Seroprevalence of Poliovirus Types 1, 2, and 3 Among Children Aged 6–11 Months: Variations Across Survey Rounds in High-Risk Areas of Pakistan
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Sampling Procedure
2.3. Sample Size Estimation
2.4. Data Collection
2.5. Laboratory Methodology
2.6. Statistical Analysis
3. Results
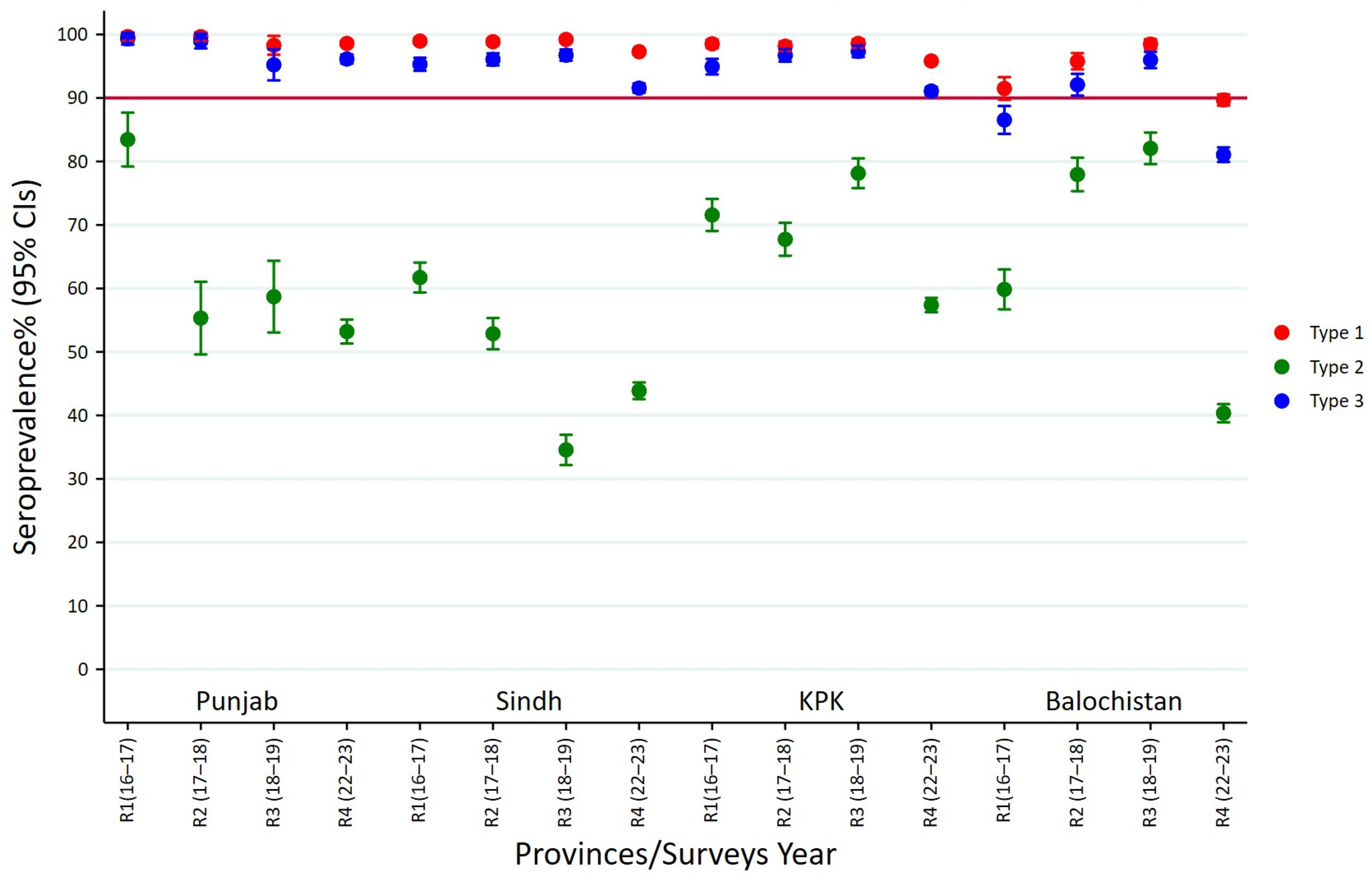
3.1. Seroprevalence of Polio Type-1 Across Provinces and Survey Rounds
3.2. Seroprevalence of Polio Type-2 Across Provinces and Survey Rounds
3.3. Seroprevalence of Polio Type-3 Across Provinces and Survey Rounds
3.4. Seroprevalence of Polio Type-1 Across High-Risk Cities
3.5. Seroprevalence of Polio Type-2 Across High-Risk Cities
3.6. Seroprevalence of Polio Type-3 Across High-Risk Cities
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. World Health Assembly. Global eradication of poliomyelitis by the year 2000. In Proceedings of the Resolution of the 41st World Health Assembly, Geneva, Switzerland, 2–13 May 1988; WHO: Geneva, Switzerland. Available online: https://apps.who.int/gb/ebwha/pdf_files/WHA57/A57_8-en.pdf (accessed on 15 September 2025).
- Haqqi, A.; Zahoor, S.; Aftab, M.N.; Tipu, I.; Rehman, Y.; Ahmed, H.; Afzal, M.S. COVID-19 in Pakistan: Impact on global polio eradication initiative. J. Med. Virol. 2020, 93, 141–143. [Google Scholar] [CrossRef]
- Bandyopadhyay, A.S.; Garon, J.; Seib, K.; Orenstein, W.A. Polio vaccination: Past, present and future. Future Microbiol. 2015, 10, 791–808. [Google Scholar] [CrossRef]
- Pons-Salort, M.; Molodecky, N.A.; O’Reilly, K.M.; Wadood, M.Z.; Safdar, R.M.; Etsano, A.; Vaz, R.G.; Jafari, H.; Grassly, N.C.; Blake, I.M. Population immunity against Serotype-2 poliomyelitis leading up to the global withdrawal of the Oral poliovirus vaccine: Spatio-temporal modelling of surveillance data. PLoS Med. 2016, 13, e1002140. [Google Scholar] [CrossRef]
- Mbaeyi, C.; Baig, S.; Safdar, R.M.; Khan, Z.; Young, H.; Jorba, J.; Wadood, Z.M.; Jafari, H.; Alam, M.M.; Franka, R. Progress Toward Poliomyelitis Eradication—Pakistan, January 2022–June 2023. Morb. Mortal. Wkly. Rep. 2023, 72, 880–885. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.E.; Greene, S.A.; Burns, C.C.; Tallis, G.; Wassilak, S.G.F.; Bolu, O. Progress toward poliomyelitis eradication—Worldwide, January 2021–March 2023. Morb. Mortal. Wkly. Rep. 2023, 72, 517–522. [Google Scholar] [CrossRef] [PubMed]
- Ataullahjan, A.; Ahsan, H.; Soofi, S.; Habib, M.A.; Bhutta, Z.A. Eradicating polio in Pakistan: A systematic review of programs and policies. Expert Rev. Vaccines 2021, 20, 661–678. [Google Scholar] [CrossRef] [PubMed]
- Ghafoor, S.; Sheikh, N. Eradication and Current Status of Poliomyelitis in Pakistan: Ground Realities. J. Immunol. Res. 2016, 2016, 6837824. [Google Scholar] [CrossRef] [PubMed]
- Shafique, F.; Hassan, M.U.; Nayab, H.; Asim, N.; Akbar, N.; Shafi, N.; Manzoor, S.; Eeden, F.V.; Ali, S. Attitude and perception towards vaccination against poliomyelitis in Peshawar, Pakistan. Rev. Saude Publica 2021, 55, 104. [Google Scholar] [CrossRef]
- Shah, M.; Khan, M.K.; Shakeel, S.; Mahmood, F.; Sher, Z.; Sarwar, M.B.; Sumrin, A. Resistance of polio to its eradication in Pakistan. Virol. J. 2011, 8, 457. [Google Scholar] [CrossRef]
- Alleman, M.M.; Jorba, J.; Henderson, E.; Diop, O.M.; Shaukat, S.; Traoré, M.A.; Wiesen, E.; Wassilak, S.G.F.; Burns, C.C. Update on Vaccine-Derived Poliovirus Outbreaks—Worldwide, January 2020–June 2021. Morb. Mortal. Wkly. Rep. 2021, 70, 1691–1699. [Google Scholar] [CrossRef]
- Macklin, G.R.; O’Reilly, K.M.; Grassly, N.C.; Edmunds, W.J.; Mach, O.; Santhana Gopala Krishnan, R.; Voorman, A.; Vertefeuille, J.F.; Abdelwahab, J.; Gumede, N.; et al. Evolving epidemiology of poliovirus serotype 2 following withdrawal of the serotype 2 oral poliovirus vaccine. Science 2020, 368, 401–405. [Google Scholar] [CrossRef]
- Burns, C.C.; Diop, O.M.; Sutter, R.W.; Kew, O.M. Vaccine-Derived Polioviruses. J. Infect. Dis. 2014, 210 (Suppl. S1), S283–S293. [Google Scholar] [CrossRef]
- Hampton, L.M.; Farrell, M.; Ramirez-Gonzalez, A.; Menning, L.; Shendale, S.; Lewis, I.; Rubin, J.; Garon, J.; Harris, J.; Hyde, T.; et al. Cessation of Trivalent Oral Poliovirus Vaccine and Introduction of Inactivated Poliovirus Vaccine—Worldwide, 2016. Morb. Mortal. Wkly. Rep. 2016, 65, 934–938. [Google Scholar] [CrossRef] [PubMed]
- Sutter, R.W.; Platt, L.; Mach, O.; Jafari, H.; Aylward, R.B. The New Polio Eradication End Game: Rationale and Supporting Evidence. J. Infect. Dis. 2014, 210 (Suppl. S1), S434–S438. [Google Scholar] [CrossRef] [PubMed]
- Duintjer Tebbens, R.J.; Hampton, L.M.; Thompson, K.M. Implementation of Coordinated Global Serotype 2 Oral Poliovirus Vaccine Cessation: Risks of Potential Non-Synchronous Cessation. BMC Infect. Dis. 2016, 16, 237. [Google Scholar] [CrossRef]
- Garon, J.; Seib, K.; Orenstein, W.A.; Gonzalez, A.R.; Blanc, D.C.; Zaffran, M.; Patel, M. Polio endgame: The global switch from tOPV to bOPV. Expert Rev. Vaccines 2016, 15, 693–708. [Google Scholar] [CrossRef]
- Taniuchi, M.; Famulare, M.; Zaman, K.; Uddin, M.J.; Upfill-Brown, A.M.; Ahmed, T.; Saha, P.; Haque, R.; Bandyopadhyay, A.S.; Modlin, J.F.; et al. Community transmission of type 2 poliovirus after cessation of trivalent oral polio vaccine in Bangladesh: An open-label cluster-randomised trial and modelling study. Lancet Infect. Dis. 2017, 17, 1069–1079. [Google Scholar] [CrossRef] [PubMed]
- Estívariz, C.F.; Pallansch, M.A.; Anand, A.; Wassilak, S.G.; Sutter, R.W.; Wenger, J.D.; Orenstein, W.A. Poliovirus vaccination options for achieving eradication and securing the endgame. Curr. Opin. Virol. 2013, 3, 309–315. [Google Scholar] [CrossRef]
- Pakistan Polio Eradication Programme. Polio Cases in Provinces. 2025. Available online: https://www.endpolio.com.pk/polioin-pakistan/polio-cases-in-provinces (accessed on 20 September 2025).
- Mir, F.; Quadri, F.; Mach, O.; Ahmed, I.; Bhatti, Z.; Khan, A.; Rehman, N.U.; Durry, E.; Salama, M.; Oberste, S.M.; et al. Monovalent Type-1 Oral Poliovirus Vaccine Given at Short Intervals in Pakistan: A Randomised Controlled, Four-Arm, Open-Label, Non-Inferiority Trial. Lancet Infect. Dis. 2015, 15, 889–897. [Google Scholar] [CrossRef]
- Asghar, H.; Diop, O.M.; Weldegebriel, G.; Malik, F.; Shetty, S.; Bassioni, L.E.; Akande, A.O.; Maamoun, E.A.; Zaidi, S.; Adeniji, A.J.; et al. Environmental Surveillance for Polioviruses in the Global Polio Eradication Initiative. J. Infect. Dis. 2014, 210 (Suppl. S1), S294–S303. [Google Scholar] [CrossRef]
- Alam, M.M.; Shaukat, S.; Sharif, S.; Angez, M.; Khurshid, A.; Malik, F.; Rehman, L.; Zaidi, S.S.Z. Detection of Multiple Cocirculating Wild Poliovirus Type 1 Lineages Through Environmental Surveillance: Impact and Progress During 2011-2013 in Pakistan. J. Infect. Dis. 2014, 210 (Suppl. S1), S324–S332. [Google Scholar] [CrossRef]
- Sahito, A.M.; Saleem, A.; Javed, S.O.; Farooq, M.; Ullah, I.; Hasan, M.M. Polio amidst COVID-19 in Pakistan: Ongoing efforts, challenges, and recommendations. Int. J. Health Plann Manag. 2022, 37, 1907–1911. [Google Scholar] [CrossRef]
- Din, M.; Asghar, M.; Ali, M. Delays in polio vaccination programs due to COVID-19 in Pakistan: A major threat to Pakistan’s long war against polio virus. Public Health 2020, 189, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, S.; Babar, M.S.; Ahmadi, A.; Essar, M.Y.; Khawaja, U.A.; Lucero-Prisno, D.E. Polio Amidst COVID-19 in Pakistan: What are the Efforts Being Made and Challenges at Hand? Am. J. Trop. Med. Hyg. 2020, 104, 446–448. [Google Scholar] [CrossRef] [PubMed]
- Rana, M.S.; Usman, M.M.; Ikram, A.; Salman, M.; Zaidi, S.S.Z.; Umair, M. The negative impact of the COVID-19 Pandemic on immunization and the positive impact on Polio eradication in Pakistan and Afghanistan. J. Infect. 2022, 85, 174–211. [Google Scholar] [CrossRef]
- Khan, M.T.; Zaheer, S.; Shafique, K. Maternal Education, Empowerment, Economic Status and Child Polio Vaccination Uptake in Pakistan: A Population Based Cross Sectional Study. BMJ Open 2017, 7, e013853. [Google Scholar] [CrossRef]
- Ben Hamida, A.; Alam, F.; Stewart, B.; Ahmad, S.; Sherani, E.N.; Khan, H.; Adekunle, A.; Mohamed, A.; Mbaeyi, C.; Franka, R.; et al. Estimating proportions of missed children and reasons for non-vaccination following implementation of “reaching the unreached” multiantigen immunization campaign—South Khyber Pakhtunkhwa, Pakistan, July–August 2023. Front. Public Health 2025, 13, 1591325. [Google Scholar] [CrossRef]
- Bjork, A.; Akbar, I.E.; Chaudhury, S.; Wadood, M.Z.; Ather, F.; Jorba, J.; Martinez, M. Progress Toward Poliomyelitis Eradication—Afghanistan, January 2022–June 2023. Morb. Mortal. Wkly. Rep. 2023, 72, 1020–1026. [Google Scholar] [CrossRef]
- Jorba, J.; Diop, O.M.; Iber, J.; Henderson, E.; Zhao, K.; Quddus, A.; Sutter, R.; Vertefeuille, J.F.; Wenger, J.; Wassilak, S.G.F.; et al. Update on Vaccine-Derived Poliovirus Outbreaks—Worldwide, January 2018–June 2019. Morb. Mortal. Wkly. Rep. 2019, 68, 1024–1028. [Google Scholar] [CrossRef]
- Cowger, T.L.; Burns, C.C.; Sharif, S.; Iber, J.; Henderson, E.; Malik, F.; Zaidi, S.S.Z.; Shaukat, S.; Rehman, L.; Pallansch, M.A.; et al. The Role of Supplementary Environmental Surveillance to Complement Acute Flaccid Paralysis Surveillance for Wild Poliovirus in Pakistan—2011–2013. PLoS ONE 2017, 12, e0180608. [Google Scholar] [CrossRef] [PubMed]
- Mbaeyi, C.; Baig, S.; Safdar, M.R.; Khan, Z.; Young, H.; Jorba, J.; Wadood, Z.M.; Jafari, H.; Alam, M.M.; Franka, R. Progress Toward Poliomyelitis Eradication—Pakistan, January 2021–July 2022. Morb. Mortal. Wkly. Rep. 2022, 71, 1313–1318. [Google Scholar] [CrossRef] [PubMed]
- Sodhar, I.A.; Mehraj, J.; Hussaini, A.S.; Ahmed, S.; Shaikh, A.A.; Zardari, A.A.; Sahitia, S.; Rasool, S.; Khowaja, A.; Stuckey, E.M. Redefining High-Risk and Mobile Population in Pakistan Polio Eradication Program; 2024. Vaccines 2025, 13, 1016. [Google Scholar] [CrossRef]
- Sutter, R.W.; John, T.J.; Jain, H.; Agarkhedkar, S.; Ramanan, P.V.; Verma, H.; Deshpande, J.; Singh, A.P.; Sreevatsava, M.; Malankar, P.; et al. Immunogenicity of Bivalent Types 1 and 3 Oral Poliovirus Vaccine: A Randomised, Double-Blind, Controlled Trial. Lancet 2010, 376, 1682–1688. [Google Scholar] [CrossRef] [PubMed]
- Grassly, N.C. The Final Stages of the Global Eradication of Poliomyelitis. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2013, 368, 20120140. [Google Scholar] [CrossRef]
- Hussain, I.; Mach, O.; Habib, A.; Bhatti, Z.; Suhag, Z.; Oberste, M.S.; Weldon, W.C.; Sutter, R.W.; Soofi, S.B.; Bhutta, Z.A. Seroprevalence of Anti-polio Antibodies in Children From Polio High-risk Areas of Pakistan: A Cross-Sectional Survey 2015–2016. Pediatr. Infect. Dis. J. 2017, 36, e230–e236. [Google Scholar] [CrossRef]
- Grassly, N.C.; Wadood, M.Z.; Safdar, R.M.; Mahamud, A.S.; Sutter, R.W. Effect of Inactivated Poliovirus Vaccine Campaigns, Pakistan, 2014–2017. Emerg. Infect. Dis. 2018, 24, 2113–2115. [Google Scholar] [CrossRef]
- Voorman, A.; Habib, M.A.; Hussian, I.; Safdar, R.M.; Ahmed, J.A.; Weldon, W.C.; Ahmed, I.; Umer, M.; Partridge, J.; Soofi, S.B. Immunity and field efficacy of type 2-containing polio vaccines after cessation of trivalent oral polio vaccine: A population-based serological study in Pakistan. Vaccine 2020, 5, 100067. [Google Scholar] [CrossRef]
- Hussain, I.; Umer, M.; Khan, A.; Sajid, M.; Ahmed, I.; Begum, K.; Iqbal, J.; Alam, M.M.; Safdar, R.M.; Baig, S.; et al. Exploring the path to polio eradication: Insights from consecutive seroprevalence surveys among Pakistani children. Front. Public Health 2024, 12, 1384410. [Google Scholar] [CrossRef]
- Weldon, W.C.; Oberste, M.S.; Pallansch, M.A. Standardized Methods for Detection of Poliovirus Antibodies. In Poliovirus; Methods in Molecular Biology, Volume 1387; Humana Press: New York, NY, USA, 2016; pp. 145–176. [Google Scholar] [CrossRef]
- Plotkin, S.A. Correlates of protection induced by vaccination. Clin. Vaccine Immunol. 2010, 17, 1055–1065. [Google Scholar] [CrossRef]
- StataCorp. Stata Statistical Software: Release 18; StataCorp LLC: College Station, TX, USA, 2024. [Google Scholar]
- Bigouette, J.P.; Wilkinson, A.L.; Tallis, G.; Burns, C.C.; Wassilak, S.G.F.; Vertefeuille, J.F. Progress Toward Polio Eradication—Worldwide, January 2019–June 2021. Morb. Mortal. Wkly. Rep. 2021, 70, 1129–1135. [Google Scholar] [CrossRef] [PubMed]
- O’Reilly, K.M.; Durry, E.; ul Islam, O.; Quddus, A.; Abid, N.; Mir, T.P.; Tangermann, R.H.; Aylward, R.B.; Grassly, N.C. The Effect of Mass Immunisation Campaigns and New Oral Poliovirus Vaccines on the Incidence of Poliomyelitis in Pakistan and Afghanistan, 2001–2011: A Retrospective Analysis. Lancet 2012, 380, 491–498. [Google Scholar] [CrossRef] [PubMed]
- Minor, P.D. Polio Vaccines and the Eradication of Poliomyelitis. Lancet 2021, 398, 1731–1740. [Google Scholar] [CrossRef] [PubMed]
- Global Polio Eradication Initiative. Report from the Twentieth Meeting of the Global Commission for the Certification of Eradication of Poliomyelitis; World Health Organization: Geneva, Switzerland, 2019; Available online: https://polioeradication.org/wp-content/uploads/2016/07/20th-meeting-of-the-Global-Commission-for-the-Certification-of-Eradication-of-Poliomyelitis-17-18-October-2019.pdf (accessed on 25 September 2025).
- Kew, O.M.; Cochi, S.L.; Jafari, H.S.; Wassilak, S.G.; Mast, E.E.; Diop, O.M.; Tangermann, R.H.; Armstrong, G.L. Possible Eradication of Wild Poliovirus Type 3—Worldwide, 2012. Morb. Mortal. Wkly. Rep. 2014, 63, 1031–1033. [Google Scholar] [PubMed Central]
- Molodecky, N.A.; Blake, I.M.; O’Reilly, K.M.; Wadood, M.Z.; Safdar, R.M.; Wesolowski, A.; Buckee, C.O.; Bandyopadhyay, A.S.; Okayasu, H.; Grassly, N.C. Risk Factors and Short-term Projections for Serotype-1 Poliomyelitis Incidence in Pakistan: A Spatiotemporal Analysis. PLoS Med. 2017, 14, e1002323. [Google Scholar] [CrossRef] [PubMed]

| Survey Rounds | Number of Districts | Clusters Covered | Households Covered | Number of Children Surveyed (N) | Male (%) | Vaccination Card (%) | OPV3 Coverage (%) | IPV Coverage (%) | Caregiver Education Level (Illiteracy Rate-%) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 10 | 326 | 4143 | 4146 | 52.0 | 65.3 | 75.3 | 69.2 | 73.3 |
| 2 | 10 | 325 | 4093 | 4094 | 52.2 | 60.3 | 69.0 | 74.0 | 76.6 |
| 3 | 10 | 324 | 3985 | 3987 | 53.0 | 70.8 | 68.8 | 81.9 | 73.2 |
| 4 | 38 | 1109 | 20,150 | 20,680 | 51.9 | 40.0 | 74.1 | 55.4 | 67.5 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hussain, I.; Khan, A.; Umer, M.; Sajid, M.; Abbas, H.; Alam, M.M.; Bosan, A.; Partridge, J.; Hafiz, R.; Haq, A.-u.; et al. Seroprevalence of Poliovirus Types 1, 2, and 3 Among Children Aged 6–11 Months: Variations Across Survey Rounds in High-Risk Areas of Pakistan. Vaccines 2025, 13, 1067. https://doi.org/10.3390/vaccines13101067
Hussain I, Khan A, Umer M, Sajid M, Abbas H, Alam MM, Bosan A, Partridge J, Hafiz R, Haq A-u, et al. Seroprevalence of Poliovirus Types 1, 2, and 3 Among Children Aged 6–11 Months: Variations Across Survey Rounds in High-Risk Areas of Pakistan. Vaccines. 2025; 13(10):1067. https://doi.org/10.3390/vaccines13101067
Chicago/Turabian StyleHussain, Imtiaz, Ahmad Khan, Muhammad Umer, Muhammad Sajid, Haider Abbas, Muhammad Masroor Alam, Altaf Bosan, Jeffrey Partridge, Rehan Hafiz, Anwar-ul Haq, and et al. 2025. "Seroprevalence of Poliovirus Types 1, 2, and 3 Among Children Aged 6–11 Months: Variations Across Survey Rounds in High-Risk Areas of Pakistan" Vaccines 13, no. 10: 1067. https://doi.org/10.3390/vaccines13101067
APA StyleHussain, I., Khan, A., Umer, M., Sajid, M., Abbas, H., Alam, M. M., Bosan, A., Partridge, J., Hafiz, R., Haq, A.-u., & Soofi, S. (2025). Seroprevalence of Poliovirus Types 1, 2, and 3 Among Children Aged 6–11 Months: Variations Across Survey Rounds in High-Risk Areas of Pakistan. Vaccines, 13(10), 1067. https://doi.org/10.3390/vaccines13101067









