Exploring the Inherent Heterogeneity of Vaccine Hesitancy: A Study of a Childhood-Vaccine-Hesitant Population
Abstract
1. Introduction
2. Predictors of Vaccine Hesitancy
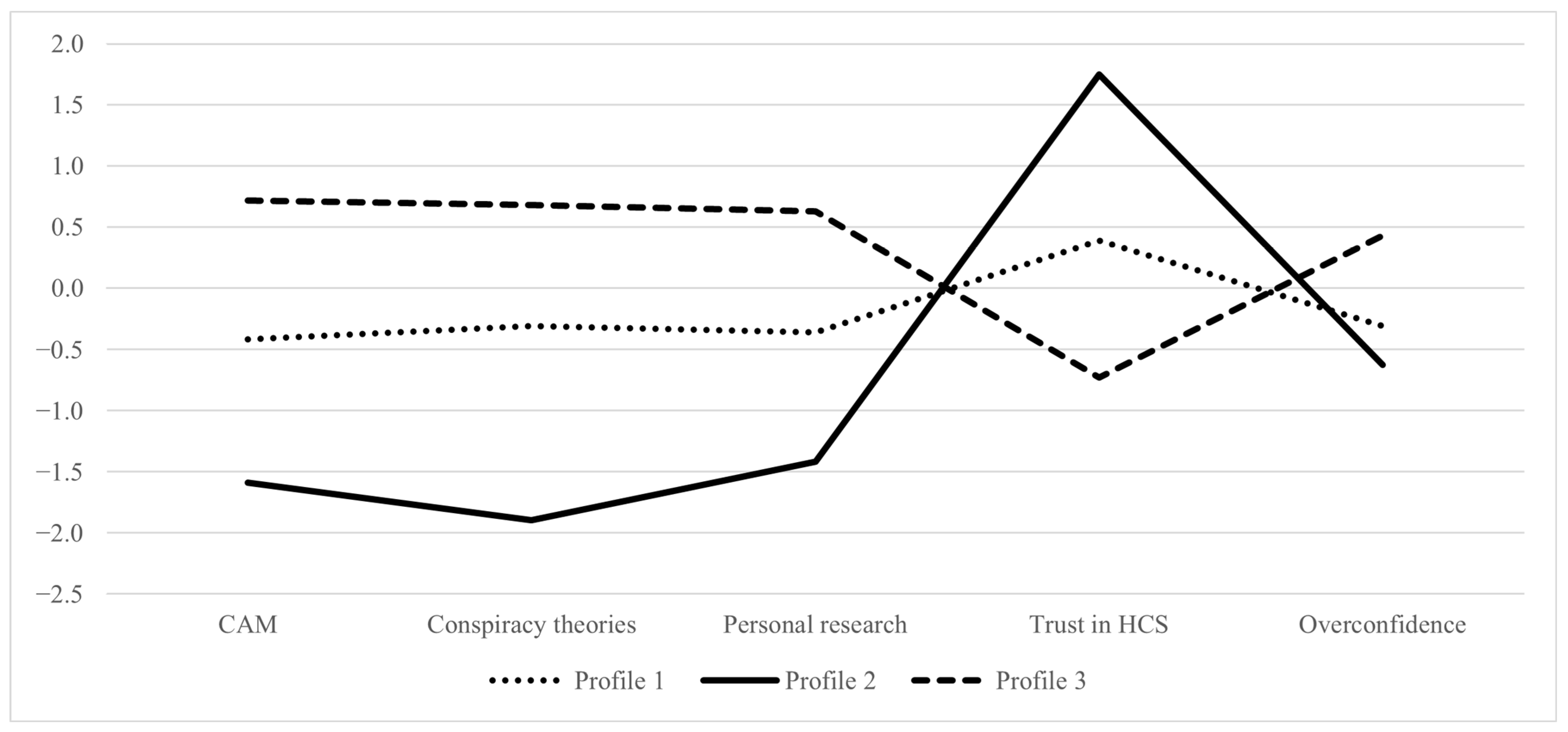
Research Question 1: Do distinct profiles of vaccine hesitant individuals exist that vary qualitatively and quantitatively in their endorsement of complementary and alternative medicine, conspiracy theories, trust in the healthcare system, engagement in “self” researching information, and overconfidence in their knowledge?
2.1. Sociodemographic Characteristics of Vaccine Hesitant Individuals
Research Question 2: Do sociodemographic determinants (gender, age, education, income, and political orientation) predict the profile membership of vaccine-hesitant individuals?
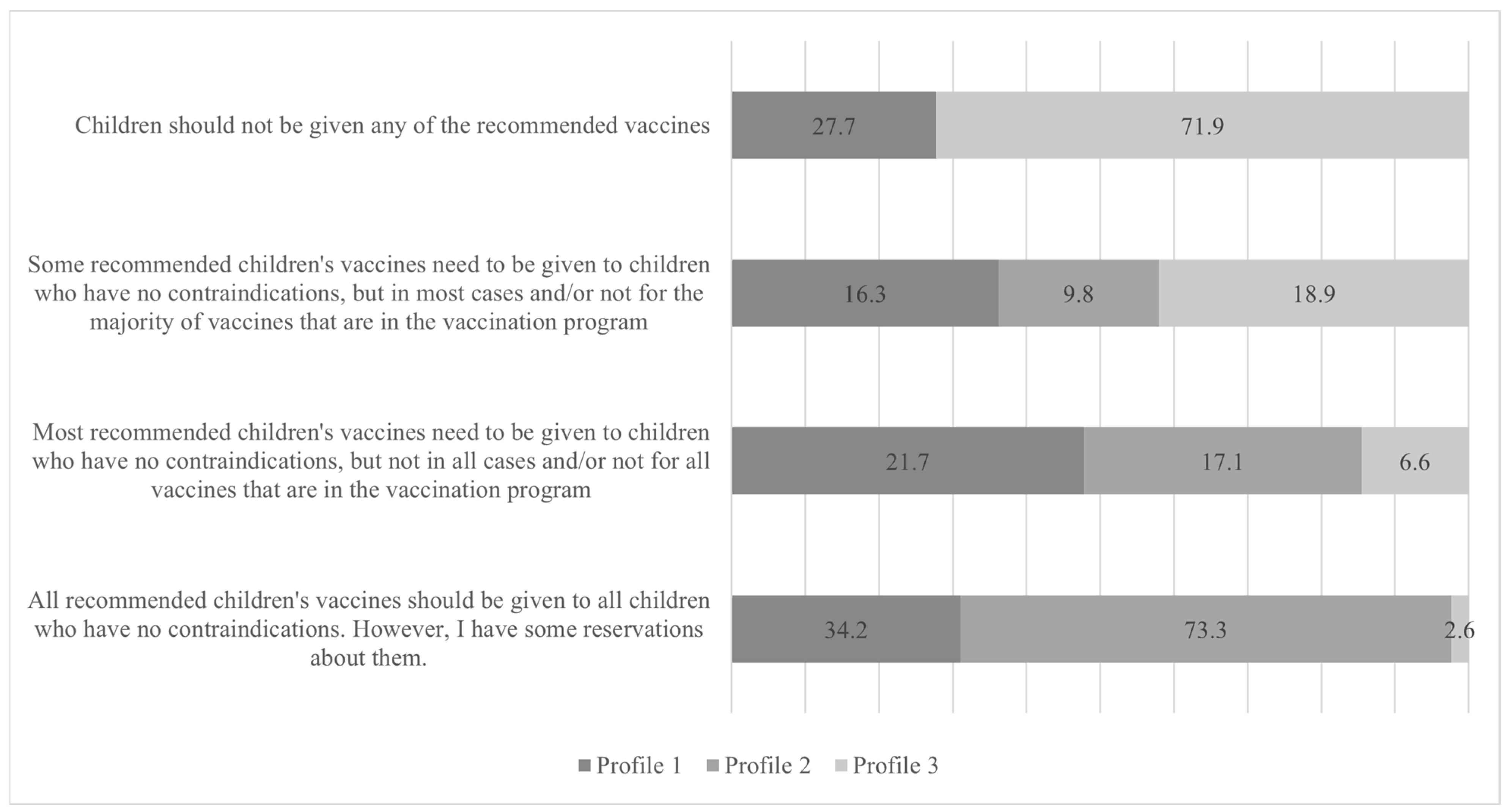
2.2. Do Vaccine Hesitant Individuals Differ on Their Stance on Vaccination and Specific Vaccines?
Research Question 3: Do identified profiles differ in vaccine-related concerns (vaccine safety, efficacy, and importance)?
Research Question 4: Do identified profiles differ in attitudes towards specific vaccines (against MMR, HPV, and Seasonal Influenza)?
2.3. The Role of Information Sources in Understanding Vaccine Hesitancy
Research Question 5: Do identified profiles differ in the importance they give to different information sources about vaccines?
3. Methods
3.1. Data Collection
3.2. Participants
3.3. Measures
Latent Indicators
3.4. Outcomes
3.5. Sociodemographic Predictors
3.6. Statistical Analyses
4. Results
5. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- MacDonald, N.E. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef] [PubMed]
- Allington, D.; McAndrew, S.; Moxham-Hall, V.; Duffy, B. Coronavirus conspiracy suspicions, general vaccine attitudes, trust and coronavirus information source as predictors of vaccine hesitancy among UK residents during the COVID-19 pandemic. Psychol. Med. 2021, 53, 236–247. [Google Scholar] [CrossRef]
- Hwang, S.E.; Kim, W.-H.; Heo, J. Socio-demographic, psychological, and experiential predictors of COVID-19 vaccine hesitancy in South Korea, October–December 2020. Hum. Vaccin. Immunother. 2022, 18, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Howard, M.C. Integrating the person-centered approach with the study of vaccine hesitancy: Applying latent profile analysis to identify vaccine hesitancy subpopulations and assess their relations with correlates and vaccination outcomes. Vaccine 2023, 41, 4823–4835. [Google Scholar] [CrossRef]
- Zhou, Y.; Li, R.; Shen, L. Psychological profiles of COVID vaccine-hesitant individuals and implications for vaccine message design strategies. Vaccine X 2023, 13, 100279. [Google Scholar] [CrossRef]
- Lamot, M.; Kerman, K.; Kirbiš, A. Distrustful, Dissatisfied, and Conspiratorial: A Latent Profile Analysis of COVID-19 Vaccination Rejection. Int. J. Environ. Res. Public Health 2022, 19, 10096. [Google Scholar] [CrossRef] [PubMed]
- Larson, H.J.; Jarrett, C.; Eckersberger, E.; Smith, D.M.D.; Paterson, P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: A systematic review of published literature, 2007–2012. Vaccine 2014, 32, 2150–2159. [Google Scholar] [CrossRef]
- Toshkov, D. What accounts for the variation in COVID-19 vaccine hesitancy in Eastern, Southern and Western Europe? Vaccine 2023, 41, 3178–3188. [Google Scholar] [CrossRef]
- Browne, M.; Thomson, P.; Rockloff, M.J.; Pennycook, G. Going against the Herd: Psychological and Cultural Factors Underlying the ‘Vaccination Confidence Gap’. PLoS ONE 2015, 10, e0132562. [Google Scholar] [CrossRef]
- Hornsey, M.J.; Lobera, J.; Díaz-Catalán, C. Vaccine hesitancy is strongly associated with distrust of conventional medicine, and only weakly associated with trust in alternative medicine. Soc. Sci. Med. 2020, 255, 113019. [Google Scholar] [CrossRef]
- Ahorsu, D.K.; Lin, C.-Y.; Yahaghai, R.; Alimoradi, Z.; Broström, A.; Griffiths, M.D.; Pakpour, A.H. The mediational role of trust in the healthcare system in the association between generalized trust and willingness to get COVID-19 vaccination in Iran. Hum. Vaccin. Immunother. 2022, 18, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Özer, Ö.; Budak, F.; Alp, S. Is Vaccine Hesitancy Affected by Distrust in the Healthcare System? A Study in Turkish Population. Soc. Work. Public. Health 2023, 38, 323–333. [Google Scholar] [CrossRef] [PubMed]
- Jennings, W.; Stoker, G.; Bunting, H.; Valgarðsson, V.O.; Gaskell, J.; Devine, D.; McKay, L.; Mills, M.C. Lack of Trust, Conspiracy Beliefs, and Social Media Use Predict COVID-19 Vaccine Hesitancy. Vaccines 2021, 9, 593. [Google Scholar] [CrossRef] [PubMed]
- Nazlı, Ş.B.; Yığman, F.; Sevindik, M.; Deniz Özturan, D. Psychological factors affecting COVID-19 vaccine hesitancy. Ir. J. Med. Sci. 2022, 191, 71–80. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, B.L.; Felter, E.M.; Chu, K.-H.; Shensa, A.; Hermann, C.; Wolynn, T.; Williams, D.; Primack, B.A. It’s not all about autism: The emerging landscape of anti-vaccination sentiment on Facebook. Vaccine 2019, 37, 2216–2223. [Google Scholar] [CrossRef] [PubMed]
- Kata, A. Anti-vaccine activists, Web 2.0, and the postmodern paradigm--an overview of tactics and tropes used online by the anti-vaccination movement. Vaccine 2012, 30, 3778–3789. [Google Scholar] [CrossRef] [PubMed]
- Vrdelja, M.; Kraigher, A.; Verčič, D.; Kropivnik, S. The growing vaccine hesitancy: Exploring the influence of the internet. Eur. J. Public Health 2018, 28, 934–939. [Google Scholar] [CrossRef]
- Motta, M.; Callaghan, T.; Sylvester, S. Knowing less but presuming more: Dunning-Kruger effects and the endorsement of anti-vaccine policy attitudes. Soc. Sci. Med. 2018, 211, 274–281. [Google Scholar] [CrossRef] [PubMed]
- Morales, D.X.; Beltran, T.F.; Morales, S.A. Gender, socioeconomic status, and COVID-19 vaccine hesitancy in the US: An intersectionality approach. Sociol. Health Illn. 2022, 44, 953–971. [Google Scholar] [CrossRef]
- Fadhel, F.H. Vaccine hesitancy and acceptance: An examination of predictive factors in COVID-19 vaccination in Saudi Arabia. Health Promot. Int. 2021, 38, daab209. [Google Scholar] [CrossRef]
- Troiano, G.; Nardi, A. Vaccine hesitancy in the era of COVID-19. Public Health 2021, 194, 245–251. [Google Scholar] [CrossRef]
- Schwarzinger, M.; Watson, V.; Arwidson, P.; Alla, F.; Luchini, S. COVID-19 vaccine hesitancy in a representative working-age population in France: A survey experiment based on vaccine characteristics. Lancet Public Health 2021, 6, e210–e221. [Google Scholar] [CrossRef] [PubMed]
- Willis, D.E.; Andersen, J.A.; Bryant-Moore, K.; Selig, J.P.; Long, C.R.; Felix, H.C.; Curran, G.M.; McElfish, P.A. COVID-19 vaccine hesitancy: Race/ethnicity, trust, and fear. Clin. Transl. Sci. 2021, 14, 2200–2207. [Google Scholar] [CrossRef] [PubMed]
- Bocquier, A.; Ward, J.; Raude, J.; Peretti-Watel, P.; Verger, P. Socioeconomic differences in childhood vaccination in developed countries: A systematic review of quantitative studies. Expert. Rev. Vaccines 2017, 16, 1107–1118. [Google Scholar] [CrossRef] [PubMed]
- Galarce, E.M.; Minsky, S.; Viswanath, K. Socioeconomic status, demographics, beliefs and A(H1N1) vaccine uptake in the United States. Vaccine 2011, 29, 5284–5289. [Google Scholar] [CrossRef] [PubMed]
- Robertson, E.; Reeve, K.S.; Niedzwiedz, C.L.; Moore, J.; Blake, M.; Green, M.; Katikireddi, S.V.; Benzeval, M.J. Predictors of COVID-19 vaccine hesitancy in the UK household longitudinal study. Brain Behav. Immun. 2021, 94, 41–50. [Google Scholar] [CrossRef]
- Fridman, A.; Gershon, R.; Gneezy, A. COVID-19 and vaccine hesitancy: A longitudinal study. PLoS ONE 2021, 16, e0250123. [Google Scholar] [CrossRef] [PubMed]
- Howard, M.C. Investigating the Relation of Political Orientation and Vaccination Outcomes: Identifying the Roles of Political Ideology, Party Affiliation, and Vaccine Hesitancy. Psychol. Rep. 2022, 127, 1796–1817. [Google Scholar] [CrossRef]
- Stroope, S.; Kroeger, R.A.; Williams, C.E.; Baker, J.O. Sociodemographic correlates of vaccine hesitancy in the United States and the mediating role of beliefs about governmental conspiracies. Soc. Sci. Q. 2021, 102, 2472–2481. [Google Scholar] [CrossRef]
- Pires, C. Global Predictors of COVID-19 Vaccine Hesitancy: A Systematic Review. Vaccines 2022, 10, 1349. [Google Scholar] [CrossRef]
- Hornsey, M.J.; Edwards, M.; Lobera, J.; Díaz-Catalán, C.; Barlow, F.K. Resolving the small-pockets problem helps clarify the role of education and political ideology in shaping vaccine scepticism. Br. J. Psychol. 2021, 112, 992–1011. [Google Scholar] [CrossRef] [PubMed]
- Gravelle, T.B.; Phillips, J.B.; Reifler, J.; Scotto, T.J. Estimating the size of “anti-vax” and vaccine hesitant populations in the US, UK, and Canada: Comparative latent class modeling of vaccine attitudes. Hum. Vaccin. Immunother. 2022, 18, 2008214. [Google Scholar] [CrossRef]
- Kricorian, K.; Civen, R.; Equils, O. COVID-19 vaccine hesitancy: Misinformation and perceptions of vaccine safety. Hum. Vaccin. Immunother. 2022, 18, 1950504. [Google Scholar] [CrossRef] [PubMed]
- Edwards, K.M.; Hackell, J.M. Countering Vaccine Hesitancy. Pediatrics 2016, 138, e20162146. [Google Scholar] [CrossRef] [PubMed]
- Chamberlain, A.T.; Seib, K.; Ault, K.A.; Orenstein, W.A.; Frew, P.M.; Malik, F.; Cortés, M.; Cota, P.; Whitney, E.A.S.; Flowers, L.C.; et al. Factors Associated with Intention to Receive Influenza and Tetanus, Diphtheria, and Acellular Pertussis (Tdap) Vaccines during Pregnancy: A Focus on Vaccine Hesitancy and Perceptions of Disease Severity and Vaccine Safety. PLoS Curr. 2015, 7. [Google Scholar] [CrossRef] [PubMed]
- Suryadevara, M.; Handel, A.; Bonville, C.A.; Cibula, D.A.; Domachowske, J.B. Pediatric provider vaccine hesitancy: An under-recognized obstacle to immunizing children. Vaccine 2015, 33, 6629–6634. [Google Scholar] [CrossRef] [PubMed]
- Roberts, J.R.; Thompson, D.; Rogacki, B.; Hale, J.J.; Jacobson, R.M.; Opel, D.J.; Darden, P.M. Vaccine hesitancy among parents of adolescents and its association with vaccine uptake. Vaccine 2015, 33, 1748–1755. [Google Scholar] [CrossRef] [PubMed]
- Soares, P.; Rocha, J.V.; Moniz, M.; Gama, A.; Laires, P.A.; Pedro, A.R.; Dias, S.; Leite, A.; Nunes, C. Factors Associated with COVID-19 Vaccine Hesitancy. Vaccines 2021, 9, 300. [Google Scholar] [CrossRef] [PubMed]
- Lucia, V.C.; Kelekar, A.; Afonso, N.M. COVID-19 vaccine hesitancy among medical students. J. Public Health 2021, 43, 445–449. [Google Scholar] [CrossRef] [PubMed]
- Murphy, J.; Vallières, F.; Bentall, R.P.; Shevlin, M.; McBride, O.; Hartman, T.K.; McKay, R.; Bennett, K.; Mason, L.; Gibson-Miller, J.; et al. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat. Commun. 2021, 12, 29. [Google Scholar] [CrossRef]
- Khubchandani, J.; Sharma, S.; Price, J.H.; Wiblishauser, M.J.; Sharma, M.; Webb, F.J. COVID-19 Vaccination Hesitancy in the United States: A Rapid National Assessment. J. Commun. Health 2021, 46, 270–277. [Google Scholar] [CrossRef] [PubMed]
- Aw, J.; Seng, J.J.B.; Seah, S.S.Y.; Low, L.L. COVID-19 Vaccine Hesitancy-A Scoping Review of Literature in High-Income Countries. Vaccines 2021, 9, 900. [Google Scholar] [CrossRef] [PubMed]
- Dubé, E.; Laberge, C.; Guay, M.; Bramadat, P.; Roy, R.; Bettinger, J. Vaccine hesitancy: An overview. Hum. Vaccin. Immunother. 2013, 9, 1763–1773. [Google Scholar] [CrossRef] [PubMed]
- Karafillakis, E.; Simas, C.; Jarrett, C.; Verger, P.; Peretti-Watel, P.; Dib, F.; de Angelis, S.; Takacs, J.; Ali, K.A.; Pastore Celentano, L.; et al. HPV vaccination in a context of public mistrust and uncertainty: A systematic literature review of determinants of HPV vaccine hesitancy in Europe. Hum. Vaccin. Immunother. 2019, 15, 1615–1627. [Google Scholar] [CrossRef] [PubMed]
- Weiss, C.; Schröpfer, D.; Merten, S. Parental attitudes towards measles vaccination in the canton of Aargau, Switzerland: A latent class analysis. BMC Infect. Dis. 2016, 16, 400. [Google Scholar] [CrossRef][Green Version]
- Charron, J.; Gautier, A.; Jestin, C. Influence of information sources on vaccine hesitancy and practices. Med. Mal. Infect. 2020, 50, 727–733. [Google Scholar] [CrossRef] [PubMed]
- Puri, N.; Coomes, E.A.; Haghbayan, H.; Gunaratne, K. Social media and vaccine hesitancy: New updates for the era of COVID-19 and globalized infectious diseases. Hum. Vaccin. Immunother. 2020, 16, 2586–2593. [Google Scholar] [CrossRef] [PubMed]
- Reno, C.; Maietti, E.; Di Valerio, Z.; Montalti, M.; Fantini, M.P.; Gori, D. Vaccine Hesitancy towards COVID-19 Vaccination: Investigating the Role of Information Sources through a Mediation Analysis. Infect. Dis. Rep. 2021, 13, 712–723. [Google Scholar] [CrossRef] [PubMed]
- Thornton, L.; Batterham, P.J.; Fassnacht, D.B.; Kay-Lambkin, F.; Calear, A.L.; Hunt, S. Recruiting for health, medical or psychosocial research using Facebook: Systematic review. Internet Interv. 2016, 4, 72–81. [Google Scholar] [CrossRef] [PubMed]
- King, D.B.; O’Rourke, N.; DeLongis, A. Social media recruitment and online data collection: A beginner’s guide and best practices for accessing low-prevalence and hard-to-reach populations. Can. Psychol. 2014, 55, 240–249. [Google Scholar] [CrossRef]
- Hyland, M.E.; Lewith, G.T.; Westoby, C. Developing a measure of attitudes: The holistic complementary and alternative medicine questionnaire. Complement. Ther. Med. 2003, 11, 33–38. [Google Scholar] [CrossRef]
- Brotherton, R.; French, C.C.; Pickering, A.D. Measuring belief in conspiracy theories: The generic conspiracist beliefs scale. Front. Psychol. 2013, 4, 279. [Google Scholar] [CrossRef] [PubMed]
- Bianco, A.; Mascaro, V.; Zucco, R.; Pavia, M. Parent perspectives on childhood vaccination: How to deal with vaccine hesitancy and refusal? Vaccine 2019, 37, 984–990. [Google Scholar] [CrossRef] [PubMed]
- Rozbroj, T.; Lyons, A.; Lucke, J. Psychosocial and demographic characteristics relating to vaccine attitudes in Australia. Patient Educ. Couns. 2019, 102, 172–179. [Google Scholar] [CrossRef]
- Casiday, R.; Cresswell, T.; Wilson, D.; Panter-Brick, C. A survey of UK parental attitudes to the MMR vaccine and trust in medical authority. Vaccine 2006, 24, 177–184. [Google Scholar] [CrossRef]
- Navalpakam, A.; Dany, M.; Hajj Hussein, I. Behavioral Perceptions of Oakland University Female College Students towards Human Papillomavirus Vaccination. PLoS ONE 2016, 11, e0155955. [Google Scholar] [CrossRef]
- Ferguson, S.L.; Moore, E.W.G.; Hull, D.M. Finding latent groups in observed data: A primer on latent profile analysis in Mplus for applied researchers. Int. J. Behav. Dev. 2020, 44, 458–468. [Google Scholar] [CrossRef]
- Spurk, D.; Hirschi, A.; Wang, M.; Valero, D.; Kauffeld, S. Latent profile analysis: A review and “how to” guide of its application within vocational behavior research. J. Vocat. Behav. 2020, 120, 103445. [Google Scholar] [CrossRef]
- Tein, J.-Y.; Coxe, S.; Cham, H. Statistical Power to Detect the Correct Number of Classes in Latent Profile Analysis. Struct. Equ. Model. 2013, 20, 640–657. [Google Scholar] [CrossRef]
- Park, Y.W.; Bragard, E.; Madhivanan, P.; Fisher, C.B. A Latent Profile Analysis of COVID-19 and Influenza Vaccine Hesitancy among Economically Marginalized Hispanic Mothers of Children under Five Years of Age in the US. J. Racial Ethn. Health Disparities 2024. epub ahead of print. [Google Scholar] [CrossRef]
- Leung, C.L.K.; Li, K.-K.; Wei, V.W.; Tang, A.; Wong, S.Y.S.; Lee, S.S.; Kwok, K.O. Profiling vaccine believers and skeptics in nurses: A latent profile analysis. Int. J. Nurs. Stud. 2022, 126, 104142. [Google Scholar] [CrossRef]
- Portoghese, I.; Siddi, M.; Chessa, L.; Costanzo, G.; Garcia-Larsen, V.; Perra, A.; Littera, R.; Sambugaro, G.; Del Giacco, S.; Campagna, M.; et al. COVID-19 Vaccine Hesitancy among Italian Healthcare Workers: Latent Profiles and Their Relationships to Predictors and Outcome. Vaccines 2023, 11, 273. [Google Scholar] [CrossRef] [PubMed]
- Colville, S.; Lockey, S.; Gillespie, N.; Jane Kelly, S. Compliance with COVID-19 preventative health measures in the United Kingdom: A latent profile analysis. Health Promot. Int. 2024, 39, daae007. [Google Scholar] [CrossRef] [PubMed]

| Profiles | LL | AIC | BIC | SA-BIC | Entropy | LMR-p | BLRT-p | % Smallest Class |
|---|---|---|---|---|---|---|---|---|
| 1 | −2700.522 | 5421.044 | 5461.47 | 5429.737 | / | / | / | / |
| 2 | −2406.051 | 4844.102 | 4908.784 | 4858.011 | 0.85 | <0.001 | <0.001 | 32.5 |
| 3 | −2324.466 | 4692.932 | 4781.87 | 4712.057 | 0.82 | <0.001 | <0.001 | 10.1 |
| 4 | −2290.096 | 4636.191 | 4749.385 | 4660.532 | 0.76 | <0.001 | <0.001 | 7.8 |
| 5 | −2278.810 | 4625.62 | 4763.069 | 4655.176 | 0.77 | 0.394 | 0.013 | 6.6 |
| 6 | −2268.700 | 4617.4 | 4779.105 | 4652.173 | 0.8 | 0.171 | 0.05 | 0.7 |
| Profile 1 | Profile 2 | Profile 3 | ||||||
|---|---|---|---|---|---|---|---|---|
| (n = 184) | (n = 41) | (n = 196) | ||||||
| M | SD | M | SD | M | SD | F (df) | η2 | |
| CAM a | 3.22 B,C | 0.55 | 2.22 C | 0.56 | 4.19 | 0.56 | 275.650 *** | 0.62 |
| (2, 416) | ||||||||
| Conspiracy theories b | 3.4 B,C | 0.58 | 2.05 C | 0.56 | 4.33 | 0.53 | 318.506 *** | 0.65 |
| (2, 145) | ||||||||
| Personal research b | 2.64 B,C | 0.7 | 1.71 C | 0.78 | 3.52 | 0.59 | 150.447 *** | 0.5 |
| (2, 107.169) | ||||||||
| Trust in HCS b | 2.35 B,C | 0.57 | 3.46 C | 0.54 | 1.43 | 0.44 | 338.914 *** | 0.66 |
| (2, 109.023) | ||||||||
| Overconfidence b | 1.95 C | 0.81 | 1.64 C | 0.88 | 2.66 | 0.92 | 41.247 *** | 0.23 |
| (2, 109.02) | ||||||||
| B | SE | Wald | p | ||
|---|---|---|---|---|---|
| Profile 1 | Age | −0.03 | 0.01 | 4.357 | 0.04 |
| Gender (male) | 1.27 | 0.36 | 12.624 | <0.001 | |
| Education | 0.12 | 0.06 | 4.306 | 0.04 | |
| Income | 0 | 0 | 4.945 | 0.03 | |
| Political orientation | −0.01 | 0.06 | 0.01 | 0.92 | |
| Profile 2 | Age | −0.00 | 0.02 | 0.025 | 0.87 |
| Gender (male) | 1.81 | 0.51 | 12.752 | <0.001 | |
| Education | 0.2 | 0.1 | 3.86 | 0.05 | |
| Income | 0 | 0 | 2.015 | 0.16 | |
| Political orientation | −0.35 | 0.1 | 13.382 | <0.001 |
| Profile 1 | Profile 2 | Profile 3 | ||||
|---|---|---|---|---|---|---|
| (A) | (B) | (C) | ||||
| M (SD) | M (SD) | M (SD) | F (df) | η2 | ||
| Attitudes towards vaccination | Efficacy | 3.00 (1.25) B,C | 4.29 (0.90) C | 1.63 (1.00) | 168.455 *** | 0.39 |
| (2, 120.527) | ||||||
| Safety | 2.56 (1.28) B,C | 3.93 (0.78) C | 1.24 (0.63) | 257.162 *** | 0.44 | |
| (2, 108.588) | ||||||
| Importance | 2.79 (1.32) B,C | 4.29 (0.95) C | 1.42 (0.80) | 201.427 *** | 0.43 | |
| (2, 110.484) | ||||||
| Attitudes toward specific vaccines | MMR | 2.82 (1.39) B,C | 4.29 (0.89) C | 1.38 (0.86) | 189.177 *** | 0.42 |
| (2, 97.113) | ||||||
| HPV | 2.56 (1.29) B,C | 3.58 (1.15) C | 1.33 (0.81) | 91.483 *** | 0.26 | |
| (2, 78.064) | ||||||
| Seasonal Influenza | 2.31 (1.17) B,C | 3.50 (1.11) C | 1.13 (0.51) | 148.688 *** | 0.43 | |
| (2, 93.928) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lamot, M.; Kirbiš, A.; Vrdelja, M. Exploring the Inherent Heterogeneity of Vaccine Hesitancy: A Study of a Childhood-Vaccine-Hesitant Population. Vaccines 2024, 12, 839. https://doi.org/10.3390/vaccines12080839
Lamot M, Kirbiš A, Vrdelja M. Exploring the Inherent Heterogeneity of Vaccine Hesitancy: A Study of a Childhood-Vaccine-Hesitant Population. Vaccines. 2024; 12(8):839. https://doi.org/10.3390/vaccines12080839
Chicago/Turabian StyleLamot, Monika, Andrej Kirbiš, and Mitja Vrdelja. 2024. "Exploring the Inherent Heterogeneity of Vaccine Hesitancy: A Study of a Childhood-Vaccine-Hesitant Population" Vaccines 12, no. 8: 839. https://doi.org/10.3390/vaccines12080839
APA StyleLamot, M., Kirbiš, A., & Vrdelja, M. (2024). Exploring the Inherent Heterogeneity of Vaccine Hesitancy: A Study of a Childhood-Vaccine-Hesitant Population. Vaccines, 12(8), 839. https://doi.org/10.3390/vaccines12080839






