Influenza Vaccination and Non-Pharmaceutical Measure Effectiveness for Preventing Influenza Outbreaks in Schools: A Surveillance-Based Evaluation in Beijing
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Information Collection
2.2. Influenza Identification
2.3. Data Management and Statistical Analysis
3. Results
3.1. Febrile Illness Outbreak Characteristics
3.2. Serious Outbreaks vs. Mild Outbreaks
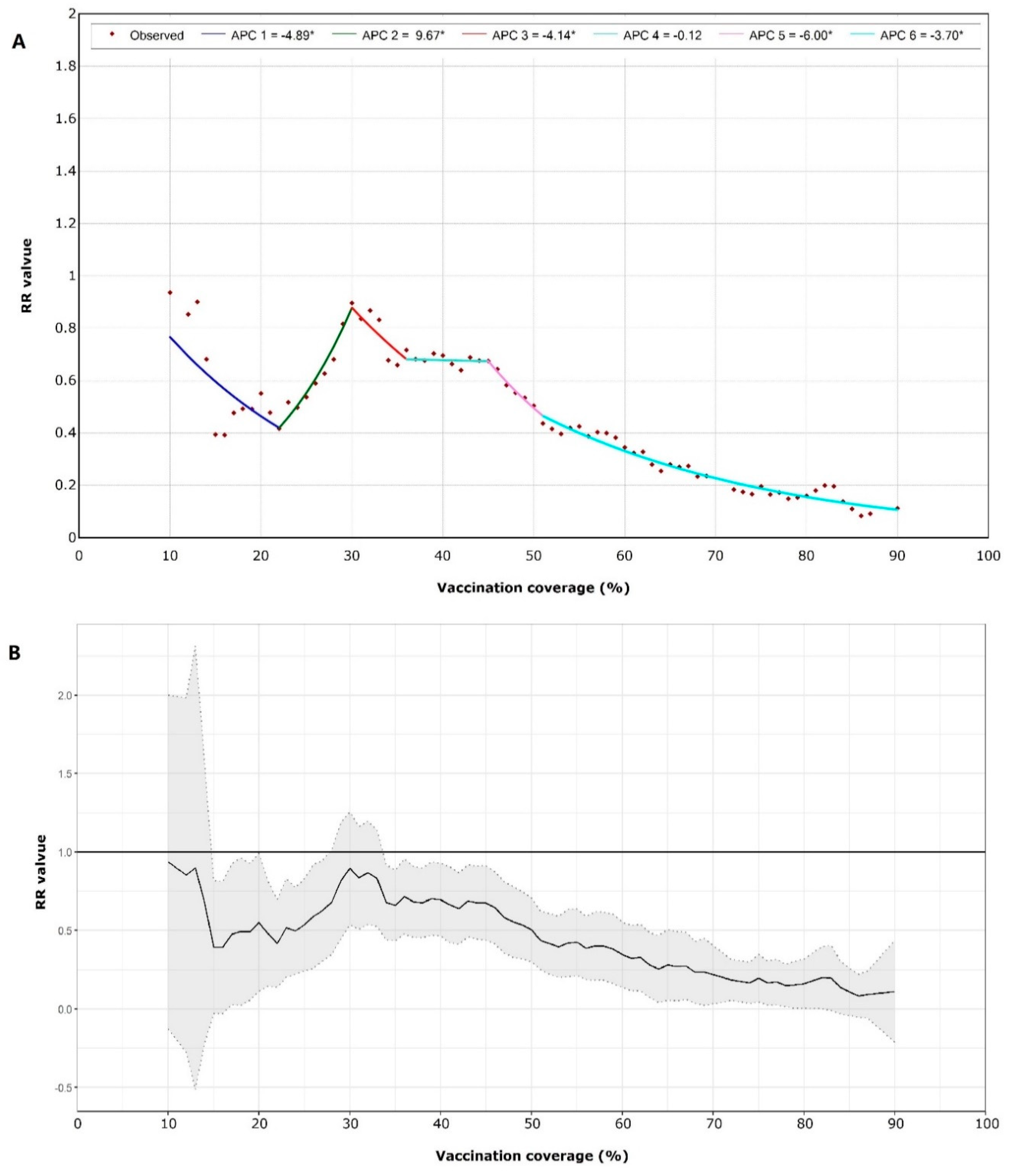
3.3. Vaccination for School Influenza Outbreaks
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Tokars, J.I.; Olsen, S.J.; Reed, C. Seasonal Incidence of Symptomatic Influenza in the United States. Clin Infect. Dis 2018, 66, 1511–1518. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Influenza (Seasonal). Available online: https://www.who.int/en/news-room/fact-sheets/detail/influenza-(seasonal) (accessed on 20 July 2020).
- National Immunization Advisory Committee (NIAC); Technical Working Group (TWG); Influenza Vaccination TWG. Technical guidelines for seasonal influenza vaccination in China, 2019–2020. Chin. J. Epidemiol. 2019, 40, 1333–1349. [Google Scholar]
- Gemmetto, V.; Barrat, A.; Cattuto, C. Mitigation of infectious disease at school: Targeted class closure vs school closure. BMC Infect. Dis. 2014, 14, 695. [Google Scholar] [CrossRef] [PubMed]
- Barclay, V.C.; Smieszek, T.; He, J.; Cao, G.; Rainey, J.J.; Gao, H.; Uzicanin, A.; Salathé, M. Positive network assortativity of influenza vaccination at a high school: Implications for outbreak risk and herd immunity. PLoS ONE 2014, 9, e87042. [Google Scholar] [CrossRef] [PubMed]
- Li, C.C.; Wang, L.; Eng, H.L.; You, H.L.; Chang, L.S.; Tang, K.S.; Lin, Y.J.; Kuo, H.C.; Lee, I.K.; Liu, J.W.; et al. Correlation of pandemic (H1N1) 2009 viral load with disease severity and prolonged viral shedding in children. Emerg. Infect. Dis 2010, 16, 1265–1272. [Google Scholar] [CrossRef] [PubMed]
- Sauerbrei, A.; Schmidt-Ott, R.; Hoyer, H.; Wutzler, P. Seroprevalence of influenza A and B in German infants and adolescents. Med. Microbiol. Immunol. 2009, 198, 93–101. [Google Scholar] [CrossRef] [PubMed]
- Longini, I.J.; Koopman, J.S.; Monto, A.S.; Fox, J.P. Estimating household and community transmission parameters for influenza. Am. J. Epidemiol. 1982, 115, 736–751. [Google Scholar] [CrossRef] [PubMed]
- Viboud, C.; Boëlle, P.Y.; Cauchemez, S.; Lavenu, A.; Valleron, A.J.; Flahault, A.; Carrat, F. Risk factors of influenza transmission in households. Br. J. Gen. Pract. 2004, 54, 684–689. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, L.; Yang, J.; Zhu, F.; Wang, L.; Guo, J.; Tang, J.; Fang, Q.; Wang, D.; Chen, T. Influenza–like illness outbreaks in China during 2017–2018 surveillance season. Chin. J. Prev. Med. 2019, 53, 982–986. [Google Scholar]
- Li, M.; Feng, L.; Cao, Y.; Peng, Z.; Yu, H. Epidemiological characteristics of influenza outbreaks in China, 2005–2013. Chin. J. Epidemiol. 2015, 7, 705–708. [Google Scholar]
- Grohskopf, L.A.; Alyanak, E.; Broder, K.R.; Walter, E.B.; Fry, A.M.; Jernigan, D.B. Prevention and Control of Seasonal Influenza with Vaccines: Recommendations of the Advisory Committee on Immunization Practices-United States, 2019–2020 Influenza Season. MMWR Recomm. Rep. 2019, 68, 1–21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. Vaccines against influenza WHO position paper–November 2012. Wkly. Epidemiol. Rec. 2012, 87, 461–476. [Google Scholar]
- European Centre for Disease Prevention and Control. Factsheet about Seasonal Influenza. Available online: https://www.ecdc.europa.eu/en/seasonal-influenza/facts/factsheet (accessed on 23 July 2020).
- Pan, Y.; Wang, Q.; Yang, P.; Zhang, L.; Wu, S.; Zhang, Y.; Sun, Y.; Duan, W.; Ma, C.; Zhang, M.; et al. Influenza vaccination in preventing outbreaks in schools: A long-term ecological overview. Vaccine 2017, 35, 7133–7138. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.; Huang, Y.; Liu, R.; Xie, Z.; Chen, S.; Hu, G. Evaluating the effects of common control measures for influenza A (H1N1) outbreak at school in China: A modeling study. PLoS ONE 2017, 12, e177672. [Google Scholar] [CrossRef] [PubMed]
- Flannery, B.; Clippard, J.; Zimmerman, R.K.; Nowalk, M.P.; Jackson, M.L.; Jackson, L.A.; Monto, A.S.; Petrie, J.G.; McLean, H.Q.; Belongia, E.A.; et al. Early estimates of seasonal influenza vaccine effectiveness-United States, January 2015. MMWR Morb. Mortal. Wkly. Rep. 2015, 64, 10–15. [Google Scholar] [PubMed]
- Chinese National Influenza Center. Chinese National Technical Guidelines for Influenza Surveillance (2017 Edition). Available online: http://ivdc.chinacdc.cn/cnic/zyzx/jcfa/201709/t20170930_153976.htm (accessed on 20 July 2020).
- Wang, J.; Xie, H.; Fisher, J.H. Multilevel Models: Applications Using SAS, 1st ed.; Higher Education Press: Beijing, China, 2009; pp. 113–139. [Google Scholar]
- Sun, Y.; Yang, P.; Zhang, L.; Wu, S.; Zhang, Y.; Duan, W.; Wang, Q.; Wang, H. Epidemiological characteristics of febrile outbreaks in Beijing during 2018–2019 influenza season. Int. J. Virol. 2020, 27, 19–22. [Google Scholar]
- Chinese National Influenza Center. China Influenza Surveillance Weekly Report No. 549, Week 25, 2019. Available online: http://www.chinaivdc.cn/cnic/zyzx/lgzb/201906/t20190628_203621.htm (accessed on 1 August 2020).
- World Health Organization. WHO Recommended Composition of Influenza Virus Vaccines for Use in the 2019–2020 Northern Hemisphere Influenza Season. Available online: https://www.who.int/influenza/vaccines/virus/recommendations/2019_20_north/en/ (accessed on 1 August 2020).
- Moa, A.M.; Chughtai, A.A.; Muscatello, D.J.; Turner, R.M.; MacIntyre, C.R. Immunogenicity and safety of inactivated quadrivalent influenza vaccine in adults: A systematic review and meta-analysis of randomised controlled trials. Vaccine 2016, 34, 4092–4102. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Characteristic | Mild Febrile Outbreaks (n = 354) | Serious Febrile Outbreaks (n = 108) | Total | Z/χ2 | p Value |
|---|---|---|---|---|---|
| Type of school 1 | |||||
| Primary school | 282 (77.90%) | 80 (22.10%) | 362 (100.00%) | 1.52 | 0.22 |
| Middle/high school | 72 (72.00%) | 28 (28.00%) | 100 (100.00%) | ||
| Areas 2 | |||||
| Urban | 205 (78.54%) | 56 (21.46%) | 261 (100.00%) | 1.24 | 0.27 |
| Rural | 149 (74.13%) | 52 (25.87%) | 201 (100.00%) | ||
| Male/female in febrile illnesses 2 | 1.17 (0.67–1.67) | 1.14 (0.79–1.42) | 1.14 (0.67–1.67) | 0.22 | 0.83 |
| Male/female of class 2 | 1.07 (0.95–1.21) | 1.10 (0.95–1.23) | 1.07 (0.95–1.21) | 0.55 | 0.58 |
| Number of students in class 2 | 39.00 (34–43) | 41.00 (37.0–45.5) | 39.00 (35–43) | 3.73 | 0.0002 |
| Subtype/lineage 1 | |||||
| B(Victoria) | 173 (78.28%) | 48 (21.72%) | 221 (100.00%) | 3.54 | 0.32 |
| A(H1N1)pdm09 | 53 (82.81%) | 11 (17.19%) | 64 (100.00%) | ||
| A(H3N2) | 110 (72.37%) | 42 (27.63%) | 152 (100.00%) | ||
| Other | 18 (72.00%) | 7 (28.00%) | 25 (100.00%) | ||
| Days from first case to intervention 2 | 3.00 (2.00–4.00) | 4.00 (3.00–5.00) | 3.00 (2.00–4.00) | 4.84 | <0.0001 |
| Influenza activity when outbreak reported 2,3 | 0.40 (0.30–0.55) | 0.44 (0.29–0.55) | 0.40 (0.29–0.55) | 0.44 | 0.66 |
| Vaccination coverage of class 2 | 0.39 (0.24–0.52) | 0.33 (0.21–0.47) | 0.37 (0.23–0.51) | 2.17 | 0.03 |
| Vaccination coverage of school 2 | 0.38 (0.31–0.47) | 0.36 (0.27–0.46) | 0.38 (0.30–0.47) | 1.98 | 0.047 |
| Variables | β | t | p | OR (95%CI) |
|---|---|---|---|---|
| Intercept | −2.19 | −3.61 | 0.003 | 0.11 (0.03–0.42) |
| Primary school | −0.27 | −0.81 | 0.43 | 0.76 (0.37–1.54) |
| Urban | 0.57 | 1.09 | 0.29 | 1.78 (0.57–5.44) |
| More male illnesses | −0.02 | −0.08 | 0.94 | 0.98 (0.56–1.66) |
| More male students in class | 0.26 | 0.93 | 0.37 | 1.29 (0.72–2.36) |
| Large class | 0.87 | 3.08 | 0.008 | 2.38 (1.28–4.26) |
| High level influenza activity when outbreak reported | 0.17 | 0.65 | 0.53 | 1.19 (0.68–2.14) |
| A(H1N1)pdm09 vs. A(H3N2) | −0.63 | −1.44 | 0.17 | 0.53 (0.21–1.36) |
| B(Victoria) vs. A(H3N2) | −0.24 | −0.72 | 0.48 | 0.79 (0.4–1.63) |
| Other vs. A(H3N2) | 0.02 | 0.04 | 0.97 | 1.02 (0.33–3.21) |
| Days from first case to intervention | 0.16 | 2.37 | 0.03 | 1.17 (1.02–1.34) |
| High vaccination coverage of class | −0.27 | −0.85 | 0.41 | 0.77 (0.35–1.35) |
| High vaccination coverage of school | −0.10 | −0.28 | 0.78 | 0.9 (0.4–1.89) |
| Characteristic | School without Outbreak (n = 1728) | School with Outbreaks (n = 283) | Total | Z/χ2 | p |
|---|---|---|---|---|---|
| Type of school 1 | |||||
| Primary school | 1010 (83.82%) | 195 (16.18%) | 1205 (100%) | 39.94 | <0.001 |
| Nine-year school | 53 (68.83%) | 24 (31.17%) | 77 (100%) | ||
| Middle/high school | 665 (91.22%) | 64 (8.78%) | 729 (100%) | ||
| Number of classes in school 1 | 17 (10–25) | 26 (18–37) | 18 (11–28) | 10.57 | <0.001 |
| Number of students in school 1 | 488 (235.5–844) | 910 (574–1395) | 535 (269–910) | 12.01 | <0.001 |
| Vaccination coverage of school 1 | 0.49 (0.34–0.67) | 0.42 (0.32–0.53) | 0.48 (0.33–0.65) | −5.36 | <0.001 |
| Areas 2 | |||||
| Urban | 915 (86.24%) | 146 (13.76%) | 1061 (100%) | 0.18 | 0.67 |
| Rural | 813 (85.58%) | 137 (14.42%) | 950 (100%) |
| Subtype/Lineage | Outbreaks | School with Outbreaks | Effect of High Vaccination Coverage (RR) | 95%CI | t | p |
|---|---|---|---|---|---|---|
| A(H3N2) | 152 | 114 | 0.78 | 0.20–3.10 | −0.38 | 0.71 |
| B(Victoria) | 221 | 144 | 0.40 | 0.24–0.67 | −3.8 | 0.002 |
| A(H1N1)pdm09 1 | 64 | 51 | 0.59 | 0.20–1.72 | −1.06 | 0.31 |
| Other 2 | 25 | 23 | - | - | - | - |
| Total 3 | 462 | 283 | 0.50 | 0.34–0.75 | −3.65 | 0.003 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sun, Y.; Yang, P.; Wang, Q.; Zhang, L.; Duan, W.; Pan, Y.; Wu, S.; Wang, H. Influenza Vaccination and Non-Pharmaceutical Measure Effectiveness for Preventing Influenza Outbreaks in Schools: A Surveillance-Based Evaluation in Beijing. Vaccines 2020, 8, 714. https://doi.org/10.3390/vaccines8040714
Sun Y, Yang P, Wang Q, Zhang L, Duan W, Pan Y, Wu S, Wang H. Influenza Vaccination and Non-Pharmaceutical Measure Effectiveness for Preventing Influenza Outbreaks in Schools: A Surveillance-Based Evaluation in Beijing. Vaccines. 2020; 8(4):714. https://doi.org/10.3390/vaccines8040714
Chicago/Turabian StyleSun, Ying, Peng Yang, Quanyi Wang, Li Zhang, Wei Duan, Yang Pan, Shuangsheng Wu, and Huaqing Wang. 2020. "Influenza Vaccination and Non-Pharmaceutical Measure Effectiveness for Preventing Influenza Outbreaks in Schools: A Surveillance-Based Evaluation in Beijing" Vaccines 8, no. 4: 714. https://doi.org/10.3390/vaccines8040714
APA StyleSun, Y., Yang, P., Wang, Q., Zhang, L., Duan, W., Pan, Y., Wu, S., & Wang, H. (2020). Influenza Vaccination and Non-Pharmaceutical Measure Effectiveness for Preventing Influenza Outbreaks in Schools: A Surveillance-Based Evaluation in Beijing. Vaccines, 8(4), 714. https://doi.org/10.3390/vaccines8040714





