Virulence and Immune Evasion Strategies of FMDV: Implications for Vaccine Design
Abstract
1. Introduction
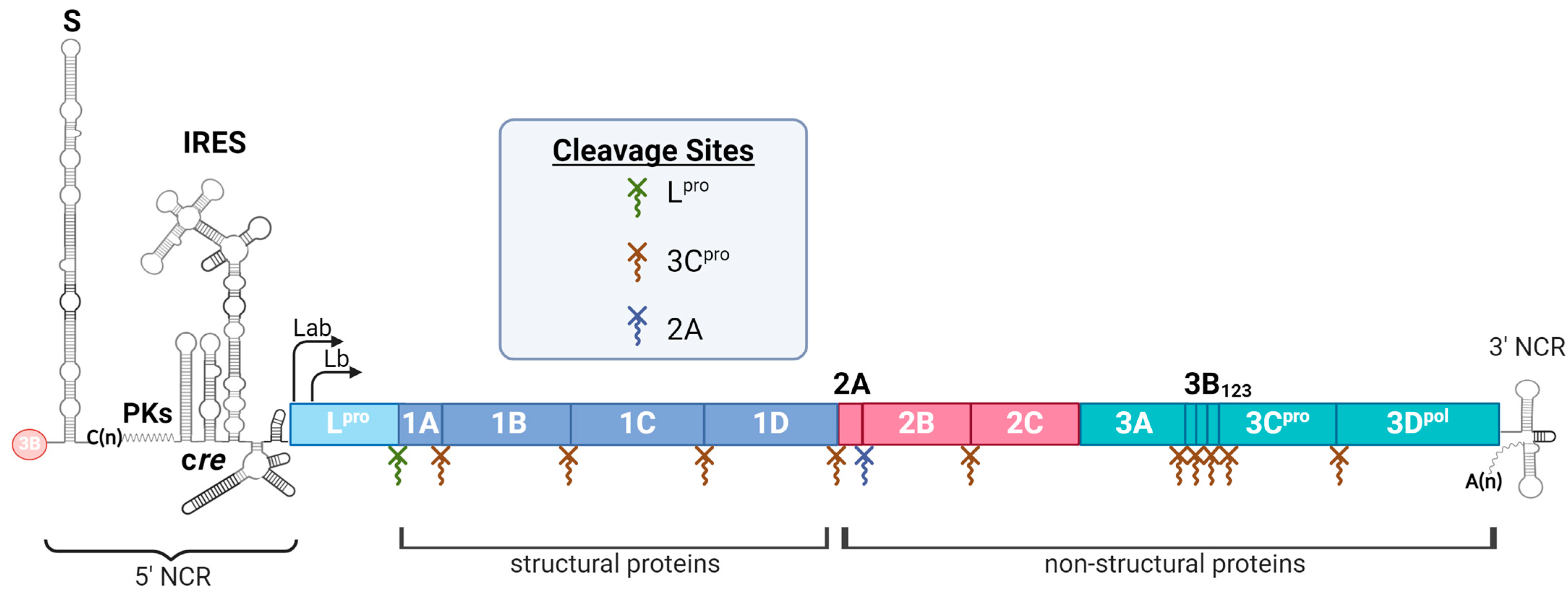
2. Virulence Factors of FMDV and Their Roles in Immune Evasion
2.1. Non-Coding Regions (NCRs)
2.2. Non-Structural Proteins (NSPs)
2.2.1. Lpro
2.2.2. 2B
2.2.3. 2C
2.2.4. 3A
2.2.5. 3B
2.2.6. 3C
2.2.7. 3D
2.3. Structural Proteins (SPs)
3. Host Pathogenesis and Immune Response to Understand FMDV in In Vivo Immune Evasion Strategies
4. Pathogenesis
5. Innate Immune Responses In Vivo
5.1. Cytokine Immune Response
5.2. Cellular Immune Response
6. Adaptive Immune Responses In Vivo
6.1. Humoral Immune Response
6.2. Cellular Immune Response
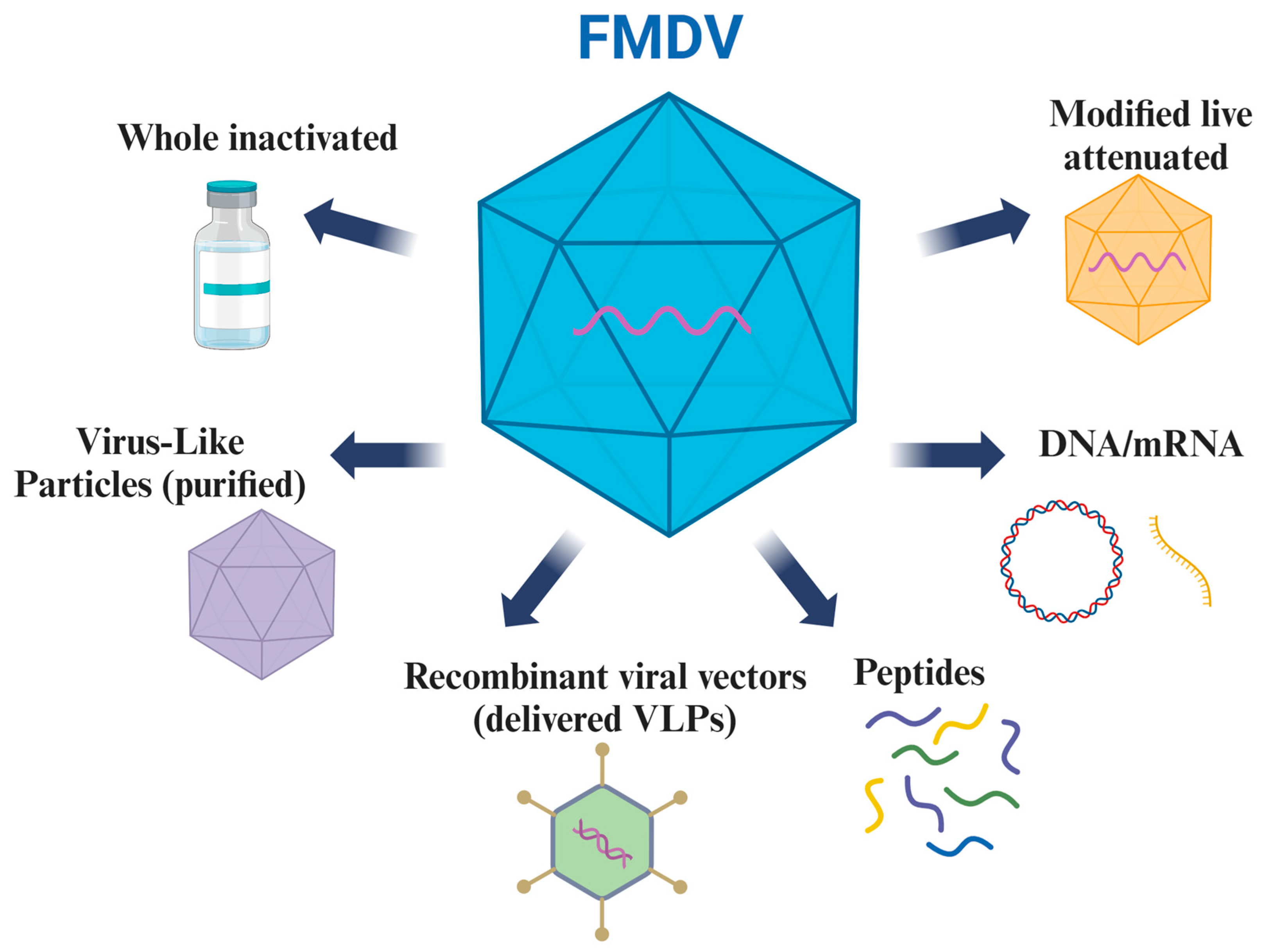
7. Vaccine Design Strategies against FMDV
7.1. Inactivated Vaccine Platform
7.2. Virus-like Particle Vaccine Platform
7.3. Synthetic Peptide and DNA Vaccine Platforms
7.4. Modified Live-Attenuated Vaccine Platform
7.5. Potential Use of Novel Technologies
8. Conclusions and Future Directions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Paton, D.J.; Di Nardo, A.; Knowles, N.J.; Wadsworth, J.; Pituco, E.M.; Cosivi, O.; Rivera, A.M.; Kassimi, L.B.; Brocchi, E.; de Clercq, K.; et al. The history of foot-and-mouth disease virus serotype C: The first known extinct serotype? Virus Evol. 2021, 7, veab009. [Google Scholar] [CrossRef] [PubMed]
- Yoon, S.H.; Park, W.; King, D.P.; Kim, H. Phylogenomics and molecular evolution of foot-and-mouth disease virus. Mol. Cells 2011, 31, 413–421. [Google Scholar] [CrossRef] [PubMed]
- Grant, C.F.J.; Carr, B.V.; Kotecha, A.; van den Born, E.; Stuart, D.I.; Hammond, J.A.; Charleston, B. The B Cell Response to Foot-and-Mouth Disease Virus in Cattle following Sequential Vaccination with Multiple Serotypes. J. Virol. 2017, 91, 10–1128. [Google Scholar] [CrossRef] [PubMed]
- Alexandersen, S.; Mowat, N. Foot-and-mouth disease: Host range and pathogenesis. Curr. Top. Microbiol. Immunol. 2005, 288, 9–42. [Google Scholar]
- Paton, D.J.; Gubbins, S.; King, D.P. Understanding the transmission of foot-and-mouth disease virus at different scales. Curr. Opin. Virol. 2018, 28, 85–91. [Google Scholar] [CrossRef]
- Arzt, J.; Pacheco, J.M.; Rodriguez, L.L. The early pathogenesis of foot-and-mouth disease in cattle after aerosol inoculation. Identification of the nasopharynx as the primary site of infection. Vet. Pathol. 2010, 47, 1048–1063. [Google Scholar] [CrossRef] [PubMed]
- Nathanson, N.; González-Scarano, F. Patterns of Infection: Unwanted Guests—Quick Visits and Extended Stays. In Viral Pathogenesis; Katze, M.G., Korth, M.J., Law, G.L., Nathanson, N., Eds.; Academic Press: New York, NY, USA, 2016; pp. 81–94. [Google Scholar]
- Domingo, E.; Garcia-Crespo, C.; Perales, C. Historical Perspective on the Discovery of the Quasispecies Concept. Annu. Rev. Virol. 2021, 8, 51–72. [Google Scholar] [CrossRef]
- LaRocco, M.; Ahmed, Z.; Rodriguez-Calzada, M.; Azzinaro, P.A.; Barrette, R.; Krug, P.; Rodriguez, L.L.; de Los Santos, T.; Medina, G.N. An adventitious agent-free clonal cell line that is highly susceptible to foot -and-mouth disease virus. Biologicals 2021, 72, 33–41. [Google Scholar] [CrossRef]
- Harvey, Y.; Jackson, B.; Carr, B.V.; Childs, K.; Moffat, K.; Freimanis, G.; Tennakoon, C.; Juleff, N.; Seago, J. An Improved alphavbeta6-Receptor-Expressing Suspension Cell Line for Foot-and-Mouth Disease Vaccine Production. Viruses 2022, 14, 621. [Google Scholar] [CrossRef]
- Brehm, K.E.; Kumar, N.; Thulke, H.H.; Haas, B. High potency vaccines induce protection against heterologous challenge with foot-and-mouth disease virus. Vaccine 2008, 26, 1681–1687. [Google Scholar] [CrossRef] [PubMed]
- Dekker, A.; Sanz-Bernardo, B.; Singanallur, N.B.; Ludi, A.B.; Horsington, J.; Eble, P.L.; King, D.P.; Vosloo, W. Cross-Protection Induced by a A/MAY/97 Emergency Vaccine Against Intra-Serotype Heterologous Challenge with a Foot-and-Mouth Disease Virus from the A/ASIA/G-VII Lineage. Vaccines 2020, 8, 24. [Google Scholar] [CrossRef] [PubMed]
- Galdo Novo, S.; Malirat, V.; Maradei, E.D.; Pedemonte, A.R.; Espinoza, A.M.; Smitsaart, E.; Lee, K.N.; Park, J.H.; Bergmann, I.E. Efficacy of a high quality O1/Campos foot-and-mouth disease vaccine upon challenge with a heterologous Korean O Mya98 lineage virus in pigs. Vaccine 2018, 36, 1570–1576. [Google Scholar] [CrossRef] [PubMed]
- Fishbourne, E.; Ludi, A.B.; Wilsden, G.; Hamblin, P.; Statham, B.; Bin-Tarif, A.; Brocchi, E.; Grazioli, S.; Dekker, A.; Eblé, P.; et al. Efficacy of a high potency O1 Manisa foot-and-mouth disease vaccine in cattle against heterologous challenge with a field virus from the O/ME-SA/Ind-2001 lineage collected in North Africa. Vaccine 2017, 35, 2761–2765. [Google Scholar] [CrossRef] [PubMed]
- Scott, K.A.; Kotecha, A.; Seago, J.; Ren, J.; Fry, E.E.; Stuart, D.I.; Charleston, B.; Maree, F.F. SAT2 Foot-and-Mouth Disease Virus Structurally Modified for Increased Thermostability. J. Virol. 2017, 91, 10–1128. [Google Scholar] [CrossRef] [PubMed]
- Dong, H.; Lu, Y.; Zhang, Y.; Mu, S.; Wang, N.; Du, P.; Zhi, X.; Wen, X.; Wang, X.; Sun, S.; et al. A Heat-Induced Mutation on VP1 of Foot-and-Mouth Disease Virus Serotype O Enhanced Capsid Stability and Immunogenicity. J. Virol. 2021, 95, e0017721. [Google Scholar] [CrossRef]
- Lopez-Arguello, S.; Rincon, V.; Rodriguez-Huete, A.; Martinez-Salas, E.; Belsham, G.J.; Valbuena, A.; Mateu, M.G. Thermostability of the Foot-and-Mouth Disease Virus Capsid Is Modulated by Lethal and Viability-Restoring Compensatory Amino Acid Substitutions. J. Virol. 2019, 93, 10–1128. [Google Scholar] [CrossRef]
- Yuan, H.; Li, P.; Bao, H.; Sun, P.; Bai, X.; Bai, Q.; Li, N.; Ma, X.; Cao, Y.; Fu, Y.; et al. Engineering viable foot-and-mouth disease viruses with increased acid stability facilitate the development of improved vaccines. Appl. Microbiol. Biotechnol. 2020, 104, 1683–1694. [Google Scholar] [CrossRef]
- Kotecha, A.; Perez-Martin, E.; Harvey, Y.; Zhang, F.; Ilca, S.L.; Fry, E.E.; Jackson, B.; Maree, F.; Scott, K.; Hecksel, C.W.; et al. Chimeric O1K foot-and-mouth disease virus with SAT2 outer capsid as an FMD vaccine candidate. Sci. Rep. 2018, 8, 13654. [Google Scholar] [CrossRef]
- Li, P.; Huang, S.; Zha, J.; Sun, P.; Li, D.; Bao, H.; Cao, Y.; Bai, X.; Fu, Y.; Ma, X.; et al. Evaluation of immunogenicity and cross-reactive responses of vaccines prepared from two chimeric serotype O foot-and-mouth disease viruses in pigs and cattle. Vet. Res. 2022, 53, 56. [Google Scholar] [CrossRef]
- Rieder, E.; Bunch, T.; Brown, F.; Mason, P.W. Genetically engineered foot-and-mouth disease viruses with poly(C) tracts of two nucleotides are virulent in mice. J. Virol. 1993, 67, 5139–5145. [Google Scholar] [CrossRef]
- Li, P.; Bai, X.; Sun, P.; Li, D.; Lu, Z.; Cao, Y.; Fu, Y.; Bao, H.; Chen, Y.; Xie, B.; et al. Evaluation of a genetically modified foot-and-mouth disease virus vaccine candidate generated by reverse genetics. BMC Vet. Res. 2012, 8, 57. [Google Scholar] [CrossRef] [PubMed]
- Uddowla, S.; Hollister, J.; Pacheco, J.M.; Rodriguez, L.L.; Rieder, E. A safe foot-and-mouth disease vaccine platform with two negative markers for differentiating infected from vaccinated animals. J. Virol. 2012, 86, 11675–11685. [Google Scholar] [CrossRef] [PubMed]
- Hardham, J.M.; Krug, P.; Pacheco, J.M.; Thompson, J.; Dominowski, P.; Moulin, V.; Gay, C.G.; Rodriguez, L.L.; Rieder, E. Novel Foot-and-Mouth Disease Vaccine Platform: Formulations for Safe and DIVA-Compatible FMD Vaccines With Improved Potency. Front. Vet. Sci. 2020, 7, 554305. [Google Scholar] [CrossRef]
- Steigerwald, R.; Brake, D.A.; Barrera, J.; Schutta, C.J.; Kalla, M.; Wennier, S.T.; Volkmann, A.; Hurtle, W.; Clark, B.A.; Zurita, M.; et al. Evaluation of modified Vaccinia Ankara-based vaccines against foot-and-mouth disease serotype A24 in cattle. Vaccine 2020, 38, 769–778. [Google Scholar] [CrossRef]
- Ma, M.; Jin, N.; Shen, G.; Zhu, G.; Liu, H.J.; Zheng, M.; Lu, H.; Huo, X.; Jin, M.; Yin, G.; et al. Immune responses of swine inoculated with a recombinant fowlpox virus co-expressing P12A and 3C of FMDV and swine IL-18. Vet. Immunol. Immunopathol. 2008, 121, 1–7. [Google Scholar] [CrossRef]
- Hong, Q.; Qian, P.; Li, X.M.; Yu, X.L.; Chen, H.C. A recombinant pseudorabies virus co-expressing capsid proteins precursor P1-2A of FMDV and VP2 protein of porcine parvovirus: A trivalent vaccine candidate. Biotechnol. Lett. 2007, 29, 1677–1683. [Google Scholar] [CrossRef]
- Gullberg, M.; Lohse, L.; Botner, A.; McInerney, G.M.; Burman, A.; Jackson, T.; Polacek, C.; Belsham, G.J. A Prime-Boost Vaccination Strategy in Cattle to Prevent Foot-and-Mouth Disease Using a “Single-Cycle” Alphavirus Vector and Empty Capsid Particles. PLoS ONE 2016, 11, e0157435. [Google Scholar] [CrossRef]
- Mayr, G.A.; Chinsangaram, J.; Grubman, M.J. Development of replication-defective adenovirus serotype 5 containing the capsid and 3C protease coding regions of foot-and-mouth disease virus as a vaccine candidate. Virology 1999, 263, 496–506. [Google Scholar] [CrossRef] [PubMed]
- Moraes, M.P.; Mayr, G.A.; Mason, P.W.; Grubman, M.J. Early protection against homologous challenge after a single dose of replication-defective human adenovirus type 5 expressing capsid proteins of foot-and-mouth disease virus (FMDV) strain A24. Vaccine 2002, 20, 1631–1639. [Google Scholar] [CrossRef]
- Pena, L.; Moraes, M.P.; Koster, M.; Burrage, T.; Pacheco, J.M.; Segundo, F.D.; Grubman, M.J. Delivery of a foot-and-mouth disease virus empty capsid subunit antigen with nonstructural protein 2B improves protection of swine. Vaccine 2008, 26, 5689–5699. [Google Scholar] [CrossRef]
- Grubman, M.J.; Diaz-San Segundo, F.; Dias, C.C.; Moraes, M.; Perez-Martin, E.; de Los Santos, T. Use of replication-defective adenoviruses to develop vaccines and biotherapeutics against foot-and-mouth disease. Future Virol. 2012, 7, 12. [Google Scholar] [CrossRef]
- Schutta, C.; Barrera, J.; Pisano, M.; Zsak, L.; Grubman, M.J.; Mayr, G.A.; Moraes, M.P.; Kamicker, B.J.; Brake, D.A.; Ettyreddy, D.; et al. Multiple efficacy studies of an adenovirus-vectored foot-and-mouth disease virus serotype A24 subunit vaccine in cattle using homologous challenge. Vaccine 2016, 34, 3214–3220. [Google Scholar] [CrossRef] [PubMed]
- Zhi, Y.; Ji, H.J.; Guo, H.; Lim, J.H.; Byun, E.B.; Kim, W.S.; Seo, H.S. Salmonella Vaccine Vector System for Foot-and-Mouth Disease Virus and Evaluation of Its Efficacy with Virus-Like Particles. Vaccines 2021, 9, 22. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Qi, L.; Lv, J.; Zhang, Z.; Zhou, P.; Ma, Z.; Wang, Y.; Zhang, Y.; Pan, L. The immune response to a recombinant Lactococcus lactis oral vaccine against foot-and-mouth disease virus in mice. Biotechnol. Lett. 2020, 42, 1907–1917. [Google Scholar] [CrossRef] [PubMed]
- Kotecha, A.; Seago, J.; Scott, K.; Burman, A.; Loureiro, S.; Ren, J.; Porta, C.; Ginn, H.M.; Jackson, T.; Perez-Martin, E.; et al. Structure-based energetics of protein interfaces guides foot-and-mouth disease virus vaccine design. Nat. Struct. Mol. Biol. 2015, 22, 788–794. [Google Scholar] [CrossRef] [PubMed]
- Porta, C.; Kotecha, A.; Burman, A.; Jackson, T.; Ren, J.; Loureiro, S.; Jones, I.M.; Fry, E.E.; Stuart, D.I.; Charleston, B. Rational engineering of recombinant picornavirus capsids to produce safe, protective vaccine antigen. PLoS Pathog. 2013, 9, e1003255. [Google Scholar] [CrossRef]
- Ganji, V.K.; Biswal, J.K.; Lalzampuia, H.; Basagoudanavar, S.H.; Saravanan, P.; Tamil Selvan, R.P.; Umapathi, V.; Reddy, G.R.; Sanyal, A.; Dechamma, H.J. Mutation in the VP2 gene of P1-2A capsid protein increases the thermostability of virus-like particles of foot-and-mouth disease virus serotype O. Appl. Microbiol. Biotechnol. 2018, 102, 8883–8893. [Google Scholar] [CrossRef]
- Xiao, Y.; Chen, H.Y.; Wang, Y.; Yin, B.; Lv, C.; Mo, X.; Yan, H.; Xuan, Y.; Huang, Y.; Pang, W.; et al. Large-scale production of foot-and-mouth disease virus (serotype Asia1) VLP vaccine in Escherichia coli and protection potency evaluation in cattle. BMC Biotechnol. 2016, 16, 56. [Google Scholar] [CrossRef]
- Song, H.; Waheed Abdullah, S.; Yin, S.; Dong, H.; Zhang, Y.; Tan, S.; Bai, M.; Ding, Y.; Teng, Z.; Sun, S.; et al. Virus-like particle-based multipathogen vaccine of FMD and SVA elicits balanced and broad protective efficacy in mice and pigs. Vaccine 2024, 42, 3789–3801. [Google Scholar] [CrossRef]
- Dus Santos, M.J.; Carrillo, C.; Ardila, F.; Rios, R.D.; Franzone, P.; Piccone, M.E.; Wigdorovitz, A.; Borca, M.V. Development of transgenic alfalfa plants containing the foot and mouth disease virus structural polyprotein gene P1 and its utilization as an experimental immunogen. Vaccine 2005, 23, 1838–1843. [Google Scholar] [CrossRef]
- Veerapen, V.P.; van Zyl, A.R.; Wigdorovitz, A.; Rybicki, E.P.; Meyers, A.E. Novel expression of immunogenic foot-and-mouth disease virus-like particles in Nicotiana benthamiana. Virus Res. 2017, 244, 213–217. [Google Scholar] [CrossRef] [PubMed]
- Puckette, M.; Primavera, V.; Martel, E.; Barrera, J.; Hurtle, W.; Clark, B.; Kamicker, B.; Zurita, M.; Brake, D.; Neilan, J. Transiently Transfected Mammalian Cell Cultures: An Adaptable and Effective Platform for Virus-like Particle-Based Vaccines against Foot-and-Mouth Disease Virus. Viruses 2022, 14, 989. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.Y.; Chang, T.Y.; Walfield, A.M.; Ye, J.; Shen, M.; Chen, S.P.; Li, M.C.; Lin, Y.L.; Jong, M.H.; Yang, P.C.; et al. Effective synthetic peptide vaccine for foot-and-mouth disease in swine. Vaccine 2002, 20, 2603–2610. [Google Scholar] [CrossRef]
- Rodriguez, L.L.; Barrera, J.; Kramer, E.; Lubroth, J.; Brown, F.; Golde, W.T. A synthetic peptide containing the consensus sequence of the G-H loop region of foot-and-mouth disease virus type-O VP1 and a promiscuous T-helper epitope induces peptide-specific antibodies but fails to protect cattle against viral challenge. Vaccine 2003, 21, 3751–3756. [Google Scholar] [CrossRef] [PubMed]
- Blanco, E.; Guerra, B.; de la Torre, B.G.; Defaus, S.; Dekker, A.; Andreu, D.; Sobrino, F. Full protection of swine against foot-and-mouth disease by a bivalent B-cell epitope dendrimer peptide. Antivir. Res. 2016, 129, 74–80. [Google Scholar] [CrossRef]
- Soria, I.; Quattrocchi, V.; Langellotti, C.; Gammella, M.; Digiacomo, S.; Garcia de la Torre, B.; Andreu, D.; Montoya, M.; Sobrino, F.; Blanco, E.; et al. Dendrimeric peptides can confer protection against foot-and-mouth disease virus in cattle. PLoS ONE 2017, 12, e0185184. [Google Scholar] [CrossRef]
- Fowler, V.; Robinson, L.; Bankowski, B.; Cox, S.; Parida, S.; Lawlor, C.; Gibson, D.; O’Brien, F.; Ellefsen, B.; Hannaman, D.; et al. A DNA vaccination regime including protein boost and electroporation protects cattle against foot-and-mouth disease. Antivir. Res. 2012, 94, 25–34. [Google Scholar] [CrossRef] [PubMed]
- Borrego, B.; Argilaguet, J.M.; Perez-Martin, E.; Dominguez, J.; Perez-Filgueira, M.; Escribano, J.M.; Sobrino, F.; Rodriguez, F. A DNA vaccine encoding foot-and-mouth disease virus B and T-cell epitopes targeted to class II swine leukocyte antigens protects pigs against viral challenge. Antivir. Res. 2011, 92, 359–363. [Google Scholar] [CrossRef]
- Gulce Iz, S.; Doskaya, M.; Borrego, B.; Rodriguez, F.; Guruz, Y.; Gurhan, I.D. Co-expression of the Bcl-xL antiapoptotic protein enhances the induction of Th1-like immune responses in mice immunized with DNA vaccines encoding FMDV B and T cell epitopes. Vet. Res. Commun. 2013, 37, 187–196. [Google Scholar] [CrossRef]
- Diaz-San Segundo, F.; Weiss, M.; Perez-Martin, E.; Dias, C.C.; Grubman, M.J.; Santos Tde, L. Inoculation of swine with foot-and-mouth disease SAP-mutant virus induces early protection against disease. J. Virol. 2012, 86, 1316–1327. [Google Scholar] [CrossRef]
- Medina, G.N.; Azzinaro, P.; Ramirez-Medina, E.; Gutkoska, J.; Fang, Y.; Diaz-San Segundo, F.; de Los Santos, T. Impairment of the DeISGylation Activity of Foot-and-Mouth Disease Virus Lpro Causes Attenuation In Vitro and In Vivo. J. Virol. 2020, 94, 10–1128. [Google Scholar] [CrossRef] [PubMed]
- Azzinaro, P.A.; Medina, G.N.; Rai, D.; Ramirez-Medina, E.; Spinard, E.; Rodriguez-Calzada, M.; Zhu, J.; Rieder, E.; de Los Santos, T.; Diaz-San Segundo, F. Mutation of FMDV L(pro) H138 residue drives viral attenuation in cell culture and in vivo in swine. Front. Vet. Sci. 2022, 9, 1028077. [Google Scholar] [CrossRef] [PubMed]
- Uddowla, S.; Pacheco, J.M.; Larson, C.; Bishop, E.; Rodriguez, L.L.; Rai, D.K.; Arzt, J.; Rieder, E. Characterization of a chimeric foot-and-mouth disease virus bearing a bovine rhinitis B virus leader proteinase. Virology 2013, 447, 172–180. [Google Scholar] [CrossRef] [PubMed]
- Rai, D.K.; Diaz-San Segundo, F.; Campagnola, G.; Keith, A.; Schafer, E.A.; Kloc, A.; de Los Santos, T.; Peersen, O.; Rieder, E. Attenuation of Foot-and-Mouth Disease Virus by Engineered Viral Polymerase Fidelity. J. Virol. 2017, 91, 10–1128. [Google Scholar] [CrossRef]
- Rodríguez Pulido, M.; Sobrino, F.; Borrego, B.; Sáiz, M. Attenuated foot-and-mouth disease virus RNA carrying a deletion in the 3′ noncoding region can elicit immunity in swine. J. Virol. 2009, 83, 3475–3485. [Google Scholar] [CrossRef]
- Kloc, A.; Diaz-San Segundo, F.; Schafer, E.A.; Rai, D.K.; Kenney, M.; de Los Santos, T.; Rieder, E. Foot-and-mouth disease virus 5′-terminal S fragment is required for replication and modulation of the innate immune response in host cells. Virology 2017, 512, 132–143. [Google Scholar] [CrossRef]
- Diaz-San Segundo, F.; Medina, G.N.; Ramirez-Medina, E.; Velazquez-Salinas, L.; Koster, M.; Grubman, M.J.; de los Santos, T. Synonymous Deoptimization of Foot-and-Mouth Disease Virus Causes Attenuation In Vivo while Inducing a Strong Neutralizing Antibody Response. J. Virol. 2015, 90, 1298–1310. [Google Scholar] [CrossRef]
- Diaz-San Segundo, F.; Medina, G.N.; Spinard, E.; Kloc, A.; Ramirez-Medina, E.; Azzinaro, P.; Mueller, S.; Rieder, E.; de Los Santos, T. Use of Synonymous Deoptimization to Derive Modified Live Attenuated Strains of Foot and Mouth Disease Virus. Front. Microbiol. 2020, 11, 610286. [Google Scholar] [CrossRef]
- Medina, G.N.; Spinard, E.; Azzinaro, P.A.; Rodriguez-Calzada, M.; Gutkoska, J.; Kloc, A.; Rieder, E.A.; Taillon, B.E.; Mueller, S.; de Los Santos, T.; et al. Deoptimization of FMDV P1 Region Results in Robust Serotype-Independent Viral Attenuation. Viruses 2023, 15, 1332. [Google Scholar] [CrossRef] [PubMed]
- Herod, M.R.; Gold, S.; Lasecka-Dykes, L.; Wright, C.; Ward, J.C.; McLean, T.C.; Forrest, S.; Jackson, T.; Tuthill, T.J.; Rowlands, D.J.; et al. Genetic economy in picornaviruses: Foot-and-mouth disease virus replication exploits alternative precursor cleavage pathways. PLoS Pathog. 2017, 13, e1006666. [Google Scholar] [CrossRef]
- Gao, Y.; Sun, S.Q.; Guo, H.C. Biological function of Foot-and-mouth disease virus non-structural proteins and non-coding elements. Virol. J. 2016, 13, 107. [Google Scholar] [CrossRef]
- Rodriguez Pulido, M.; Saiz, M. Molecular Mechanisms of Foot-and-Mouth Disease Virus Targeting the Host Antiviral Response. Front. Cell Infect. Microbiol. 2017, 7, 252. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Pulido, M.; Borrego, B.; Sobrino, F.; Saiz, M. RNA structural domains in noncoding regions of the foot-and-mouth disease virus genome trigger innate immunity in porcine cells and mice. J. Virol. 2011, 85, 6492–6501. [Google Scholar] [CrossRef] [PubMed]
- Yang, F.; Zhu, Z.; Cao, W.; Liu, H.; Wei, T.; Zheng, M.; Zhang, K.; Jin, Y.; He, J.; Guo, J.; et al. Genetic Determinants of Altered Virulence of Type O Foot-and-Mouth Disease Virus. J. Virol. 2020, 94, 10–1128. [Google Scholar] [CrossRef] [PubMed]
- Penza, V.; Russell, S.J.; Schulze, A.J. The long-lasting enigma of polycytidine (polyC) tract. PLoS Pathog. 2021, 17, e1009739. [Google Scholar] [CrossRef]
- Escarmis, C.; Toja, M.; Medina, M.; Domingo, E. Modifications of the 5′ untranslated region of foot-and-mouth disease virus after prolonged persistence in cell culture. Virus Res. 1992, 26, 113–125. [Google Scholar] [CrossRef] [PubMed]
- Harris, T.J.; Brown, F. Biochemical analysis of a virulent and an avirulent strain of foot-and-mouth disease virus. J. Gen. Virol. 1977, 34, 87–105. [Google Scholar] [CrossRef]
- Costa Giomi, M.P.; Bergmann, I.E.; Scodeller, E.A.; Auge de Mello, P.; Gomez, I.; La Torre, J.L. Heterogeneity of the polyribocytidylic acid tract in aphthovirus: Biochemical and biological studies of viruses carrying polyribocytidylic acid tracts of different lengths. J. Virol. 1984, 51, 799–805. [Google Scholar] [CrossRef]
- Zhu, Z.; Yang, F.; Cao, W.; Liu, H.; Zhang, K.; Tian, H.; Dang, W.; He, J.; Guo, J.; Liu, X.; et al. The Pseudoknot Region of the 5′ Untranslated Region Is a Determinant of Viral Tropism and Virulence of Foot-and-Mouth Disease Virus. J. Virol. 2019, 93, 10–1128. [Google Scholar] [CrossRef]
- Ward, J.C.; Lasecka-Dykes, L.; Neil, C.; Adeyemi, O.O.; Gold, S.; McLean-Pell, N.; Wright, C.; Herod, M.R.; Kealy, D.; Warner, E.; et al. The RNA pseudoknots in foot-and-mouth disease virus are dispensable for genome replication, but essential for the production of infectious virus. PLoS Pathog. 2022, 18, e1010589. [Google Scholar] [CrossRef]
- Logan, G.; Newman, J.; Wright, C.F.; Lasecka-Dykes, L.; Haydon, D.T.; Cottam, E.M.; Tuthill, T.J. Deep Sequencing of Foot-and-Mouth Disease Virus Reveals RNA Sequences Involved in Genome Packaging. J. Virol. 2018, 92, 10–1128. [Google Scholar] [CrossRef] [PubMed]
- Yang, D.; Sun, C.; Gao, R.; Wang, H.; Liu, W.; Yu, K.; Zhou, G.; Zhao, B.; Yu, L. A Temperature-Dependent Translation Defect Caused by Internal Ribosome Entry Site Mutation Attenuates Foot-and-Mouth Disease Virus: Implications for Rational Vaccine Design. J. Virol. 2020, 94, 10–1128. [Google Scholar] [CrossRef] [PubMed]
- Serrano, P.; Pulido, M.R.; Saiz, M.; Martinez-Salas, E. The 3′ end of the foot-and-mouth disease virus genome establishes two distinct long-range RNA-RNA interactions with the 5′ end region. J. Gen. Virol. 2006, 87, 3013–3022. [Google Scholar] [CrossRef]
- Garcia-Nunez, S.; Gismondi, M.I.; Konig, G.; Berinstein, A.; Taboga, O.; Rieder, E.; Martinez-Salas, E.; Carrillo, E. Enhanced IRES activity by the 3′UTR element determines the virulence of FMDV isolates. Virology 2014, 448, 303–313. [Google Scholar] [CrossRef][Green Version]
- Lopez de Quinto, S.; Saiz, M.; de la Morena, D.; Sobrino, F.; Martinez-Salas, E. IRES-driven translation is stimulated separately by the FMDV 3′-NCR and poly(A) sequences. Nucleic Acids Res. 2002, 30, 4398–4405. [Google Scholar] [CrossRef]
- Han, S.; Wang, X.; Guan, J.; Wu, J.; Zhang, Y.; Li, P.; Liu, Z.; Abdullah, S.W.; Zhang, Z.; Jin, Y.; et al. Nucleolin Promotes IRES-Driven Translation of Foot-and-Mouth Disease Virus by Supporting the Assembly of Translation Initiation Complexes. J. Virol. 2021, 95, e0023821. [Google Scholar] [CrossRef]
- Rodriguez Pulido, M.; Serrano, P.; Saiz, M.; Martinez-Salas, E. Foot-and-mouth disease virus infection induces proteolytic cleavage of PTB, eIF3a,b, and PABP RNA-binding proteins. Virology 2007, 364, 466–474. [Google Scholar] [CrossRef]
- Abdullah, S.W.; Wu, J.; Zhang, Y.; Bai, M.; Guan, J.; Liu, X.; Sun, S.; Guo, H. DDX21, a Host Restriction Factor of FMDV IRES-Dependent Translation and Replication. Viruses 2021, 13, 1765. [Google Scholar] [CrossRef] [PubMed]
- Piccone, M.E.; Rieder, E.; Mason, P.W.; Grubman, M.J. The foot-and-mouth disease virus leader proteinase gene is not required for viral replication. J. Virol. 1995, 69, 5376–5382. [Google Scholar] [CrossRef]
- Liu, Y.; Zhu, Z.; Zhang, M.; Zheng, H. Multifunctional roles of leader protein of foot-and-mouth disease viruses in suppressing host antiviral responses. Vet. Res. 2015, 46, 127. [Google Scholar] [CrossRef]
- de los Santos, T.; Segundo, F.D.; Zhu, J.; Koster, M.; Dias, C.C.; Grubman, M.J. A conserved domain in the leader proteinase of foot-and-mouth disease virus is required for proper subcellular localization and function. J. Virol. 2009, 83, 1800–1810. [Google Scholar] [CrossRef] [PubMed]
- Eschbaumer, M.; Dill, V.; Carlson, J.C.; Arzt, J.; Stenfeldt, C.; Krug, P.W.; Hardham, J.M.; Stegner, J.E.; Rodriguez, L.L.; Rieder, E. Foot-and-Mouth Disease Virus Lacking the Leader Protein and Containing Two Negative DIVA Markers (FMDV LL3B3D A(24)) Is Highly Attenuated in Pigs. Pathogens 2020, 9, 129. [Google Scholar] [CrossRef] [PubMed]
- Mason, P.W.; Piccone, M.E.; McKenna, T.S.; Chinsangaram, J.; Grubman, M.J. Evaluation of a live-attenuated foot-and-mouth disease virus as a vaccine candidate. Virology 1997, 227, 96–102. [Google Scholar] [CrossRef]
- Brown, C.C.; Piccone, M.E.; Mason, P.W.; McKenna, T.S.; Grubman, M.J. Pathogenesis of wild-type and leaderless foot-and-mouth disease virus in cattle. J. Virol. 1996, 70, 5638–5641. [Google Scholar] [CrossRef] [PubMed]
- Carrillo, C.; Tulman, E.R.; Delhon, G.; Lu, Z.; Carreno, A.; Vagnozzi, A.; Kutish, G.F.; Rock, D.L. Comparative genomics of foot-and-mouth disease virus. J. Virol. 2005, 79, 6487–6504. [Google Scholar] [CrossRef] [PubMed]
- Gladue, D.P.; Largo, E.; de la Arada, I.; Aguilella, V.M.; Alcaraz, A.; Arrondo, J.L.R.; Holinka, L.G.; Brocchi, E.; Ramirez-Medina, E.; Vuono, E.A.; et al. Molecular Characterization of the Viroporin Function of Foot-and-Mouth Disease Virus Nonstructural Protein 2B. J. Virol. 2018, 92, 10–1128. [Google Scholar] [CrossRef]
- Ao, D.; Guo, H.C.; Sun, S.Q.; Sun, D.H.; Fung, T.S.; Wei, Y.Q.; Han, S.C.; Yao, X.P.; Cao, S.Z.; Liu, D.X.; et al. Viroporin Activity of the Foot-and-Mouth Disease Virus Non-Structural 2B Protein. PLoS ONE 2015, 10, e0125828. [Google Scholar] [CrossRef]
- Weerawardhana, A.; Uddin, M.B.; Choi, J.H.; Pathinayake, P.; Shin, S.H.; Chathuranga, K.; Park, J.H.; Lee, J.S. Foot-and-mouth disease virus non-structural protein 2B downregulates the RLR signaling pathway via degradation of RIG-I and MDA5. Front. Immunol. 2022, 13, 1020262. [Google Scholar] [CrossRef]
- Zhi, X.; Zhang, Y.; Sun, S.; Zhang, Z.; Dong, H.; Luo, X.; Wei, Y.; Lu, Z.; Dou, Y.; Wu, R.; et al. NLRP3 inflammasome activation by Foot-and-mouth disease virus infection mainly induced by viral RNA and non-structural protein 2B. RNA Biol. 2020, 17, 335–349. [Google Scholar] [CrossRef]
- Liu, H.; Zhu, Z.; Xue, Q.; Yang, F.; Cao, W.; Zhang, K.; Liu, X.; Zheng, H. Foot-and-Mouth Disease Virus Antagonizes NOD2-Mediated Antiviral Effects by Inhibiting NOD2 Protein Expression. J. Virol. 2019, 93, 10–1128. [Google Scholar] [CrossRef]
- Zhu, Z.; Li, C.; Du, X.; Wang, G.; Cao, W.; Yang, F.; Feng, H.; Zhang, X.; Shi, Z.; Liu, H.; et al. Foot-and-mouth disease virus infection inhibits LGP2 protein expression to exaggerate inflammatory response and promote viral replication. Cell Death Dis. 2017, 8, e2747. [Google Scholar] [CrossRef] [PubMed]
- Nishi, T.; Morioka, K.; Saito, N.; Yamakawa, M.; Kanno, T.; Fukai, K. Genetic Determinants of Virulence between Two Foot-and-Mouth Disease Virus Isolates Which Caused Outbreaks of Differing Severity. Msphere 2019, 4, 10–1128. [Google Scholar] [CrossRef]
- Moraes, M.P.; Segundo, F.D.; Dias, C.C.; Pena, L.; Grubman, M.J. Increased efficacy of an adenovirus-vectored foot-and-mouth disease capsid subunit vaccine expressing nonstructural protein 2B is associated with a specific T cell response. Vaccine 2011, 29, 9431–9440. [Google Scholar] [CrossRef] [PubMed]
- Moffat, K.; Howell, G.; Knox, C.; Belsham, G.J.; Monaghan, P.; Ryan, M.D.; Wileman, T. Effects of foot-and-mouth disease virus nonstructural proteins on the structure and function of the early secretory pathway: 2BC but not 3A blocks endoplasmic reticulum-to-Golgi transport. J. Virol. 2005, 79, 4382–4395. [Google Scholar] [CrossRef] [PubMed]
- Gladue, D.P.; O’Donnell, V.; Baker-Branstetter, R.; Holinka, L.G.; Pacheco, J.M.; Fernandez Sainz, I.; Lu, Z.; Ambroggio, X.; Rodriguez, L.; Borca, M.V. Foot-and-mouth disease virus modulates cellular vimentin for virus survival. J. Virol. 2013, 87, 6794–6803. [Google Scholar] [CrossRef]
- Gladue, D.P.; O’Donnell, V.; Baker-Branstetter, R.; Holinka, L.G.; Pacheco, J.M.; Fernandez-Sainz, I.; Lu, Z.; Brocchi, E.; Baxt, B.; Piccone, M.E.; et al. Foot-and-mouth disease virus nonstructural protein 2C interacts with Beclin1, modulating virus replication. J. Virol. 2012, 86, 12080–12090. [Google Scholar] [CrossRef]
- Agudo, R.; de la Higuera, I.; Arias, A.; Grande-Perez, A.; Domingo, E. Involvement of a joker mutation in a polymerase-independent lethal mutagenesis escape mechanism. Virology 2016, 494, 257–266. [Google Scholar] [CrossRef]
- Domingo, E.; Schuster, P. What Is a Quasispecies? Historical Origins and Current Scope. Curr. Top. Microbiol. Immunol. 2016, 392, 1–22. [Google Scholar] [CrossRef] [PubMed]
- Yuan, T.; Wang, H.; Li, C.; Yang, D.; Zhou, G.; Yu, L. T135I substitution in the nonstructural protein 2C enhances foot-and-mouth disease virus replication. Virus Genes 2017, 53, 840–847. [Google Scholar] [CrossRef]
- Dunn, C.S.; Donaldson, A.I. Natural adaption to pigs of a Taiwanese isolate of foot-and-mouth disease virus. Vet. Rec. 1997, 141, 174–175. [Google Scholar] [CrossRef]
- Beard, C.W.; Mason, P.W. Genetic determinants of altered virulence of Taiwanese foot-and-mouth disease virus. J. Virol. 2000, 74, 987–991. [Google Scholar] [CrossRef] [PubMed]
- Ma, X.; Ling, Y.; Li, P.; Sun, P.; Cao, Y.; Bai, X.; Li, K.; Fu, Y.; Zhang, J.; Li, D.; et al. Cellular Vimentin Interacts with Foot-and-Mouth Disease Virus Nonstructural Protein 3A and Negatively Modulates Viral Replication. J. Virol. 2020, 94, 10–1128. [Google Scholar] [CrossRef]
- Lee, H.W.; Jiang, Y.F.; Chang, H.W.; Cheng, I.C. Foot-and-Mouth Disease Virus 3A Hijacks Sar1 and Sec12 for ER Remodeling in a COPII-Independent Manner. Viruses 2022, 14, 839. [Google Scholar] [CrossRef] [PubMed]
- Pacheco, J.M.; Gladue, D.P.; Holinka, L.G.; Arzt, J.; Bishop, E.; Smoliga, G.; Pauszek, S.J.; Bracht, A.J.; O’Donnell, V.; Fernandez-Sainz, I.; et al. A partial deletion in non-structural protein 3A can attenuate foot-and-mouth disease virus in cattle. Virology 2013, 446, 260–267. [Google Scholar] [CrossRef][Green Version]
- Stenfeldt, C.; Arzt, J.; Pacheco, J.M.; Gladue, D.P.; Smoliga, G.; Silva, E.B.; Rodriguez, L.L.; Borca, M.V. A partial deletion within foot-and-mouth disease virus non-structural protein 3A causes clinical attenuation in cattle but does not prevent subclinical infection. Virology 2018, 516, 115–126. [Google Scholar] [CrossRef]
- Fu, S.Z.; Yang, W.P.; Ru, Y.; Zhang, K.S.; Wang, Y.; Liu, X.T.; Li, D.; Zheng, H.X. DDX56 cooperates with FMDV 3A to enhance FMDV replication by inhibiting the phosphorylation of IRF3. Cell. Signal. 2019, 64, 109393. [Google Scholar] [CrossRef]
- Li, D.; Lei, C.; Xu, Z.; Yang, F.; Liu, H.; Zhu, Z.; Li, S.; Liu, X.; Shu, H.; Zheng, H. Foot-and-mouth disease virus non-structural protein 3A inhibits the interferon-beta signaling pathway. Sci. Rep. 2016, 6, 21888. [Google Scholar] [CrossRef]
- Yang, W.; Li, D.; Ru, Y.; Bai, J.; Ren, J.; Zhang, J.; Li, L.; Liu, X.; Zheng, H. Foot-and-Mouth Disease Virus 3A Protein Causes Upregulation of Autophagy-Related Protein LRRC25 To Inhibit the G3BP1-Mediated RIG-Like Helicase-Signaling Pathway. J. Virol. 2020, 94, 10–1128. [Google Scholar] [CrossRef]
- Grubman, M.J.; Baxt, B. Foot-and-mouth disease. Clin. Microbiol. Rev. 2004, 17, 465–493. [Google Scholar] [CrossRef]
- Zhang, X.; Zhu, Z.; Wang, C.; Yang, F.; Cao, W.; Li, P.; Du, X.; Zhao, F.; Liu, X.; Zheng, H. Foot-and-Mouth Disease Virus 3B Protein Interacts with Pattern Recognition Receptor RIG-I to Block RIG-I-Mediated Immune Signaling and Inhibit Host Antiviral Response. J. Immunol. 2020, 205, 2207–2221. [Google Scholar] [CrossRef]
- Falk, M.M.; Sobrino, F.; Beck, E. VPg gene amplification correlates with infective particle formation in foot-and-mouth disease virus. J. Virol. 1992, 66, 2251–2260. [Google Scholar] [CrossRef] [PubMed]
- Pacheco, J.M.; Henry, T.M.; O’Donnell, V.K.; Gregory, J.B.; Mason, P.W. Role of nonstructural proteins 3A and 3B in host range and pathogenicity of foot-and-mouth disease virus. J. Virol. 2003, 77, 13017–13027. [Google Scholar] [CrossRef]
- Belsham, G.J.; McInerney, G.M.; Ross-Smith, N. Foot-and-mouth disease virus 3C protease induces cleavage of translation initiation factors eIF4A and eIF4G within infected cells. J. Virol. 2000, 74, 272–280. [Google Scholar] [CrossRef] [PubMed]
- Du, Y.; Bi, J.; Liu, J.; Liu, X.; Wu, X.; Jiang, P.; Yoo, D.; Zhang, Y.; Wu, J.; Wan, R.; et al. 3Cpro of foot-and-mouth disease virus antagonizes the interferon signaling pathway by blocking STAT1/STAT2 nuclear translocation. J. Virol. 2014, 88, 4908–4920. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Fang, L.; Li, K.; Zhong, H.; Fan, J.; Ouyang, C.; Zhang, H.; Duan, E.; Luo, R.; Zhang, Z.; et al. Foot-and-mouth disease virus 3C protease cleaves NEMO to impair innate immune signaling. J. Virol. 2012, 86, 9311–9322. [Google Scholar] [CrossRef]
- Ekanayaka, P.; Shin, S.H.; Weeratunga, P.; Lee, H.; Kim, T.H.; Chathuranga, K.; Subasinghe, A.; Park, J.H.; Lee, J.S. Foot-and-Mouth Disease Virus 3C Protease Antagonizes Interferon Signaling and C142T Substitution Attenuates the FMD Virus. Front. Microbiol. 2021, 12, 737031. [Google Scholar] [CrossRef]
- Ye, X.; Pan, T.; Wang, D.; Fang, L.; Ma, J.; Zhu, X.; Shi, Y.; Zhang, K.; Zheng, H.; Chen, H.; et al. Foot-and-Mouth Disease Virus Counteracts on Internal Ribosome Entry Site Suppression by G3BP1 and Inhibits G3BP1-Mediated Stress Granule Assembly via Post-Translational Mechanisms. Front. Immunol. 2018, 9, 1142. [Google Scholar] [CrossRef]
- Domingo, E. Mechanisms of viral emergence. Vet. Res. 2010, 41, 38. [Google Scholar] [CrossRef]
- Zeng, J.; Wang, H.; Xie, X.; Li, C.; Zhou, G.; Yang, D.; Yu, L. Ribavirin-resistant variants of foot-and-mouth disease virus: The effect of restricted quasispecies diversity on viral virulence. J. Virol. 2014, 88, 4008–4020. [Google Scholar] [CrossRef]
- Li, C.; Wang, H.; Yuan, T.; Woodman, A.; Yang, D.; Zhou, G.; Cameron, C.E.; Yu, L. Foot-and-mouth disease virus type O specific mutations determine RNA-dependent RNA polymerase fidelity and virus attenuation. Virology 2018, 518, 87–94. [Google Scholar] [CrossRef]
- Vignuzzi, M.; Wendt, E.; Andino, R. Engineering attenuated virus vaccines by controlling replication fidelity. Nat. Med. 2008, 14, 154–161. [Google Scholar] [CrossRef] [PubMed]
- Yuan, H.; Li, P.; Ma, X.; Lu, Z.; Sun, P.; Bai, X.; Zhang, J.; Bao, H.; Cao, Y.; Li, D.; et al. The pH stability of foot-and-mouth disease virus. Virol. J. 2017, 14, 233. [Google Scholar] [CrossRef] [PubMed]
- Curry, S.; Abrams, C.C.; Fry, E.; Crowther, J.C.; Belsham, G.J.; Stuart, D.I.; King, A.M. Viral RNA modulates the acid sensitivity of foot-and-mouth disease virus capsids. J. Virol. 1995, 69, 430–438. [Google Scholar] [CrossRef] [PubMed]
- Doel, T.R.; Baccarini, P.J. Thermal stability of foot-and-mouth disease virus. Arch. Virol. 1981, 70, 21–32. [Google Scholar] [CrossRef]
- Fox, G.; Parry, N.R.; Barnett, P.V.; McGinn, B.; Rowlands, D.J.; Brown, F. The cell attachment site on foot-and-mouth disease virus includes the amino acid sequence RGD (arginine-glycine-aspartic acid). J. Gen. Virol. 1989, 70 Pt 3, 625–637. [Google Scholar] [CrossRef]
- Rowlands, D.J.; Clarke, B.E.; Carroll, A.R.; Brown, F.; Nicholson, B.H.; Bittle, J.L.; Houghten, R.A.; Lerner, R.A. Chemical basis of antigenic variation in foot-and-mouth disease virus. Nature 1983, 306, 694–697. [Google Scholar] [CrossRef]
- Francis, M.J.; Hastings, G.Z.; Clarke, B.E.; Brown, A.L.; Beddell, C.R.; Rowlands, D.J.; Brown, F. Neutralizing antibodies to all seven serotypes of foot-and-mouth disease virus elicited by synthetic peptides. Immunology 1990, 69, 171–176. [Google Scholar]
- Jackson, T.; Blakemore, W.; Newman, J.W.; Knowles, N.J.; Mould, A.P.; Humphries, M.J.; King, A.M. Foot-and-mouth disease virus is a ligand for the high-affinity binding conformation of integrin alpha5beta1: Influence of the leucine residue within the RGDL motif on selectivity of integrin binding. J. Gen. Virol. 2000, 81, 1383–1391. [Google Scholar]
- Zhang, K.; Yan, M.; Hao, J.; Shen, C.; Zhu, Z.; Zhang, D.; Hou, J.; Xu, G.; Li, D.; Zheng, H.; et al. Foot-and-Mouth Disease Virus Structural Protein VP1 Destroys the Stability of TPL2 Trimer by Degradation TPL2 to Evade Host Antiviral Immunity. J. Virol. 2021, 95, 10–1128. [Google Scholar] [CrossRef]
- Li, D.; Yang, W.; Yang, F.; Liu, H.; Zhu, Z.; Lian, K.; Lei, C.; Li, S.; Liu, X.; Zheng, H.; et al. The VP3 structural protein of foot-and-mouth disease virus inhibits the IFN-beta signaling pathway. FASEB J. 2016, 30, 1757–1766. [Google Scholar] [CrossRef]
- Stenfeldt, C.; Eschbaumer, M.; Pacheco, J.M.; Rekant, S.I.; Rodriguez, L.L.; Arzt, J. Pathogenesis of Primary Foot-and-Mouth Disease Virus Infection in the Nasopharynx of Vaccinated and Non-Vaccinated Cattle. PLoS ONE 2015, 10, e0143666. [Google Scholar] [CrossRef] [PubMed]
- Stenfeldt, C.; Pacheco, J.M.; Borca, M.V.; Rodriguez, L.L.; Arzt, J. Morphologic and phenotypic characteristics of myocarditis in two pigs infected by foot-and mouth disease virus strains of serotypes O or A. Acta Vet. Scand. 2014, 56, 42. [Google Scholar] [CrossRef] [PubMed]
- Stenfeldt, C.; Eschbaumer, M.; Rekant, S.I.; Pacheco, J.M.; Smoliga, G.R.; Hartwig, E.J.; Rodriguez, L.L.; Arzt, J. The Foot-and-Mouth Disease Carrier State Divergence in Cattle. J. Virol. 2016, 90, 6344–6364. [Google Scholar] [CrossRef] [PubMed]
- Stenfeldt, C.; Pacheco, J.M.; Smoliga, G.R.; Bishop, E.; Pauszek, S.J.; Hartwig, E.J.; Rodriguez, L.L.; Arzt, J. Detection of Foot-and-mouth Disease Virus RNA and Capsid Protein in Lymphoid Tissues of Convalescent Pigs Does Not Indicate Existence of a Carrier State. Transbound. Emerg. Dis. 2016, 63, 152–164. [Google Scholar] [CrossRef] [PubMed]
- Pacheco, J.M.; Smoliga, G.R.; O’Donnell, V.; Brito, B.P.; Stenfeldt, C.; Rodriguez, L.L.; Arzt, J. Persistent Foot-and-Mouth Disease Virus Infection in the Nasopharynx of Cattle; Tissue-Specific Distribution and Local Cytokine Expression. PLoS ONE 2015, 10, e0125698. [Google Scholar] [CrossRef]
- Zhang, Z.D.; Kitching, R.P. The localization of persistent foot and mouth disease virus in the epithelial cells of the soft palate and pharynx. J. Comp. Pathol. 2001, 124, 89–94. [Google Scholar] [CrossRef]
- O’Neill, A.; Mantri, C.K.; Tan, C.W.; Saron, W.A.A.; Nagaraj, S.K.; Kala, M.P.; Joy, C.M.; Rathore, A.P.S.; Tripathi, S.; Wang, L.F.; et al. Mucosal SARS-CoV-2 vaccination of rodents elicits superior systemic T central memory function and cross-neutralising antibodies against variants of concern. EBioMedicine 2024, 99, 104924. [Google Scholar] [CrossRef]
- Windsor, M.A.; Carr, B.V.; Bankowski, B.; Gibson, D.; Reid, E.; Hamblin, P.; Gubbins, S.; Juleff, N.; Charleston, B. Cattle remain immunocompetent during the acute phase of foot-and-mouth disease virus infection. Vet. Res. 2011, 42, 108. [Google Scholar] [CrossRef]
- Arzt, J.; Pacheco, J.M.; Smoliga, G.R.; Tucker, M.T.; Bishop, E.; Pauszek, S.J.; Hartwig, E.J.; de los Santos, T.; Rodriguez, L.L. Foot-and-mouth disease virus virulence in cattle is co-determined by viral replication dynamics and route of infection. Virology 2014, 452, 12–22. [Google Scholar] [CrossRef]
- Eschbaumer, M.; Stenfeldt, C.; Rekant, S.I.; Pacheco, J.M.; Hartwig, E.J.; Smoliga, G.R.; Kenney, M.A.; Golde, W.T.; Rodriguez, L.L.; Arzt, J. Systemic immune response and virus persistence after foot-and-mouth disease virus infection of naive cattle and cattle vaccinated with a homologous adenovirus-vectored vaccine. BMC Vet. Res. 2016, 12, 205. [Google Scholar] [CrossRef]
- Stenfeldt, C.; Heegaard, P.M.; Stockmarr, A.; Tjornehoj, K.; Belsham, G.J. Analysis of the acute phase responses of serum amyloid a, haptoglobin and type 1 interferon in cattle experimentally infected with foot-and-mouth disease virus serotype O. Vet. Res. 2011, 42, 66. [Google Scholar] [CrossRef] [PubMed]
- Reid, E.; Juleff, N.; Gubbins, S.; Prentice, H.; Seago, J.; Charleston, B. Bovine plasmacytoid dendritic cells are the major source of type I interferon in response to foot-and-mouth disease virus in vitro and in vivo. J. Virol. 2011, 85, 4297–4308. [Google Scholar] [CrossRef] [PubMed]
- Perez-Martin, E.; Weiss, M.; Diaz-San Segundo, F.; Pacheco, J.M.; Arzt, J.; Grubman, M.J.; de los Santos, T. Bovine type III interferon significantly delays and reduces the severity of foot-and-mouth disease in cattle. J. Virol. 2012, 86, 4477–4487. [Google Scholar] [CrossRef]
- Diaz-San Segundo, F.; Moraes, M.P.; de Los Santos, T.; Dias, C.C.; Grubman, M.J. Interferon-induced protection against foot-and-mouth disease virus infection correlates with enhanced tissue-specific innate immune cell infiltration and interferon-stimulated gene expression. J. Virol. 2010, 84, 2063–2077. [Google Scholar] [CrossRef]
- Nfon, C.K.; Toka, F.N.; Kenney, M.; Pacheco, J.M.; Golde, W.T. Loss of plasmacytoid dendritic cell function coincides with lymphopenia and viremia during foot-and-mouth disease virus infection. Viral Immunol. 2010, 23, 29–41. [Google Scholar] [CrossRef]
- Summerfield, A. Viewpoint: Factors involved in type I interferon responses during porcine virus infections. Vet. Immunol. Immunopathol. 2012, 148, 168–171. [Google Scholar] [CrossRef]
- Diaz-San Segundo, F.; Montiel, N.; de Los Santos, T.; Grubman, M.J. Understanding the Mechanisms of Interferon-Induced Protection against Foot-and-Mouth Disease. In Virology II-Advanced Issues; iConcept Press: Hong Kong, China, 2013. [Google Scholar]
- Sei, J.J.; Waters, R.A.; Kenney, M.; Barlow, J.W.; Golde, W.T. Effect of Foot-and-Mouth Disease Virus Infection on the Frequency, Phenotype and Function of Circulating Dendritic Cells in Cattle. PLoS ONE 2016, 11, e0152192. [Google Scholar] [CrossRef]
- Medina, G.N.; de Los Santos, T.; Diaz-San Segundo, F. Use of IFN-Based Biotherapeutics to Harness the Host Against Foot-And-Mouth Disease. Front. Vet. Sci. 2020, 7, 465. [Google Scholar] [CrossRef] [PubMed]
- Rigden, R.C.; Carrasco, C.P.; Summerfield, A.; KC, M.C. Macrophage phagocytosis of foot-and-mouth disease virus may create infectious carriers. Immunology 2002, 106, 537–548. [Google Scholar] [CrossRef]
- Toka, F.N.; Nfon, C.K.; Dawson, H.; Estes, D.M.; Golde, W.T. Activation of porcine natural killer cells and lysis of foot-and-mouth disease virus infected cells. J. Interferon Cytokine Res. 2009, 29, 179–192. [Google Scholar] [CrossRef]
- McCullough, K.C.; Parkinson, D.; Crowther, J.R. Opsonization-enhanced phagocytosis of foot-and-mouth disease virus. Immunology 1988, 65, 187–191. [Google Scholar] [PubMed]
- Guzylack-Piriou, L.; Bergamin, F.; Gerber, M.; McCullough, K.C.; Summerfield, A. Plasmacytoid dendritic cell activation by foot-and-mouth disease virus requires immune complexes. Eur. J. Immunol. 2006, 36, 1674–1683. [Google Scholar] [CrossRef] [PubMed]
- Toka, F.N.; Nfon, C.; Dawson, H.; Golde, W.T. Natural killer cell dysfunction during acute infection with foot-and-mouth disease virus. Clin. Vaccine Immunol. 2009, 16, 1738–1749. [Google Scholar] [CrossRef] [PubMed]
- Patch, J.R.; Dar, P.A.; Waters, R.; Toka, F.N.; Barrera, J.; Schutta, C.; Kondabattula, G.; Golde, W.T. Infection with foot-and-mouth disease virus (FMDV) induces a natural killer (NK) cell response in cattle that is lacking following vaccination. Comp. Immunol. Microbiol. Infect. Dis. 2014, 37, 249–257. [Google Scholar] [CrossRef] [PubMed]
- Tandel, N.; Negi, S.; Dalai, S.K.; Tyagi, R.K. Role of natural killer and B cell interaction in inducing pathogen specific immune responses. Int. Rev. Immunol. 2023, 42, 304–322. [Google Scholar] [CrossRef]
- Notario, L.; Redondo-Anton, J.; Alari-Pahissa, E.; Albentosa, A.; Leiva, M.; Lopez, D.; Sabio, G.; Lauzurica, P. CD69 Targeting Enhances Anti-vaccinia Virus Immunity. J. Virol. 2019, 93, 10–1128. [Google Scholar] [CrossRef]
- Zanna, M.Y.; Yasmin, A.R.; Omar, A.R.; Arshad, S.S.; Mariatulqabtiah, A.R.; Nur-Fazila, S.H.; Mahiza, M.I.N. Review of Dendritic Cells, Their Role in Clinical Immunology, and Distribution in Various Animal Species. Int. J. Mol. Sci. 2021, 22, 8044. [Google Scholar] [CrossRef]
- Diaz-San Segundo, F.; Rodriguez-Calvo, T.; de Avila, A.; Sevilla, N. Immunosuppression during acute infection with foot-and-mouth disease virus in swine is mediated by IL-10. PLoS ONE 2009, 4, e5659. [Google Scholar] [CrossRef]
- Sei, J.J.; Ochoa, A.S.; Bishop, E.; Barlow, J.W.; Golde, W.T. Phenotypic, ultra-structural, and functional characterization of bovine peripheral blood dendritic cell subsets. PLoS ONE 2014, 9, e109273. [Google Scholar] [CrossRef]
- Nfon, C.K.; Ferman, G.S.; Toka, F.N.; Gregg, D.A.; Golde, W.T. Interferon-alpha production by swine dendritic cells is inhibited during acute infection with foot-and-mouth disease virus. Viral Immunol. 2008, 21, 68–77. [Google Scholar] [CrossRef]
- Bautista, E.M.; Ferman, G.S.; Gregg, D.; Brum, M.C.; Grubman, M.J.; Golde, W.T. Constitutive expression of alpha interferon by skin dendritic cells confers resistance to infection by foot-and-mouth disease virus. J. Virol. 2005, 79, 4838–4847. [Google Scholar] [CrossRef] [PubMed]
- Matsui, T.; Akahoshi, T.; Namai, R.; Hashimoto, A.; Kurihara, Y.; Rana, M.; Nishimura, A.; Endo, H.; Kitasato, H.; Kawai, S.; et al. Selective recruitment of CCR6-expressing cells by increased production of MIP-3 alpha in rheumatoid arthritis. Clin. Exp. Immunol. 2001, 125, 155–161. [Google Scholar] [CrossRef] [PubMed]
- Sumida, S.M.; McKay, P.F.; Truitt, D.M.; Kishko, M.G.; Arthur, J.C.; Seaman, M.S.; Jackson, S.S.; Gorgone, D.A.; Lifton, M.A.; Letvin, N.L.; et al. Recruitment and expansion of dendritic cells in vivo potentiate the immunogenicity of plasmid DNA vaccines. J. Clin. Investig. 2004, 114, 1334–1342. [Google Scholar] [CrossRef]
- Heesters, B.A.; Myers, R.C.; Carroll, M.C. Follicular dendritic cells: Dynamic antigen libraries. Nat. Rev. Immunol. 2014, 14, 495–504. [Google Scholar] [CrossRef]
- Juleff, N.; Windsor, M.; Reid, E.; Seago, J.; Zhang, Z.; Monaghan, P.; Morrison, I.W.; Charleston, B. Foot-and-mouth disease virus persists in the light zone of germinal centres. PLoS ONE 2008, 3, e3434. [Google Scholar] [CrossRef]
- Gordon, L.; Mabbott, N.; Wells, J.; Kulik, L.; Juleff, N.; Charleston, B.; Perez-Martin, E. Foot-and-mouth disease virus localisation on follicular dendritic cells and sustained induction of neutralising antibodies is dependent on binding to complement receptors (CR2/CR1). PLoS Pathog. 2022, 18, e1009942. [Google Scholar] [CrossRef]
- Salguero, F.J.; Sanchez-Martin, M.A.; Diaz-San Segundo, F.; de Avila, A.; Sevilla, N. Foot-and-mouth disease virus (FMDV) causes an acute disease that can be lethal for adult laboratory mice. Virology 2005, 332, 384–396. [Google Scholar] [CrossRef]
- Sebastian, R.; Sravanthi, M.; Umapathi, V.; Krishnaswamy, N.; Priyanka, M.; Dechamma, H.J.; Ganesh, K.; Basagoudanavar, S.H.; Sanyal, A.; Reddy, G.R. Foot and mouth disease virus undergoes non-progressive replication in mice peritoneal macrophages and induces M1 polarization. Virus Res. 2020, 281, 197906. [Google Scholar] [CrossRef] [PubMed]
- Quattrocchi, V.; Langellotti, C.; Pappalardo, J.S.; Olivera, V.; Di Giacomo, S.; van Rooijen, N.; Mongini, C.; Waldner, C.; Zamorano, P.I. Role of macrophages in early protective immune responses induced by two vaccines against foot and mouth disease. Antivir. Res. 2011, 92, 262–270. [Google Scholar] [CrossRef]
- Robinson, L.; Knight-Jones, T.J.; Charleston, B.; Rodriguez, L.L.; Gay, C.G.; Sumption, K.J.; Vosloo, W. Global Foot-and-Mouth Disease Research Update and Gap Analysis: 6-Immunology. Transbound. Emerg. Dis. 2016, 63 (Suppl. S1), 56–62. [Google Scholar] [CrossRef]
- Collen, T.; Pullen, L.; Doel, T.R. T cell-dependent induction of antibody against foot-and-mouth disease virus in a mouse model. J. Gen. Virol. 1989, 70 Pt 2, 395–403. [Google Scholar] [CrossRef] [PubMed]
- Juleff, N.; Windsor, M.; Lefevre, E.A.; Gubbins, S.; Hamblin, P.; Reid, E.; McLaughlin, K.; Beverley, P.C.; Morrison, I.W.; Charleston, B. Foot-and-mouth disease virus can induce a specific and rapid CD4+ T-cell-independent neutralizing and isotype class-switched antibody response in naive cattle. J. Virol. 2009, 83, 3626–3636. [Google Scholar] [CrossRef] [PubMed]
- Pacheco, J.M.; Arzt, J.; Rodriguez, L.L. Early events in the pathogenesis of foot-and-mouth disease in cattle after controlled aerosol exposure. Vet. J. 2010, 183, 46–53. [Google Scholar] [CrossRef]
- Pega, J.; Bucafusco, D.; Di Giacomo, S.; Schammas, J.M.; Malacari, D.; Capozzo, A.V.; Arzt, J.; Perez-Beascoechea, C.; Maradei, E.; Rodriguez, L.L.; et al. Early adaptive immune responses in the respiratory tract of foot-and-mouth disease virus-infected cattle. J. Virol. 2013, 87, 2489–2495. [Google Scholar] [CrossRef]
- Acosta-Rodriguez, E.V.; Craxton, A.; Hendricks, D.W.; Merino, M.C.; Montes, C.L.; Clark, E.A.; Gruppi, A. BAFF and LPS cooperate to induce B cells to become susceptible to CD95/Fas-mediated cell death. Eur. J. Immunol. 2007, 37, 990–1000. [Google Scholar] [CrossRef] [PubMed]
- Bossen, C.; Schneider, P. BAFF, APRIL and their receptors: Structure, function and signaling. Semin. Immunol. 2006, 18, 263–275. [Google Scholar] [CrossRef]
- Elgueta, R.; Benson, M.J.; de Vries, V.C.; Wasiuk, A.; Guo, Y.; Noelle, R.J. Molecular mechanism and function of CD40/CD40L engagement in the immune system. Immunol. Rev. 2009, 229, 152–172. [Google Scholar] [CrossRef]
- Chen, T.H.; Hong, J.Y.; Liu, C.C.; Chen, C.C.; Jan, J.T.; Wu, S.C. Production of Multi-Subtype Influenza Virus-Like Particles by Molecular Fusion with BAFF or APRIL for Vaccine Development. Methods Mol. Biol. 2021, 2248, 139–153. [Google Scholar] [CrossRef]
- Liu, J.; Clayton, K.; Gao, W.; Li, Y.; Zealey, C.; Budylowski, P.; Schwartz, J.; Yue, F.Y.; Bie, Y.; Rini, J.; et al. Trimeric HIV-1 gp140 fused with APRIL, BAFF, and CD40L on the mucosal gp140-specific antibody responses in mice. Vaccine 2020, 38, 2149–2159. [Google Scholar] [CrossRef]
- Cao, J.; Wang, X.; Du, Y.; Li, Y.; Wang, X.; Jiang, P. CD40 ligand expressed in adenovirus can improve the immunogenicity of the GP3 and GP5 of porcine reproductive and respiratory syndrome virus in swine. Vaccine 2010, 28, 7514–7522. [Google Scholar] [CrossRef]
- Diaz-San Segundo, F.; Salguero, F.J.; de Avila, A.; de Marco, M.M.; Sanchez-Martin, M.A.; Sevilla, N. Selective lymphocyte depletion during the early stage of the immune response to foot-and-mouth disease virus infection in swine. J. Virol. 2006, 80, 2369–2379. [Google Scholar] [CrossRef] [PubMed]
- Joshi, G.; Sharma, R.; Kakker, N.K. Phenotypic and functional characterization of T-cells and in vitro replication of FMDV serotypes in bovine lymphocytes. Vaccine 2009, 27, 6656–6661. [Google Scholar] [CrossRef] [PubMed]
- Guo, Z.; Zhao, Y.; Zhang, Z.; Li, Y. Interleukin-10-Mediated Lymphopenia Caused by Acute Infection with Foot-and-Mouth Disease Virus in Mice. Viruses 2021, 13, 2358. [Google Scholar] [CrossRef]
- Collins, R.A.; Werling, D.; Duggan, S.E.; Bland, A.P.; Parsons, K.R.; Howard, C.J. Gammadelta T cells present antigen to CD4+ alphabeta T cells. J. Leukoc. Biol. 1998, 63, 707–714. [Google Scholar] [CrossRef]
- Blanco, E.; Garcia-Briones, M.; Sanz-Parra, A.; Gomes, P.; De Oliveira, E.; Valero, M.L.; Andreu, D.; Ley, V.; Sobrino, F. Identification of T-cell epitopes in nonstructural proteins of foot-and-mouth disease virus. J. Virol. 2001, 75, 3164–3174. [Google Scholar] [CrossRef]
- Garcia-Briones, M.; Rosas, M.F.; Gonzalez-Magaldi, M.; Martin-Acebes, M.A.; Sobrino, F.; Armas-Portela, R. Differential distribution of non-structural proteins of foot-and-mouth disease virus in BHK-21 cells. Virology 2006, 349, 409–421. [Google Scholar] [CrossRef] [PubMed]
- Brito, B.P.; Rodriguez, L.L.; Hammond, J.M.; Pinto, J.; Perez, A.M. Review of the Global Distribution of Foot-and-Mouth Disease Virus from 2007 to 2014. Transbound. Emerg. Dis. 2015. [Google Scholar] [CrossRef]
- PANAFTOSA-OPS/OMS. Programa Hermisférico de Erradicación de la Fiebre Aftosa-Plan de Acción 2011–2020; Centro Panamericano de Fiebre Aftosa-OPS/OMS: Rio de Janeiro, Brazil, 2011; p. 52. [Google Scholar]
- Belsham, G.J. Towards improvements in foot-and-mouth disease vaccine performance. Acta Vet. Scand. 2020, 62, 20. [Google Scholar] [CrossRef]
- Doel, T.R. FMD vaccines. Virus Res. 2003, 91, 81–99. [Google Scholar] [CrossRef]
- World Organization of Animal Health. Manual of Diagnostic Tests and Vaccines for Terrestrial Animals. In 3.1.8 Foot-and-Mouth Disease. 2018. Available online: https://www.woah.org/en/what-we-do/standards/codes-and-manuals/terrestrial-manual-online-access/ (accessed on 20 August 2024).
- Cox, S.J.; Voyce, C.; Parida, S.; Reid, S.M.; Hamblin, P.A.; Hutchings, G.; Paton, D.J.; Barnett, P.V. Effect of emergency FMD vaccine antigen payload on protection, sub-clinical infection and persistence following direct contact challenge of cattle. Vaccine 2006, 24, 3184–3190. [Google Scholar] [CrossRef]
- Cao, Y.; Lu, Z.; Liu, Z. Foot-and-mouth disease vaccines: Progress and problems. Expert Rev. Vaccines 2016, 15, 783–789. [Google Scholar] [CrossRef] [PubMed]
- Cox, S.J.; Barnett, P.V. Experimental evaluation of foot-and-mouth disease vaccines for emergency use in ruminants and pigs: A review. Vet. Res. 2009, 40, 13. [Google Scholar] [CrossRef] [PubMed]
- Golde, W.T.; Pacheco, J.M.; Duque, H.; Doel, T.; Penfold, B.; Ferman, G.S.; Gregg, D.R.; Rodriguez, L.L. Vaccination against foot-and-mouth disease virus confers complete clinical protection in 7 days and partial protection in 4 days: Use in emergency outbreak response. Vaccine 2005, 23, 5775–5782. [Google Scholar] [CrossRef] [PubMed]
- LaRocco, M.; Krug, P.W.; Kramer, E.; Ahmed, Z.; Pacheco, J.M.; Duque, H.; Baxt, B.; Rodriguez, L.L. A continuous bovine kidney cell line constitutively expressing bovine alphavbeta6 integrin has increased susceptibility to foot-and-mouth disease virus. J. Clin. Microbiol. 2013, 51, 1714–1720. [Google Scholar] [CrossRef]
- Bucafusco, D.; Di Giacomo, S.; Pega, J.; Schammas, J.M.; Cardoso, N.; Capozzo, A.V.; Perez-Filgueira, M. Foot-and-mouth disease vaccination induces cross-reactive IFN-gamma responses in cattle that are dependent on the integrity of the 140S particles. Virology 2015, 476, 11–18. [Google Scholar] [CrossRef]
- Ranjitha, H.B.; Dhanesh, V.V.; Hosamani, M.; Sreenivasa, B.P.; Jabeen, U.; Biswal, J.K.; Saravanan, P.; Sanyal, A.; Bhanuprakash, V.; Basagoudanavar, S.H. Thermostable negative-marker foot-and-mouth disease virus serotype O induces protective immunity in guinea pigs. Appl. Microbiol. Biotechnol. 2023, 107, 1285–1297. [Google Scholar] [CrossRef]
- Harmsen, M.M.; Fijten, H.P.; Westra, D.F.; Dekker, A. Stabilizing effects of excipients on dissociation of intact (146S) foot-and-mouth disease virions into 12S particles during storage as oil-emulsion vaccine. Vaccine 2015, 33, 2477–2484. [Google Scholar] [CrossRef]
- Li, J.; Chang, Y.; Yang, S.; Zhou, G.; Wei, Y. Formulation enhanced the stability of Foot-and-mouth virus and prolonged vaccine storage. Virol. J. 2022, 19, 207. [Google Scholar] [CrossRef] [PubMed]
- Paton, D.J.; Reeve, R.; Capozzo, A.V.; Ludi, A. Estimating the protection afforded by foot-and-mouth disease vaccines in the laboratory. Vaccine 2019, 37, 5515–5524. [Google Scholar] [CrossRef]
- Willems, T.; De Vleeschauwer, A.; Perez-Filgueira, M.; Li, Y.; Ludi, A.; Lefebvre, D.; Wilsden, G.; Statham, B.; Haas, B.; Mattion, N.; et al. FMD vaccine matching: Inter laboratory study for improved understanding of r(1) values. J. Virol. Methods 2020, 276, 113786. [Google Scholar] [CrossRef]
- Gubbins, S.; Paton, D.J.; Dekker, A.; Ludi, A.B.; Wilsden, G.; Browning, C.F.J.; Eschbaumer, M.; Barnabei, J.; Duque, H.; Pauszek, L.L.; et al. Predicting cross-protection against foot-and-mouth disease virus strains by serology after vaccination. Front. Vet. Sci. 2022, 9, 1027006. [Google Scholar] [CrossRef] [PubMed]
- Childs, K.; Jackson, B.; Harvey, Y.; Seago, J. Trans-Encapsidation of Foot-and-Mouth Disease Virus Genomes Facilitates Escape from Neutralizing Antibodies. Viruses 2022, 14, 1161. [Google Scholar] [CrossRef] [PubMed]
- Malirat, V.; Caldevilla, C.; Cardillo, S.; Espinoza, A.M.; Novo, S.G.; Taffarel, A.; Benito, M.B.; Bergmann, I.E. Broad immunogenic spectrum of monovalent and trivalent foot-and-mouth disease virus vaccines containing O(1) campos, A24 cruzeiro and A Argentina 2001 strains against circulating viral lineages in cattle and pigs. Vaccine 2023, 41, 5782–5790. [Google Scholar] [CrossRef]
- Kim, J.; Lee, S.H.; Kim, H.H.; Park, J.H.; Park, C.K. Heterologous Prime-Boost Vaccination with Commercial FMD Vaccines Elicits a Broader Immune Response than Homologous Prime-Boost Vaccination in Pigs. Vaccines 2023, 11, 551. [Google Scholar] [CrossRef]
- Di Giacomo, S.; Bucafusco, D.; Schammas, J.M.; Pega, J.; Miraglia, M.C.; Barrionuevo, F.; Capozzo, A.V.; Perez-Filgueira, D.M. Assessment on Different Vaccine Formulation Parameters in the Protection against Heterologous Challenge with FMDV in Cattle. Viruses 2022, 14, 1781. [Google Scholar] [CrossRef]
- Lavoria, M.A.; Di-Giacomo, S.; Bucafusco, D.; Franco-Mahecha, O.L.; Perez-Filgueira, D.M.; Capozzo, A.V. Avidity and subtyping of specific antibodies applied to the indirect assessment of heterologous protection against Foot-and-Mouth Disease Virus in cattle. Vaccine 2012, 30, 6845–6850. [Google Scholar] [CrossRef] [PubMed]
- Mansilla, F.C.; Turco, C.S.; Miraglia, M.C.; Bessone, F.A.; Franco, R.; Perez-Filgueira, M.; Sala, J.M.; Capozzo, A.V. The role of viral particle integrity in the serological assessment of foot-and-mouth disease virus vaccine-induced immunity in swine. PLoS ONE 2020, 15, e0232782. [Google Scholar] [CrossRef]
- Maree, F.F.; Nsamba, P.; Mutowembwa, P.; Rotherham, L.S.; Esterhuysen, J.; Scott, K. Intra-serotype SAT2 chimeric foot-and-mouth disease vaccine protects cattle against FMDV challenge. Vaccine 2015, 33, 2909–2916. [Google Scholar] [CrossRef]
- Fischer, W.; Perkins, S.; Theiler, J.; Bhattacharya, T.; Yusim, K.; Funkhouser, R.; Kuiken, C.; Haynes, B.; Letvin, N.L.; Walker, B.D.; et al. Polyvalent vaccines for optimal coverage of potential T-cell epitopes in global HIV-1 variants. Nat. Med. 2007, 13, 100–106. [Google Scholar] [CrossRef]
- Wubshet, A.K.; Werid, G.M.; Teklue, T.; Zhou, L.; Bayasgalan, C.; Tserendorj, A.; Liu, J.; Heath, L.; Sun, Y.; Ding, Y.; et al. Foot and mouth disease vaccine efficacy in Africa: A systematic review and meta-analysis. Front. Vet. Sci. 2024, 11, 1360256. [Google Scholar] [CrossRef]
- Cao, Y. Adjuvants for foot-and-mouth disease virus vaccines: Recent progress. Expert Rev. Vaccines 2014, 13, 1377–1385. [Google Scholar] [CrossRef]
- Quattrocchi, V.; Pappalardo, J.S.; Langellotti, C.; Smitsaart, E.; Fondevila, N.; Zamorano, P. Early protection against foot-and-mouth disease virus in cattle using an inactivated vaccine formulated with Montanide ESSAI IMS D 12802 VG PR adjuvant. Vaccine 2014, 32, 2167–2172. [Google Scholar] [CrossRef] [PubMed]
- Ahn, Y.H.; Chathuranga, W.A.G.; Shim, Y.J.; Haluwana, D.K.; Kim, E.H.; Yoon, I.J.; Lim, Y.T.; Shin, S.H.; Jo, H.; Hwang, S.Y.; et al. The Potential Adjuvanticity of CAvant((R))SOE for Foot-and-Mouth Disease Vaccine. Vaccines 2021, 9, 1091. [Google Scholar] [CrossRef]
- Rodriguez-Pulido, M.; Polo, M.; Borrego, B.; Saiz, M. Use of Foot-and-Mouth Disease Virus Non-coding Synthetic RNAs as Vaccine Adjuvants. Methods Mol. Biol. 2022, 2465, 125–135. [Google Scholar] [CrossRef]
- Wang, D.; Yang, Y.; Li, J.; Wang, B.; Zhang, A. Enhancing immune responses to inactivated foot-and-mouth virus vaccine by a polysaccharide adjuvant of aqueous extracts from Artemisia rupestris L. J. Vet. Sci. 2021, 22, e30. [Google Scholar] [CrossRef]
- Xu, H.; Niu, Y.; Hong, W.; Liu, W.; Zuo, X.; Bao, X.; Guo, C.; Lu, Y.; Deng, B. Development of a water-in-oil-in-water adjuvant for foot-and-mouth disease vaccine based on ginseng stem-leaf saponins as an immune booster. Comp. Immunol. Microbiol. Infect. Dis. 2020, 71, 101499. [Google Scholar] [CrossRef] [PubMed]
- Lu, Z.; Yu, S.; Wang, W.; Chen, W.; Wang, X.; Wu, K.; Li, X.; Fan, S.; Ding, H.; Yi, L.; et al. Development of Foot-and-Mouth Disease Vaccines in Recent Years. Vaccines 2022, 10, 1817. [Google Scholar] [CrossRef] [PubMed]
- Quattrocchi, V.; Bidart, J.; Mignaqui, A.C.; Ruiz, V.; Ferella, A.; Langellotti, C.; Gammella, M.; Ferraris, S.; Carrillo, J.; Wigdorovitz, A.; et al. Bovine Dendritic Cell Activation, T Cell Proliferation and Antibody Responses to Foot-And-Mouth Disease, Is Similar With Inactivated Virus and Virus Like Particles. Front. Vet. Sci. 2020, 7, 594. [Google Scholar] [CrossRef]
- Fernandez-Sainz, I.; Medina, G.N.; Ramirez-Medina, E.; Koster, M.J.; Grubman, M.J.; de Los Santos, T. Adenovirus-vectored foot-and-mouth disease vaccine confers early and full protection against FMDV O1 Manisa in swine. Virology 2017, 502, 123–132. [Google Scholar] [CrossRef] [PubMed]
- de Avila Botton, S.; Brum, M.C.; Bautista, E.; Koster, M.; Weiblen, R.; Golde, W.T.; Grubman, M.J. Immunopotentiation of a foot-and-mouth disease virus subunit vaccine by interferon alpha. Vaccine 2006, 24, 3446–3456. [Google Scholar] [CrossRef] [PubMed]
- Medina, G.N.; Montiel, N.; Diaz-San Segundo, F.; Sturza, D.; Ramirez-Medina, E.; Grubman, M.J.; de Los Santos, T. Evaluation of a Fiber-Modified Adenovirus Vector Vaccine against Foot-and-Mouth Disease in Cattle. Clin. Vaccine Immunol. 2015, 23, 125–136. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Diaz-San Segundo, F.; Dias, C.C.; Moraes, M.P.; Weiss, M.; Perez-Martin, E.; Salazar, A.M.; Grubman, M.J.; de los Santos, T. Poly ICLC increases the potency of a replication-defective human adenovirus vectored foot-and-mouth disease vaccine. Virology 2014, 468, 283–292. [Google Scholar] [CrossRef] [PubMed]
- Guo, H.C.; Sun, S.Q.; Jin, Y.; Yang, S.L.; Wei, Y.Q.; Sun, D.H.; Yin, S.H.; Ma, J.W.; Liu, Z.X.; Guo, J.H.; et al. Foot-and-mouth disease virus-like particles produced by a SUMO fusion protein system in Escherichia coli induce potent protective immune responses in guinea pigs, swine and cattle. Vet. Res. 2013, 44, 48. [Google Scholar] [CrossRef]
- Zhang, J.; Ge, J.; Li, J.; Li, J.; Zhang, Y.; Shi, Y.; Sun, J.; Wang, Q.; Zhang, X.; Zhao, X. Expression of FMD virus-like particles in yeast Hansenula polymorpha and immunogenicity of combine with CpG and aluminum adjuvant. J. Vet. Sci. 2023, 24, e15. [Google Scholar] [CrossRef]
- Le, N.M.T.; So, K.K.; Chun, J.; Kim, D.H. Expression of virus-like particles (VLPs) of foot-and-mouth disease virus (FMDV) using Saccharomyces cerevisiae. Appl. Microbiol. Biotechnol. 2024, 108, 81. [Google Scholar] [CrossRef] [PubMed]
- Mignaqui, A.C.; Ferella, A.; Cass, B.; Mukankurayija, L.; L’Abbe, D.; Bisson, L.; Sanchez, C.; Scian, R.; Cardillo, S.B.; Durocher, Y.; et al. Foot-and-Mouth Disease: Optimization, Reproducibility, and Scalability of High-Yield Production of Virus-Like Particles for a Next-Generation Vaccine. Front. Vet. Sci. 2020, 7, 601. [Google Scholar] [CrossRef]
- Fuenmayor, J.; Godia, F.; Cervera, L. Production of virus-like particles for vaccines. N. Biotechnol. 2017, 39, 174–180. [Google Scholar] [CrossRef]
- Bidart, J.; Mignaqui, A.; Kornuta, C.; Lupi, G.; Gammella, M.; Soria, I.; Galarza, R.; Ferella, A.; Cardillo, S.; Langellotti, C.; et al. FMD empty capsids combined with the Immunostant Particle Adjuvant-ISPA or ISA206 induce protective immunity against foot and mouth disease virus. Virus Res. 2021, 297, 198339. [Google Scholar] [CrossRef]
- Patronov, A.; Doytchinova, I. T-cell epitope vaccine design by immunoinformatics. Open Biol. 2013, 3, 120139. [Google Scholar] [CrossRef]
- Cao, Y.; Lu, Z.; Li, Y.; Sun, P.; Li, D.; Li, P.; Bai, X.; Fu, Y.; Bao, H.; Zhou, C.; et al. Poly(I:C) combined with multi-epitope protein vaccine completely protects against virulent foot-and-mouth disease virus challenge in pigs. Antivir. Res. 2013, 97, 145–153. [Google Scholar] [CrossRef]
- Taboga, O.; Tami, C.; Carrillo, E.; Nunez, J.I.; Rodriguez, A.; Saiz, J.C.; Blanco, E.; Valero, M.L.; Roig, X.; Camarero, J.A.; et al. A large-scale evaluation of peptide vaccines against foot-and-mouth disease: Lack of solid protection in cattle and isolation of escape mutants. J. Virol. 1997, 71, 2606–2614. [Google Scholar] [CrossRef] [PubMed]
- Heshmati, L.; Rezayat, S.M.; Madani, R.; Emami, T.; Jafari, M.R.; Golchinfar, F.; Kazemi, M.; Azimi Dezfouli, S.M. Immunity Evaluation of an Experimental Designed Nanoliposomal Vaccine Containing FMDV Immunodominant Peptides. Arch. Razi Inst. 2021, 76, 1183–1190. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Zhang, N.; Li, M.; Guo, A.; Zheng, Y.; Humak, F.; Qian, P.; Tao, P. Recombinant bacteriophage T4 displaying key epitopes of the foot-and-mouth disease virus as a novel nanoparticle vaccine. Int. J. Biol. Macromol. 2024, 258, 128837. [Google Scholar] [CrossRef] [PubMed]
- Ganges, L.; Borrego, B.; Fernandez-Pacheco, P.; Revilla, C.; Fernandez-Borges, N.; Dominguez, J.; Sobrino, F.; Rodriguez, F. DNA immunization of pigs with foot-and-mouth disease virus minigenes: From partial protection to disease exacerbation. Virus Res. 2011, 157, 121–125. [Google Scholar] [CrossRef]
- Puckette, M.; Clark, B.A.; Barrera, J.; Neilan, J.G.; Rasmussen, M.V. Evaluation of DNA Vaccine Candidates against Foot-and-Mouth Disease Virus in Cattle. Vaccines 2023, 11, 386. [Google Scholar] [CrossRef]
- Nagarajan, G.; Ravikumar, P.; Ashok Kumar, C.; Reddy, G.R.; Dechamma, H.J.; Suryanarayana, V.V. Self Replicating Gene Vaccine Carrying P1-2A Gene of FMDV Serotype O and its Effects on the Immune Responses of Cattle. Indian J. Virol. 2011, 22, 50–58. [Google Scholar] [CrossRef][Green Version]
- Nanda, R.K.; Hajam, I.A.; Edao, B.M.; Ramya, K.; Rajangam, M.; Chandra Sekar, S.; Ganesh, K.; Bhanuprakash, V.; Kishore, S. Immunological evaluation of mannosylated chitosan nanoparticles based foot and mouth disease virus DNA vaccine, pVAC FMDV VP1-OmpA in guinea pigs. Biologicals 2014, 42, 153–159. [Google Scholar] [CrossRef]
- Berche, P. Life and death of smallpox. Presse Med. 2022, 51, 104117. [Google Scholar] [CrossRef] [PubMed]
- Roeder, P.; Mariner, J.; Kock, R. Rinderpest: The veterinary perspective on eradication. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2013, 368, 20120139. [Google Scholar] [CrossRef]
- Hollister, J.R.; Vagnozzi, A.; Knowles, N.J.; Rieder, E. Molecular and phylogenetic analyses of bovine rhinovirus type 2 shows it is closely related to foot-and-mouth disease virus. Virology 2008, 373, 411–425. [Google Scholar] [CrossRef]
- Atkinson, N.J.; Witteveldt, J.; Evans, D.J.; Simmonds, P. The influence of CpG and UpA dinucleotide frequencies on RNA virus replication and characterization of the innate cellular pathways underlying virus attenuation and enhanced replication. Nucleic Acids Res. 2014, 42, 4527–4545. [Google Scholar] [CrossRef] [PubMed]
- Burns, C.C.; Campagnoli, R.; Shaw, J.; Vincent, A.; Jorba, J.; Kew, O. Genetic inactivation of poliovirus infectivity by increasing the frequencies of CpG and UpA dinucleotides within and across synonymous capsid region codons. J. Virol. 2009, 83, 9957–9969. [Google Scholar] [CrossRef] [PubMed]
- Gaunt, E.; Wise, H.M.; Zhang, H.; Lee, L.N.; Atkinson, N.J.; Nicol, M.Q.; Highton, A.J.; Klenerman, P.; Beard, P.M.; Dutia, B.M.; et al. Elevation of CpG frequencies in influenza A genome attenuates pathogenicity but enhances host response to infection. eLife 2016, 5, e12735. [Google Scholar] [CrossRef] [PubMed]
- Rzymski, P.; Szuster-Ciesielska, A.; Dzieciatkowski, T.; Gwenzi, W.; Fal, A. mRNA vaccines: The future of prevention of viral infections? J. Med. Virol. 2023, 95, e28572. [Google Scholar] [CrossRef]
- Le, T.; Sun, C.; Chang, J.; Zhang, G.; Yin, X. mRNA Vaccine Development for Emerging Animal and Zoonotic Diseases. Viruses 2022, 14, 401. [Google Scholar] [CrossRef]
- Alberer, M.; Gnad-Vogt, U.; Hong, H.S.; Mehr, K.T.; Backert, L.; Finak, G.; Gottardo, R.; Bica, M.A.; Garofano, A.; Koch, S.D.; et al. Safety and immunogenicity of a mRNA rabies vaccine in healthy adults: An open-label, non-randomised, prospective, first-in-human phase 1 clinical trial. Lancet 2017, 390, 1511–1520. [Google Scholar] [CrossRef]
- Wollner, C.J.; Richner, J.M. mRNA Vaccines against Flaviviruses. Vaccines 2021, 9, 148. [Google Scholar] [CrossRef]
- Pattnaik, A.; Sahoo, B.R.; Pattnaik, A.K. Current Status of Zika Virus Vaccines: Successes and Challenges. Vaccines 2020, 8, 266. [Google Scholar] [CrossRef]
- Rodriguez-Pulido, M.; Sobrino, F.; Borrego, B.; Saiz, M. Inoculation of newborn mice with non-coding regions of foot-and-mouth disease virus RNA can induce a rapid, solid and wide-range protection against viral infection. Antivir. Res. 2011, 92, 500–504. [Google Scholar] [CrossRef]
- Newman, J.; Rowlands, D.J.; Tuthill, T.J. An Engineered Maturation Cleavage Provides a Recombinant Mimic of Foot-and-Mouth Disease Virus Capsid Assembly-Disassembly. Life 2021, 11, 500. [Google Scholar] [CrossRef]
- Semkum, P.; Kaewborisuth, C.; Thangthamniyom, N.; Theerawatanasirikul, S.; Lekcharoensuk, C.; Hansoongnern, P.; Ramasoota, P.; Lekcharoensuk, P. A Novel Plasmid DNA-Based Foot and Mouth Disease Virus Minigenome for Intracytoplasmic mRNA Production. Viruses 2021, 13, 1047. [Google Scholar] [CrossRef] [PubMed]
- Greenwood, B. The contribution of vaccination to global health: Past, present and future. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2014, 369, 20130433. [Google Scholar] [CrossRef] [PubMed]
- Moss, W.J.; Strebel, P. Biological feasibility of measles eradication. J. Infect. Dis. 2011, 204 (Suppl. S1), S47–S53. [Google Scholar] [CrossRef] [PubMed]
- Shao, J.; Liu, W.; Gao, S.; Chang, H.; Guo, H. A recombinant multi-epitope trivalent vaccine for foot-and-mouth disease virus serotype O in pigs. Virology 2024, 596, 110103. [Google Scholar] [CrossRef]
- Chathuranga, W.A.G.; Hewawaduge, C.; Nethmini, N.A.N.; Kim, T.H.; Kim, J.H.; Ahn, Y.H.; Yoon, I.J.; Yoo, S.S.; Park, J.H.; Lee, J.S. Efficacy of a Novel Multiepitope Vaccine Candidate against Foot-and-Mouth Disease Virus Serotype O and A. Vaccines 2022, 10, 2181. [Google Scholar] [CrossRef]
| Type | Strategies for Vaccine Improvement | References of Interest | Coding Region Targeted | |
|---|---|---|---|---|
| Inactivated vaccines | Current inactivated vaccines | More permissive cell lines for viral growth | LaRocco et al., 2021 [9]; Harvey et al., 2022 [10] | n/a |
| High Potency | Brehm KE et al., 2008 [11], Dekker et al., 2020 [12], S Galdo Novo [13], Fishbourne et al., 2017 [14] | n/a | ||
| Capsid stabilization | Scott et al., 2017 [15]; Dong et al., 2021 [16]; Lopez-Arguello et al., 2019 [17]; Yuan et al., 2020 [18] | P1 capsid coding region | ||
| Enhancing cross-protection by reverse genetic, chimeric, and mosaic capsid designs | Kotecha et al., 2018 [19]; Li et al., 2022 [20]; Rieder et al., personal communication [21], Li et al., 2012 [22] | P1 capsid coding region | ||
| New marked inactivated vaccines | Development of avirulent FMDV strains with DIVA (differentiation between infected and vaccinated animals) markers in different NS proteins (Lpro, 3AB) that are safer for production | Uddowla et al., 2012 [23]; Hardham et al., 2020 [24] | Lpro, 3B, and 3D | |
| Virus-like particles expressed by viral vectors | Improve safety and include DIVA capabilities, possibly decreasing costs using: | |||
| Vaccinia | Vaccinia virus to deliver FMDV empty capsids with controlled 3C expression | Steigerwald et al., 2020 [25] | P1 coding region, 3Cpro | |
| Avian poxvirus | Fowlpox virus expressing VLPs and swine IL-18 | Ma et al., 2008 [26] | P1 coding region, 2A, 3Cpro | |
| Pseudorabies | Pseudo rabies V vector expressing VLPs | Hong et al., 2007 [27] | P1 coding region, 2A, 3Cpro | |
| Alphavirus | Single-cycle self-replicating RNA Semliki Forest virus vector expressing VLPs | Gullberg et al., 2016 [28] | P1 coding region, 2A, 3Cpro | |
| Adenovirus | Replication-defective human adenovirus type 5 (Ad5) expressing VLPs | Mayr et al., 1999 [29]; Moraes et al., 2002 [30]; Pena et al., 2008 [31]; Grubman et al., 2012 [32]; Schutta et al., 2016 [33] | P1 coding region, 2A, 2B, 3Cpro | |
| Bacterial vectors | Salmonella typhimurium or Lactococus lactis expressing VLPs | Zhi et al., 2021 [34]; Liu et al., 2020 [35] | VP1 | |
| Purified virus-like particles | More safety, DIVA capabilities, lower costs, and rapid adaptability to circulating strains: | |||
| Baculovirus | Purified VLPs expressed from recombinant baculovirus | Kotecha et al., 2015 [36]; Porta et al., 2013 [37]; Ganji et al., 2018 [38] | P1 coding region, 2A, 3Cpro | |
| Bacterial | Purified VLPs expressed in E. coli, VLP-based combined vaccine | Xiao et al., 2016 [39]; Song et al., 2024 [40] | VP0, VP1, VP3 | |
| Plant | VLPs expressed in transgenic alfalfa, tomato fruits, or tobacco | Dus Santos and Wigdorovitz, 2005 [41]; Veerapen et al., 2017 [42] | P1 coding region, 2A, | |
| Mammalian cells | VLPs expressed in mammalian cell cultures | Puckette et al., 2022 [43] | P1 coding region, 2A, 3Cpro | |
| Peptide vaccines | T- and B-cell peptide epitopes | Improve safety, include DIVA capabilities, and extend shelf life by producing: | ||
| Peptides combining VP1 G-H loop epitopes with T-cell epitopes | Wang et al., 2002 [44]; Rodriguez et al., 2003 [45] | VP1-GH-loop | ||
| Dendrimeric peptides containing one T-cell epitope and four B-cell epitopes | Blanco et al., 2016 [46]; Soria et al., 2017 [47] | P1 | ||
| DNA vaccines | Improve safety and include DIVA capabilities and rapid adaptability to circulating strains by: | |||
| Electroporation | Administering DNA by electroporation | Fowler et al., 2012 [48] | P1, 2A, 3C, 3D | |
| APC targeting | Using B/T cell epitopes fused to a single chain antibody or Bcl-xL anti-apoptotic signal | Borrego et al., 2011 [49]; Gülçe İz et al., 2013 [50] | P1 | |
| Modified live-attenuated vaccines | Improve safety and immune response (more rapid and sustained) by: | |||
| Mutations on Lpro | Introducing attenuating mutations in Lpro coding sequence | Diaz-San Segundo et al., 2012 [51]; Medina et al., 2020 [52]; Azzinaro et al., 2022 [53] | Lpro | |
| Chimeric virus | Substituting FMDV coding regions with other virus proteins (chimeric FMDV/bovine rhinitis B virus) | Uddowla et al., 2013 [54] | Lpro | |
| Fidelity | Introducing point mutations in 3Dpol to alter replication fidelity | Rai et al., 2017 [55] | 3Dpol | |
| Untranslated region | Introducing mutilations targeting RNA structures in the non-translated region | Rodriguez-Pulido et al., 2009 [56]; Kloc et al., 2017 [57] | 5′ or 3′ UTR | |
| Deoptimized virus | Deoptimization of P1 or P2/P3 coding regions | Diaz-San Segundo et al., 2015 [58]; 2020 [59]; Medina et al., 2023 [60] | Genome-wide |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Medina, G.N.; Diaz San Segundo, F. Virulence and Immune Evasion Strategies of FMDV: Implications for Vaccine Design. Vaccines 2024, 12, 1071. https://doi.org/10.3390/vaccines12091071
Medina GN, Diaz San Segundo F. Virulence and Immune Evasion Strategies of FMDV: Implications for Vaccine Design. Vaccines. 2024; 12(9):1071. https://doi.org/10.3390/vaccines12091071
Chicago/Turabian StyleMedina, Gisselle N., and Fayna Diaz San Segundo. 2024. "Virulence and Immune Evasion Strategies of FMDV: Implications for Vaccine Design" Vaccines 12, no. 9: 1071. https://doi.org/10.3390/vaccines12091071
APA StyleMedina, G. N., & Diaz San Segundo, F. (2024). Virulence and Immune Evasion Strategies of FMDV: Implications for Vaccine Design. Vaccines, 12(9), 1071. https://doi.org/10.3390/vaccines12091071







