Acceptance of Flu Vaccine among Parents of Diabetic Children in Jordan
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data collection and Study Instruments
2.1.1. Customized Questionnaire
2.1.2. Questionnaire Validation
2.1.3. The Validated Arabic Adaptation of the Summary of Diabetes Self-Care Activities Measure (SDSCA)
2.2. Sample Size Calculation
2.3. Statistical Analysis
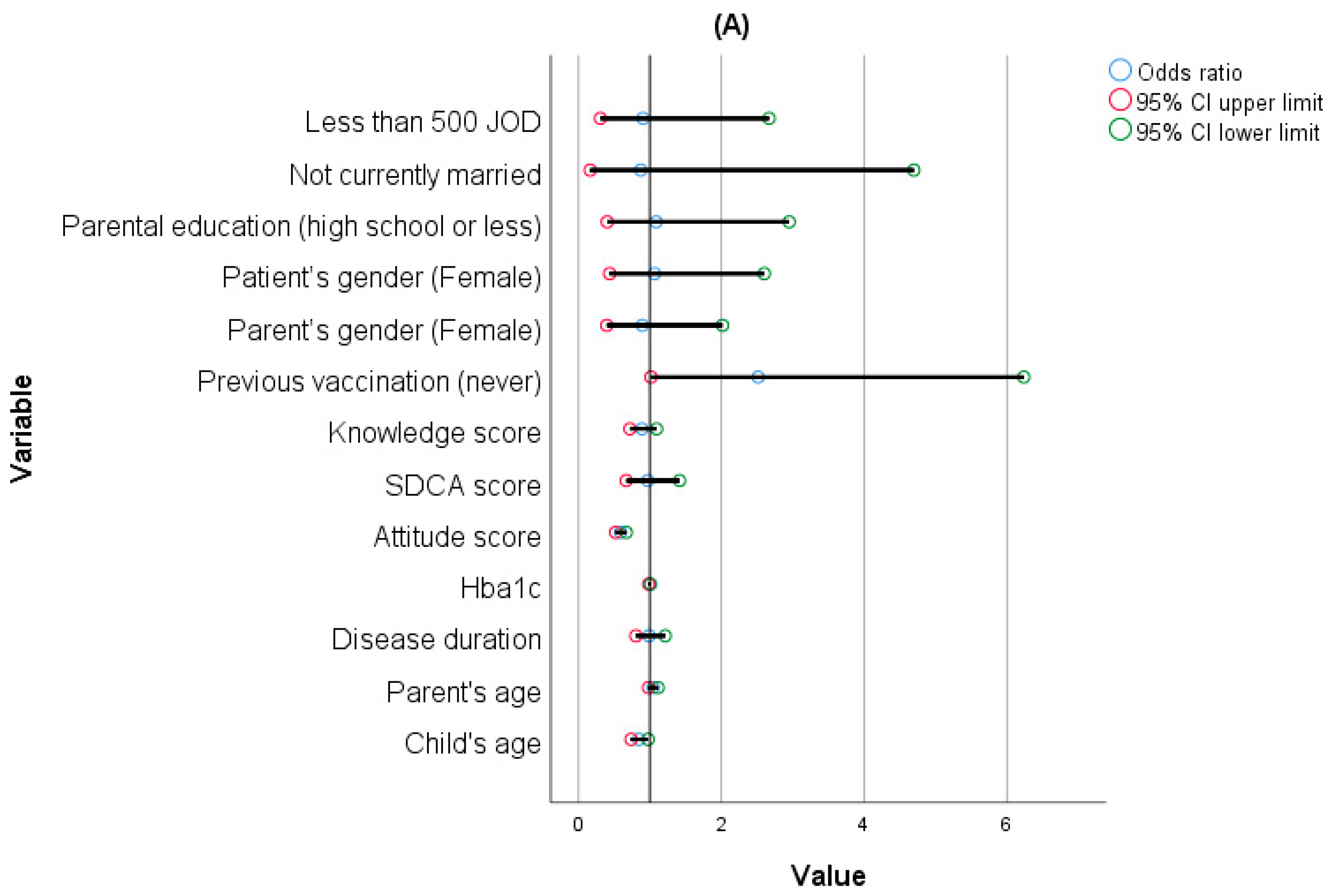
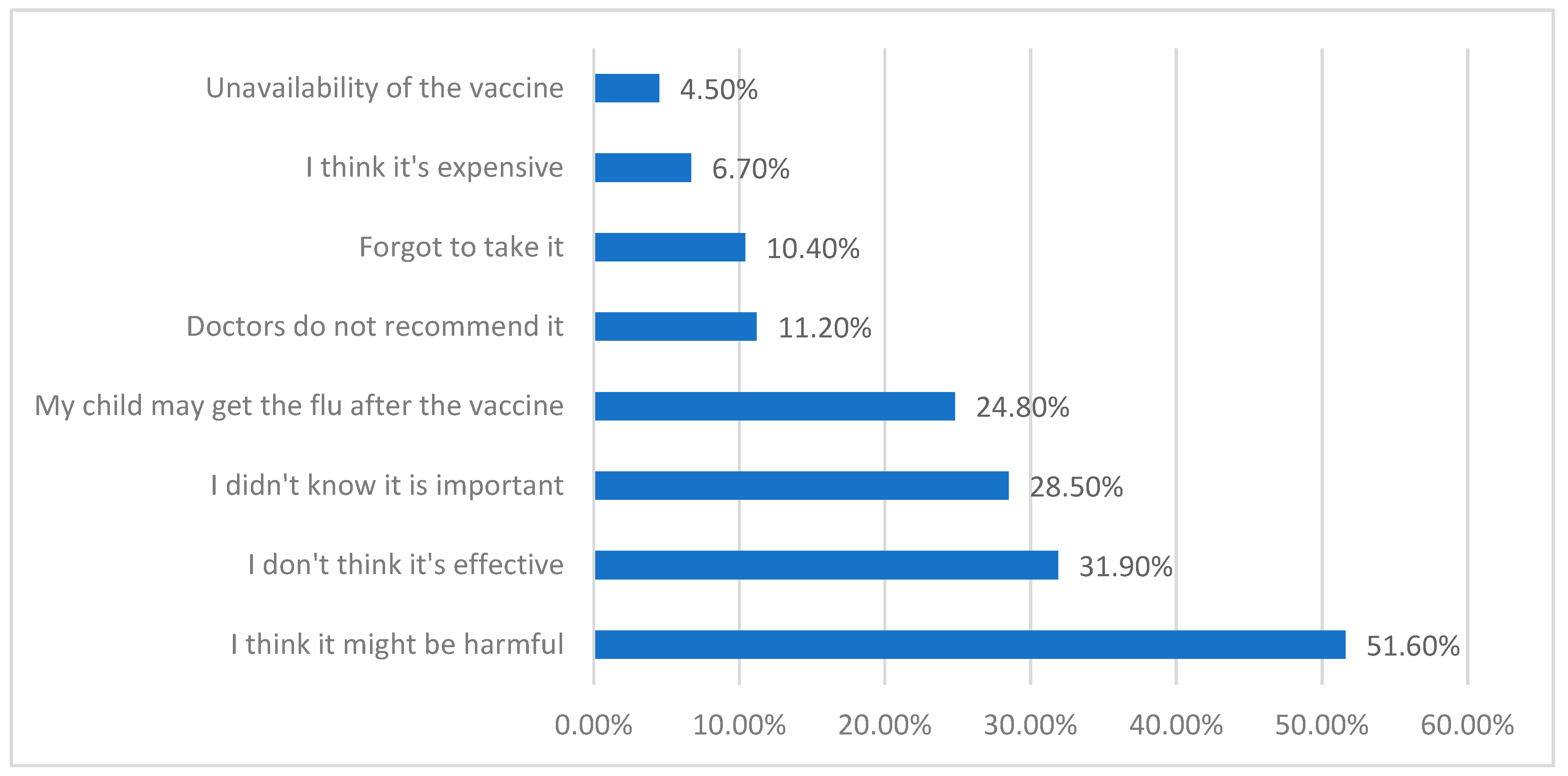
3. Results
4. Discussion
Strengths, Limitations, and Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Daryabor, G.; Atashzar, M.R.; Kabelitz, D.; Meri, S.; Kalantar, K. The Effects of Type 2 Diabetes Mellitus on Organ Metabolism and the Immune System. Front. Immunol. 2020, 11, 1582. [Google Scholar] [CrossRef]
- Diabetes. Available online: https://www.who.int/health-topics/diabetes#tab=tab_1 (accessed on 22 January 2024).
- Olokoba, A.B.; Obateru, O.A.; Olokoba, L.B. Type 2 Diabetes Mellitus: A Review of Current Trends. Oman Med. J. 2012, 27, 269–273. [Google Scholar] [CrossRef]
- Hiasat, D.A.; Salih, M.B.; Abu Jaber, A.H.; Abubaker, O.F.; Qandeel, Y.A.; Saleem, B.A.; Aburumman, S.I.; Al-Sayyed, A.R.H.; Hussein, T.I.; Hyassat, D. The Prevalence of Diabetes Distress among Patients with Type 2 Diabetes in Jordan. J. Taibah Univ. Med. Sci. 2023, 18, 1237–1243. [Google Scholar] [CrossRef]
- Papatheodorou, K.; Banach, M.; Bekiari, E.; Rizzo, M.; Edmonds, M. Complications of Diabetes 2017. J. Diabetes Res. 2018, 2018, 3086167. [Google Scholar] [CrossRef] [PubMed]
- Sabbah, M.M.; Hjazeen, A.A.; Arabiat, D. Adherence to Diabetes Management among School-Aged Children and Adolescents Living with Type 1 Diabetes in Jordan. J. Pediatr. Nurs. 2024, 74, 110–115. [Google Scholar] [CrossRef] [PubMed]
- Akash, M.S.H.; Rehman, K.; Fiayyaz, F.; Sabir, S.; Khurshid, M. Diabetes-Associated Infections: Development of Antimicrobial Resistance and Possible Treatment Strategies. Arch. Microbiol. 2020, 202, 953–965. [Google Scholar] [CrossRef] [PubMed]
- van Crevel, R.; van de Vijver, S.; Moore, D.A.J. The Global Diabetes Epidemic: What Does It Mean for Infectious Diseases in Tropical Countries? Lancet Diabetes Endocrinol. 2017, 5, 457–468. [Google Scholar] [CrossRef] [PubMed]
- Alhatim, N.; Al-Bashaireh, A.M.; Alqudah, O. Knowledge, Attitude, and Practice of Seasonal Influenza and Influenza Vaccine Immunization among People Visiting Primary Healthcare Centers in Riyadh, Saudi Arabia. PLoS ONE 2022, 17, e0266440. [Google Scholar] [CrossRef]
- Putri, W.C.W.S.; Muscatello, D.J.; Stockwell, M.S.; Newall, A.T. Economic Burden of Seasonal Influenza in the United States. Vaccine 2018, 36, 3960–3966. [Google Scholar] [CrossRef]
- Dicembrini, I.; Silverii, G.A.; Clerico, A.; Fornengo, R.; Gabutti, G.; Sordi, V.; Tafuri, S.; Peruzzi, O.; Mannucci, E. Influenza: Diabetes as a Risk Factor for Severe Related-Outcomes and the Effectiveness of Vaccination in Diabetic Population. A Meta-Analysis of Observational Studies. Nutr. Metab. Cardiovasc. Dis. 2023, 33, 1099–1110. [Google Scholar] [CrossRef] [PubMed]
- Mertz, D.; Kim, T.H.; Johnstone, J.; Lam, P.-P.; Science, M.; Kuster, S.P.; Fadel, S.A.; Tran, D.; Fernandez, E.; Bhatnagar, N.; et al. Populations at Risk for Severe or Complicated Influenza Illness: Systematic Review and Meta-Analysis. BMJ 2013, 347, f5061. [Google Scholar] [CrossRef] [PubMed]
- SAGE Working Group. A Background Paper on Influenza Vaccines and Immunization; World Health Organization: Geneva, Switzerland, 2012; p. 463. [Google Scholar]
- Bechini, A.; Ninci, A.; Del Riccio, M.; Biondi, I.; Bianchi, J.; Bonanni, P.; Mannucci, E.; Monami, M. Impact of Influenza Vaccination on All-Cause Mortality and Hospitalization for Pneumonia in Adults and the Elderly with Diabetes: A Meta-Analysis of Observational Studies. Vaccines 2020, 8, 263. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.-S.; Chang, C.-C.; Yeh, C.-C.; Chang, Y.-C.; Chen, T.-L.; Liao, C.-C. Outcomes Following Diabetes Admission in Patients Who Had Influenza Vaccination: A Population-Based Cohort Study. Diabetes Res. Clin. Pract. 2022, 189, 109930. [Google Scholar] [CrossRef] [PubMed]
- Modin, D.; Claggett, B.; Køber, L.; Schou, M.; Jensen, J.U.S.; Solomon, S.D.; Vardeny, O.; Knop, F.K.; Nielsen, S.D.; Fralick, M.; et al. Influenza Vaccination Is Associated with Reduced Cardiovascular Mortality in Adults with Diabetes: A Nationwide Cohort Study. Diabetes Care 2020, 43, 2226–2233. [Google Scholar] [CrossRef]
- Hajjo, R.; Sabbah, D.A.; Bardaweel, S.K.; Tropsha, A. Shedding the Light on Post-Vaccine Myocarditis and Pericarditis in COVID-19 and Non-COVID-19 Vaccine Recipients. Vaccines 2021, 9, 1186. [Google Scholar] [CrossRef]
- Wang, Y.; Cheng, M.; Wang, S.; Wu, F.; Yan, Q.; Yang, Q.; Li, Y.; Guo, X.; Fu, C.; Shi, Y.; et al. Vaccination Coverage with the Pneumococcal and Influenza Vaccine among Persons with Chronic Diseases in Shanghai, China, 2017. BMC Public Health 2020, 20, 359. [Google Scholar] [CrossRef]
- Santaularia, J.; Hou, W.; Perveen, G.; Welsh, E.; Faseru, B. Prevalence of Influenza Vaccination and Its Association with Health Conditions and Risk Factors among Kansas Adults in 2013: A Cross-Sectional Study. BMC Public Health 2016, 16, 185. [Google Scholar] [CrossRef]
- Ababneh, M.; Jaber, M.; Rababa’h, A.; Ababneh, F. Seasonal Influenza Vaccination among Older Adults in Jordan: Prevalence, Knowledge, and Attitudes. Hum. Vaccines Immunother. 2020, 16, 2252–2256. [Google Scholar] [CrossRef]
- Sato, A.P.S.; Antunes, J.L.F.; Moura, R.F.; de Andrade, F.B.; Duarte, Y.A.O.; Lebrão, M.L. Factors Associated to Vaccination against Influenza among Elderly in a Large Brazilian Metropolis. PLoS ONE 2015, 10, e0123840. [Google Scholar] [CrossRef]
- Bdair, O.A.; Bdair, I.A.; Gogazeh, E.; Al-Fawares, O.; Alwadi, M.; Badaineh, R.; Al-Tarawneh, F. A Cross-Sectional Survey of Knowledge, Attitude, and Practices Regarding Influenza Vaccination among Jordanians Aged 18-64 Years with Chronic Diseases. Turk. J. Pharm. Sci. 2023, 20, 310–317. [Google Scholar] [CrossRef]
- Al-Qerem, W.; Jarab, A.; Hammad, A.; Alasmari, F.; Ling, J.; Alsajri, A.H.; Al-Hishma, S.W.; Abu Heshmeh, S.R. Iraqi Parents’ Knowledge, Attitudes, and Practices towards Vaccinating Their Children: A Cross-Sectional Study. Vaccines 2022, 10, 820. [Google Scholar] [CrossRef] [PubMed]
- Zhao, M.; Liu, H.; Qu, S.; He, L.; Campy, K.S. Factors Associated with Parental Acceptance of Influenza Vaccination for Their Children: The Evidence from Four Cities of China. Hum. Vaccin. Immunother. 2021, 17, 457–464. [Google Scholar] [CrossRef] [PubMed]
- Camurdan, M.O.; Duyan Camurdan, A.; Beyazova, U.; Bideci, A. The Rate of Seasonal Influenza Vaccination in Diabetic Children, the Effect of Recommendation and the Factors Influencing the Acceptance of Recommendation: An Interventional Study. Balk. Med. J. 2012, 29, 434–439. [Google Scholar] [CrossRef] [PubMed]
- Tan, E.K.; Lim, L.H.; Teoh, Y.L.; Ong, G.; Bock, H.L. Influenza and Seasonal Influenza Vaccination among Diabetics in Singapore: Knowledge, Attitudes and Practices. Singap. Med. J. 2010, 51, 623–630. [Google Scholar]
- Olatunbosun, O.D.; Esterhuizen, T.M.; Wiysonge, C.S. A Cross Sectional Survey to Evaluate Knowledge, Attitudes and Practices Regarding Seasonal Influenza and Influenza Vaccination among Diabetics in Pretoria, South Africa. Vaccine 2017, 35, 6375–6386. [Google Scholar] [CrossRef]
- Alsufyani, S. Acceptance Rate of Influenza Vaccination among Patients with Type II Diabetes. J. Fam. Med. Prim. Care 2022, 11, 44. [Google Scholar] [CrossRef]
- Lin, C.J.; Nowalk, M.P.; Zimmerman, R.K.; Ko, F.-S.; Zoffel, L.; Hoberman, A.; Kearney, D.H. Beliefs and Attitudes about Influenza Immunization among Parents of Children with Chronic Medical Conditions over a Two-Year Period. J. Urban Health 2006, 83, 874–883. [Google Scholar] [CrossRef]
- Fadl, N.; Al Awaidy, S.T.; Elshabrawy, A.; Makhlouf, M.S.A.H.; Ibrahim, S.A.; Abdel-Rahman, S.; Tookhy, N.A.; Alsalmani, A.; Al-Saeedi, M.; Al-Sawalha, I.; et al. Determinants of Parental Seasonal Influenza Vaccine Hesitancy in the Eastern Mediterranean Region: A Cross-Sectional Study. Front. Public Health 2023, 11, 1132798. [Google Scholar] [CrossRef]
- Kempe, A.; Saville, A.W.; Albertin, C.; Zimet, G.; Breck, A.; Helmkamp, L.; Vangala, S.; Dickinson, L.M.; Rand, C.; Humiston, S.; et al. Parental Hesitancy about Routine Childhood and Influenza Vaccinations: A National Survey. Pediatrics 2020, 146, e20193852. [Google Scholar] [CrossRef]
- Zalloum, W.A.; Elayeh, E.R.; Ali, B.A.H.; Zalloum, N. Perception, Knowledge and Attitude towards Influenza Vaccine during COVID-19 Pandemic in Jordanian Population. Eur. J. Integr. Med. 2022, 49, 102100. [Google Scholar] [CrossRef]
- Al-Qerem, W.; Jarab, A.; AlBawab, A.Q.; Hammad, A.; Alazab, B.; Abu Husein, D.; Eberhardt, J.; Alasmari, F. Examining Influenza Vaccination Patterns and Barriers: Insights into Knowledge, Attitudes, and Practices among Diabetic Adults (A Cross-Sectional Survey). Vaccines 2023, 11, 1689. [Google Scholar] [CrossRef]
- Al-Qerem, W.; Jarab, A.; Hammad, A.; Alasmari, F.; Ling, J.; Al-Zayadneh, E.; Al-Iede, M.; Alazab, B.; Hajeer, L. Knowledge, Attitudes, and Practices of Influenza Vaccination among Parents of Children with Asthma: A Cross-Sectional Study. Vaccines 2023, 11, 1074. [Google Scholar] [CrossRef] [PubMed]
- Al Hashmi, I.; Al-Noumani, H.; Alaloul, F.; Murthi, S.; Khalaf, A. Translation and Psychometric Validation of the Arabic Version of Summary of the Diabetes Self-Care Activities (SDSCA) among Pregnant Women with Gestational Diabetes. BMC Pregnancy Childbirth 2022, 22, 563. [Google Scholar] [CrossRef]
- Krejcie, R.V.; Morgan, D.W. Determining Sample Size for Research Activities. Educ. Psychol. Meas. 1970, 30, 607–610. [Google Scholar] [CrossRef]
- Dyda, A.; King, C.; Dey, A.; Leask, J.; Dunn, A.G. A Systematic Review of Studies That Measure Parental Vaccine Attitudes and Beliefs in Childhood Vaccination. BMC Public Health 2020, 20, 1253. [Google Scholar] [CrossRef]
- Strelitz, B.; Gritton, J.; Klein, E.J.; Bradford, M.C.; Follmer, K.; Zerr, D.M.; Englund, J.A.; Opel, D.J. Parental Vaccine Hesitancy and Acceptance of Seasonal Influenza Vaccine in the Pediatric Emergency Department. Vaccine 2015, 33, 1802–1807. [Google Scholar] [CrossRef] [PubMed]
- Goss, M.D.; Temte, J.L.; Barlow, S.; Temte, E.; Bell, C.; Birstler, J.; Chen, G. An Assessment of Parental Knowledge, Attitudes, and Beliefs Regarding Influenza Vaccination. Vaccine 2020, 38, 1565–1571. [Google Scholar] [CrossRef]
- Dardas, L.A.; Al-leimon, O.; Jaber, A.R.; Saadeh, M.; Al-leimon, A.; Al-Hurani, A.; Jaber, A.-R.; Aziziye, O.; Al-salieby, F.; Aljahalin, M.; et al. Flu Shots Unveiled: A Global Systematic Review of Healthcare Providers’ Uptake of, Perceptions, and Attitudes toward Influenza Vaccination. Vaccines 2023, 11, 1760. [Google Scholar] [CrossRef] [PubMed]
- Dopelt, K.; Abudin, A.; Yukther, S.; Shmukler, T.; Davidovitch, N. The Association between Levels of Trust in the Healthcare System and Influenza Vaccine Hesitancy among College Students in Israel. Vaccines 2023, 11, 1728. [Google Scholar] [CrossRef]
- Bach, A.T.; Kang, A.Y.; Lewis, J.; Xavioer, S.; Portillo, I.; Goad, J.A. Addressing Common Barriers in Adult Immunizations: A Review of Interventions. Expert Rev. Vaccines 2019, 18, 1167–1185. [Google Scholar] [CrossRef]
- Price, T.; McColl, E.; Visram, S. Barriers and Facilitators of Childhood Flu Vaccination: The Views of Parents in North East England. J. Public Health 2022, 30, 2619–2626. [Google Scholar] [CrossRef] [PubMed]
- Flood, E.M.; Rousculp, M.D.; Ryan, K.J.; Beusterien, K.M.; Divino, V.M.; Toback, S.L.; Sasané, M.; Block, S.L.; Hall, M.C.; Mahadevia, P.J. Parents’ Decision-Making Regarding Vaccinating Their Children against Influenza: A Web-Based Survey. Clin. Ther. 2010, 32, 1448–1467. [Google Scholar] [CrossRef]
- Takagi, M.A.; Hess, S.; Smith, Z.; Gawronski, K.; Kumar, A.; Horsley, J.; Haddad, N.; Noveloso, B.; Zyzanski, S.; Ragina, N. The Impact of Educational Interventions on COVID-19 and Vaccination Attitudes among Patients in Michigan: A Prospective Study. Front. Public Health 2023, 11, 1144659. [Google Scholar] [CrossRef] [PubMed]
- Al-Qerem, W. Flu vaccine acceptance among parents of diabetic Jordanian children [Data set]. Zenodo 2024. [Google Scholar] [CrossRef]

| Median (25–75) Or Frequency (%) | ||
|---|---|---|
| Child’s age | 10.0 (6.0–13.0) | |
| Parent’s age | 37 (32–43) | |
| Child’s gender | Female | 210 (51.9%) |
| Male | 195 (48.1%) | |
| Parent’s gender | Female | 253 (62.5%) |
| Male | 152 (37.5%) | |
| Level of education | High school or lower | 244 (60.2%) |
| University/college degree | 161 (39.8%) | |
| Social status | Other | 28 (6.9%) |
| Married | 377 (93.1%) | |
| Income (Jordanian Dinars) * | Less than 500 | 297 (73.3%) |
| 500 or more | 108 (26.7%) | |
| Hba1c | 9.0 (8.0–10.0) | |
| Disease duration | 4.0 (2.0–5.0) | |
| Intent to vaccinate your child this year? | Yes | 93 (23%) |
| Not sure | 118 (29.1) | |
| No | 194 (47.9) | |
| Previous flu vaccination | Never | 277 (68.4) |
| One | 55 (13.5%) | |
| More than one | 47 (11.6%) | |
| Annually | 26 (6.4%) | |
| No | Unsure | Yes | |
|---|---|---|---|
| Do you know how to measure your child’s blood sugar levels at home? * | 33 (8.1%) | 8 (2%) | 364 (89.9%) |
| Are you aware that weight loss can be a sign of diabetes? * | 65 (16%) | 100 (24.7%) | 240 (59.3%) |
| Is diabetes hereditary? * | 167 (41.2%) | 21 (5.2%) | 217 (53.6%) |
| Is diabetes a chronic disease? * | 36 (8.9%) | 9 (2.2%) | 360 (88.9%) |
| Can you recognize the symptoms of low blood sugar? * | 48 (11.9%) | 9 (2.2%) | 348 (85.9%) |
| Is there a vaccine against the flu? * | 35 (8.6%) | 125 (30.9%) | 245 (60.5%) |
| Does the vaccine have side effects? * | 35 (8.6%) | 249 (61.5%) | 121 (29.9%) |
| The flu is caused by bacteria ** | 207 (51.1%) | 86 (21.2%) | 112 (27.7%) |
| The flu can spread from one person to another. * | 18 (4.4%) | 11 (2.7%) | 376 (92.8%) |
| Do you know how to properly use diabetes medications? * | 22 (5.4%) | 4 (1.0%) | 397 (93.6%) |
| Can antibiotics be used to treat the flu? ** | 146 (36%) | 24 (5.9%) | 235 (58.0%) |
| When is the appropriate time to take the flu vaccine? # | |||
| January–March | September–October | November–December | Unsure |
| 16 (4.0%) | 114 (28.1%) | 42 (10.4%) | 233 (57.5%) |
| Strongly Disagree | Disagree | Neutral | Agree/Strongly Agree | |
|---|---|---|---|---|
| I believe that my child must receive the flu vaccination | 29 (7.2%) | 130 (32.1%) | 77 (19%) | 169 (41.7%) |
| It is easy to reach the pharmacy/hospital to receive a flu vaccination | 49 (12.1%) | 60 (14.8%) | 60 (14.8%) | 236 (58.2%) |
| My physician believes that my child should receive the flu vaccine | 25 (6.2%) | 85 (21.1%) | 165 (41%) | 127 (31.6%) |
| Flu vaccination prevents infection by the influenza virus | 8 (2%) | 76 (18.9%) | 115 (28.6%) | 203 (50.4%) |
| The flu vaccination may cause complications/troubles for my child * | 19 (4.7%) | 70 (17.3%) | 100 (24.8%) | 215 (53.2%) |
| I believe that my child gets sick because of the flu shot * | 19 (4.7%) | 85 (21%) | 105 (25.9%) | 196 (48.4%) |
| I am worried about the chances of my child contracting the flu because of the flu vaccine * | 20 (5%) | 84 (20.9%) | 77 (19.2%) | 221 (55%) |
| Catching the flu is not a problem for my child * | 75 (18.6%) | 149 (37%) | 35 (8.7%) | 144 (35.7%) |
| Median | Percentile 25 | Percentile 75 | |
|---|---|---|---|
| How many of the last SEVEN DAYS has your child followed a healthful eating plan? | 5 | 3 | 7 |
| On average, over the past month, how many DAYS PER WEEK has your child followed his/her eating plan? | 4 | 3 | 7 |
| On how many of the last SEVEN DAYS did your child eat five or more servings of fruits and vegetables? | 3 | 2 | 7 |
| On how many of the last SEVEN DAYS did your child eat high-fat foods such as red meat or full-fat dairy products? * | 2 | 1 | 3 |
| On how many of the last SEVEN DAYS did your child participate in at least 30 min of physical activity? (Total minutes of continuous activity, including walking). | 5 | 3 | 6 |
| On how many of the last SEVEN DAYS did your child participate in a specific exercise session (such as swimming, walking, biking) | 2 | 1 | 5 |
| On how many of the last SEVEN DAYS did you test your child’s blood sugar? | 7 | 5 | 7 |
| On how many of the last SEVEN DAYS did you test your child’s blood sugar the number of times recommended by your health care provider? | 7 | 5 | 7 |
| On how many of the last SEVEN DAYS did you check your child’s feet? | 5 | 2 | 7 |
| On how many of the last SEVEN DAYS did you inspect the inside of your child’s shoes? | 5 | 1 | 7 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Qerem, W.; Jarab, A.; Eberhardt, J.; Alasmari, F.; Hammad, A.; Hour, S.A. Acceptance of Flu Vaccine among Parents of Diabetic Children in Jordan. Vaccines 2024, 12, 262. https://doi.org/10.3390/vaccines12030262
Al-Qerem W, Jarab A, Eberhardt J, Alasmari F, Hammad A, Hour SA. Acceptance of Flu Vaccine among Parents of Diabetic Children in Jordan. Vaccines. 2024; 12(3):262. https://doi.org/10.3390/vaccines12030262
Chicago/Turabian StyleAl-Qerem, Walid, Anan Jarab, Judith Eberhardt, Fawaz Alasmari, Alaa Hammad, and Sarah Abu Hour. 2024. "Acceptance of Flu Vaccine among Parents of Diabetic Children in Jordan" Vaccines 12, no. 3: 262. https://doi.org/10.3390/vaccines12030262
APA StyleAl-Qerem, W., Jarab, A., Eberhardt, J., Alasmari, F., Hammad, A., & Hour, S. A. (2024). Acceptance of Flu Vaccine among Parents of Diabetic Children in Jordan. Vaccines, 12(3), 262. https://doi.org/10.3390/vaccines12030262








