zhao, J.; Hu, X.; Wang, C.; Jia, Y.; Zhu, C.; Xie, S.; Lee, J.; Li, F.; Ling, D. A Peritumorally Injected Immunomodulating Adjuvant Elicits Robust and Safe Metalloimmunotherapy against Solid Tumors. Adv. Mater. 2022, 34, e2206915. [Google Scholar] [CrossRef] [PubMed]
- Ding, Y.; Tong, Z.; Jin, L.; Ye, B.; Zhou, J.; Sun, Z.; Yang, H.; Hong, L.; Huang, F.; Wang, W.; et al. An NIR Discrete Metallacycle Constructed from Perylene Bisimide and Tetraphenylethylene Fluorophores for Imaging-Guided Cancer Radio-Chemotherapy. Adv. Mater. 2022, 34, e2106388. [Google Scholar] [CrossRef]
- Han, S.; Bi, S.; Guo, T.; Sun, D.; Zou, Y.; Wang, L.; Song, L.; Chu, D.; Liao, A.; Song, X.; et al. Nano co-delivery of Plumbagin and Dihydrotanshinone I reverses immunosuppressive TME of liver cancer. J. Control. Release 2022, 348, 250–263. [Google Scholar] [CrossRef]
- Jiang, W.; Zhou, H.; Wang, Q.; Chen, Z.; Dong, W.; Guo, Z.; Li, Y.; Zhao, W.; Zhan, M.; Wang, Y.; et al. High drug loading and pH-responsive nanomedicines driven by dynamic boronate covalent chemistry for potent cancer immunotherapy. Nano Res. 2021, 14, 3913–3920. [Google Scholar] [CrossRef]
- Liang, Q.; Lan, Y.; Li, Y.; Cao, Y.; Li, J.; Liu, Y. Crizotinib prodrug micelles co-delivered doxorubicin for synergistic immunogenic cell death induction on breast cancer chemo-immunotherapy. Eur. J. Pharm. Biopharm. 2022, 177, 260–272. [Google Scholar] [CrossRef]
- Zhao, D.H.; Li, C.Q.; Hou, X.L.; Xie, X.T.; Zhang, B.; Wu, G.Y.; Jin, F.; Zhao, Y.D.; Liu, B. Tumor Microenvironment-Activated Theranostics Nanozymes for Fluorescence Imaging and Enhanced Chemo-Chemodynamic Therapy of Tumors. ACS Appl. Mater. Interfaces 2021, 13, 55780–55789. [Google Scholar] [CrossRef]
- Wang, Z.; Chen, J.; Hu, J.; Zhang, H.; Xu, F.; He, W.; Wang, X.; Li, M.; Lu, W.; Zeng, G.; et al. cGAS/STING axis mediates a topoisomerase II inhibitor-induced tumor immunogenicity. J. Clin. Investig. 2019, 129, 4850–4862. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Wang, Z.; Jia, S.; Zhang, Y.; Ji, S.; Zhao, Z.; Kwok, R.T.K.; Lam, J.W.Y.; Ding, D.; Shi, Y.; et al. Evoking Highly Immunogenic Ferroptosis Aided by Intramolecular Motion-Induced Photo-Hyperthermia for Cancer Therapy. Adv. Sci. 2022, 9, e2104885. [Google Scholar] [CrossRef] [PubMed]
- Gao, W.; Wang, X.; Zhou, Y.; Wang, X.; Yu, Y. Autophagy, ferroptosis, pyroptosis, and necroptosis in tumor immunotherapy. Signal Transduct. Target. Ther. 2022, 7, 196. [Google Scholar] [CrossRef]
- Chattopadhyay, S.; Liu, Y.H.; Fang, Z.S.; Lin, C.L.; Lin, J.C.; Yao, B.Y.; Hu, C.J. Synthetic Immunogenic Cell Death Mediated by Intracellular Delivery of STING Agonist Nanoshells Enhances Anticancer Chemo-immunotherapy. Nano Lett. 2020, 20, 2246–2256. [Google Scholar] [CrossRef] [PubMed]
- Zhang, R.; Kang, R.; Tang, D. The STING1 network regulates autophagy and cell death. Signal Transduct. Target. 2021, 6, 208. [Google Scholar] [CrossRef]
- Li, C.; Zhang, Y.; Wan, Y.; Wang, J.; Lin, J.; Li, Z.; Huang, P. STING-activating drug delivery systems: Design strategies and biomedical applications. Chin. Chem. Lett. 2021, 32, 1615–1625. [Google Scholar] [CrossRef]
- Garland, K.M.; Sheehy, T.L.; Wilson, J.T. Chemical and Biomolecular Strategies for STING Pathway Activation in Cancer Immunotherapy. Chem. Rev. 2022, 122, 5977–6039. [Google Scholar] [CrossRef]
- Samson, N.; Ablasser, A. The cGAS–STING pathway and cancer. Nat. Cancer 2022, 3, 1452–1463. [Google Scholar] [CrossRef]
- Ma, X.; Su, W.; Ye, M.; Gao, Y.; Qiu, W.; Liang, M.; Xue, P.; Kang, Y.; Sun, Z.-J.; Xu, Z. Endogenous/exogenous stimulies inspired polyprodrug nano-inducer switches pyroptosis path for promoting antitumor immunity. Nano Today 2023, 48, e101727. [Google Scholar] [CrossRef]
- Wang, H.; Gao, Z.; Jiao, D.; Zhang, Y.; Zhang, J.; Wang, T.; Huang, Y.; Zheng, D.; Hou, J.; Ding, D.; et al. A Microenvironment Dual-Responsive Nano-Drug Equipped with PD-L1 Blocking Peptide Triggers Immunogenic Pyroptosis for Prostate Cancer Self-Synergistic Immunotherapy. Adv. Funct. Mater. 2023, 33, e2214499. [Google Scholar] [CrossRef]
- Tang, Y.; Bisoyi, H.K.; Chen, X.M.; Liu, Z.; Chen, X.; Zhang, S.; Li, Q. Pyroptosis-Mediated Synergistic Photodynamic and Photothermal Immunotherapy Enabled by Tumor Membrane-Targeted Photosensitive Dimer. Adv. Mater. 2023, 35, e2300232. [Google Scholar] [CrossRef]
- Stockwell, B.R.; Friedmann Angeli, J.P.; Bayir, H.; Bush, A.I.; Conrad, M.; Dixon, S.J.; Fulda, S.; Gascon, S.; Hatzios, S.K.; Kagan, V.E.; et al. Ferroptosis: A Regulated Cell Death Nexus Linking Metabolism, Redox Biology, and Disease. Cell 2017, 171, 273–285. [Google Scholar] [CrossRef]
- Yang, C.; Wang, M.; Chang, M.; Yuan, M.; Zhang, W.; Tan, J.; Ding, B.; Ma, P.; Lin, J. Heterostructural Nanoadjuvant CuSe/CoSe2 for Potentiating Ferroptosis and Photoimmunotherapy through Intratumoral Blocked Lactate Efflux. J. Am. Chem. Soc. 2023, 145, 7205–7217. [Google Scholar] [CrossRef] [PubMed]
- Luo, L.; Wang, H.; Tian, W.; Li, X.; Zhu, Z.; Huang, R.; Luo, H. Targeting ferroptosis-based cancer therapy using nanomaterials: Strategies and applications. Theranostics 2021, 11, 9937–9952. [Google Scholar] [CrossRef] [PubMed]
- Yu, B.; Choi, B.; Li, W.; Kim, D.H. Magnetic field boosted ferroptosis-like cell death and responsive MRI using hybrid vesicles for cancer immunotherapy. Nat. Commun. 2020, 11, 3637. [Google Scholar] [CrossRef] [PubMed]
- Zafar, H.; Raza, F.; Ma, S.; Wei, Y.; Zhang, J.; Shen, Q. Recent progress on nanomedicine-induced ferroptosis for cancer therapy. Biomater. Sci. 2021, 9, 5092–5115. [Google Scholar] [CrossRef] [PubMed]
- Du, Y.; Zhang, R.; Yang, J.; Liu, S.; Zhou, J.; Zhao, R.; He, F.; Zhang, Y.; Yang, P.; Lin, J. A “Closed-Loop” Therapeutic Strategy Based on Mutually Reinforced Ferroptosis and Immunotherapy. Adv. Funct. Mater. 2022, 32, e2111784. [Google Scholar] [CrossRef]
- Jiang, Q.; Wang, K.; Zhang, X.; Ouyang, B.; Liu, H.; Pang, Z.; Yang, W. Platelet Membrane-Camouflaged Magnetic Nanoparticles for Ferroptosis-Enhanced Cancer Immunotherapy. Small 2020, 16, e2001704. [Google Scholar] [CrossRef]
- Ishimwe, N.; Zhang, W.; Qian, J.; Zhang, Y.; Wen, L. Autophagy regulation as a promising approach for improving cancer immunotherapy. Cancer Lett. 2020, 475, 34–42. [Google Scholar] [CrossRef]
- Xia, H.; Green, D.R.; Zou, W. Autophagy in tumour immunity and therapy. Nat. Rev. Cancer 2021, 21, 281–297. [Google Scholar] [CrossRef]
- Yu, N.; Ding, M.; Wang, F.; Zhou, J.; Shi, X.; Cai, R.; Li, J. Near-infrared photoactivatable semiconducting polymer nanocomplexes with bispecific metabolism interventions for enhanced cancer immunotherapy. Nano Today 2022, 46, 101600. [Google Scholar] [CrossRef]
- Chen, M.; Yang, D.; Sun, Y.; Liu, T.; Wang, W.; Fu, J.; Wang, Q.; Bai, X.; Quan, G.; Pan, X.; et al. In Situ Self-Assembly Nanomicelle Microneedles for Enhanced Photoimmunotherapy via Autophagy Regulation Strategy. ACS Nano 2021, 15, 3387–3401. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Li, M.; Ren, K.; Xia, C.; Li, J.; Yu, Q.; Qiu, Y.; Lu, Z.; Long, Y.; Zhang, Z.; et al. On-Demand Autophagy Cascade Amplification Nanoparticles Precisely Enhanced Oxaliplatin-Induced Cancer Immunotherapy. Adv. Mater. 2020, 32, e2002160. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guo, Y.; Ma, R.; Zhang, M.; Cao, Y.; Zhang, Z.; Yang, W. Nanotechnology-Assisted Immunogenic Cell Death for Effective Cancer Immunotherapy. Vaccines 2023, 11, 1440. https://doi.org/10.3390/vaccines11091440
Guo Y, Ma R, Zhang M, Cao Y, Zhang Z, Yang W. Nanotechnology-Assisted Immunogenic Cell Death for Effective Cancer Immunotherapy. Vaccines. 2023; 11(9):1440. https://doi.org/10.3390/vaccines11091440
Chicago/Turabian StyleGuo, Yichen, Rong Ma, Mengzhe Zhang, Yongjian Cao, Zhenzhong Zhang, and Weijing Yang. 2023. "Nanotechnology-Assisted Immunogenic Cell Death for Effective Cancer Immunotherapy" Vaccines 11, no. 9: 1440. https://doi.org/10.3390/vaccines11091440
APA StyleGuo, Y., Ma, R., Zhang, M., Cao, Y., Zhang, Z., & Yang, W. (2023). Nanotechnology-Assisted Immunogenic Cell Death for Effective Cancer Immunotherapy. Vaccines, 11(9), 1440. https://doi.org/10.3390/vaccines11091440






