Immunogenicity and Protective Efficacy of Aerosolized Live-Attenuated Yellow Fever 17D Vaccine in Mice
Abstract
:1. Introduction
2. Material and Methods
2.1. Cells and Viruses
2.2. Aerosolization of YF-17D
2.3. In Vitro Phenotypic Characteristics of Aerosolized YF-17D
2.4. Animal Experiments
2.5. ELISA
2.6. ELISPOT
2.7. PRNT
2.8. RT-qPCR
2.9. Statistical Analysis
3. Results
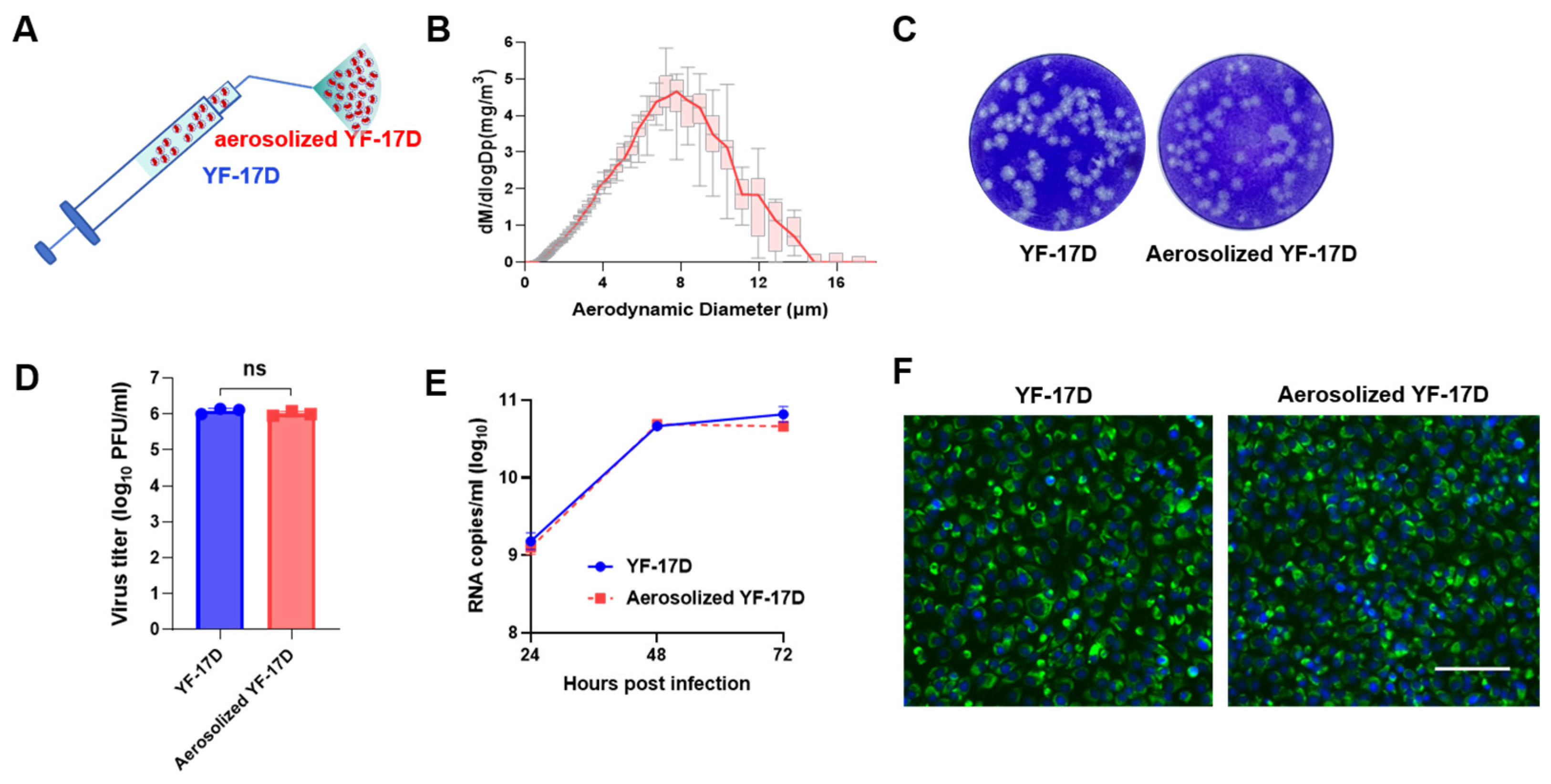
3.1. Characterization of Aerosolized YF-17D
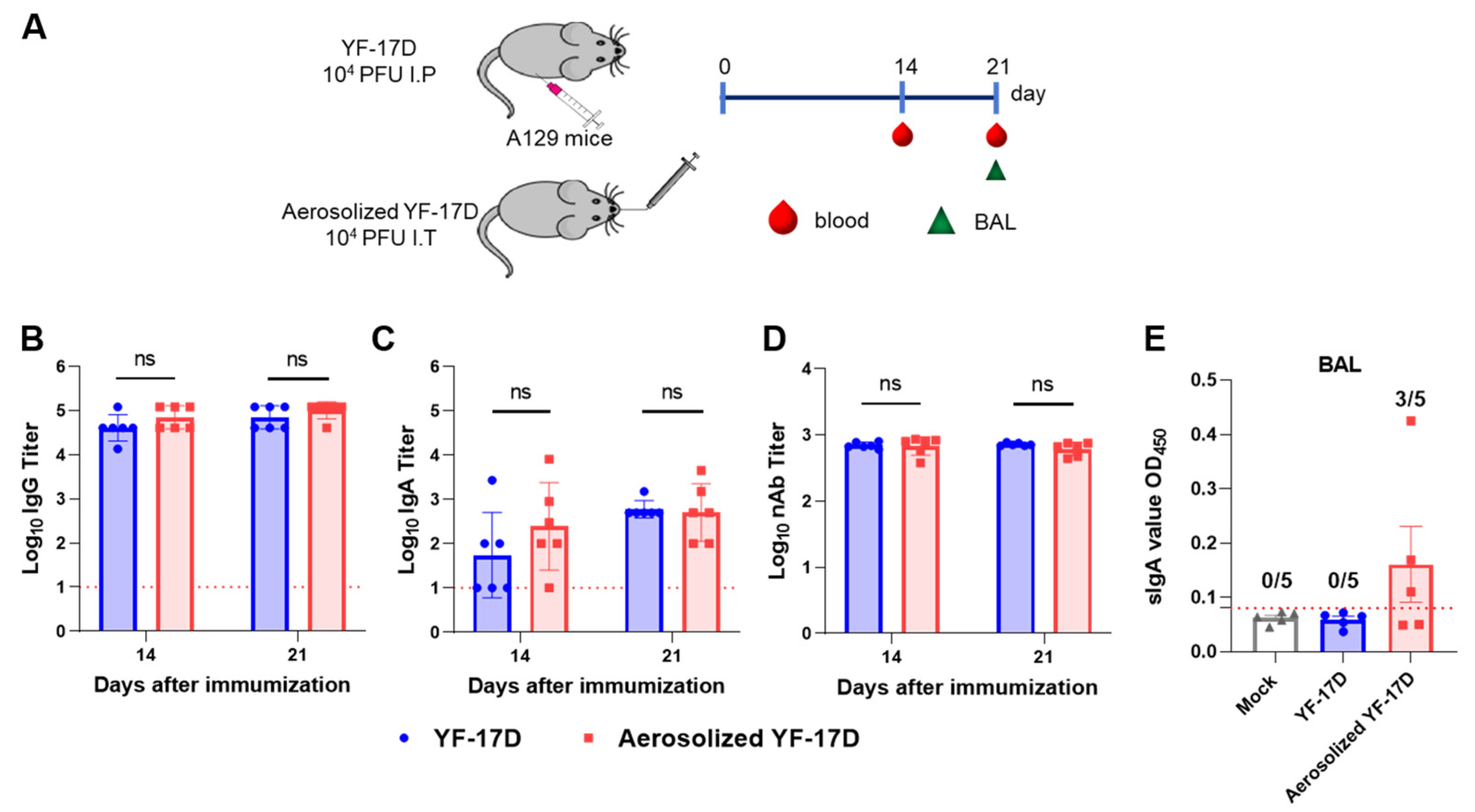
3.2. Aerosolized YF-17D Induced Humoral and Mucosal Immune Response
3.3. Aerosolized YF-17D Induced Cellular Immune Response
3.4. Aerosolized YF-17D Conferred Full Protection against Lethal YFV Challenge
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hansen, C.A.; Barrett, A.D.T. The Present and Future of Yellow Fever Vaccines. Pharmaceuticals 2021, 14, 891. [Google Scholar] [CrossRef] [PubMed]
- Tomori, O. Yellow fever: The recurring plague. Crit. Rev. Clin. Lab. Sci. 2004, 41, 391–427. [Google Scholar] [CrossRef]
- Gardner, C.L.; Ryman, K.D. Yellow fever: A reemerging threat. Clin. Lab. Med. 2010, 30, 237–260. [Google Scholar] [CrossRef]
- Waggoner, J.J.; Rojas, A.; Pinsky, B.A. Yellow Fever Virus: Diagnostics for a Persistent Arboviral Threat. J. Clin. Microbiol. 2018, 56, e00827-18. [Google Scholar] [CrossRef] [PubMed]
- Monath, T.P.; Vasconcelos, P.F. Yellow fever. J. Clin. Virol. 2015, 64, 160–173. [Google Scholar] [CrossRef] [PubMed]
- Roukens, A.H.; Visser, L.G. Yellow fever vaccine: Past, present and future. Expert Opin. Biol. Ther. 2008, 8, 1787–1795. [Google Scholar] [CrossRef] [PubMed]
- Silva, N.I.O.; Sacchetto, L.; de Rezende, I.M.; Trindade, G.S.; LaBeaud, A.D.; de Thoisy, B.; Drumond, B.P. Recent sylvatic yellow fever virus transmission in Brazil: The news from an old disease. Virol. J. 2020, 17, 9. [Google Scholar] [CrossRef]
- Ma, J.; Boudewijns, R.; Sanchez-Felipe, L.; Mishra, N.; Vercruysse, T.; Kum, D.B.; Thibaut, H.J.; Neyts, J.; Dallmeier, K. Comparing immunogenicity and protective efficacy of the yellow fever 17D vaccine in mice. Emerg. Microbes Infect. 2021, 10, 2279–2290. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Felipe, L.; Alpizar, Y.A.; Ma, J.; Coelmont, L.; Dallmeier, K. YF17D-based vaccines–standing on the shoulders of a giant. Eur. J. Immunol. 2024, 54, e2250133. [Google Scholar] [CrossRef]
- Gotuzzo, E.; Yactayo, S.; Cordova, E. Efficacy and duration of immunity after yellow fever vaccination: Systematic review on the need for a booster every 10 years. Am. J. Trop. Med. Hyg. 2013, 89, 434–444. [Google Scholar] [CrossRef]
- Wieten, R.W.; Jonker, E.F.; van Leeuwen, E.M.; Remmerswaal, E.B.; Ten Berge, I.J.; de Visser, A.W.; van Genderen, P.J.; Goorhuis, A.; Visser, L.G.; Grobusch, M.P.; et al. A Single 17D Yellow Fever Vaccination Provides Lifelong Immunity; Characterization of Yellow-Fever-Specific Neutralizing Antibody and T-Cell Responses after Vaccination. PLoS ONE 2016, 11, e0149871. [Google Scholar] [CrossRef] [PubMed]
- Staples, J.E.; Barrett, A.D.T.; Wilder-Smith, A.; Hombach, J. Review of data and knowledge gaps regarding yellow fever vaccine-induced immunity and duration of protection. NPJ Vaccines 2020, 5, 54. [Google Scholar] [CrossRef] [PubMed]
- Lemmens, V.; Kelchtermans, L.; Debaveye, S.; Chiu, W.; Vercruysse, T.; Ma, J.; Thibaut, H.J.; Neyts, J.; Sanchez-Felipe, L.; Dallmeier, K. YF17D-vectored Ebola vaccine candidate protects mice against lethal surrogate Ebola and yellow fever virus challenge. NPJ Vaccines 2023, 8, 99. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Felipe, L.; Vercruysse, T.; Sharma, S.; Ma, J.; Lemmens, V.; Van Looveren, D.; Arkalagud Javarappa, M.P.; Boudewijns, R.; Malengier-Devlies, B.; Liesenborghs, L.; et al. A single-dose live-attenuated YF17D-vectored SARS-CoV-2 vaccine candidate. Nature 2021, 590, 320–325. [Google Scholar] [CrossRef] [PubMed]
- Gan, C.; Luo, W.; Yu, Y.; Jiao, Z.; Li, S.; Su, D.; Feng, J.; Zhao, X.; Qiu, Y.; Hu, L.; et al. Intratracheal inoculation of AHc vaccine induces protection against aerosolized botulinum neurotoxin A challenge in mice. NPJ Vaccines 2021, 6, 87. [Google Scholar] [CrossRef] [PubMed]
- Ma, J.; Yakass, M.B.; Jansen, S.; Malengier-Devlies, B.; Van Looveren, D.; Sanchez-Felipe, L.; Vercruysse, T.; Weynand, B.; Javarappa, M.P.A.; Quaye, O.; et al. Live-attenuated YF17D-vectored COVID-19 vaccine protects from lethal yellow fever virus infection in mouse and hamster models. EBioMedicine 2022, 83, 104240. [Google Scholar] [CrossRef]
- Erickson, A.K.; Pfeiffer, J.K. Spectrum of disease outcomes in mice infected with YFV-17D. J. Gen. Virol. 2015, 96, 1328–1339. [Google Scholar] [CrossRef]
- Piras-Douce, F.; Raynal, F.; Raquin, A.; Girerd-Chambaz, Y.; Gautheron, S.; Sanchez, M.E.N.; Vangelisti, M.; Mantel, N. Next generation live-attenuated yel-low fever vaccine candidate: Safety and immuno-efficacy in small animal models. Vaccine 2021, 39, 1846–1856. [Google Scholar] [CrossRef]
- Kum, D.B.; Mishra, N.; Boudewijns, R.; Gladwyn-Ng, I.; Alfano, C.; Ma, J.; Schmid, M.A.; Marques, R.E.; Schols, D.; Kaptein, S.; et al. A yellow fever-Zika chimeric virus vaccine candidate protects against Zika infection and congenital malformations in mice. NPJ Vaccines 2018, 3, 56. [Google Scholar] [CrossRef]
- Shakya, A.K.; Chowdhury, M.Y.E.; Tao, W.; Gill, H.S. Mucosal vaccine delivery: Current state and a pediatric perspective. J. Control. Release 2016, 240, 394–413. [Google Scholar] [CrossRef]
- Lu, D.; Hickey, A.J. Pulmonary vaccine delivery. Expert Rev. Vaccines 2007, 6, 213–226. [Google Scholar] [CrossRef] [PubMed]
- Zhou, F.; Huang, L.; Li, S.; Yang, W.; Chen, F.; Cai, Z.; Liu, X.; Xu, W.; Lehto, V.P.; Lächelt, U.; et al. From structural design to delivery: mRNA therapeutics for cancer immunotherapy. Exploration 2023, 4, 20210146. [Google Scholar] [CrossRef] [PubMed]
- Bhide, Y.; Tomar, J.; Dong, W.; de Vries-Idema, J.; Frijlink, H.W.; Huckriede, A.; Hinrichs, W.L. Pulmonary delivery of influenza vaccine formulations in cotton rats: Site of deposition plays a minor role in the protective efficacy against clinical isolate of H1N1pdm virus. Drug Deliv. 2018, 25, 533–545. [Google Scholar] [CrossRef] [PubMed]
- Lin, W.-H.; Griffin, D.E.; Rota, P.A.; Papania, M.; Cape, S.P.; Bennett, D.; Quinn, B.; Sievers, R.E.; Shermer, C.; Powell, K.; et al. Successful respiratory immunization with dry powder live-attenuated measles virus vaccine in rhesus macaques. Proc. Natl. Acad. Sci. USA 2011, 108, 2987–2992. [Google Scholar] [CrossRef] [PubMed]
- Qiu, H.-Y.; Zhang, N.-N.; Ma, Q.-Q.; Li, R.-T.; Guan, M.-Y.; Zhang, L.-L.; Zhou, J.; Zhang, R.-R.; Huang, X.-Y.; Yang, W.-H.; et al. Aerosolized Zika virus infection in Guinea pigs. Emerg. Microbes Infect. 2022, 11, 2350–2358. [Google Scholar] [CrossRef]
- Ma, B.; Tao, M.; Li, Z.; Zheng, Q.; Wu, H.; Chen, P. Mucosal vaccines for viral diseases: Status and prospects. Virology 2024, 593, 110026. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.-J.; Guo, Y.; He, M.-J.; Liu, Z.-Y.; Ye, Q.; Huang, X.-Y.; Deng, Y.-Q.; Li, X.-F.; Qin, C.-F. Development of a Bicistronic Yellow Fever Live Attenuated Vaccine with Reduced Neurovirulence and Viscerotropism. Microbiol. Spectr. 2022, 10, e0224622. [Google Scholar] [CrossRef] [PubMed]
- Mason, R.A.; Tauraso, N.M.; Spertzel, R.O.; Ginn, R.K. Yellow fever vaccine: Direct challenge of monkeys given graded doses of 17D vaccine. Appl. Microbiol. 1973, 25, 539–544. [Google Scholar] [CrossRef] [PubMed]
- Akondy, R.S.; Monson, N.D.; Miller, J.D.; Edupuganti, S.; Teuwen, D.; Wu, H.; Quyyumi, F.; Garg, S.; Altman, J.D.; Del Rio, C.; et al. The yellow fever virus vaccine induces a broad and polyfunctional human memory CD8+ T cell response. J. Immunol. 2009, 183, 7919–7930. [Google Scholar] [CrossRef]
- James, E.A.; LaFond, R.E.; Gates, T.J.; Mai, D.T.; Malhotra, U.; Kwok, W.W. Yellow fever vaccination elicits broad functional CD4+ T cell responses that recognize structural and nonstructural proteins. J. Virol. 2013, 87, 12794–12804. [Google Scholar] [CrossRef]
- Niedrig, M.; Stolte, N.; Fuchs, D.; Hunsmann, G.; Stahl-Hennig, C. Intra-nasal infection of macaques with Yellow Fever (YF) vaccine strain 17D: A novel and economical approach for YF vaccination in man. Vaccine 1999, 17, 1206–1210. [Google Scholar] [CrossRef] [PubMed]
- Ye, T.; Jiao, Z.; Li, X.; He, Z.; Li, Y.; Yang, F.; Zhao, X.; Wang, Y.; Huang, W.; Qin, M.; et al. Inhaled SARS-CoV-2 vaccine for single-dose dry powder aerosol immunization. Nature 2023, 624, 630–638. [Google Scholar] [CrossRef] [PubMed]
- Gianchecchi, E.; Cianchi, V.; Torelli, A.; Montomoli, E. Yellow Fever: Origin, Epidemiology, Preventive Strategies and Future Prospects. Vaccines 2022, 10, 372. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.H.; Wilson, M.E. Yellow fever control: Current epidemiology and vaccination strategies. Trop. Dis. Travel. Med. Vaccines 2020, 6, 1. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhu, F.; Sun, M.-X.; Zhao, S.-Q.; Qin, C.-F.; Wang, J.-H.; Deng, Y.-Q. Immunogenicity and Protective Efficacy of Aerosolized Live-Attenuated Yellow Fever 17D Vaccine in Mice. Vaccines 2024, 12, 856. https://doi.org/10.3390/vaccines12080856
Zhu F, Sun M-X, Zhao S-Q, Qin C-F, Wang J-H, Deng Y-Q. Immunogenicity and Protective Efficacy of Aerosolized Live-Attenuated Yellow Fever 17D Vaccine in Mice. Vaccines. 2024; 12(8):856. https://doi.org/10.3390/vaccines12080856
Chicago/Turabian StyleZhu, Feng, Meng-Xu Sun, Suo-Qun Zhao, Cheng-Feng Qin, Jin-Hua Wang, and Yong-Qiang Deng. 2024. "Immunogenicity and Protective Efficacy of Aerosolized Live-Attenuated Yellow Fever 17D Vaccine in Mice" Vaccines 12, no. 8: 856. https://doi.org/10.3390/vaccines12080856




