Increasing Measles Seroprevalence in a Sample of Pediatric and Adolescent Population of Tuscany (Italy): A Vaccination Campaign Success
Abstract
:1. Introduction
2. Materials and Methods
- Anti-measles/IgG negative ΔA < 0.100 (cut-off);
- Anti-measles/IgG positive ΔA > 0.200;
- Anti-measles/IgG equivocal 0.100 ≤ ΔA ≤ 0.200.
3. Results
3.1. Measles Antibodies Qualitative Measurement
3.2. Measles Notification, Vaccination Status and Seroprevalence Assessment
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- WHO. Immunization, Vaccines and Biologicals-Measles. Available online: https://www.who.int/immunization/diseases/measles/en/ (accessed on 10 July 2020).
- ECDC. Annual Epidemiological Report for 2019; ECDC: Stockholm, Sweden, 2020. [Google Scholar]
- Moss, W.J. Measles. Lancet 2017, 390, 2490–2502. [Google Scholar] [CrossRef]
- Laksono, B.M.; de Vries, R.D.; Verburgh, R.J.; Visser, E.G.; de Jong, A.; Fraaij, P.L.A.; Ruijs, W.L.M.; Nieuwenhuijse, D.F.; van den Ham, H.J.; Koopmans, M.P.G.; et al. Studies into the mechanism of measles-associated immune suppression during a measles outbreak in the Netherlands. Nat. Commun. 2018, 9, 4944. [Google Scholar] [CrossRef] [PubMed]
- Misin, A.; Antonello, R.M.; Di Bella, S.; Campisciano, G.; Zanotta, N.; Giacobbe, D.R.; Comar, M.; Luzzati, R. Measles: An overview of a re-emerging disease in children and immunocompromised patients. Microorganisms 2020, 8, 276. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- ECDC. Measles Cases in 2020. Available online: https://www.cdc.gov/measles/cases-outbreaks.html (accessed on 24 July 2020).
- Siani, A. Measles outbreaks in Italy: A paradigm of the re-emergence of vaccine-preventable diseases in developed countries. Prev. Med. (Baltim.) 2019, 121, 99–104. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gianfredi, V.; D’Ancona, F.; Maraglino, F.; Cenci, C.; Iannazzo, S. Polio and measles: Reasons of missed vaccination in Italy, 2015–2017. Ann. Ig. 2019, 31, 191–201. [Google Scholar] [CrossRef] [PubMed]
- Signorelli, C.; Odone, A.; Cella, P.; Iannazzo, S.; D’Ancona, F.; Guerra, R. Infant immunization coverage in Italy (2000–2016). Ann. Ist. Super. Sanità 2017, 53, 231–237. [Google Scholar]
- Ministero della Salute. Infectious Diseases News. Available online: http://www.salute.gov.it/portale/news/p3_2_1_1_1.jsplingua=italiano&menu=notizie&p=dalministero&id=2971 (accessed on 6 July 2020).
- Antimorbillo. Available online: https://www.regione.toscana.it/-/antimorbillo (accessed on 24 July 2020).
- Istituto Superiore di Sanità Morbillo & Rosolia News. Available online: https://www.epicentro.iss.it/morbillo/bollettino/RM_News_2019_58.pdf (accessed on 24 July 2020).
- Vaccini e Vaccinazioni-Riflessioni Sulle Coperture Vaccinali 2017. Available online: https://www.epicentro.iss.it/vaccini/CopertureVaccinali2017 (accessed on 24 July 2020).
- Vaccini e Vaccinazioni-le Vaccinazioni in Italia. Available online: https://www.epicentro.iss.it/vaccini/dati_Ita#morbillo (accessed on 20 July 2020).
- ARS Toscana La Sorveglianza Epidemiologica Delle Malattie Infettive in Toscana. Rapporto Novembre 2019. Available online: https://www.ars.toscana.it/images/pubblicazioni/Rapporti/2019/Rapporto_malattie_infettive.pdf (accessed on 6 July 2020).
- Bechini, A.; Levi, M.; Boccalini, S.; Tiscione, E.; Panatto, D.; Amicizia, D.; Bonanni, P. Progress in the elimination of measles and congenital rubella in Central Italy. Hum. Vaccines Immunother. 2013, 9, 649–656. [Google Scholar] [CrossRef] [Green Version]
- Ministero della Salute. Decreto Legge 7 Giugno 2017. Available online: https://www.trovanorme.salute.gov.it/norme/dettaglioAtto?id=59548 (accessed on 6 July 2020).
- Del Fava, E.; Shkedy, Z.; Bechini, A.; Bonanni, P.; Manfredi, P. Towards measles elimination in Italy: Monitoring herd immunity by Bayesian mixture modelling of serological data. Epidemics 2012, 4, 124–131. [Google Scholar] [CrossRef]
- Bechini, A.; Boccalini, S.; Tiscione, E.; Pesavento, G.; Mannelli, F.; Peruzzi, M.; Rapi, S.; Mercurio, S.; Bonanni, P. Progress towards measles and rubella elimination in Tuscany, Italy: The role of population seroepidemiological profile. Eur. J. Public Health 2010, 22, 133–139. [Google Scholar] [CrossRef] [Green Version]
- Bonanni, P.; Bechini, A.; Boccalini, S.; Peruzzi, M.; Tiscione, E.; Boncompagni, G.; Mannelli, F.; Salmaso, S.; Filia, A.; degli Atti, M.C. Progress in Italy in control and elimination of measles and congenital rubella. Vaccine 2007, 25, 3105–3110. [Google Scholar] [CrossRef]
- WHO. Immunological Basis for Immunization Series Module 7: Measles. Available online: https://apps.who.int/iris/bitstream/handle/10665/44038/9789241597555_eng.pdf;jsessionid=760769E3C7D3E05A4884C59F09B6CFF0?sequence=1 (accessed on 6 July 2020).
- Ministero della Salute. Piano Nazionale Prevenzione Vaccinale 2017–2019. 2017. Available online: http://www.salute.gov.it/imgs/C_17_pubblicazioni_2571_allegato.pdf (accessed on 24 July 2020).
- Zanella, B.; Bechini, A.; Boccalini, S.; Sartor, G.; Tiscione, E.; Bonanni, P. Hepatitis B Seroprevalence in the Pediatric and Adolescent Population of Florence (Italy): An Update 27 Years after the Implementation of Universal Vaccination. Vaccines 2020, 8, 156. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- GeoDemo Istat. Popolazione Residente al 1° Gennaio 2017 nella Provincia di Firenze. Available online: http://demo.istat.it/pop2017/index.html (accessed on 24 July 2020).
- ISTAT. NATALITÀ E FECONDITÀ DELLA POPOLAZIONE RESIDENTE|ANNO 2018 Natalità. Available online: https://www.istat.it/it/archivio/235964 (accessed on 6 July 2020).
- WHO. Eliminating Measles and Rubella and Preventing Congenital Rubella Infection; European Regional Strategic Plan 2005–2010. Available online: https://www.euro.who.int/__data/assets/pdf_file/0008/79028/E87772.pdf (accessed on 24 July 2020).
- Tafuri, S.; Gallone, M.S.; Cappelli, M.G.; Martinelli, D.; Prato, R.; Germinario, C. Addressing the anti-vaccination movement and the role of HCWs. Vaccine 2014, 32, 4860–4865. [Google Scholar] [CrossRef] [PubMed]
- Anichini, G.; Gandolfo, C.; Fabrizi, S.; Miceli, G.B.; Terrosi, C.; Savellini, G.G.; Prathyumnan, S.; Orsi, D.; Battista, G.; Cusi, M.G. Seroprevalence to measles virus after vaccination or natural infection in an adult population, in Italy. Vaccines 2020, 8, 66. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carryn, S.; Feyssaguet, M.; Povey, M.; Di Paolo, E. Long-term immunogenicity of measles, mumps and rubella-containing vaccines in healthy young children: A 10-year follow-up. Vaccine 2019, 37, 5323–5331. [Google Scholar] [CrossRef] [PubMed]
- Plotkin, S.A. Is There a Correlate of Protection for Measles Vaccine? J. Infect. Dis. 2019, 221, 1571–1572. [Google Scholar] [CrossRef]
- Kennedy, R.B.; Ovsyannikova, I.G.; Thomas, A.; Larrabee, B.R.; Rubin, S.; Poland, G.A. Differential durability of immune responses to measles and mumps following MMR vaccination. Vaccine 2019, 37, 1775–1784. [Google Scholar] [CrossRef]
- Cherry, J.D.; Zahn, M. Clinical characteristics of measles in previously vaccinated and unvaccinated patients in California. Clin. Infect. Dis. 2018, 67, 1315–1319. [Google Scholar] [CrossRef] [Green Version]
- Risco-Risco, C.; Masa-Calles, J.; López-Perea, N.; Echevarría, J.; Rodríguez-Caravaca, G. Epidemiology of measles in vaccinated people, Spain 2003–2014. Enferm. Infecc. Microbiol. Clin. 2017, 35, 569–573. [Google Scholar] [CrossRef]
- Williams, J.R.; Manfredi, P.; Butler, A.R.; Ciofi, M.; Salmaso, S. Heterogeneity in regional notification patterns and its impact on aggregate national case notification data: The example of measles in Italy. BMC Public Health 2003, 3, 23. [Google Scholar] [CrossRef]
- Manfredi, P.; Cleur, E.M.; Williams, J.R.; Salmaso, S.; degli Atti, M.C. The pre-vaccination regional epidemiological landscape of measles in Italy: Contact patterns, effort needed for eradication, and comparison with other regions of Europe. Popul. Health Metr. 2005, 3, 1. [Google Scholar] [CrossRef] [Green Version]
- WHO. Vaccine-Preventable Diseases: Monitoring System. 2019 Global Summary Senegal. Available online: https://apps.who.int/immunization_monitoring/globalsummary/countries?countrycriteria%5Bcountry%5D%5B%5D=SEN# (accessed on 24 July 2020).
- WHO. Vaccine-Preventable Diseases: Monitoring System. 2019 Global Summary Burkina-Faso. Available online: https://apps.who.int/immunization_monitoring/globalsummary/countries?countrycriteria%5Bcountry%5D%5B%5D=BFA (accessed on 24 July 2020).
- WHO. Vaccine-Preventable Diseases: Monitoring System. 2019 Global Summary Philippines. Available online: https://apps.who.int/immunization_monitoring/globalsummary/countries?countrycriteria%5Bcountry%5D%5B%5D=PHL (accessed on 24 July 2020).
- Adamo, G.; Baccolini, V.; Massimi, A.; Barbato, D.; Cocchiara, R.; Di Paolo, C.; Mele, A.; Cianfanelli, S.; Angelozzi, A.; Castellani, F.; et al. Towards elimination of measles and rubella in Italy: Progress and challenges. PLoS ONE 2019, 14, e0226513. [Google Scholar] [CrossRef] [PubMed]
- Adamo, G.; Sturabotti, G.; Baccolini, V.; De Soccio, P.; Prencipe, G.P.; Bella, A.; Magurano, F.; Iannazzo, S.; Villari, P.; Marzuillo, C. Regional reports for the subnational monitoring of measles elimination in Italy and the identification of local barriers to the attainment of the elimination goal. PLoS ONE 2018, 13, e0205147. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- U.S. National Library of Medicine. Measles Vaccine in HCW (MV-COVID19). ClinicalTrials.gov Identifier: NCT04357028. Available online: https://clinicaltrials.gov/ct2/show/study/NCT04357028#contacts (accessed on 25 June 2020).




| Age Group (Years) | Enrolled Subjects (N) |
|---|---|
| 1–4 | 40 |
| 5–9 | 48 |
| 10–14 | 50 |
| 15–18 | 27 |
| Total | 165 |
| Anti-Measles Seroprevalence | |||
|---|---|---|---|
| Group | POSITIVE % (n/N) | NEGATIVE % (n/N) | EQUIVOCAL % (n/N) |
| Overall | 88.5 (146/165) | 8.5 (14/165) | 3 (5/165) |
| Male | 90.8 (79/87) | 6.9 (6/87) | 2.3 (2/87) |
| Female | 85.9 (67/78) | 10.3 (8/78) | 3.8 (3/78) |
| Italian | 90 (134/149) | 7.3 (11/149) | 2.7 (4/149) |
| Not-Italian | 75 (12/16) | 18.8 (3/16) | 6.2 (1/16) |
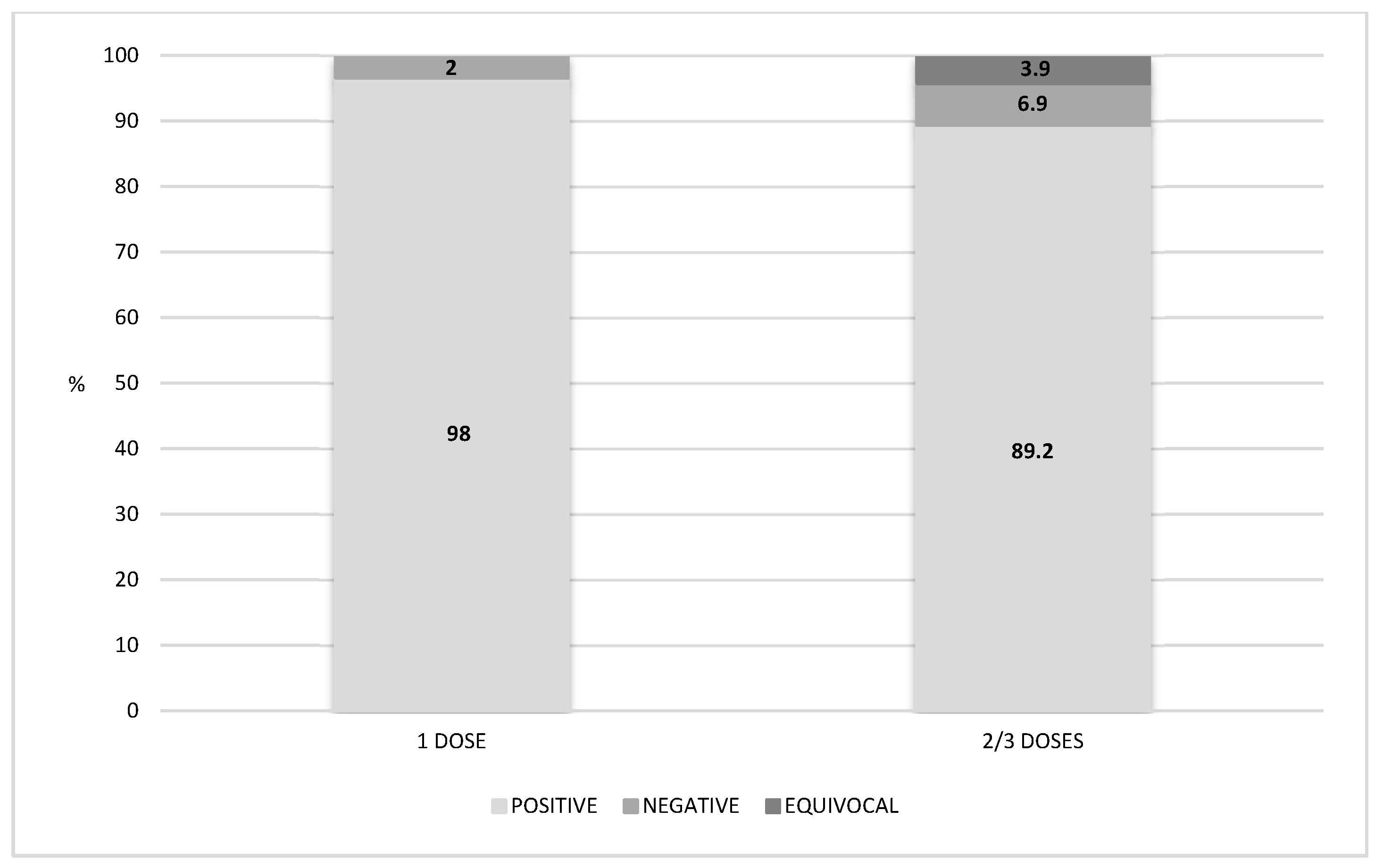
| Vaccination Status | Age Group (Years) | Positive % (n/N) | Negative % (n/N) | Equivocal % (n/N) | Total % (n/N) |
|---|---|---|---|---|---|
| Vaccinated | 92.1 (140/152) | 5.2 (8/152) | 2.7 (4/152) | 92.1 (152/165) | |
| 1–4 | 97.1 (34/35) | 2.9 (1/35) | 0 (0/35) | 23 (35/152) | |
| 5–9 | 100 (47/47) | 0 (0/47) | 0 (0/47) | 30.9 (47/152) | |
| 10–14 | 84.1 (37/44) | 9.1 (4/44) | 6.8 (3/44) | 29 (44/152) | |
| 15–18 | 89.2 (33/37) | 8.1 (3/37) | 2.7 (1/37) | 17.1 (26/152) | |
| Unvaccinated | 46.1 (6/13) | 46.1 (6/13) | 7.8 (1/13) | 7.9 (13/165) | |
| 1–4 | 20 (1/5) | 80 (4/5) | 0 (0/1) | 38.4 (5/13) | |
| 5–9 | 0 (0/1) | 100 (1/1) | 0 (0/1) | 7.8 (1/13) | |
| 10–14 | 66.6 (4/6) | 16.7 (1/6) | 16.7 (1/6) | 46 (6/13) | |
| 15–18 | 100 (1/1) | 0 (0/1) | 0 (0/1) | 7.8 (1/13) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zanella, B.; Boccalini, S.; Bonito, B.; Del Riccio, M.; Tiscione, E.; Bonanni, P.; Working Group DHS; Working Group AOUMeyer; Working Group AUSLTC; Bechini, A. Increasing Measles Seroprevalence in a Sample of Pediatric and Adolescent Population of Tuscany (Italy): A Vaccination Campaign Success. Vaccines 2020, 8, 512. https://doi.org/10.3390/vaccines8030512
Zanella B, Boccalini S, Bonito B, Del Riccio M, Tiscione E, Bonanni P, Working Group DHS, Working Group AOUMeyer, Working Group AUSLTC, Bechini A. Increasing Measles Seroprevalence in a Sample of Pediatric and Adolescent Population of Tuscany (Italy): A Vaccination Campaign Success. Vaccines. 2020; 8(3):512. https://doi.org/10.3390/vaccines8030512
Chicago/Turabian StyleZanella, Beatrice, Sara Boccalini, Benedetta Bonito, Marco Del Riccio, Emilia Tiscione, Paolo Bonanni, Working Group DHS, Working Group AOUMeyer, Working Group AUSLTC, and Angela Bechini. 2020. "Increasing Measles Seroprevalence in a Sample of Pediatric and Adolescent Population of Tuscany (Italy): A Vaccination Campaign Success" Vaccines 8, no. 3: 512. https://doi.org/10.3390/vaccines8030512







