Type IIb Heat Labile Enterotoxin B Subunit as a Mucosal Adjuvant to Enhance Protective Immunity against H5N1 Avian Influenza Viruses
Abstract
1. Introduction
2. Experimental Section
2.1. Recombinant LTIIb-B5 Cloning, Expression, and Purification
2.2. Functional TLR Ligand Assays
2.3. Recombinant HA Protein Expression and Purification
2.4. Mouse Immunization and Sample Collection
2.5. HA-Specific Antibody Titer Analysis
2.6. Neutralization Assays
2.7. Cytokine Analysis
2.8. Flow Cytometry
2.9. Virus Challenges
2.10. Histopathology
2.11. Statistical Analyses
3. Results
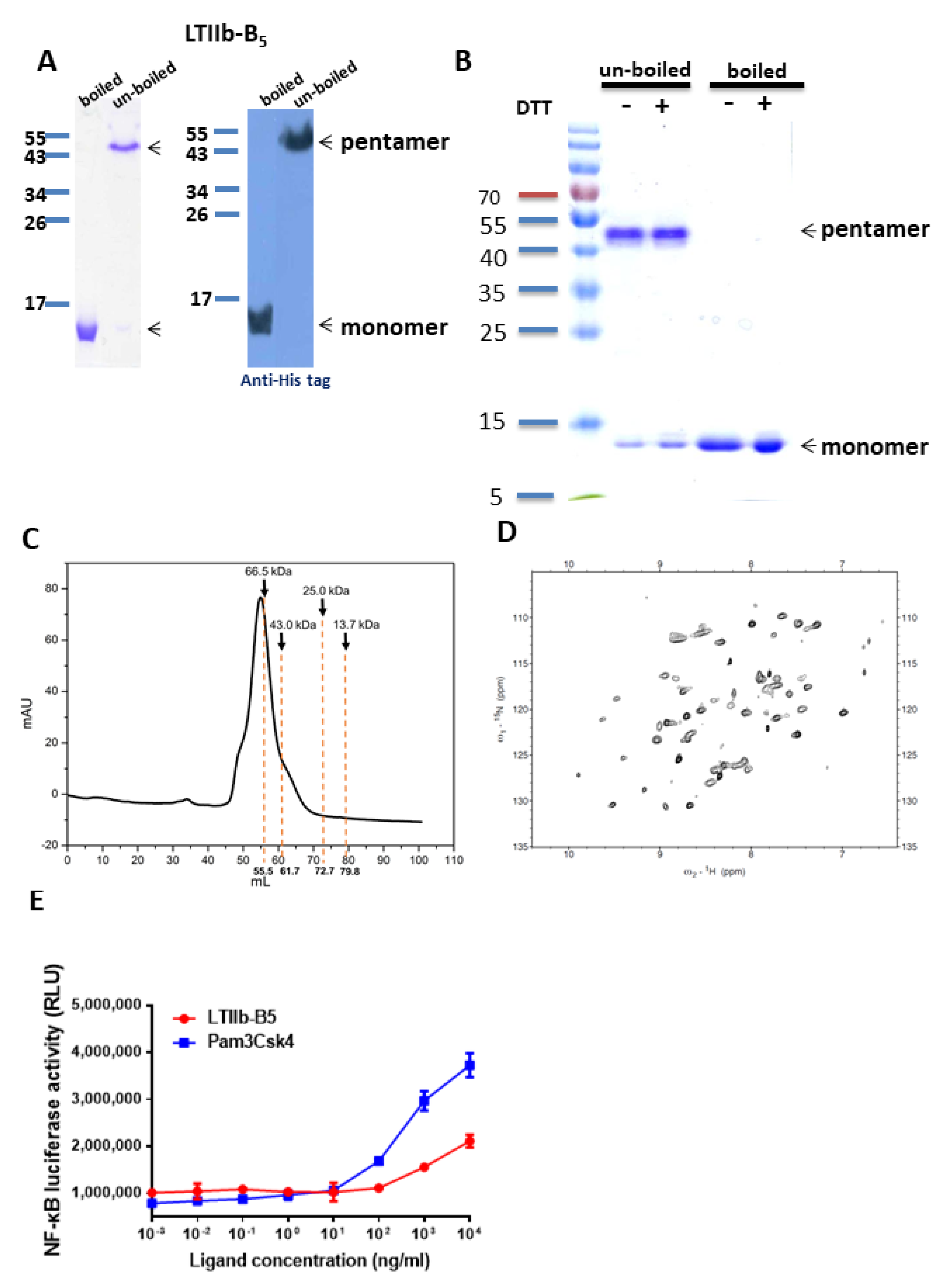
3.1. Expression, Purification, and Characterization of Recombinant LTIIb-B5 Proteins
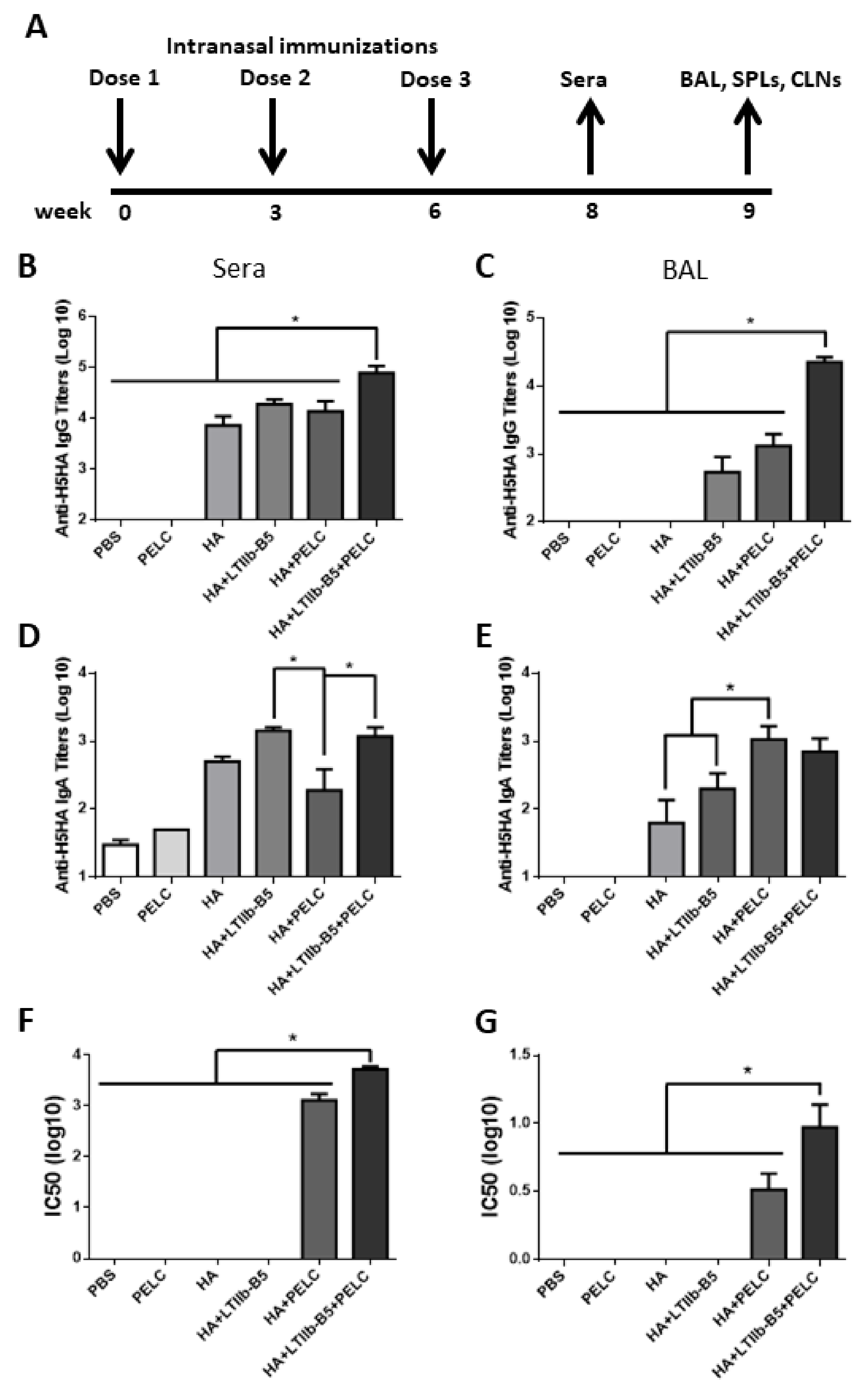
3.2. LTIIb-B5 Proteins as a Mucosal Adjuvant for HA Protein Immunizations
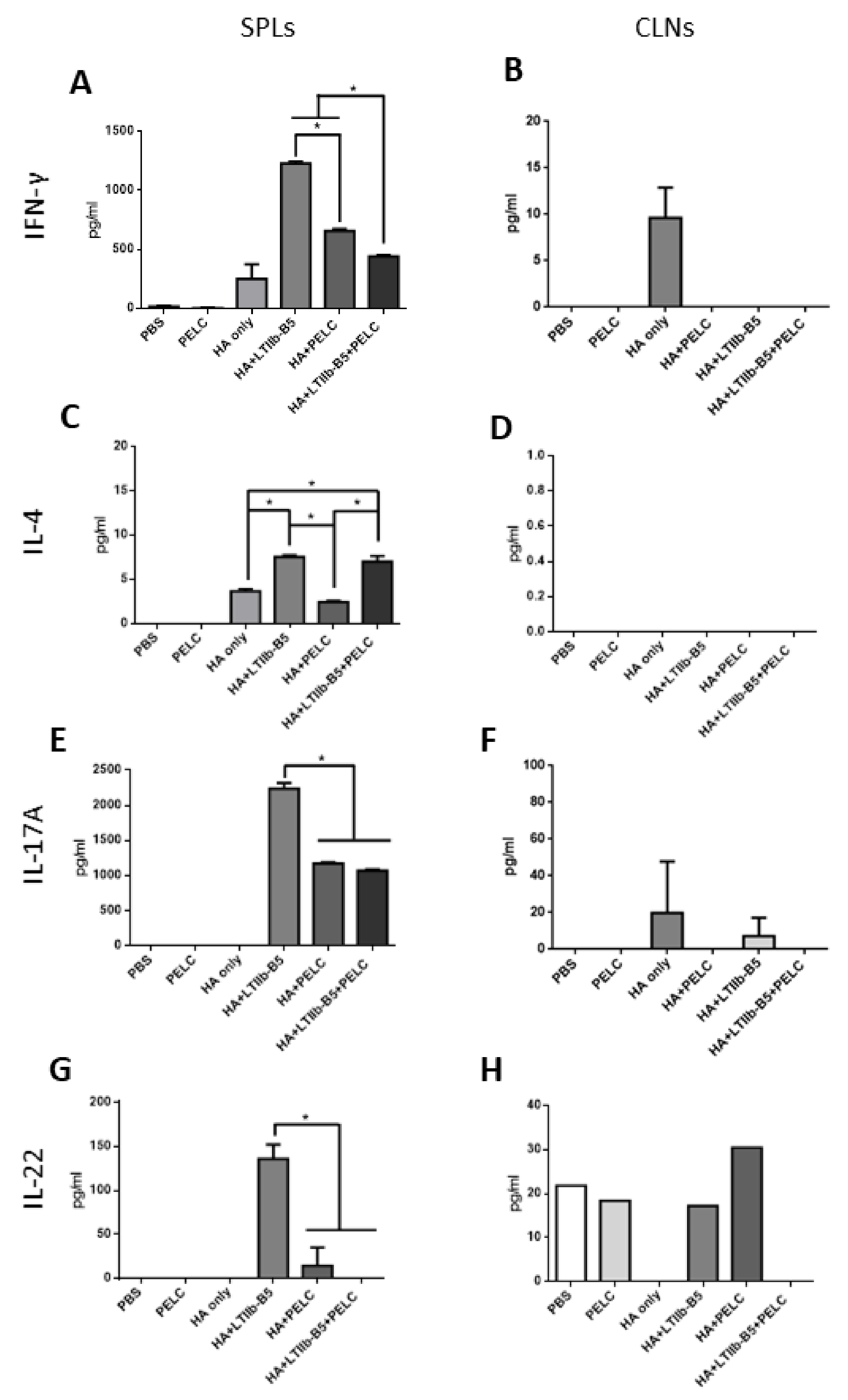
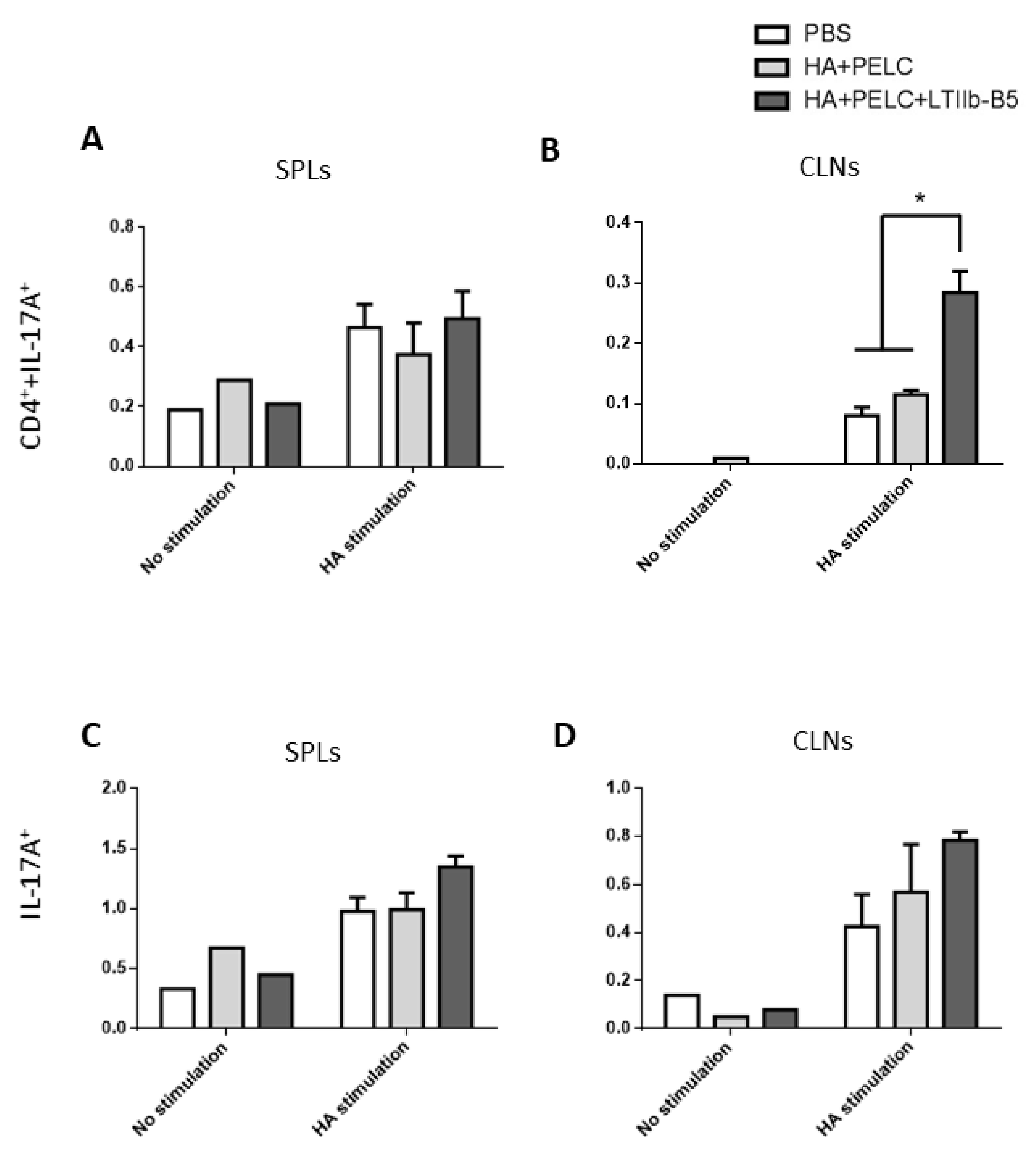
3.3. T Cell Response Detection in SPLs and CLNs
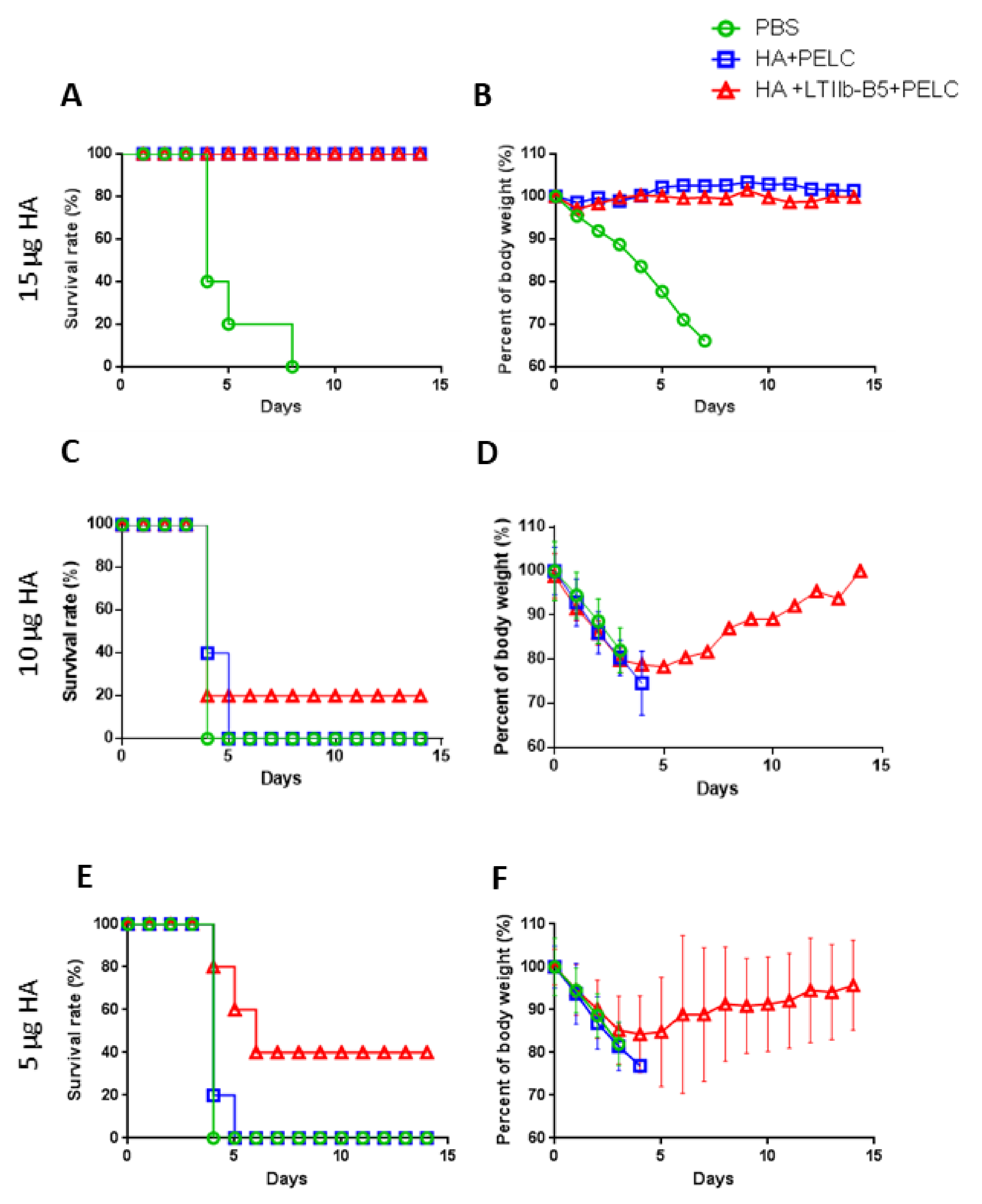
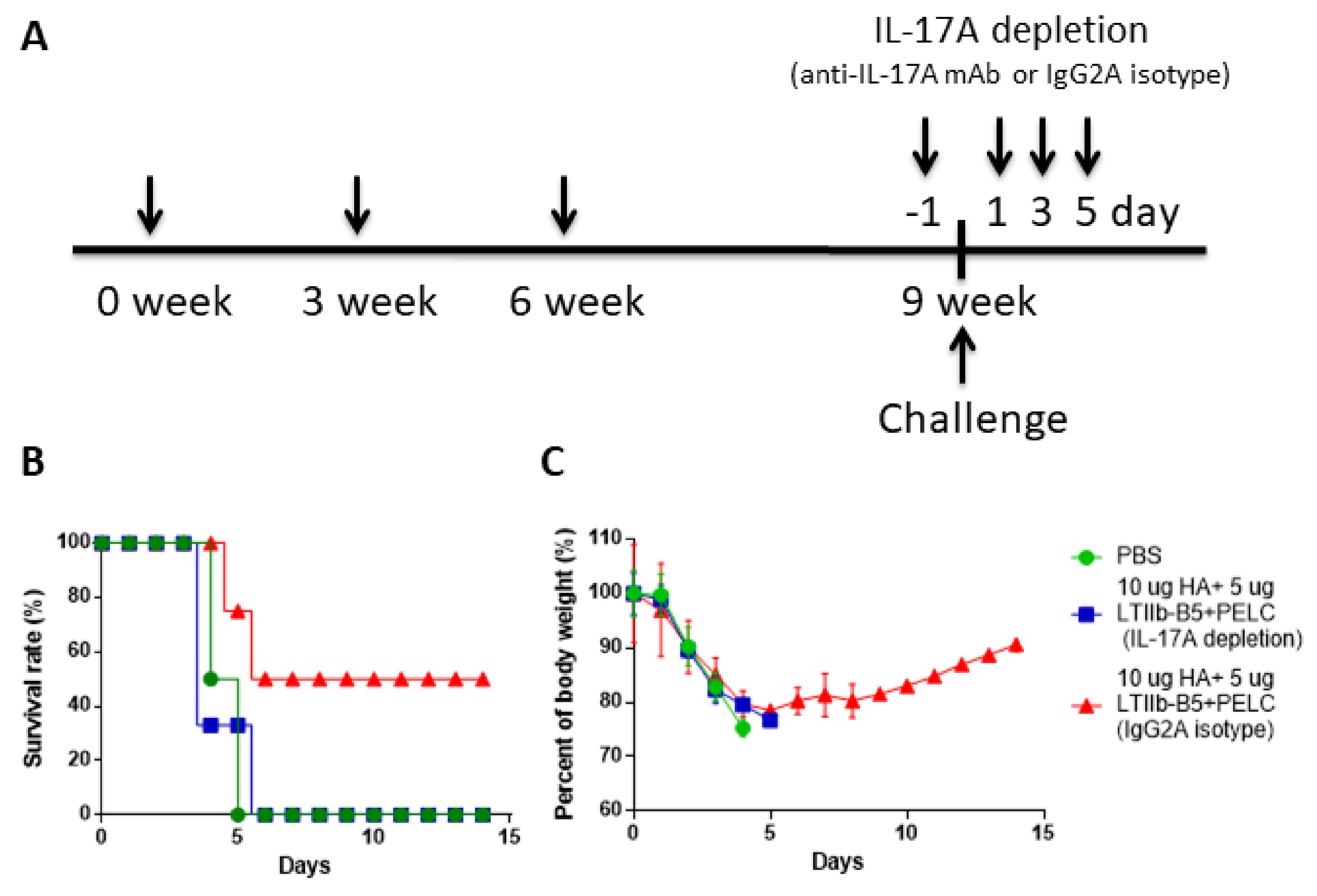
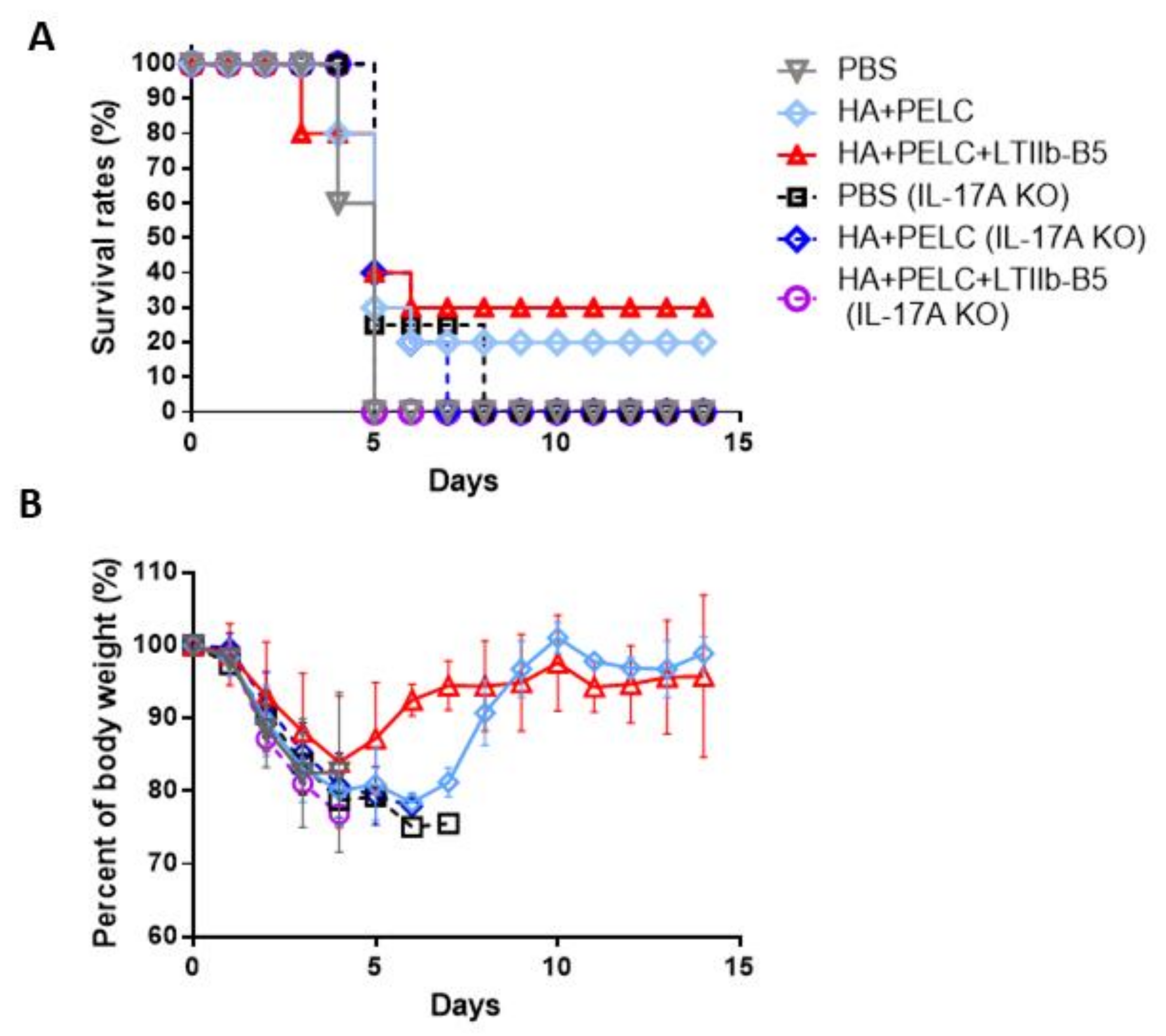
3.4. Anti-IL-17A Monoclonal Antibody Depletion, IL-17A Knockout Mice and Protective Immunity against H5N1 Challenges
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Data Availability Statement
References
- Wang, G.; Zhan, D.; Li, L.; Lei, F.; Liu, B.; Liu, D.; Xiao, H.; Feng, Y.; Li, J.; Yang, B.; et al. H5N1 avian influenza re-emergence of Lake Qinghai: Phylogenetic and antigenic analyses of the newly isolated viruses and roles of migratory birds in virus circulation. J. Gen. Virol. 2008, 89, 697–702. [Google Scholar] [CrossRef] [PubMed]
- Neumann, G.; Noda, T.; Kawaoka, Y. Emergence and pandemic potential of swine-origin H1N1 influenza virus. Nat. Cell Biol. 2009, 459, 931–939. [Google Scholar] [CrossRef] [PubMed]
- Rockman, S.; Brown, L.E. Pre-pandemic and pandemic influenza vaccines. Hum. Vaccines 2010, 6, 792–801. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, Y.; Ibrahim, M.S.; Suzuki, Y.; Ikuta, K. The changing nature of avian influenza A virus (H5N1). Trends Microbiol. 2012, 20, 11–20. [Google Scholar] [CrossRef]
- Tran, T.H.; Nquyen, T.L.; Nquyen, T.D.; Luong, T.S.; Pham, P.M.; Nguyen, V.V.; Pham, T.S.; Vo, C.D.; Le, T.Q.; Ngo, T.T.; et al. World Health Organization International Avian Influenza Investigative Team. Avian influenza A (H5N1) in 10 patients in Vietnam. N. Engl. J. Med. 2004, 350, 1179–1188. [Google Scholar] [PubMed]
- De Jong, M.D.; Simmons, C.P.; Thanh, T.T.; Hien, V.M.; Smith, M.; Chau, T.N.B.; Hoang, D.M.; Chau, N.V.V.; Khanh, T.H.; Dong, V.C.; et al. Fatal outcome of human influenza A (H5N1) is associated with high viral load and hypercytokinemia. Nat. Med. 2006, 12, 1203–1207. [Google Scholar] [CrossRef]
- Herfst, S.; Schrauwen, E.J.; Linster, M.; Chutinimitkul, S.; de Wit, E.; Munster, V.J.; Sorrell, E.M.; Bestebroer, T.M.; Burke, D.F.; Smith, D.J.; et al. Airborne Transmission of Influenza A/H5N1 Virus Between Ferrets. Science 2012, 336, 1534–1541. [Google Scholar] [CrossRef]
- Imai, M.; Watanabe, T.; Hatta, M.; Das, S.C.; Ozawa, M.; Shinya, K.; Zhong, G.; Hanson, A.; Katsura, H.; Watanabe, S.; et al. Experimental adaptation of an influenza H5 HA confers respiratory droplet transmission to a reassortant H5 HA/H1N1 virus in ferrets. Nat. Cell Biol. 2012, 486, 420–428. [Google Scholar] [CrossRef]
- Soema, P.C.; Kompier, R.; Amorij, J.-P.; Kersten, G.F. Current and next generation influenza vaccines: Formulation and production strategies. Eur. J. Pharm. Biopharm. 2015, 94, 251–263. [Google Scholar] [CrossRef]
- Czerkinsky, C.; Holmgren, J. Topical immunization strategies. Mucosal Immunol. 2010, 3, 545–555. [Google Scholar] [CrossRef]
- Davis, S.S. Nasal vaccines. Adv. Drug Deliv. Rev. 2001, 51, 21–42. [Google Scholar] [CrossRef]
- Kiyono, H.; Fukuyama, S. NALT-versus Peyer’s-patch-mediated mucosal immunity. Nat. Rev. Immunol. 2004, 4, 699–710. [Google Scholar] [CrossRef] [PubMed]
- Woodrow, K.A.; Bennett, K.M.; Lo, D.D. Mucosal Vaccine Design and Delivery. Annu. Rev. Biomed. Eng. 2012, 14, 17–46. [Google Scholar] [CrossRef] [PubMed]
- Devriendt, B.; De Geest, B.G.; Goddeeris, B.M.; Cox, E. Crossing the barrier: Targeting epithelial receptors for enhanced oral vaccine delivery. J. Control. Release 2012, 160, 431–439. [Google Scholar] [CrossRef] [PubMed]
- Liang, S.; Hosur, K.B.; Nawar, H.F.; Russell, M.W.; Connell, T.D.; Hajishengallis, G. In vivo and in vitro adjuvant activities of the B subunit of Type IIb heat-labile enterotoxin (LT-IIb-B5) from Escherichia coli. Vaccine 2009, 27, 4302–4308. [Google Scholar] [CrossRef] [PubMed]
- Liang, S.; Hajishengallis, G. Heat-Labile Enterotoxins as Adjuvants or Anti-Inflammatory Agents. Immunol. Investig. 2010, 39, 449–467. [Google Scholar] [CrossRef]
- Lin, S.-C.; Huang, M.-H.; Tsou, P.-C.; Huang, L.-M.; Chong, P.; Wu, S.-C. Recombinant Trimeric HA Protein Immunogenicity of H5N1 Avian Influenza Viruses and Their Combined Use with Inactivated or Adenovirus Vaccines. PLoS ONE 2011, 6, e20052. [Google Scholar] [CrossRef]
- Liu, W.-C.; Lin, S.-C.; Yu, Y.-L.; Chu, C.-L.; Wu, S.-C. Dendritic Cell Activation by Recombinant Hemagglutinin Proteins of H1N1 and H5N1 Influenza A Viruses. J. Virol. 2010, 84, 12011–12017. [Google Scholar] [CrossRef]
- Huang, M.-H.; Lin, S.-C.; Hsiao, C.-H.; Chao, H.-J.; Yang, H.-R.; Liao, C.-C.; Chuang, P.-W.; Wu, H.-P.; Huang, C.-Y.; Leng, C.-H.; et al. Emulsified Nanoparticles Containing Inactivated Influenza Virus and CpG Oligodeoxynucleotides Critically Influences the Host Immune Responses in Mice. PLoS ONE 2010, 5, e12279. [Google Scholar] [CrossRef]
- Nefkens, I.; Garcia, J.-M.; Ling, C.S.; Lagarde, N.; Nicholls, J.M.; Tang, D.J.; Peiris, M.; Buchy, P.; Altmeyer, R. Hemagglutinin pseudotyped lentiviral particles: Characterization of a new method for avian H5N1 influenza sero-diagnosis. J. Clin. Virol. 2007, 39, 27–33. [Google Scholar] [CrossRef]
- Lin, S.-C.; Liu, W.-C.; Jan, J.-T.; Wu, S.-C. Glycan Masking of Hemagglutinin for Adenovirus Vector and Recombinant Protein Immunizations Elicits Broadly Neutralizing Antibodies against H5N1 Avian Influenza Viruses. PLoS ONE 2014, 9, e92822. [Google Scholar] [CrossRef] [PubMed]
- Freytag, L.; Clements, J. Mucosal adjuvants. Vaccine 2005, 23, 1804–1813. [Google Scholar] [CrossRef] [PubMed]
- Milpied, P.J.; McHeyzer-Williams, M.G. High-affinity IgA needs TH17 cell functional plasticity. Nat. Immunol. 2013, 14, 313–315. [Google Scholar] [CrossRef] [PubMed]
- Mitsdoerffer, M.; Lee, Y.; Jäger, A.; Kim, H.-J.; Korn, T.; Kolls, J.K.; Cantor, H.; Bettelli, E.; Kuchroo, V.K. Proinflammatory T helper type 17 cells are effective B-cell helpers. Proc. Natl. Acad. Sci. USA 2010, 107, 14292–14297. [Google Scholar] [CrossRef]
- Lai, C.-H.; Tang, N.; Jan, J.-T.; Huang, M.-H.; Bor-Luen, C.; Chiang, B.-L.; Huang, L.-M.; Wu, S.-C. Use of recombinant flagellin in oil-in-water emulsions enhances hemagglutinin-specific mucosal IgA production and IL-17 secreting T cells against H5N1 avian influenza virus infection. Vaccine 2015, 33, 4321–4329. [Google Scholar] [CrossRef]
- Gupta, N.K.; Tomar, P.; Sharma, V.; Dixit, V.K. Development and characterization of chitosan coated poly-(ɛ-caprolactone) nanoparticulate system for effective immunization against influenza. Vaccine 2011, 29, 9026–9037. [Google Scholar] [CrossRef]
- Moon, H.-J.; Lee, J.-S.; Talactac, M.R.; Chowdhury, M.Y.; Kim, J.-H.; Park, M.-E.; Choi, Y.-K.; Sung, M.-H.; Kim, C.-J. Mucosal immunization with recombinant influenza hemagglutinin protein and poly gamma-glutamate/chitosan nanoparticles induces protection against highly pathogenic influenza A virus. Vet. Microbiol. 2012, 160, 277–289. [Google Scholar] [CrossRef]
- Meng, S.; Liu, Z.; Xu, L.; Li, L.; Mei, S.; Bao, L.; Deng, W.; Li, L.; Lei, R.; Xie, L.; et al. Intranasal immunization with recombinant HA and mast cell activator C48/80 elicits protective immunity against 2009 pandemic H1N1 influenza in mice. PLoS ONE 2011, 6, e19863. [Google Scholar] [CrossRef]
- Rubino, S.J.; Geddes, K.; Girardin, S.E. Innate IL-17 and IL-22 responses to enteric bacterial pathogens. Trends Immunol. 2012, 33, 112–118. [Google Scholar] [CrossRef]
- Aliahmadi, E.; Gramlich, R.; Grützkau, A.; Hitzler, M.; Krüger, M.; Baumgrass, R.; Schreiner, M.; Wittig, B.; Wanner, R.; Peiser, M. TLR2-activated human langerhans cells promote Th17 polarization via IL-1beta, TGF-beta and IL-23. Eur. J. Immunol. 2009, 39, 1221–1230. [Google Scholar] [CrossRef]
- De Aquino, S.G.; Abdollahi-Roodsaz, S.; Koenders, M.I.; Van De Loo, F.A.J.; Pruijn, G.J.M.; Marijnissen, R.J.; Walgreen, B.; Helsen, M.M.; Bersselaar, L.A.V.D.; De Molon, R.S.; et al. Periodontal Pathogens Directly Promote Autoimmune Experimental Arthritis by Inducing a TLR2- and IL-1–Driven Th17 Response. J. Immunol. 2014, 192, 4103–4111. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Fan, X.; Bi, S.; Li, N.; Wang, B. Toll-like Receptor 2-and 4-Mediated Reciprocal Th17 and Antibody Responses to Group A Streptococcus Infection. J. Infect. Dis. 2016, 215, 644–652. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hamada, H.; Garcia-Hernandez, M.D.L.L.; Reome, J.B.; Misra, S.K.; Strutt, T.M.; McKinstry, K.K.; Cooper, A.M.; Swain, S.L.; Dutton, R.W. Tc17, a Unique Subset of CD8 T Cells That Can Protect against Lethal Influenza Challenge. J. Immunol. 2009, 182, 3469–3481. [Google Scholar] [CrossRef] [PubMed]
- McKinstry, K.K.; Strutt, T.M.; Buck, A.; Curtis, J.D.; Dibble, J.P.; Huston, G.; Tighe, M.; Hamada, H.; Sell, S.; Dutton, R.W.; et al. IL-10 Deficiency Unleashes an Influenza-Specific Th17 Response and Enhances Survival against High-Dose Challenge. J. Immunol. 2009, 182, 7353–7363. [Google Scholar] [CrossRef]
- Crowe, C.R.; Chen, K.; Pociask, D.A.; Alcorn, J.F.; Krivich, C.; Enelow, R.I.; Ross, T.M.; Witztum, J.L.; Kolls, J.K. Critical Role of IL-17RA in Immunopathology of Influenza Infection. J. Immunol. 2009, 183, 5301–5310. [Google Scholar] [CrossRef]
- Maroof, A.; Yorgensen, Y.M.; Li, Y.; Evans, J.T. Intranasal Vaccination Promotes Detrimental Th17-Mediated Immunity against Influenza Infection. PLoS Pathog. 2014, 10, e1003875. [Google Scholar] [CrossRef]
- Kumar, P.; Chen, K.; Kolls, J.K. Th17 cell based vaccines in mucosal immunity. Curr. Opin. Immunol. 2013, 25, 373–380. [Google Scholar] [CrossRef]
- Korn, T.; Bettelli, E.; Oukka, M.; Kuchroo, V.K. IL-17 and Th17 Cells. Annu. Rev. Immunol. 2009, 27, 485–517. [Google Scholar] [CrossRef]
- Wang, X.; Ma, K.; Chen, M.; Ko, K.-H.; Zheng, B.-J.; Lu, L. IL-17A Promotes Pulmonary B-1a Cell Differentiation via Induction of Blimp-1 Expression during Influenza Virus Infection. PLoS Pathog. 2016, 12, e1005367. [Google Scholar] [CrossRef]
- Gopal, R.; Rangel-Moreno, J.; Slight, S.; Lin, Y.; Nawar, H.F.; Junecko, B.A.F.; Reinhart, T.A.; Kolls, J.K.; Randall, T.D.; Connell, T.D.; et al. Interleukin-17-dependent CXCL13 mediates mucosal vaccine–induced immunity against tuberculosis. Mucosal Immunol. 2013, 6, 972–984. [Google Scholar] [CrossRef]
- Mutsch, M.; Zhou, W.; Rhodes, P.; Bopp, M.; Chen, R.T.; Linder, T.; Spyr, C.; Steffen, R. Use of the inactivated intranasal influenza vaccine and the risk of Bell’s palsy in Switzerland. N. Engl. J. Med. 2004, 350, 896–903. [Google Scholar] [CrossRef] [PubMed]
- Lewis, D.J.; Huo, Z.; Barnett, S.; Kromann, I.; Giemza, R.; Galiza, E.; Woodrow, M.; Thierry-Carstensen, B.; Andersen, P.; Novicki, D.; et al. Transient facial nerve paralysis (Bell’s palsy) following intranasal delivery of a genetically detoxified mutant of Escherichia coli heat labile toxin. PLoS ONE 2009, 4, e6999. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tang, N.; Lu, C.-Y.; Sue, S.-C.; Chen, T.-H.; Jan, J.-T.; Huang, M.-H.; Huang, C.-H.; Chen, C.-C.; Chiang, B.-L.; Huang, L.-M.; et al. Type IIb Heat Labile Enterotoxin B Subunit as a Mucosal Adjuvant to Enhance Protective Immunity against H5N1 Avian Influenza Viruses. Vaccines 2020, 8, 710. https://doi.org/10.3390/vaccines8040710
Tang N, Lu C-Y, Sue S-C, Chen T-H, Jan J-T, Huang M-H, Huang C-H, Chen C-C, Chiang B-L, Huang L-M, et al. Type IIb Heat Labile Enterotoxin B Subunit as a Mucosal Adjuvant to Enhance Protective Immunity against H5N1 Avian Influenza Viruses. Vaccines. 2020; 8(4):710. https://doi.org/10.3390/vaccines8040710
Chicago/Turabian StyleTang, Neos, Chun-Yi Lu, Shih-Che Sue, Ting-Hsuan Chen, Jia-Tsrong Jan, Ming-Hsi Huang, Chung-Hsiung Huang, Chung-Chu Chen, Bor-Luen Chiang, Li-Min Huang, and et al. 2020. "Type IIb Heat Labile Enterotoxin B Subunit as a Mucosal Adjuvant to Enhance Protective Immunity against H5N1 Avian Influenza Viruses" Vaccines 8, no. 4: 710. https://doi.org/10.3390/vaccines8040710
APA StyleTang, N., Lu, C.-Y., Sue, S.-C., Chen, T.-H., Jan, J.-T., Huang, M.-H., Huang, C.-H., Chen, C.-C., Chiang, B.-L., Huang, L.-M., & Wu, S.-C. (2020). Type IIb Heat Labile Enterotoxin B Subunit as a Mucosal Adjuvant to Enhance Protective Immunity against H5N1 Avian Influenza Viruses. Vaccines, 8(4), 710. https://doi.org/10.3390/vaccines8040710







