Enhanced Immune Responses in Mice by Combining the Mpox Virus B6R-Protein and Aluminum Hydroxide-CpG Vaccine Adjuvants
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethical Approval
2.2. Biological Compounds and Chemicals
2.3. Immunization and Sampling
2.4. ELISA Assays
2.5. Neutralization Assays
2.6. ELISPOT Assays
2.7. Flow Cytometry Analysis
2.8. Statistical Methods
3. Results
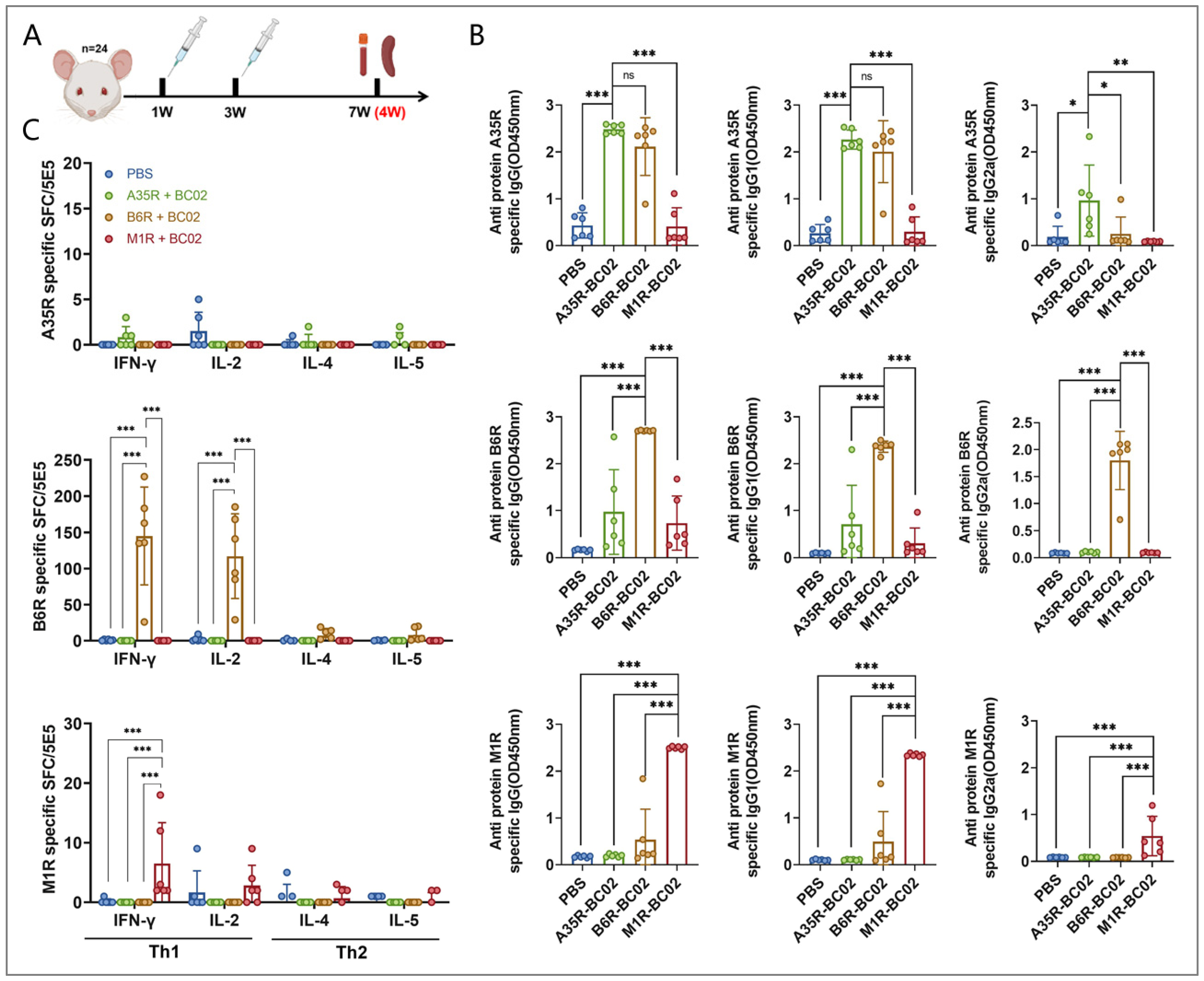
3.1. B6R Is More Effective than A35R and M1R in Inducing Cellular Immunity
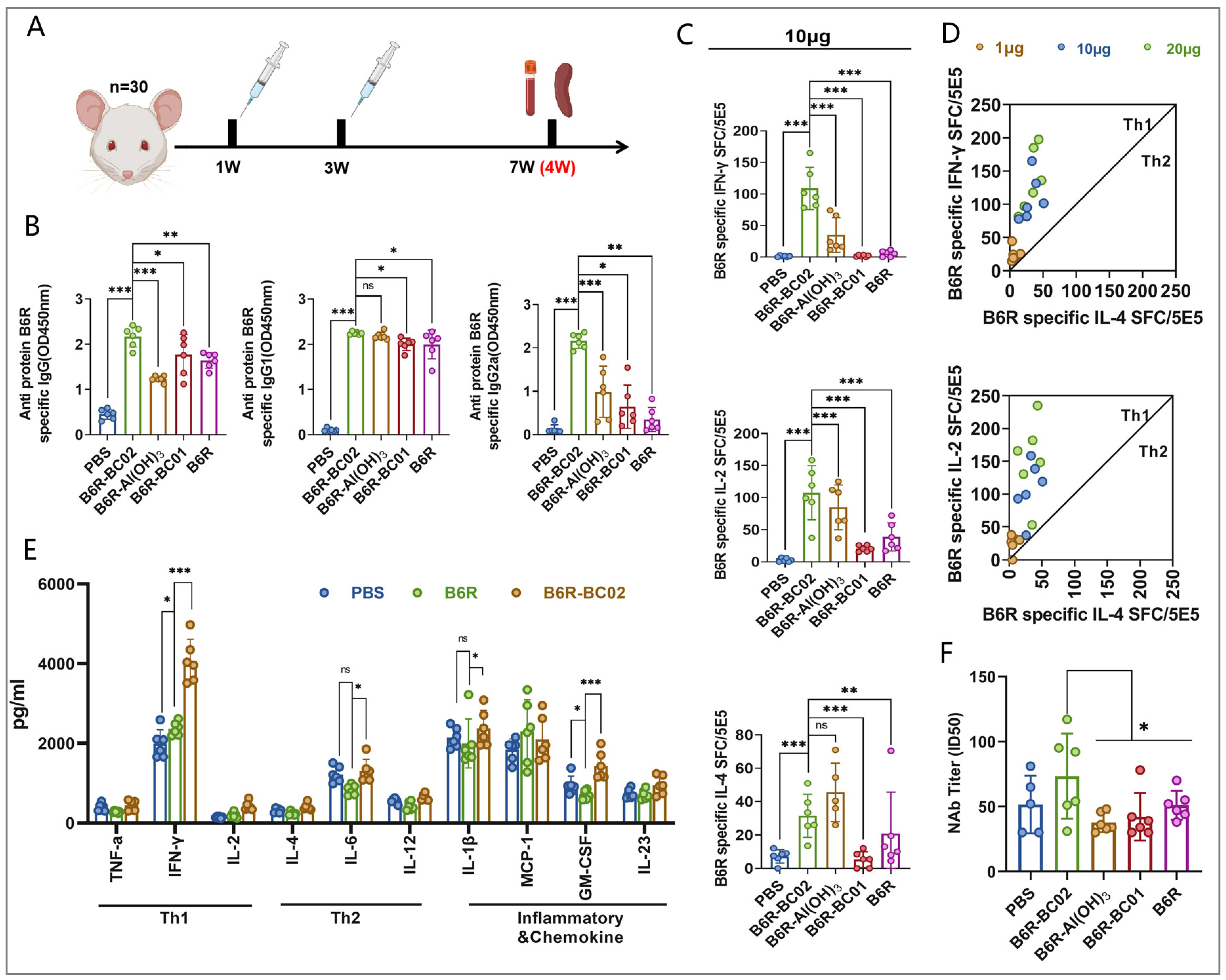
3.2. BC02 Compound Adjuvant Significantly Enhances Cellular and Humoral Immunity via B6R
3.3. BC02-B6R Induces Longer-Term Antibody Responses in Mice
3.4. BC02-B6R Induces Sustained Cellular Immune Response in Mice
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Facciola, A.; Visalli, G.; Lagana, A.; Di Pietro, A. An Overview of Vaccine Adjuvants: Current Evidence and Future Perspectives. Vaccines 2022, 10, 819. [Google Scholar] [CrossRef] [PubMed]
- Verma, S.K.; Mahajan, P.; Singh, N.K.; Gupta, A.; Aggarwal, R.; Rappuoli, R.; Johri, A.K. New-age vaccine adjuvants, their development, and future perspective. Front. Immunol. 2023, 14, 1043109. [Google Scholar] [CrossRef] [PubMed]
- Ko, E.J.; Kang, S.M. Immunology and efficacy of MF59-adjuvanted vaccines. Hum. Vaccin. Immunother. 2018, 14, 3041–3045. [Google Scholar] [CrossRef] [PubMed]
- Beran, J. Safety and immunogenicity of a new hepatitis B vaccine for the protection of patients with renal insufficiency including pre-haemodialysis and haemodialysis patients. Expert. Opin. Biol. Ther. 2008, 8, 235–247. [Google Scholar] [CrossRef] [PubMed]
- McKeage, K.; Romanowski, B. AS04-adjuvanted human papillomavirus (HPV) types 16 and 18 vaccine (Cervarix®): A review of its use in the prevention of premalignant cervical lesions and cervical cancer causally related to certain oncogenic HPV types. Drugs 2011, 71, 465–488. [Google Scholar]
- Edwards, K.; Lambert, P.H.; Black, S. Narcolepsy and Pandemic Influenza Vaccination: What We Need to Know to be Ready for the Next Pandemic. Pediatr. Infect. Dis. J. 2019, 38, 873–876. [Google Scholar] [CrossRef] [PubMed]
- Syed, Y.Y. Recombinant Zoster Vaccine (Shingrix®): A Review in Herpes Zoster. Drugs Aging 2018, 35, 1031–1040. [Google Scholar] [CrossRef] [PubMed]
- Syed, Y.Y. RTS,S/AS01 malaria vaccine (Mosquirix®): A profile of its use. Drugs Ther. Perspect. 2022, 38, 373–381. [Google Scholar] [CrossRef] [PubMed]
- Campbell, J.D. Development of the CpG Adjuvant 1018: A Case Study. Methods Mol. Biol. 2017, 1494, 15–27. [Google Scholar]
- Stertman, L.; Palm, A.E.; Zarnegar, B.; Carow, B.; Lunderius Andersson, C.; Magnusson, S.E.; Carnrot, C.; Shinde, V.; Smith, G.; Glenn, G.; et al. The Matrix-M adjuvant: A critical component of vaccines for the 21st century. Hum. Vaccin. Immunother. 2023, 19, 2189885. [Google Scholar] [CrossRef]
- Datoo, M.S.; Natama, H.M.; Some, A.; Bellamy, D.; Traoré, O.; Rouamba, T.; Tahita, M.C.; Ido, N.F.A.; Yameogo, P.; Valia, D.; et al. Efficacy and immunogenicity of R21/Matrix-M vaccine against clinical malaria after 2 years’ follow-up in children in Burkina Faso: A phase 1/2b randomised controlled trial. Lancet Infect. Dis. 2022, 22, 1728–1736. [Google Scholar] [CrossRef] [PubMed]
- Datoo, M.S.; Dicko, A.; Tinto, H.; Ouédraogo, J.B.; Hamaluba, M.; Olotu, A.; Beaumont, E.; Lopez, F.R.; Natama, H.M.; Weston, S.; et al. Safety and efficacy of malaria vaccine candidate R21/Matrix-M in African children: A multicentre, double-blind, randomised, phase 3 trial. Lancet 2024, 403, 533–544. [Google Scholar] [CrossRef]
- Chen, L.; Xu, M.; Wang, Z.Y.; Chen, B.W.; Du, W.X.; Su, C.; Shen, X.B.; Zhao, A.H.; Dong, N.; Wang, Y.J.; et al. The development and preliminary evaluation of a new Mycobacterium tuberculosis vaccine comprising Ag85b, HspX and CFP-10:ESAT-6 fusion protein with CpG DNA and aluminum hydroxide adjuvants. FEMS Immunol. Med. Microbiol. 2010, 59, 42–52. [Google Scholar] [CrossRef]
- Zhang, Y.; Yang, Y.C.; Zhang, J.; Bo, S.Y.; Xin, X.F.; Wang, G.Z. Immune effect of STAg combined with BCG-DNA and aluminum hydroxide adjuvant in mice. Chin. J. Biol. 2011, 24, 1177–1179. [Google Scholar]
- Li, J.L.; Fu, L.L.; Wang, G.Z.; Yang, X.M.; Zhao, A.H. Synergistic enhancement of macrophage innate immune response with BC02 complex adjuvant. Chin. J. Biol. 2018, 31, 941–948. [Google Scholar]
- Li, J.L.; Fu, L.L.; Yang, Y.; Wang, G.Z.; Zhao, A.H. Analysis of synergistic enhancement of innate immune response by BC02 compound adjuvant components. Chin. J. Biol. 2022, 35, 11–18. [Google Scholar]
- Li, J.; Fu, L.; Yang, Y.; Wang, G.; Zhao, A. Enhanced Potency and Persistence of Immunity to Varicella-Zoster Virus Glycoprotein E in Mice by Addition of a Novel BC02 Compound Adjuvant. Vaccines 2022, 10, 529. [Google Scholar] [CrossRef]
- Li, J.; Fu, L.; Guo, X.; Yang, Y.; Dong, J.; Wang, G.; Zhao, A. Novel BC02 Compound Adjuvant Enhances Adaptive and Innate Immunity Induced by Recombinant Glycoprotein E of Varicella-Zoster Virus. Vaccines 2022, 10, 2155. [Google Scholar] [CrossRef]
- Li, J.; Xie, H.; Fu, L.; Guo, X.; Dong, J.; Xu, M.; Wang, G.; Zhao, A. Comparison of the Immune Responses to Different Formulations of BC02-Adjuvanted HPV Types 16 and 18 Bivalent Vaccines in Mice. Vaccines 2023, 11, 1553. [Google Scholar] [CrossRef]
- World Health Organization. Vaccines and Immunization for Monkeypox; WHO: Geneva, Switzerland, 2022.
- Jhancy, M. Poxvirus Vaccines: Past, Present, and Future. Adv. Exp. Med. Biol. 2024, 1451, 273–287. [Google Scholar]
- Berhanu, A.; Prigge, J.T.; Silvera, P.M.; Honeychurch, K.M.; Hruby, D.E.; Grosenbach, D.W. Treatment with the smallpox antiviral tecovirimat (ST-246) alone or in combination with ACAM2000 vaccination is effective as a postsymptomatic therapy for monkeypox virus infection. Antimicrob. Agents Chemother. 2015, 59, 4296–4300. [Google Scholar] [CrossRef] [PubMed]
- Pittman, P.R.; Hahn, M.; Lee, H.S.; Koca, C.; Samy, N.; Schmidt, D.; Hornung, J.; Weidenthaler, H.; Heery, C.R.; Meyer, T.P.; et al. Phase 3 Efficacy Trial of Modified Vaccinia Ankara as a Vaccine against Smallpox. N. Engl. J. Med. 2019, 381, 1897–1908. [Google Scholar] [CrossRef] [PubMed]
- Reina, J.; Iglesias, C. Vaccines against monkeypox. Med. Clin. (Engl. Ed.) 2023, 160, 305–309. [Google Scholar] [CrossRef] [PubMed]
- Nalca, A.; Zumbrun, E.E. ACAM2000: The new smallpox vaccine for United States Strategic National Stockpile. Drug Des. Dev. Ther. 2010, 4, 71–79. [Google Scholar] [CrossRef]
- Weidenthaler, H.; Vidojkovic, S.; Martin, B.K.; De Moerlooze, L. Real-world safety data for MVA-BN: Increased frequency of syncope following intradermal administration for immunization against mpox disease. Vaccine 2024. [Google Scholar] [CrossRef] [PubMed]
- Dashraath, P.; Nielsen-Saines, K.; Mattar, C.; Musso, D.; Tambyah, P.; Baud, D. Guidelines for pregnant individuals with monkeypox virus exposure. Lancet 2022, 400, 21–22. [Google Scholar] [CrossRef] [PubMed]
- Tomita, N.; Terada-Hirashima, J.; Uemura, Y.; Shimizu, Y.; Iwasaki, H.; Yano, R.; Suzuki, T.; Saito, S.; Okumura, N.; Sugiura, W.; et al. An open-label, non-randomized study investigating the safety and efficacy of smallpox vaccine, LC16, as post-exposure prophylaxis for mpox. Hum. Vaccin. Immunother. 2023, 19, 2242219. [Google Scholar] [CrossRef]
- Zaeck, L.M.; Lamers, M.M.; Verstrepen, B.E.; Bestebroer, T.M.; van Royen, M.E.; Götz, H.; Shamier, M.C.; van Leeuwen, L.P.M.; Schmitz, K.S.; Alblas, K.; et al. Low levels of monkeypox virus-neutralizing antibodies after MVA-BN vaccination in healthy individuals. Nat. Med. 2023, 29, 270–278. [Google Scholar] [CrossRef]
- Moschetta, N.; Raccagni, A.R.; Bianchi, M.; Diotallevi, S.; Lolatto, R.; Candela, C.; Foppa, C.U.; Gismondo, M.R.; Castagna, A.; Nozza, S.; et al. Mpox neutralising antibodies at 6 months from mpox infection or MVA-BN vaccination: A comparative analysis. Lancet Infect. Dis. 2023, 23, e455–e456. [Google Scholar] [CrossRef]
- Cohn, H.; Bloom, N.; Cai, G.Y.; Clark, J.J.; Tarke, A.; Bermúdez-González, M.C.; Altman, D.R.; Lugo, L.A.; Lobo, F.P.; Marquez, S.; et al. Mpox vaccine and infection-driven human immune signatures: An immunological analysis of an observational study. Lancet Infect. Dis. 2023, 23, 1302–1312. [Google Scholar] [CrossRef]
- Morino, E.; Mine, S.; Tomita, N.; Uemura, Y.; Shimizu, Y.; Saito, S.; Suzuki, T.; Okumura, N.; Iwasaki, H.; Terada, J.; et al. Mpox Neutralizing Antibody Response to LC16m8 Vaccine in Healthy Adults. NEJM Evid. 2024, 3. [Google Scholar] [CrossRef] [PubMed]
- Hazra, A.; Rusie, L.; Hedberg, T.; Schneider, J.A. Human Monkeypox Virus Infection in the Immediate Period After Receiving Modified Vaccinia Ankara Vaccine. JAMA 2022, 328, 2064–2067. [Google Scholar] [CrossRef] [PubMed]
- Merad, Y.; Gaymard, A.; Cotte, L.; Perpoint, T.; Alfaiate, D.; Godinot, M.; Becker, A.; Cannesson, O.; Batalla, A.-S.; Oria-Yassir, F.; et al. Outcomes of post-exposure vaccination by modified vaccinia Ankara to prevent mpox (formerly monkeypox): A retrospective observational study in Lyon, France, June to August 2022. Euro Surveill. 2022, 27, 2200882. [Google Scholar] [CrossRef] [PubMed]
- Hooper, J.W.; Custer, D.M.; Thompson, E. Four-gene-combination DNA vaccine protects mice against a lethal vaccinia virus challenge and elicits appropriate antibody responses in nonhuman primates. Virology 2003, 306, 181–195. [Google Scholar] [CrossRef] [PubMed]
- Manes, N.P.; Estep, R.D.; Mottaz, H.M.; Moore, R.J.; Clauss, T.R.; Monroe, M.E.; Du, X.; Adkins, J.N.; Wong, S.W.; Smith, R.D. Comparative proteomics of human monkeypox and vaccinia intracellular mature and extracellular enveloped virions. Proteome Res. 2008, 7, 960–968. [Google Scholar] [CrossRef] [PubMed]
- Monticelli, S.R.; Earley, A.K.; Stone, R.; Norbury, C.C.; Ward, B.M. Vaccinia Virus Glycoproteins A33, A34, and B5 Form a Complex for Efficient Endoplasmic Reticulum to trans-Golgi Network Transport. J. Virol. 2020, 94, e02155-19. [Google Scholar] [CrossRef] [PubMed]
- Matho, M.H.; Schlossman, A.; Meng, X.; Benhnia, M.R.; Kaever, T.; Buller, M.; Doronin, K.; Parker, S.; Peters, B.; Crotty, S.; et al. Structural and Functional Characterization of Anti-A33 Antibodies Reveal a Potent Cross-Species Orthopoxviruses Neutralizer. PLoS Pathog. 2015, 11, e1005148. [Google Scholar] [CrossRef] [PubMed]
- Perdiguero, B.; Blasco, R. Interaction between vaccinia virus extracellular virus envelope A33 and B5 glycoproteins. J. Virol. 2006, 80, 8763–8777. [Google Scholar] [CrossRef]
- Doceul, V.; Hollinshead, M.; Breiman, A.; Laval, K.; Smith, G.L. Protein B5 is required on extracellular enveloped vaccinia virus for repulsion of superinfecting virions. J. Gen. Virol. 2012, 93 Pt 9, 1876–1886. [Google Scholar] [CrossRef]
- Pütz, M.M.; Midgley, C.M.; Law, M.; Smith, G.L. Quantification of antibody responses against multiple antigens of the two infectious forms of Vaccinia virus provides a benchmark for smallpox vaccination. Nat. Med. 2006, 12, 1310–1315. [Google Scholar] [CrossRef]
- Senkevich, T.G.; White, C.L.; Koonin, E.V.; Moss, B. Complete pathway for protein disulfide bond formation encoded by poxviruses. Proc. Natl. Acad. Sci. USA 2002, 99, 6667–6672. [Google Scholar] [CrossRef] [PubMed]
- Franke, C.A.; Wilson, E.M.; Hruby, D.E. Use of a cell-free system to identify the vaccinia virus L1R gene product as the major late myristylated virion protein M25. J. Virol. 1990, 64, 5988–5996. [Google Scholar] [CrossRef] [PubMed]
- Foo, C.H.; Lou, H.; Whitbeck, J.C.; Ponce-de-León, M.; Atanasiu, D.; Eisenberg, R.J.; Cohen, G.H. Vacciniavirus L1 binds to cell surfaces and blocks virus entry independently of glycosaminoglycans. Virology 2009, 385, 368–382. [Google Scholar] [CrossRef] [PubMed]
- Wolffe, E.J.; Vijaya, S.; Moss, B. A myristylated membrane protein encoded by the vaccinia virus L1R open reading frame is the target of potent neutralizing monoclonal antibodies. Virology 1995, 211, 53–63. [Google Scholar] [CrossRef] [PubMed]
- Papukashvili, D.; Rcheulishvili, N.; Liu, C.; Wang, X.; He, Y.; Wang, P.G. Strategy of developing nucleic acid-based universal monkeypox vaccine candidates. Front. Immunol. 2022, 13, 1050309. [Google Scholar] [CrossRef] [PubMed]
- Earl, P.L.; Americo, J.L.; Moss, B. Lethal monkeypox virus infection of Cast/Eij mice is associated with a deficient gamma interferon response. J. Virol. 2012, 86, 9105–9112. [Google Scholar] [CrossRef]
- Estep, R.D.; Messaoudi, I.; O’Connor, M.A.; Li, H.; Sprague, J.; Barron, A.; Engelmann, F.; Yen, B.; Powers, M.F.; Jones, J.M.; et al. Deletion of the monkeypox virus inhibitor of complement enzymes locus impacts the adaptive immune response to monkeypox virus in a nonhuman primate model of infection. J. Virol. 2011, 85, 9527–9542. [Google Scholar] [CrossRef]
- Saylor, K.; Gillam, F.; Lohneis, T.; Zhang, C. Designs of Antigen Structure and Composition for Improved Protein-Based Vaccine Efficacy. Front. Immunol. 2020, 11, 283. [Google Scholar] [CrossRef]
- Tontini, M.; Romano, M.R.; Proietti, D.; Balducci, E.; Micoli, F.; Balocchi, C.; Santini, L.; Masignani, V.; Berti, F.; Costantino, P. Preclinical studies on new proteins as carrier for glycoconjugate vaccines. Vaccine 2016, 34, 4235–4242. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, J.; Li, X.; Dong, J.; Wei, J.; Guo, X.; Wang, G.; Xu, M.; Zhao, A. Enhanced Immune Responses in Mice by Combining the Mpox Virus B6R-Protein and Aluminum Hydroxide-CpG Vaccine Adjuvants. Vaccines 2024, 12, 776. https://doi.org/10.3390/vaccines12070776
Li J, Li X, Dong J, Wei J, Guo X, Wang G, Xu M, Zhao A. Enhanced Immune Responses in Mice by Combining the Mpox Virus B6R-Protein and Aluminum Hydroxide-CpG Vaccine Adjuvants. Vaccines. 2024; 12(7):776. https://doi.org/10.3390/vaccines12070776
Chicago/Turabian StyleLi, Junli, Xiaochi Li, Jiaxin Dong, Jiazheng Wei, Xiaonan Guo, Guozhi Wang, Miao Xu, and Aihua Zhao. 2024. "Enhanced Immune Responses in Mice by Combining the Mpox Virus B6R-Protein and Aluminum Hydroxide-CpG Vaccine Adjuvants" Vaccines 12, no. 7: 776. https://doi.org/10.3390/vaccines12070776




