Health System Determinants of Delivery and Uptake of HPV Vaccination Services Among Involuntary Migrant Populations: A Qualitative Systematic Review
Abstract
1. Introduction
- ⮚
- Asylum seeker—a person seeking protection in a country outside of their home country but whose status is yet to be determined by the host country.
- ⮚
- Refugee—a person who is forced to leave their home country to seek international protection due to armed conflict, persecution, and/or other humanitarian crises.
- ⮚
- Internally displaced person—a person forced out of their home who moves to a different location within their home country.
- ⮚
- Unaccompanied and separated child/minor—a person aged 18 years and below who has been separated from both parents and other legal guardians.
2. Materials and Methods
3. Search Strategy
4. Eligibility Criteria
5. Screening and Study Selection
6. Data Extraction
7. Data Analysis and Synthesis
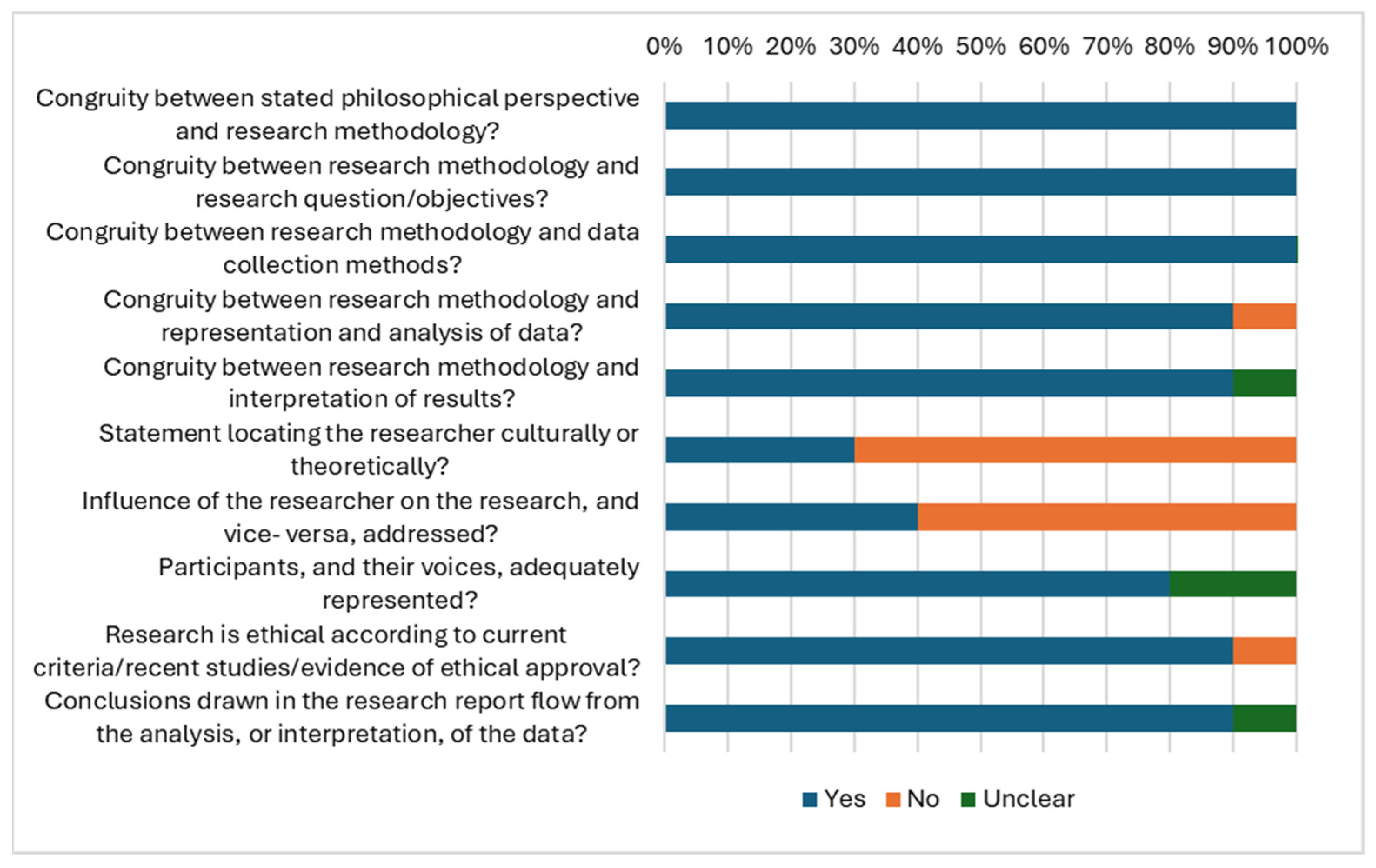
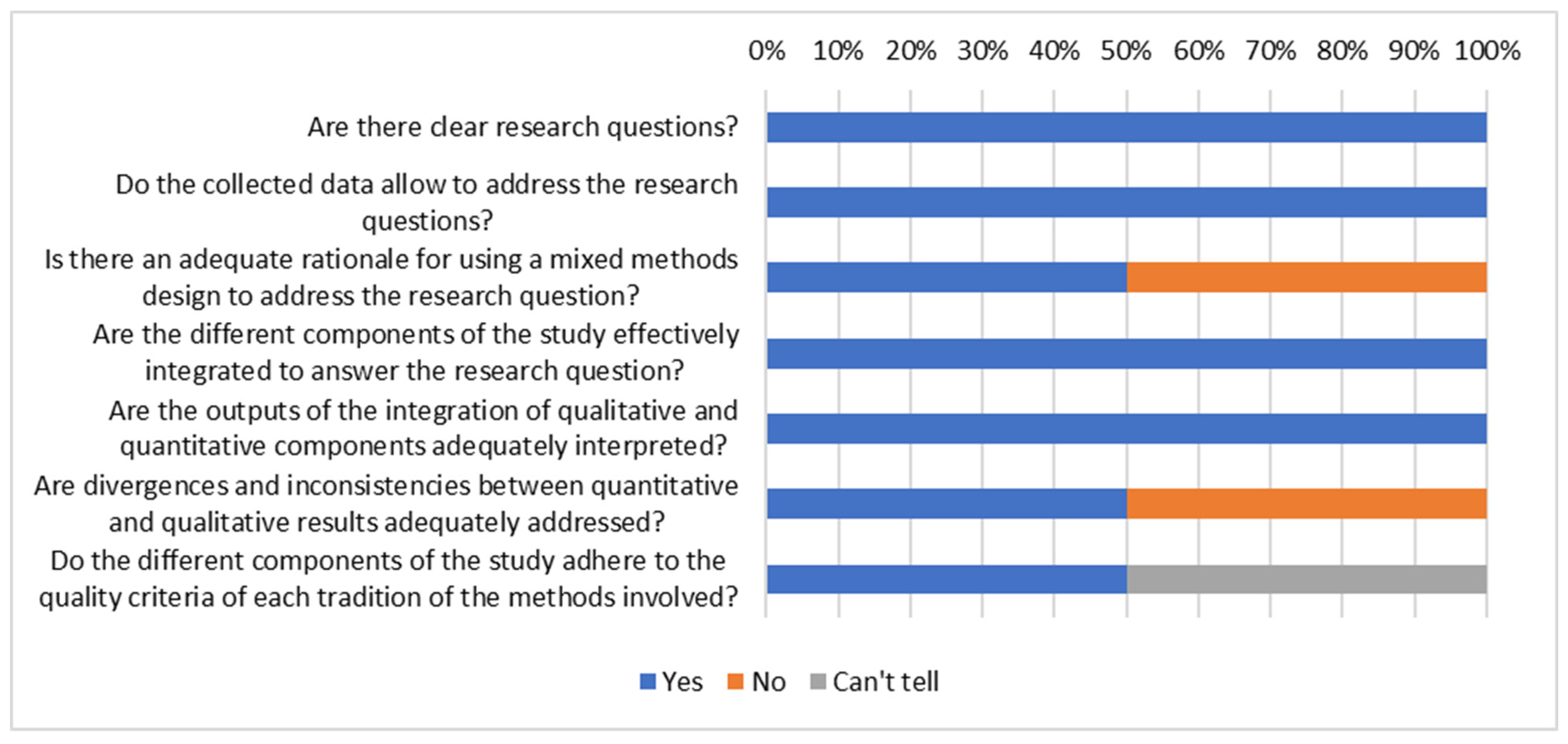
8. Quality Assessment
9. Results
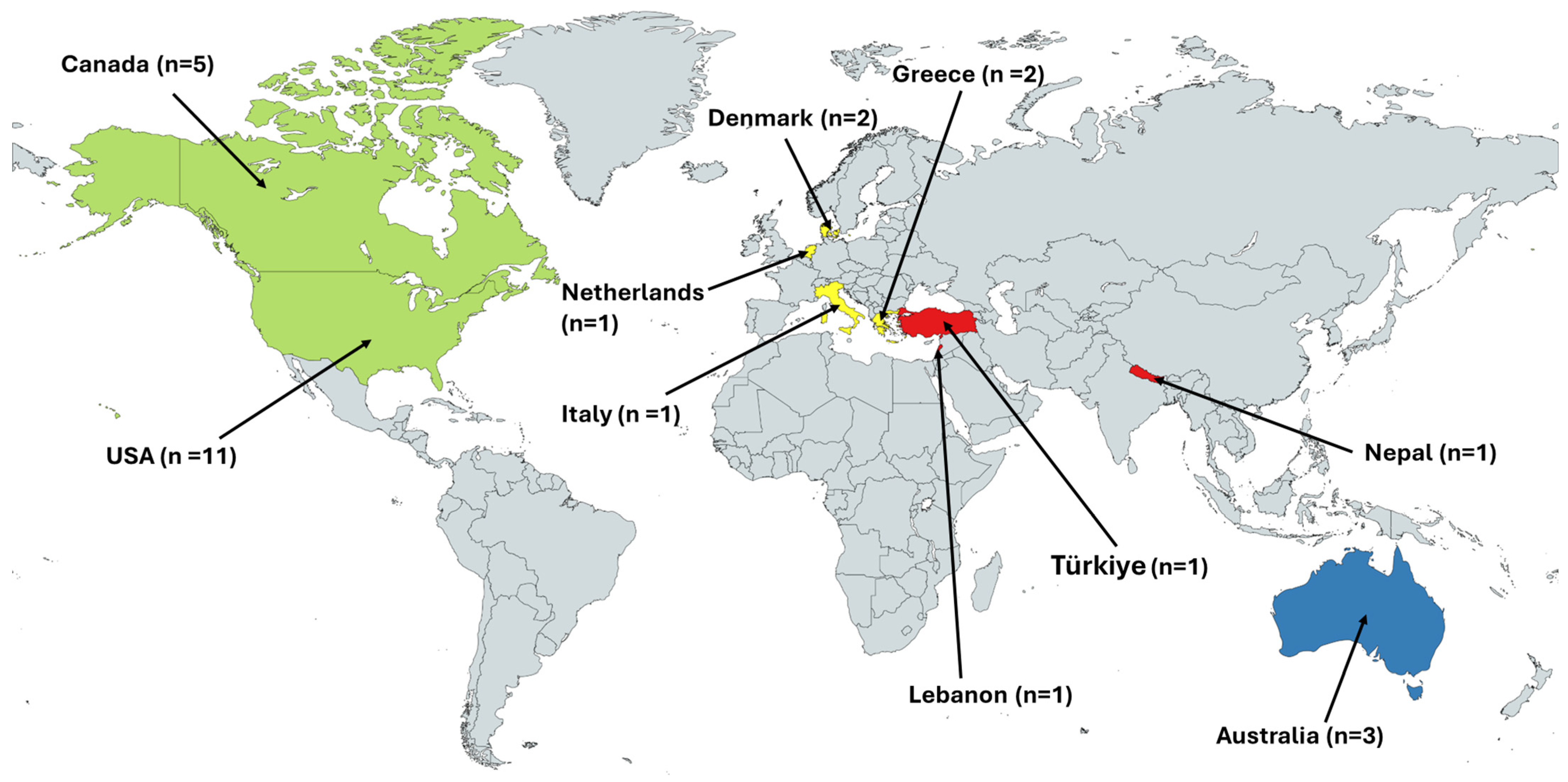
10. Descriptive Characteristics
11. Appraisal of Included Studies
12. Health System Determinants of HPV Vaccination Service Delivery
13. Health System Determinants of HPV Vaccination Uptake
14. Health System Performance Indicators and Reported Considerations for Migrant-Inclusive HPV Vaccination Services
15. Discussion
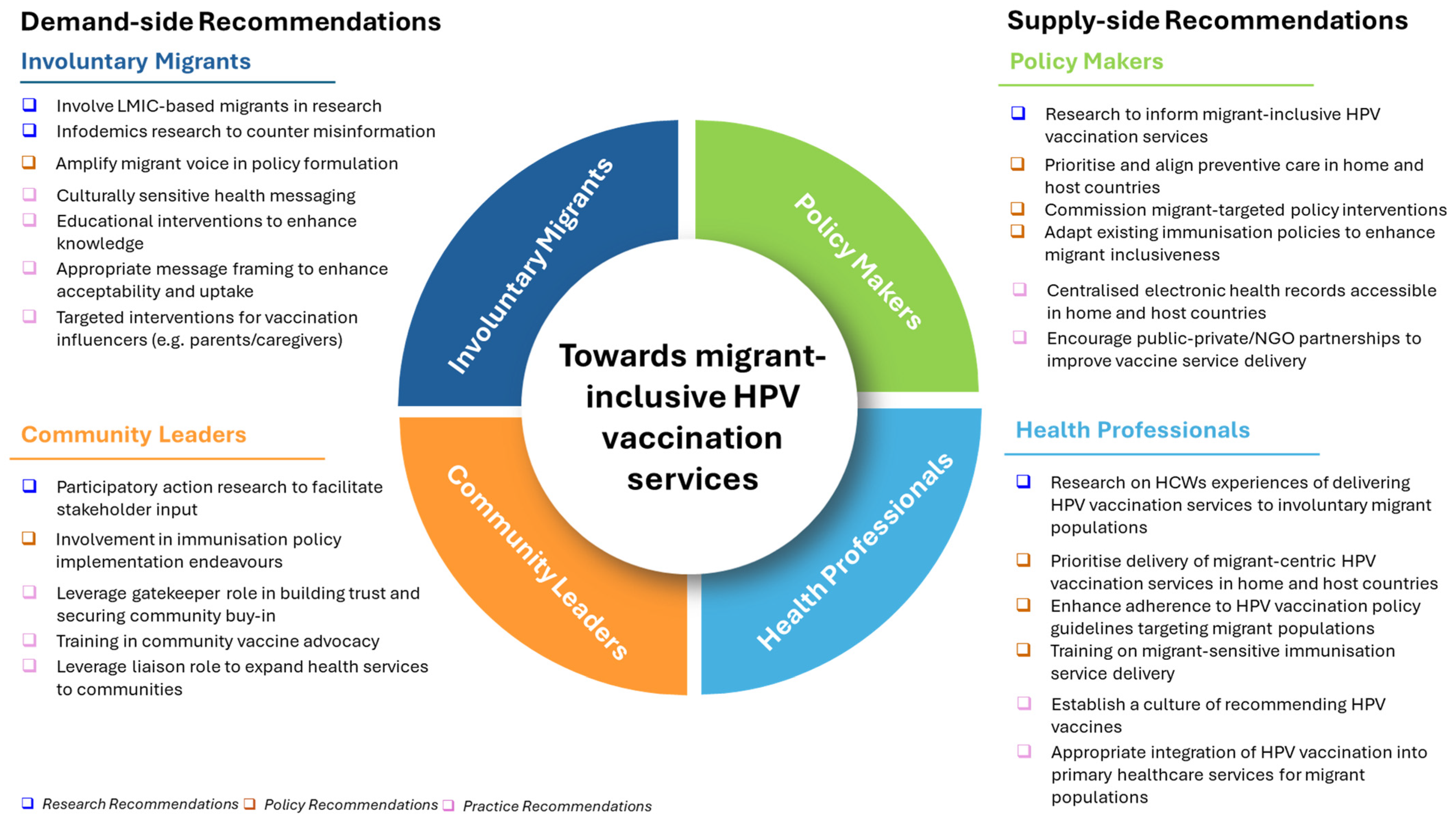
16. Recommendations
17. Limitations
18. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| HPV | Human Papillomavirus |
| LMICs | Low-and-Middle-Income Countries |
| HICs | High-Income Countries |
| WHO | World Health Organization |
| NIPs | National Immunisation Programmes |
| USA | United States of America |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| JBI | Joanna Briggs Institute |
| RHAP | Refugee Health Assessment Program |
References
- Bray, F.; Laversanne, M.; Sung, H.; Ferlay, J.; Siegel, R.L.; Soerjomataram, I.; Jemal, A. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA A Cancer J. Clin. 2024, 74, 229–263. [Google Scholar] [CrossRef]
- Allanson, E.R.; Schmeler, K.M. Cervical cancer prevention in low-and middle-income countries. Clin. Obstet. Gynecol. 2021, 64, 501–518. [Google Scholar] [CrossRef]
- Hull, R.; Mbele, M.; Makhafola, T.; Hicks, C.; Wang, S.M.; Reis, R.M.; Mehrotra, R.; Mkhize-Kwitshana, Z.; Kibiki, G.; Bates, D.O. Cervical cancer in low and middle-income countries. Oncol. Lett. 2020, 20, 2058–2074. [Google Scholar] [CrossRef] [PubMed]
- Guida, F.; Kidman, R.; Ferlay, J.; Schüz, J.; Soerjomataram, I.; Kithaka, B.; Ginsburg, O.; Mailhot Vega, R.B.; Galukande, M.; Parham, G. Global and regional estimates of orphans attributed to maternal cancer mortality in 2020. Nat. Med. 2022, 28, 2563–2572. [Google Scholar] [CrossRef] [PubMed]
- Marques, P.; Nunes, M.; Antunes, M.d.L.; Heleno, B.; Dias, S. Factors associated with cervical cancer screening participation among migrant women in Europe: A scoping review. Int. J. Equity Health 2020, 19, 160. [Google Scholar] [CrossRef] [PubMed]
- Collatuzzo, G.; Ferrante, M.; Ippolito, A.; Di Prima, A.; Colarossi, C.; Scarpulla, S.; Boffetta, P.; Sciacca, S. Cancer in Migrants: A Population-Based Study in Italy. Cancers 2023, 15, 3103. [Google Scholar] [CrossRef]
- Leinonen, M.K.; Campbell, S.; Ursin, G.; Tropé, A.; Nygård, M. Barriers to cervical cancer screening faced by immigrants: A registry-based study of 1.4 million women in Norway. Eur. J. Public Health 2017, 27, 873–879. [Google Scholar] [CrossRef]
- De Martel, C.; Plummer, M.; Vignat, J.; Franceschi, S. Worldwide burden of cancer attributable to HPV by site, country and HPV type. Int. J. Cancer 2017, 141, 664–670. [Google Scholar] [CrossRef]
- Amponsah-Dacosta, E.; Blose, N.; Nkwinika, V.V.; Chepkurui, V. Human Papillomavirus Vaccination in South Africa: Programmatic Challenges and Opportunities for Integration With Other Adolescent Health Services? Front. Public Health 2022, 10, 799984. [Google Scholar] [CrossRef]
- World Health Organisation. WHO Recommendations for Routine Immunisation—Summary Tables; World Health Organization: Geneva, Switzerland, 2023. [Google Scholar]
- Dau, H.; Trawin, J.; Nakisige, C.; Payne, B.A.; Vidler, M.; Singer, J.; Orem, J.; Smith, L.; Ogilvie, G. The social and economic impacts of cervical cancer on women and children in low-and middle-income countries: A systematic review. Int. J. Gynecol. Obstet. 2023, 160, 751–761. [Google Scholar] [CrossRef]
- World Health Organisation. Global Strategy to Accelerate the Elimination of Cervical Cancer as a Public Health Problem; World Health Organisation: Geneva, Switzerland, 2020. [Google Scholar]
- Bruni, L.; Saura-Lázaro, A.; Montoliu, A.; Brotons, M.; Alemany, L.; Diallo, M.S.; Afsar, O.Z.; LaMontagne, D.S.; Mosina, L.; Contreras, M. HPV vaccination introduction worldwide and WHO and UNICEF estimates of national HPV immunization coverage 2010–2019. Prev. Med. 2021, 144, 106399. [Google Scholar] [CrossRef]
- Castelli, F. Drivers of migration: Why do people move? J. Travel Med. 2018, 25, tay040. [Google Scholar] [CrossRef]
- Giménez-Gómez, J.-M.; Walle, Y.M.; Zergawu, Y.Z. Trends in African migration to Europe: Drivers beyond economic motivations. J. Confl. Resolut. 2019, 63, 1797–1831. [Google Scholar] [CrossRef]
- International Organisation for Migration. International Migration Law: Glossary of Migration; International Organisation for Migration: Geneva, Switzerland, 2019. [Google Scholar]
- World Health Organisation. Ensuring the Integration of Refugees and Migrants in Immunization Policies, Planning and Service Delivery Globally; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- Babakura, B.; Nomhwange, T.; Jean Baptiste, A.E.; Dede, O.; Taiwo, L.; Abba, S.; Soyemi, M.; Idowu, A.M.; Terna Richard, M.; Braka, F.; et al. The challenges of insecurity on implementing vaccination campaign and its effect on measles elimination and control efforts: A case study of 2017/18 measles campaign in Borno state, Nigeria. Vaccine 2021, 39 (Suppl. S3), C66–C75. [Google Scholar] [CrossRef] [PubMed]
- Ngo, N.V.; Pemunta, N.V.; Muluh, N.E.; Adedze, M.; Basil, N.; Agwale, S. Armed conflict, a neglected determinant of childhood vaccination: Some children are left behind. Hum. Vaccines Immunother. 2020, 16, 1454–1463. [Google Scholar] [CrossRef] [PubMed]
- Crawshaw, A.F.; Farah, Y.; Deal, A.; Rustage, K.; Hayward, S.E.; Carter, J.; Knights, F.; Goldsmith, L.P.; Campos-Matos, I.; Wurie, F.; et al. Defining the determinants of vaccine uptake and undervaccination in migrant populations in Europe to improve routine and COVID-19 vaccine uptake: A systematic review. Lancet Infect. Dis. 2022, 22, E254–E266. [Google Scholar] [CrossRef]
- Deal, A.; Crawshaw, A.F.; Carter, J.; Knights, F.; Iwami, M.; Darwish, M.; Hossain, R.; Immordino, P.; Kaojaroen, K.; Severoni, S.; et al. Defining drivers of under-immunisation and vaccine hesitancy in refugee and migrant populations globally to support strategies to strengthen vaccine uptake for COVID-19: A rapid review. medRxiv 2023, 30, taad084. [Google Scholar] [CrossRef]
- Gorman, D.R.; Bielecki, K.; Larson, H.J.; Willocks, L.J.; Craig, J.; Pollock, K.G. Comparing vaccination hesitancy in Polish migrant parents who accept or refuse nasal flu vaccination for their children. Vaccine 2020, 38, 2795–2799. [Google Scholar] [CrossRef]
- Ganczak, M.; Bielecki, K.; Drozd-Dąbrowska, M.; Topczewska, K.; Biesiada, D.; Molas-Biesiada, A.; Dubiel, P.; Gorman, D. Vaccination concerns, beliefs and practices among Ukrainian migrants in Poland: A qualitative study. BMC Public Health 2021, 21, 93. [Google Scholar] [CrossRef]
- Fang, H.; Yang, L.; Zhang, H.; Li, C.; Wen, L.; Sun, L.; Hanson, K.; Meng, Q. Strengthening health system to improve immunization for migrants in China. Int. J. Equity Health 2017, 16, 19. [Google Scholar] [CrossRef]
- Ekezie, W.; Awwad, S.; Krauchenberg, A.; Karara, N.; Dembinski, L.; Grossman, Z.; del Torso, S.; Dornbusch, H.J.; Neves, A.; Copley, S.; et al. Access to Vaccination among Disadvantaged, Isolated and Difficult-to-Reach Communities in the WHO European Region: A Systematic Review. Vaccines 2022, 10, 1038. [Google Scholar] [CrossRef]
- Hill, D.C.; Andrade-Romo, Z.; Solari, K.; Adams, E.; Forman, L.; Grace, D.; Silva-Santisteban, A.; Perez-Brumer, A. COVID-19 vaccine equity and the right to health for displaced Venezuelans in Latin America. PLOS Glob. Public Health 2023, 3, e0001275. [Google Scholar] [CrossRef] [PubMed]
- Tankwanchi, A.S.; Bowman, B.; Garrison, M.; Larson, H.; Wiysonge, C.S. Vaccine hesitancy in migrant communities: A rapid review of latest evidence. Curr. Opin. Immunol. 2021, 71, 62–68. [Google Scholar] [CrossRef] [PubMed]
- Deal, A.; Halliday, R.; Crawshaw, A.F.; Hayward, S.E.; Burnard, A.; Rustage, K.; Carter, J.; Mehrotra, A.; Knights, F.; Campos-Matos, I. Migration and outbreaks of vaccine-preventable disease in Europe: A systematic review. Lancet Infect. Dis. 2021, 21, e387–e398. [Google Scholar] [CrossRef] [PubMed]
- UNHCR. Global Trends: Forced Displacement in 2022; United Nations High Commissioner for Refugees: Copenhagen, Denmark, 2023. [Google Scholar]
- Sheikh, K.; Gilson, L.; Agyepong, I.A.; Hanson, K.; Ssengooba, F.; Bennett, S. Building the field of health policy and systems research: Framing the questions. PLoS Med. 2011, 8, e1001073. [Google Scholar] [CrossRef]
- Oxford Textbook of Global Public Health, 7th ed.; Detels, R., Abdool Karim, Q., Baum, F., Li, L., Leyland, A.H., Eds.; Oxford University Press: New York, NY, USA, 2022. [Google Scholar]
- Atun, R. Health systems, systems thinking and innovation. Health Policy Plan. 2012, 27 (Suppl. S4), iv4–iv8. [Google Scholar] [CrossRef]
- World Health Organisation. Immunization Agenda 2030: A Global Strategy to Leave No One Behind; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Aromataris, E.; Lockwood, C.; Porritt, K.; Pilla, B.; Jordan, Z. (Eds.) JBI Manual for Evidence Synthesis; The Joanna Briggs Institute (JBI): Adelaide, Australia, 2021; Available online: https://synthesismanual.jbi.global (accessed on 4 May 2025). [CrossRef]
- Page, M.; McKenzie, J.; Bossuyt, P.; Boutron, I.; Hoffmann, T.; Mulrow, C. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. PLoS Med. 2021, 18, e1003583. [Google Scholar] [CrossRef]
- Githaiga, J.N.; Noll, S.; Olivier, J.; Amponsah-Dacosta, E. What’s in a name?–How migrant populations are classified and why this matters for (in) equitable access to routine childhood and adolescent immunisation services: A scoping review. Vaccine 2025, 49, 126784. [Google Scholar] [CrossRef]
- Methley, A.M.; Campbell, S.; Chew-Graham, C.; McNally, R.; Cheraghi-Sohi, S. PICO, PICOS and SPIDER: A comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv. Res. 2014, 14, 579. [Google Scholar] [CrossRef]
- The EndNote Team. EndNote; EndNote 20; Clarivate: Philadelphia, PA, USA, 2013. [Google Scholar]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
- Bednarczyk, R.A.; Chamberlain, A.; Mathewson, K.; Salmon, D.A.; Omer, S.B. Practice-, provider-, and patient-level interventions to improve preventive care: Development of the P3 model. Prev. Med. Rep. 2018, 11, 131–138. [Google Scholar] [CrossRef]
- Thomson, A.; Robinson, K.; Vallée-Tourangeau, G. The 5As: A practical taxonomy for the determinants of vaccine uptake. Vaccine 2016, 34, 1018–1024. [Google Scholar] [CrossRef]
- Vu, M.; Ta, D.; Berg, C.J.; Bednarczyk, R.A.; Huynh, V.N.; King, A.R.; Escoffery, C. US Vietnamese Mothers’ HPV Vaccine Decision- Making for Their Adolescents: A Qualitative Study. J. Health Care Poor Underserved 2022, 33, 1985–2006. [Google Scholar] [CrossRef]
- WHO. Everybody’s Business: Strengthening Health Systems to Improve Health Outcomes: WHO’s Framework for Action; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- Witter, S.; Palmer, N.; Balabanova, D.; Mounier-Jack, S.; Martineau, T.; Klicpera, A.; Jensen, C.; Pugliese-Garcia, M.; Gilson, L. Health system strengthening—Reflections on its meaning, assessment, and our state of knowledge. Int. J. Health Plan. Manag. 2019, 34, e1980–e1989. [Google Scholar] [CrossRef] [PubMed]
- Joanna Briggs Institute. Checklist for Qualitative Research; The Joanna Briggs Institute (JBI): Adelaide, Australia, 2017. [Google Scholar]
- Joanna Briggs Institute. Checklist for Cohort Studies; The Joanna Briggs Institute (JBI): Adelaide, Australia, 2017. [Google Scholar]
- Joanna Briggs Institute. Checklist for Analytical Cross Sectional Studies; The Joanna Briggs Institute (JBI): Adelaide, Australia, 2017. [Google Scholar]
- Hong, Q.N.; Pluye, P.; Fàbregues, S.; Bartlett, G.; Boardman, F.; Cargo, M.; Dagenais, P.; Gagnon, M.-P.; Griffiths, F.; Nicolau, B. Mixed Methods Appraisal Tool (MMAT); Version 2018; Registration of Copyright (#1148552); Canadian Intellectual Property Office: Gatineau, QC, Canada, 2018. [Google Scholar]
- Allen, E.M.; Lee, H.Y.; Pratt, R.; Vang, H.; Lightfoot, E.; Desai, J.R.; Dube, A. Facilitators and Barriers of Cervical Cancer Screening and Human Papilloma Virus Vaccination Among Somali Refugee Women in the United States: A Qualitative Analysis. J. Transcult. Nurs. 2019, 30, 55–63. [Google Scholar] [CrossRef] [PubMed]
- Burke, N.J.; Do, H.H.; Talbot, J.; Sos, C.; Ros, S.; Taylor, V.M. Protecting our Khmer daughters: Ghosts of the past, uncertain futures, and the human papillomavirus vaccine. Ethn. Health 2015, 20, 376–390. [Google Scholar] [CrossRef]
- Do, H.; Seng, P.; Talbot, J.; Acorda, E.; Coronado, G.D.; Taylor, V.M. HPV vaccine knowledge and beliefs among Cambodian American parents and community leaders. Asian Pac. J. Cancer Prev. APJCP 2009, 10, 339. [Google Scholar]
- Ghebrendrias, S.; Pfeil, S.; Crouthamel, B.; Chalmiers, M.; Kully, G.; Mody, S. An Examination of Misconceptions and Their Impact on Cervical Cancer Prevention Practices among Sub-Saharan African and Middle Eastern Refugees. Health Equity 2021, 5, 382–389. [Google Scholar] [CrossRef]
- Khan, A.; Abonyi, S.; Neudorf, C.; Galea, S.; Ahmed, S. Barriers to and facilitators of human papillomavirus vaccination in an ethnically diverse group of migrant parents: A qualitative mixed methods study. Hum. Vaccines Immunother. 2023, 19, 2269721. [Google Scholar] [CrossRef]
- McComb, E.; Ramsden, V.; Olatunbosun, O.; Williams-Roberts, H. Knowledge, Attitudes and Barriers to Human Papillomavirus (HPV) Vaccine Uptake Among an Immigrant and Refugee Catch-Up Group in a Western Canadian Province. J. Immigr. Minor. Health 2018, 20, 1424–1428. [Google Scholar] [CrossRef]
- Metusela, C.; Ussher, J.; Perz, J.; Hawkey, A.; Morrow, M.; Narchal, R.; Estoesta, J.; Monteiro, M. “In my culture, we don’t know anything about that”: Sexual and reproductive health of migrant and refugee women. Int. J. Behav. Med. 2017, 24, 836–845. [Google Scholar] [CrossRef]
- Rubens-Augustson, T.; Wilson, L.A.; Murphy, M.S.Q.; Jardine, C.; Pottie, K.; Hui, C.; Stafstrom, M.; Wilson, K. Healthcare provider perspectives on the uptake of the human papillomavirus vaccine among newcomers to Canada: A qualitative study. Hum. Vaccines Immunother. 2019, 15, 1697–1707. [Google Scholar] [CrossRef]
- Salad, J.; Verdonk, P.; de Boer, F.; Abma, T.A. “A Somali girl is Muslim and does not have premarital sex. Is vaccination really necessary?” A qualitative study into the perceptions of Somali women in the Netherlands about the prevention of cervical cancer. Int. J. Equity Health 2015, 14, 68. [Google Scholar] [CrossRef] [PubMed]
- Davidson, N.; Fisher, J. “If I know about it of course I would give my son and daughter”, barriers to and enablers of accessing human papillomavirus vaccination among women from refugee and asylum-seeking backgrounds resettling in Melbourne, Australia—A qualitative study. Vaccine 2025, 53, 127064. [Google Scholar] [CrossRef] [PubMed]
- Bhatta, M.P.; Johnson, D.C.; Lama, M.; Maharjan, B.; Lhaki, P.; Shrestha, S. Cervical Cancer and Human Papillomavirus Vaccine Awareness Among Married Bhutanese Refugee and Nepali Women in Eastern Nepal. J. Community Health 2020, 45, 516–525. [Google Scholar] [CrossRef] [PubMed]
- Dalla, V.; Panagiotopoulou, E.-K.; Deltsidou, A.; Kalogeropoulou, M.; Kostagiolas, P.; Niakas, D.; Labiris, G. Level of awareness regarding cervical cancer among female Syrian refugees in Greece. J. Cancer Educ. 2020, 37, 717–727. [Google Scholar] [CrossRef]
- Gebre, H.; Ghamli, S.; Jackson, F.; Chavan, B.; Kingori, C. Knowledge, perception and utilization of cervical cancer screening and Human Papillomavirus (HPV) vaccination among immigrants and refugees in Central Ohio. Columbia Univ. J. Glob. Health 2021, 11. [Google Scholar] [CrossRef]
- Kepka, D.; Bodson, J.; Lai, D.; Sanchez-Birkhead, A.; Villalta, J.; Mukundente, V.; Tavake-Pasi, F.; Davis, F.A.; Lee, D.; Napia, E.; et al. Factors Associated with Human Papillomavirus Vaccination among Diverse Adolescents in a Region with Low Human Papillomavirus Vaccination Rates. Health Equity 2018, 2, 223–232. [Google Scholar] [CrossRef]
- Kmeid, M.; Azouri, H.; Aaraj, R.; Bechara, E.; Antonios, D. Vaccine coverage for Lebanese citizens and Syrian refugees in Lebanon. Int. Health 2019, 11, 568–579. [Google Scholar] [CrossRef]
- Lee, H.; Kim, M.; Kiang, P.; Shi, L.; Tan, K.; Chea, P.; Peou, S.; Grigg-Saito, D.C. Factors associated with HPV vaccination among Cambodian American teenagers. Public Health Nurs. 2016, 33, 493–501. [Google Scholar]
- Napolitano, F.; Gualdieri, L.; Santagati, G.; Angelillo, I.F. Knowledge and attitudes toward HPV infection and vaccination among immigrants and refugees in Italy. Vaccine 2018, 36, 7536–7541. [Google Scholar] [CrossRef]
- Riza, E.; Karakosta, A.; Tsiampalis, T.; Lazarou, D.; Karachaliou, A.; Ntelis, S.; Karageorgiou, V.; Psaltopoulou, T. Knowledge, Attitudes and Perceptions about Cervical Cancer Risk, Prevention and Human Papilloma Virus (HPV) in Vulnerable Women in Greece. Int. J. Environ. Res. Public Health 2020, 17, 6892. [Google Scholar] [CrossRef]
- Snoubar, Y.; Abusafia, B.; Turan, Z. Factors affecting cervical cancer screening and human papilloma virus vaccination among Middle Eastern refugee women in Türkiye: Indicators for social workers and nurses. Ann. Med. 2025, 57, 2468261. [Google Scholar] [CrossRef] [PubMed]
- Badre-Esfahani, S.; Larsen, M.; Seibæk, L.; Petersen, L.; Blaakær, J.; Andersen, B. Low attendance by non-native women to human papillomavirus vaccination and cervical cancer screening—A Danish nationwide register-based cohort study. Prev. Med. Rep. 2020, 19, 101106. [Google Scholar] [CrossRef] [PubMed]
- Berman, R.S.; Smock, L.; Bair-Merritt, M.H.; Cochran, J.; Geltman, P.L. Giving It Our Best Shot? Human Papillomavirus and Hepatitis B Virus Immunization Among Refugees, Massachusetts, 2011–2013. Prev. Chronic Dis. 2017, 14, E50. [Google Scholar] [CrossRef] [PubMed]
- Elmore, C.E.; Keim-Malpass, J.; Mitchell, E.M. Health Inequity in Cervical Cancer Control Among Refugee Women in the United States by Country of Origin. Health Equity 2021, 5, 119–123. [Google Scholar] [CrossRef]
- Kenny, D.X.; Hsueh, K.; Walters, R.W.; Coté, J.J. Human Papillomavirus Vaccination and Pap Smear Rates Among Burmese Refugee Girls in a Healthcare System in Omaha, Nebraska. J. Community Health 2021, 46, 1170–1176. [Google Scholar] [CrossRef]
- Moller, S.P.; Kristiansen, M.; Norredam, M. Human papillomavirus immunization uptake among girls with a refugee background compared with Danish-born girls: A national register-based cohort study. Eur. J. Cancer Prev. 2018, 27, 42–45. [Google Scholar] [CrossRef]
- Nyanchoga, M.M.; Lee, P.; Barbery, G. Exploring electronic health records to estimate the extent of catch-up immunisation and factors associated with under-immunisation among refugees and asylum seekers in south east Queensland. Vaccine 2021, 39, 6238–6244. [Google Scholar] [CrossRef]
- Lai, D.J.; Bodson, J.; Davis, F.A.; Lee, D.; Tavake-Pasi, F.; Napia, E.; Villalta, J.; Mukundente, V.; Mooney, R.; Coulter, H.; et al. Diverse Families’ Experiences with HPV Vaccine Information Sources: A Community-Based Participatory Approach. J. Community Health 2017, 42, 400–412. [Google Scholar] [CrossRef]
- Wilson, L.A.; Quan, A.M.L.; Bota, A.B.; Mithani, S.S.; Paradis, M.; Jardine, C.; Hui, C.; Pottie, K.; Crowcroft, N.; Wilson, K. Newcomer knowledge, attitudes, and beliefs about human papillomavirus (HPV) vaccination. BMC Fam. Pract. 2021, 22, 17. [Google Scholar] [CrossRef]
- Graci, D.; Piazza, N.; Ardagna, S.; Casuccio, A.; Drobov, A.; Geraci, F.; Immordino, A.; Pirrello, A.; Restivo, V.; Rumbo, R. Barriers to and Facilitators for Accessing HPV Vaccination in Migrant and Refugee Populations: A Systematic Review. Vaccines 2024, 12, 256. [Google Scholar] [CrossRef] [PubMed]
- Netfa, F.; Tashani, M.; Booy, R.; King, C.; Rashid, H.; Skinner, S.R. Knowledge, Attitudes and Perceptions of Immigrant Parents Towards Human Papillomavirus (HPV) Vaccination: A Systematic Review. Trop. Med. Infect. Dis. 2020, 5, 58. [Google Scholar] [CrossRef] [PubMed]
- Essa-Hadad, J.; Gorelik, Y.; Vervoort, J.; Jansen, D.; Edelstein, M. Understanding the health system barriers and enablers to childhood MMR and HPV vaccination among disadvantaged, minority or underserved populations in middle- and high-income countries: A systematic review. Eur. J. Public Health 2024, 34, 368–374. [Google Scholar] [CrossRef] [PubMed]
- Carreras-Abad, C.; Oliveira-Souto, I.; Pou-Ciruelo, D.; Pujol-Morro, J.M.; Soler-Palacin, P.; Soriano-Arandes, A.; Sulleiro, E.; Trevino-Maruri, B.; Broto-Cortes, C.; Esperalba, J.; et al. Health and Vaccination Status of Unaccompanied Minors After Arrival in a European Border Country: A Cross-sectional Study (2017–2020). Pediatr. Infect. Dis. J. 2022, 41, 872–877. [Google Scholar] [CrossRef]
- Fozouni, L.; Weber, C.; Lindner, A.K.; Rutherford, G.W. Immunization coverage among refugee children in Berlin. J. Glob. Health 2019, 9, 010432. [Google Scholar] [CrossRef]
- Giambi, C.; Del Manso, M.; Marchetti, G.; Olsson, K.; Adel Ali, K.; Declich, S. Immunisation of migrants in EU/EEA countries: Policies and practices. Vaccine 2019, 37, 5439–5451. [Google Scholar] [CrossRef]
- Mellou, K.; Silvestros, C.; Saranti-Papasaranti, E.; Koustenis, A.; Pavlopoulou, I.D.; Georgakopoulou, T.; Botsi, C.; Terzidis, A. Increasing childhood vaccination coverage of the refugee and migrant population in Greece through the European programme PHILOS, April 2017 to April 2018. Euro Surveill. 2019, 24, 1800326. [Google Scholar] [CrossRef]
- MacDonald, N.E. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef]
- Dinleyici, E.C.; Borrow, R. Meningococcal infections among refugees and immigrants: Silent threats of past, present and future. Hum. Vaccines Immunother. 2020, 16, 2781–2786. [Google Scholar] [CrossRef]
- Gargano, L.M.; Hajjeh, R.; Cookson, S.T. Pneumonia prevention: Cost-effectiveness analyses of two vaccines among refugee children aged under two years, Haemophilus influenzae type b-containing and pneumococcal conjugate vaccines, during a humanitarian emergency, Yida camp, South Sudan. Vaccine 2017, 35, 435–442. [Google Scholar] [CrossRef] [PubMed]
- Saifee, J.; Franco-Paredes, C.; Lowenstein, S.R. Refugee health during COVID-19 and future pandemics. Curr. Trop. Med. Rep. 2021, 8, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Oladeji, O.; Campbell, P.; Jaiswal, C.; Chamla, D.; Oladeji, B.; Ajumara, C.O.; Minguiel, L.M.; Senesie, J. Integrating immunization services into nutrition sites to improve immunization status of internally displaced persons’ children living in Bentiu protection of civilian site, South Sudan. Pan Afr. Med. J. 2019, 32, 28. [Google Scholar] [CrossRef] [PubMed]
- Kapuria, B.; Hamadeh, R.S.; Mazloum, F.; Chaalan, K.; Aung, K.; Higgins, E.; Kanaan, W.; Tohme, T.; Kamal, D.; Khoury, C.E. Immunization as an entry point for primary health care and beyond healthcare interventions—Process and insights from an integrated approach in Lebanon. Front. Health Serv. 2023, 3, 1251775. [Google Scholar] [CrossRef]
- Mirzoev, T.; Kane, S. What is health systems responsiveness? Review of existing knowledge and proposed conceptual framework. BMJ Glob. Health 2017, 2, e000486. [Google Scholar] [CrossRef]
- Fiks, A.G.; Nekrasova, E.; Hambidge, S.J. Health systems as a catalyst for immunization delivery. Acad. Pediatr. 2021, 21, S40–S47. [Google Scholar] [CrossRef]
- Lahariya, C. “Health system approach” for improving immunization program performance. J. Fam. Med. Prim. Care 2015, 4, 487–494. [Google Scholar] [CrossRef]
- Chee, G.; Pielemeier, N.; Lion, A.; Connor, C. Why differentiating between health system support and health system strengthening is needed. Int. J. Health Plan. Manag. 2013, 28, 85–94. [Google Scholar] [CrossRef]
- Mitchell, H.; Lim, R.; Gill, P.K.; Dhanoa, J.; Dubé, È.; Bettinger, J.A. What do adolescents think about vaccines? Systematic review of qualitative studies. PLoS Glob. Public Health 2022, 2, e0001109. [Google Scholar] [CrossRef]



| Selection Criteria | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Population | Involuntary migrants/forcibly displaced | Studies that do not include involuntary migrants either as the main population or as a sub-population of migrants |
| Intervention | HPV vaccination | Other vaccines recommended for adolescents including Tetanus, Diphtheria, and Pertussis (Tdap) booster, Hepatitis B, and Rubella, unless HPV vaccination was included in the regimen of vaccines reported in a study |
| Comparison | N/A | N/A |
| Outcomes | Health system determinants of delivery and uptake of HPV vaccination services among involuntary migrant populations | Studies that do not include evidence on HPV vaccination service provision-related supply- and demand-side factors |
| Study design | Peer-reviewed qualitative, quantitative, and mixed-methods empirical studies written in English language | Secondary studies (including reviews), opinions, perspectives, and commentaries |
| Context | |||
| |||
| 5As framework domains | WHO health system building blocks | Indicators of robust health systems | P3 model—health system influences |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| |
|
|
| |
|
| ||
| Author/Year | Design | Classification of Migrants | Home Countries/Region(s) | Host Countries | Actors, e.g., Providers, Patients, Caregivers |
|---|---|---|---|---|---|
| Allen et al., 2019 [49] | Qualitative | Refugees | Somalia | USA | mothers |
| Badre-Esfahani et al., 2020 [68] | Cohort | Involuntary vs. voluntary migrants | Central Asia, SE Asia, SSA, Latin America, Western countries; Turkey, Iraq, Lebanon, Pakistan, Afghanistan, Somalia, Iran, Morocco | Denmark | women |
| Berman et al., 2017 [69] | Cohort | Refugees | Predominantly Iraq, Bhutan, Somalia, and other SSA countries | USA | adolescent males and females (9–26 years) |
| Bhatta et al., 2020 [59] | Cross-sectional | Refugees | Bhutan | Nepal | women |
| Burke et al., 2015 [50] | Qualitative | Refugees | Cambodia | USA | mothers |
| Dalla et al., 2022 [60] | Cross-sectional | Refugees | Syria | Greece | women |
| Davidson and Fisher, 2025 [58] | Qualitative | Refugees and asylum seekers | Myanmar, Iraq, Syria, Iran, Sri Lanka, Colombia, Indonesia, Lebanon, Malaysia, Togo, Pakistan | Australia | women |
| Do et al., 2009 [51] | Qualitative | Refugees/migrants | Cambodia | USA | parents and community leaders |
| Elmore et al., 2021 [70] | Cohort | Refugees | Afghanistan, Bhutan, Burma, ColombiaDR Congo, El Salvador, Eritrea, Iran, Iraq, Moldova, Nepal, Syria, Russia, Sudan, Syria, Ukraine | USA | women |
| Gebre et al., 2021 [61] | Cross-sectional | Refugees/migrants | Somalia and Mexico | USA | women |
| Ghebrendrias et al., 2021 [52] | Qualitative | Refugees | Sudan, Somalia, Kenya, Ethiopia, Eritrea, Congo, Uganda, Syria, Iraq, Egypt, and Morocco | USA | women |
| Kenny et al., 2021 [71] | Cohort | Refugees | Burma | USA | adolescent females (11–26 years) |
| Kepka et al., 2018 [62] (see Lai sequel study) | Mixed Methods | Refugees | Burundi, Congo, Rwanda, Liberia, Tanzania | USA | parents, legal guardians, caregivers |
| Khan et al., 2023 [53] | Qualitative | Migrants including refugees | Refugees from West Asia; migrants from South and Southeast Asia | Canada | parents |
| Kmeid et al., 2019 [63] | Cross-sectional | Refugees | Syria | Lebanon | parents and legal guardians |
| Lai et al., 2017 [74] (see Kepka sequel study) | Mixed Methods | Refugees | Burundi, Congo, Rwanda, Liberia, Tanzania | USA | parents, legal guardians, caregivers |
| Lee et al., 2016 [64] | Cross-sectional | Refugees | Cambodia | USA | mothers |
| McComb et al., 2018 [54] | Qualitative | Immigrants including refugees | Africa, Asia, South America | Canada | women (16–26 years old) |
| Metusela et al., 2017 [55] | Qualitative | Refugees/migrants | Afghanistan, Iraq, Somalia, South Sudan, Sudan, Sri-Lanka (Tamil), India (Punjabi), South America (Latina), Sudan | Canada and Australia | women |
| Moller et al., 2018 [72] | Cohort | Refugees | 55 | Denmark | adolescent females |
| Napolitano et al., 2018 [65] | Cross-sectional | Refugees/immigrants | mainly SSA (64.5%), Eastern Europe, South Asia, North Africa, South America, Central Asia | Italy | adolescent females (12–26 years) and parents |
| Nyanchoga et al., 2021 [73] | Cohort | Refugees and asylum seekers | 42 countries—listed ones: Middle East (Afghanistan, Iran, Iraq); Asia (Myanmar, India, Pakistan, Sri Lanka); SSA (DRC, Eritrea, Ethiopia, Kenya, Somalia, Sudan); Papua New Guinea, Solomon Islands | Australia | children, adolescents, and adults |
| Riza et al., 2020 [66] | Cross-sectional | Involuntary vs. voluntary migrants | Middle East incl. Syria, Afghanistan, and Iran; SSA incl. Nigeria, Ethiopia, Cameroon, and Kenya; Eastern European countries incl. Albania, Bulgaria, and Georgia | Greece | women |
| Rubens-Augustson et al., 2019 [56] | Qualitative | Immigrants including refugees | Not given | Canada | health providers |
| Salad et al., 2015 [57] | Qualitative | Refugees | Somalia | Netherlands | women |
| Snoubar et al., 2025 [67] | Cross-sectional | Refugees | Iraq, Palestine, Syria, Yemen | Türkiye | women |
| Wilson et al., 2021 [75] | Mixed Methods | Immigrants including refugees | SSA (36%); MENA (58%); Other (6%) | Canada | adolescents (16–27 years) and caregivers |
| Building Blocks | Enablers (+) | Impediments (−) |
|---|---|---|
| 1. Leadership/governance | 1.1 policies prioritising migrants’ health needs | 1.1(a) HPV vaccination policies not implemented in some countries |
| 1.2 decentralised governance and variations in immunisation policy implementation | 1.2(a) decentralised governance and variations in immunisation policy implementation | |
| 1.3 governments as gatekeepers in migrant-inclusive immunisation policy implementation | ||
| 2. Service delivery AND medicines/vaccines | 2.1 school-based HPV vaccination programmes | 2.1(a) no HPV vaccination programme available |
| 2.2 supplementary catch-up vaccination | 2.2(a) HPV vaccination available in NIP but as voluntary routine not mandatory routine vaccination | |
| 2.3 migrant-targeted interventions | 2.3(a) health messaging targets limited audience | |
| 2.4 integrated services | 2.4(a) limited access, e.g., schools, holding camps, eligibility based on legal status | |
| 2.5 public–private partnerships | ||
| 3. Health workforce | 3.1 health provider recommendation | 3.1(a) no health provider recommendation |
| 3.2 health provider main source of HPV vaccination-related information | 3.2(a) health provider time constraints—limited time to discuss HPV vaccination | |
| 3.3 vaccine administration (including consent) | 3.3(a) health provider reticence to recommend vaccination | |
| 3.4(a) health provider inadequately trained to serve migrant populations | ||
| 4. Health information systems | 4.1 electronic health databases with migrants’ records (including immunisation data) | 4.1(a) no vaccination records available for migrant populations |
| 4.2(a) no centralised or synchronised electronic databases with migrants’ immunisation data | ||
| 5. Financing | 5.1 HPV vaccination free for all (including migrants) via NIPs and other support programmes | 5.1(a) cost for ineligible, partially covered and uninsured migrants |
| Determinants of Uptake (5As) | Enablers (+) | Impediments (−) |
|---|---|---|
| 1. Access | 1.1 easy access/convenience | 1.1(a) legal status |
| 1.2 navigating language barriers | 1.2(a) unfamiliarity with host country’s healthcare system | |
| 1.3(a) language barriers | ||
| 2. Affordability | 2.1 free vaccination | 2.1(a) cost-prohibitive |
| 2.2 willingness to vaccinate | ||
| 3. Awareness and Acceptance | 3.1 adequate knowledge about HPV vaccination:
| 3.1(a) low/lack of knowledge about HPV vaccination:
|
3.2 framing/perception of HPV vaccination:
| 3.2(a) concerns about long-term effects and effectiveness of vaccine | |
| 3.3 length of stay in host country | 3.3(a) length of stay in host country | |
3.4(a) sociocultural and religious attitudes, beliefs, and practices
| ||
| 4. Activation | 4.1 health provider recommendation | 4.1(a) health provider reticence to recommend HPV vaccination |
| 4.2 women’s agency and family support | 4.2(a) mothers’ disapproval | |
| 4.4 assumption that HPV vaccination is compulsory | 4.4(a) preventive care not prioritised | |
| 4.5 incentives |
| Health System Performance Indicators | Practice-Level Influences | Provider-Level Influences | Patient-Level Influences | WHO Building Blocks/Delivery Determinants | 5As of Uptake |
|---|---|---|---|---|---|
| Equity | Delivery: enabler—policy adaptation and implementation to include migrants | Delivery: enabler—policy implementation to include migrants impediment—differential implementation (exclusion of certain migrant sub-populations) | Uptake: enabler—easy, convenient, free access impediments—access contingent on legal status, language, knowledge/awareness-related barriers | Leadership/governance/ policy | Access Affordability |
| Quality | Delivery: enabler—updated, synchronised electronic health databases with migrants’ immunisation records impediment—no records of migrant immunisation data | Delivery: enablers—public–private partnerships impediments—health provider time constraints, limited/lack of training, reticence to recommend HPV vaccine | Delivery: impediments—no records of migrant immunisation data (could result in under- and/or over-immunisation) | Health information systems Service delivery Medicines/vaccines | Access Awareness |
| Resource mobilisation | Delivery: enablers—school-based programmes, supplementary catch-up, migrant-specific interventions, integrated services | Delivery: enablers—school-based programmes, supplementary catch-up, migrant-specific interventions, integrated services | Delivery: enablers—school-based programmes, supplementary catch-up, migrant-specific interventions, integrated services | Service delivery Medicines/vaccines | Access |
| High immunisation coverage | Delivery: enablers—public–private partnerships Uptake: enablers—culturally appropriate health messaging | Delivery: enablers—public–private partnerships, health provider recommendations; impediments—no health provider recommendation | Uptake: enablers—easy, convenient, free access, health provider recommendation, incentives impediments—difficult to access, socio-cultural beliefs | Service delivery Medicines/vaccines Health workforce | Access Awareness Acceptance Activation |
| Social/financial risk protection | Delivery and uptake: enabler—free HPV vaccine regardless of legal status impediment—HPV vaccine cost partially covered or at own cost | Delivery and uptake: enabler—free HPV vaccine regardless of legal status impediment—HPV vaccine cost partially covered or at own cost | Delivery and uptake: enabler—free HPV vaccine regardless of legal status impediment—HPV vaccine cost partially covered or at own cost | Health financing | Affordability Access Awareness |
| Responsiveness | Delivery: impediment—health promotion materials in English are not understood | Uptake: enablers—health provider recommendations, framing HPV vaccination as protective impediments—no health provider recommendation, limited/lack of training, reticence to recommend HPV vaccine | Uptake: enablers—health provider recommendations, framing HPV vaccination as protective Uptake: impediments—language barriers, mistrust of host country governments, misinformation, no health provider recommendation, under-prioritisation of preventive care | Service delivery | Access Awareness Acceptance Activation |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Githaiga, J.N.; Olivier, J.; Noll, S.; Amponsah-Dacosta, E. Health System Determinants of Delivery and Uptake of HPV Vaccination Services Among Involuntary Migrant Populations: A Qualitative Systematic Review. Vaccines 2025, 13, 1064. https://doi.org/10.3390/vaccines13101064
Githaiga JN, Olivier J, Noll S, Amponsah-Dacosta E. Health System Determinants of Delivery and Uptake of HPV Vaccination Services Among Involuntary Migrant Populations: A Qualitative Systematic Review. Vaccines. 2025; 13(10):1064. https://doi.org/10.3390/vaccines13101064
Chicago/Turabian StyleGithaiga, Jennifer Nyawira, Jill Olivier, Susanne Noll, and Edina Amponsah-Dacosta. 2025. "Health System Determinants of Delivery and Uptake of HPV Vaccination Services Among Involuntary Migrant Populations: A Qualitative Systematic Review" Vaccines 13, no. 10: 1064. https://doi.org/10.3390/vaccines13101064
APA StyleGithaiga, J. N., Olivier, J., Noll, S., & Amponsah-Dacosta, E. (2025). Health System Determinants of Delivery and Uptake of HPV Vaccination Services Among Involuntary Migrant Populations: A Qualitative Systematic Review. Vaccines, 13(10), 1064. https://doi.org/10.3390/vaccines13101064











