Use of Measles and Rubella Rapid Diagnostic Tests to Improve Case Detection and Targeting of Vaccinations
Abstract
1. Introduction
2. Measles and Rubella Immunization
3. Laboratory Testing for Measles and Rubella Surveillance to Guide Immunization Programs
4. Measles and Rubella Laboratory Testing
4.1. Current Laboratory Testing Methods
4.2. Role of the Global Measles and Rubella Laboratory Network
4.3. Laboratory Testing Challenges
5. Current Status of Measles and Rubella IgM Rapid Diagnostic Tests
5.1. Measles IgM Rapid Diagnostic Tests
5.2. Rubella IgM Rapid Diagnostic Tests
5.3. Integration of RDTs into Measles and Rubella Surveillance Programs
6. Deployment of Measles and Rubella IgM Rapid Diagnostic Tests: Challenges in Low- and Middle-Income Countries
6.1. Financing Challenges for Measles and Rubella IgM RDT Deployment
6.2. Validation of Commercially Available Measles and Rubella IgM RDTs and Guidance on Deployment
6.3. Future Directions and Way Forward
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Minta, A.A.; Ferrari, M.; Antoni, S.; Portnoy, A.; Sbarra, A.; Lambert, B.; Hauryski, S.; Hatcher, C.; Nedelec, Y.; Datta, D.; et al. Progress Toward Regional Measles Elimination—Worldwide, 2000–2021. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 1489–1495. [Google Scholar] [CrossRef] [PubMed]
- Ou, A.C.; Zimmerman, L.A.; Alexander, J.P., Jr.; Crowcroft, N.S.; O’Connor, P.M.; Knapp, J.K. Progress Toward Rubella and Congenital Rubella Syndrome Elimination—Worldwide, 2012–2022. MMWR Morb. Mortal. Wkly. Rep. 2024, 73, 162–167. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. Immunization Agenda 2030: A Global Strategy to Leave No One Behind. 2020. Available online: https://www.who.int (accessed on 25 February 2024).
- Gastanaduy, P.A.; Redd, S.B.; Clemmons, N.S.; Lee, A.D.; Hickman, C.J.; Rota, P.A.; Patel, M. Measles [Chapter 7]. In Manual for the Surveillance of Vaccine-Preventable Diseases; US Department of Health and Human Services, CDC: Atlanta, GA, USA, 2023. Available online: https://www.cdc.gov/vaccines/pubs/surv-manual/chpt07-measles.html (accessed on 5 June 2024).
- Cutts, F.T.; Ferrari, M.J.; Krause, L.K.; Tatem, A.J.; Mosser, J.F. Vaccination strategies for measles control and elimination: Time to strengthen local initiatives. BMC Med. 2021, 19, 1–8. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. Measles vaccines: WHO position paper, April 2017–Recommendations. Vaccine 2019, 37, 219–222. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. Rubella vaccines: WHO position paper–July 2020–Note de synthèse: Position de l’OMS concernant les vaccins antirubéoleux. Wkly. Epidemiol. Rec. 2020, 95, 306–324. [Google Scholar]
- Gastañaduy, P.A.; Banerjee, E.; DeBolt, C.; Bravo-Alcántara, P.; Samad, S.A.; Pastor, D.; Rota, P.A.; Patel, M.; Crowcroft, N.S.; Durrheim, D.N. Public health responses during measles outbreaks in elimination settings: Strategies and challenges. Hum. Vaccin Immunother. 2018, 14, 2222–2238. [Google Scholar] [CrossRef] [PubMed]
- Moss, W.J. Measles. Lancet 2017, 390, 2490–2502. [Google Scholar] [CrossRef]
- World Health Organisation. Vaccine Preventable Diseases Surveillance Standards: Measles Chapter; WHO: Geneva, Switzerland, 2018; Available online: https://www.who.int/publications/m/item/vaccine-preventable-diseases-surveillance-standards-measles (accessed on 28 February 2024).
- Gavi, the Vaccine Alliance. Improving Yellow Fever Diagnostic Testing for More Efficient, Effective, and Equitable Vaccination. 2021. Available online: https://www.gavi.org/vaccineswork/improving-yellow-fever-diagnostic-testing-more-efficient-effective-and-equitable (accessed on 7 July 2024).
- World Health Organisation. Global Deployment of Rapid Diagnostic Tests to Boost Fight against Cholera. 2024. Available online: https://www.who.int/news/item/05-04-2024-global-deployment-of-rapid-diagnostic-tests-to-boost-fight-against-cholera (accessed on 9 July 2024).
- Global Taskforce on Cholera Control. Public Health Surveillance for Cholera: Interim Guidance February 2023. Available online: https://www.gtfcc.org/wp-content/uploads/2023/02/gtfcc-public-health-surveillance-for-cholera-interim-guidance.pdf (accessed on 9 July 2024).
- Grais, R.F.; Conlan, A.J.; Ferrari, M.J.; Djibo, A.; Le Menach, A.; Bjørnstad, O.N.; Grenfell, B.T. Time is of the essence: Exploring a measles outbreak response vaccination in Niamey, Niger. J. R. Soc. Interface 2008, 5, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Grais, R.F.; Dubray, C.; Fermon, F.; Guerin, P.J. Exploring the time to intervene with a reactive mass vaccination campaign in measles epidemics. Epidemiol. Infect. 2006, 134, 845–849. [Google Scholar] [CrossRef][Green Version]
- Muscat, M.; Ben Mamou, M.; Reynen-de Kat, C.; Jankovic, D.; Hagan, J.; Singh, S.; Datta, S.S. Progress and Challenges in Measles and Rubella Elimination in the WHO European Region. Vaccines 2024, 12, 696. [Google Scholar] [CrossRef]
- Roberts, L. In Vietnam, an anatomy of a measles outbreak. Science 2015, 348, 962. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization & United States Centers for Disease Control and Prevention. Triangulation for Improved Decision-Making in Immunization Programmes 2020. 2022. Available online: https://www.technet-21.org/media/com_resources/trl/6616/multi_upload/0_Triangulation_CoverOrientation_DRAFT_27Jul2020.pdf (accessed on 25 February 2024).
- World Health Organisation. Manual for the Laboratory-Based Surveillance of Measles, Rubella, and Congenital Rubella Syndrome; World Health Organisation: Geneva, Switzerland, 2018; Available online: https://www.who.int/publications/m/item/chapter-1-manual-for-the-laboratory-based-surveillance-of-measles-rubella-and-congenital-rubella-syndrome (accessed on 21 February 2024).
- Bolotin, S.; Lim, G.; Dang, V.; Crowcroft, N.; Gubbay, J.; Mazzulli, T.; Schabas, R. The utility of measles and rubella IgM serology in an elimination setting, Ontario, Canada, 2009–2014. PLoS ONE 2017, 12, e0181172. [Google Scholar] [CrossRef] [PubMed]
- Riddell, M.A.; Chibo, D.; Kelly, H.A.; Catton, M.G.; Birch, C.J. Investigation of optimal specimen type and sampling time for detection of measles virus RNA during a measles epidemic. J. Clin. Microbiol. 2001, 39, 375–376. [Google Scholar] [CrossRef] [PubMed][Green Version]
- van Binnendijk, R.S.; van den Hof, S.; van den Kerkhof, H.; Kohl, R.H.; Woonink, F.; Berbers, G.A.; Conyn-van Spaendonck, M.A.; Kimman, T.G. Evaluation of serological and virological tests in the diagnosis of clinical and subclinical measles virus infections during an outbreak of measles in The Netherlands. J. Infect. Dis. 2003, 188, 898–903. [Google Scholar] [CrossRef] [PubMed]
- Mulders, M.N. Global measles and rubella laboratory network support for elimination goals, 2010–2015. MMWR Morb. Mortal. Wkly. Rep. 2016, 65, 438–442. [Google Scholar] [CrossRef] [PubMed]
- Strebel, P.; Grabowsky, M.; Hoekstra, E.; Gay, A.; Cochi, S. Evolution and Contribution of a Global Partnership against Measles and Rubella, 2001–2023. Vaccines 2024, 12, 693. [Google Scholar] [CrossRef]
- Mulders, M.N.; Serhan, F.; Goodson, J.L.; Icenogle, J.; Johnson, B.W.; Rota, P.A. Expansion of Surveillance for Vaccine-preventable Diseases: Building on the Global Polio Laboratory Network and the Global Measles and Rubella Laboratory Network Platforms. J. Infect. Dis. 2017, 216, S324–S330. [Google Scholar] [CrossRef] [PubMed]
- Brown, K.E.; Rota, P.A.; Goodson, J.L.; Williams, D.; Abernathy, E.; Takeda, M.; Mulders, M.N. Genetic characterization of measles and rubella viruses detected through global measles and rubella elimination surveillance, 2016–2018. MMWR Morb. Mortal. Wkly. Rep. 2019, 68, 587–591. [Google Scholar] [CrossRef]
- Williams, D.; Penedos, A.; Bankamp, B.; Anderson, R.; Hübschen, J.; Mamou, M.B.; Beck, A.; Brown, D.; Rey-Benito, G.; Evans, R.; et al. Update: Circulation of Active Genotypes of Measles Virus and Recommendations for Use of Sequence Analysis to Monitor Viral Transmission; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- Patel, M.K.; Gibson, R.; Cohen, A.; Dumolard, L.; Gacic-Dobo, M. Global landscape of measles and rubella surveillance. Vaccine 2018, 36, 7385–7392. [Google Scholar] [CrossRef] [PubMed]
- Scobie, H.M.; Ilunga, B.K.; Mulumba, A.; Shidi, C.; Coulibaly, T.; Obama, R.; Tamfum, J.J.M.; Simbu, E.P.; Smit, S.B.; Masresha, B.; et al. Antecedent causes of a measles resurgence in the Democratic Republic of the Congo. Pan Afr. Med. J. 2015, 21, 30. [Google Scholar] [CrossRef]
- Orenstein, W.A.; Hinman, A.; Nkowane, B.; Olive, J.M.; Reingold, A. Measles and Rubella Global Strategic Plan 2012-2020 midterm review. Vaccine 2018, 36 (Suppl. 1), A1–A34. [Google Scholar] [CrossRef]
- Nigeria Centers for Disease Control. An Update of Measles Outbreak in Nigeria Measles Situation Report. Abuja, Nigeria. 2023. Available online: https://ncdc.gov.ng/diseases/sitreps/?cat=11&name=An%20Update%20of%20Measles%20Outbreak%20in%20Nigeria (accessed on 2 March 2024).
- Pai, N.P.; Vadnais, C.; Denkinger, C.; Engel, N.; Pai, M. Point-of-care testing for infectious diseases: Diversity, complexity, and barriers in low-and middle-income countries. PLoS Med. 2012, 9, e1001306. [Google Scholar] [CrossRef]
- Osorio, L.; Garcia, J.A.; Parra, L.G.; Garcia, V.; Torres, L.; Degroote, S.; Ridde, V. A scoping review on the field validation and implementation of rapid diagnostic tests for vector-borne and other infectious diseases of poverty in urban areas. Infect. Dis. Poverty 2018, 7, 1–18. [Google Scholar] [CrossRef]
- Warrener, L.; Slibinskas, R.; Chua, K.B.; Nigatu, W.; Brown, K.E.; Sasnauskas, K.; Samuel, D.; Brown, D. A point-of-care test for measles diagnosis: Detection of measles-specific IgM antibodies and viral nucleic acid. Bull. World Health Organ. 2011, 89, 675–682. [Google Scholar] [CrossRef]
- Shonhai, A.; Warrener, L.; Mangwanya, D.; Slibinskas, R.; Brown, K.; Brown, D.; Featherstone, D.; Samuel, D. Investigation of a measles outbreak in Zimbabwe, 2010: Potential of a point of care test to replace laboratory confirmation of suspected cases. Epidemiol. Infect. 2015, 143, 3442–3450. [Google Scholar] [CrossRef] [PubMed]
- Warrener, L.; Andrews, N.; Koroma, H.; Alessandrini, I.; Haque, M.; Garcia, C.C.; Matos, A.R.; Caetano, B.; Lemos, X.R.; Siqueira, M.M.; et al. Evaluation of a rapid diagnostic test for measles IgM detection; accuracy and the reliability of visual reading using sera from the measles surveillance programme in Brazil, 2015. Epidemiol. Infect. 2023, 151, e151. [Google Scholar] [CrossRef]
- Brown, D.W.; Warrener, L.; Scobie, H.M.; Donadel, M.; Waku-Kouomou, D.; Mulders, M.N.; Rota, P.A. Rapid diagnostic tests to address challenges for global measles surveillance. Curr. Opin. Virol. 2020, 41, 77–84. [Google Scholar] [CrossRef]
- Senin, A.A.; Noordin, N.M.; Sani, J.A.M.; Mahat, D.; Donadel, M.; Scobie, H.M.; Omar, A.; Chem, Y.K.; Zahari, M.I.; Ismail, F.; et al. A measles IgM rapid diagnostic test to address challenges with national measles surveillance and response in Malaysia. PLoS ONE 2024, 19, e0298730. [Google Scholar] [CrossRef]
- Institut Pasteur Dakar. Launch of the Rapid Diagnostic Test Production Platform at the Institut Pasteur in Dakar. 2020. Available online: https://www.fondation-merieux.org/en/news/inauguration-of-the-diatropix-production-platform-at-the-institut-pasteur-of-dakar/ (accessed on 5 March 2024).
- Médecins Sans Frontières. RDTs: Measles and Meningitis. Geneva, Switzerland. Available online: https://fondation.msf.fr/en/projects/rdts-measles-and-meningitis#in-detail (accessed on 16 March 2024).
- United States Centers for Disease Control and Prevention. Serology Testing for Rubella and Congenital Rubella Syndrome (CRS). 2023. Available online: https://www.cdc.gov/rubella/lab/serology.html (accessed on 6 March 2024).
- Cullen, A.; Brown, S.; Cafferkey, M.; O’Brien, N.; Griffin, E. Current use of the TORCH screen in the diagnosis of congenital infection. J. Infect. 1998, 36, 185–188. Available online: https://www.sciencedirect.com/science/article/pii/S016344539880011X (accessed on 6 March 2024). [CrossRef] [PubMed]
- Jin, L.; Vyse, A.; Brown, D.W. The role of RT-PCR assay of oral fluid for diagnosis and surveillance of measles, mumps and rubella. Bull. World Health Organ. 2002, 80, 76–77. [Google Scholar]
- The Academy of Medical Sciences. Improving the Development and Deployment of Rapid Diagnostic Tests in Lmics, Workshop Report, 21 November 2016. London, United Kingdom. 2016. Available online: https://acmedsci.ac.uk/file-download/18597310 (accessed on 8 June 2024).
- PATH. Market Failures and Opportunities for Increasing Access to Diagnostics in Low- and Middle-Income Countries. PATH: Seattle. 2022. Available online: https://www.path.org/resources/market-failures-andopportunities-for-increasing-access-to-diagnosticsin-low-and-middle-income-countries/ (accessed on 10 June 2024).
- Yimer, S.A.; Booij, B.B.; Tobert, G.; Hebbeler, A.; Oloo, P.; Brangel, P.; Jackson, M.L.A.; Jarman, R.; Craig, D.; Avumegah, M.S.; et al. Rapid diagnostic test: A critical need for outbreak preparedness and response for high priority pathogens. BMJ Glob. Health 2024, 9, e014386. [Google Scholar] [CrossRef]
- Gavi, the Vaccine Alliance. Measles Rapid Diagnostics Capacity Roadmap: Public Summary. Geneva, Switzerland. 2023. Available online: https://www.gavi.org/sites/default/files/about/market-shaping/roadmaps/Public-Summary_Measles-Diagnostics-Roadmap-2023.pdf (accessed on 10 March 2024).
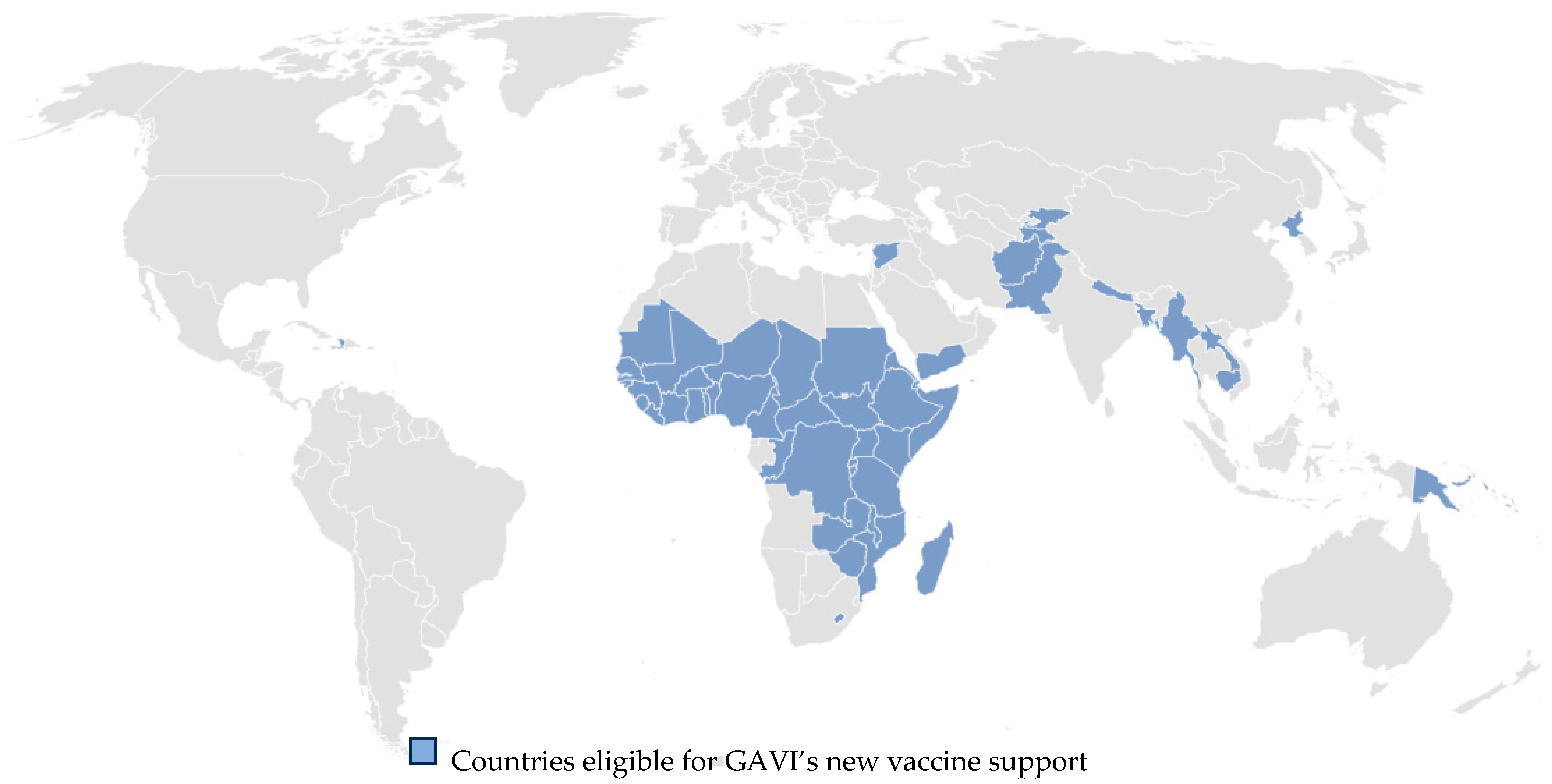
- Gavi, the Vaccine Alliance. Eligibility. Geneva, Switzerland. 2024. Available online: https://www.gavi.org/types-support/sustainability/eligibility (accessed on 10 March 2024).
- World Health Organisation. Global Measles and Rubella Monthly Update 2024. Geneva, Switzerland. 2024. Available online: https://cdn.who.int/media/docs/default-source/immunization/immunization-coverage/global_mr_update.pptx?sfvrsn=c83eebae_147 (accessed on 10 March 2024).
- Foundation for Innovative New Diagnostics (FIND). Target Product Profile for Surveillance Tests for Measles and Rubella. Geneva, Switzerland. 2024. Available online: https://www.finddx.org/wp-content/uploads/2024/06/20240613_tpp_measles_rubell_FV_EN.pdf (accessed on 17 June 2024).
- Abimbola, T.O.; Marston, B.J.; Date, A.A.; Blandford, J.M.; Sangrujee, N.; Wiktor, S.Z. Cost-effectiveness of tuberculosis diagnostic strategies to reduce early mortality among persons with advanced HIV infection initiating antiretroviral therapy. JAIDS J. Acquir. Immune Defic. Syndr. 2012, 60, e1–e7. [Google Scholar] [CrossRef] [PubMed]
- de Oliveira, M.R.F.; Giozza, S.P.; Peixoto, H.M.; Romero, G.A. Cost-effectiveness of diagnostic for malaria in Extra-Amazon Region, Brazil. Malar. J. 2012, 11, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Doyle, N.M.; Levison, J.E.; Gardner, M.O. Rapid HIV versus enzyme-linked immunosorbent assay screening in a low-risk Mexican American population presenting in labor: A cost-effectiveness analysis. Am. J. Obstet. Gynecol. 2005, 193, 1280–1285. [Google Scholar] [CrossRef] [PubMed]
- Sohn, H.; Kasaie, P.; Kendall, E.; Gomez, G.B.; Vassall, A.; Pai, M.; Dowdy, D. Informing decision-making for universal access to quality tuberculosis diagnosis in India: An economic-epidemiological model. BMC Med. 2019, 17, 155. [Google Scholar] [CrossRef] [PubMed]
- Odaga, J.; Sinclair, D.; Lokong Adaktar, J.; Donegan, S.; Hopkins, H.; Garner, P. Rapid diagnostic tests versus clinical diagnosis for managing people with fever in malaria endemic settings. Cochrane Database Syst. Rev. 2014, 4, CD008998. [Google Scholar] [CrossRef] [PubMed]
- Thompson, K.M.; Odahowski, C.L. Systematic Review of Health Economic Analyses of Measles and Rubella Immunization Interventions. Risk Anal. 2016, 36, 1297–1314. [Google Scholar] [CrossRef] [PubMed]
- Pai, N.P.; Wilkinson, S.; Deli-Houssein, R.; Vijh, R.; Vadnais, C.; Behlim, T.; Steben, M.; Engel, N.; Wong, T. Barriers to Implementation of Rapid and Point-of-Care Tests for Human Immunodeficiency Virus Infection: Findings From a Systematic Review (1996–2014). Point Care 2015, 14, 81–87. [Google Scholar] [CrossRef]
- Asiimwe, C.; Kyabayinze, D.J.; Kyalisiima, Z.; Nabakooza, J.; Bajabaite, M.; Counihan, H.; Tibenderana, J.K. Early experiences on the feasibility, acceptability, and use of malaria rapid diagnostic tests at peripheral health centres in Uganda-insights into some barriers and facilitators. Implement Sci. 2012, 7, 1–12. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rachlin, A.; Hampton, L.M.; Rota, P.A.; Mulders, M.N.; Papania, M.; Goodson, J.L.; Krause, L.K.; Hanson, M.; Osborn, J.; Kelly-Cirino, C.; et al. Use of Measles and Rubella Rapid Diagnostic Tests to Improve Case Detection and Targeting of Vaccinations. Vaccines 2024, 12, 823. https://doi.org/10.3390/vaccines12080823
Rachlin A, Hampton LM, Rota PA, Mulders MN, Papania M, Goodson JL, Krause LK, Hanson M, Osborn J, Kelly-Cirino C, et al. Use of Measles and Rubella Rapid Diagnostic Tests to Improve Case Detection and Targeting of Vaccinations. Vaccines. 2024; 12(8):823. https://doi.org/10.3390/vaccines12080823
Chicago/Turabian StyleRachlin, Audrey, Lee M. Hampton, Paul A. Rota, Mick N. Mulders, Mark Papania, James L. Goodson, L. Kendall Krause, Matt Hanson, Jennifer Osborn, Cassandra Kelly-Cirino, and et al. 2024. "Use of Measles and Rubella Rapid Diagnostic Tests to Improve Case Detection and Targeting of Vaccinations" Vaccines 12, no. 8: 823. https://doi.org/10.3390/vaccines12080823
APA StyleRachlin, A., Hampton, L. M., Rota, P. A., Mulders, M. N., Papania, M., Goodson, J. L., Krause, L. K., Hanson, M., Osborn, J., Kelly-Cirino, C., Evans, B., Sinha, A., Warrener, L., Featherstone, D., & Brown, D. (2024). Use of Measles and Rubella Rapid Diagnostic Tests to Improve Case Detection and Targeting of Vaccinations. Vaccines, 12(8), 823. https://doi.org/10.3390/vaccines12080823






