Knowledge, Attitude and Practice of Main Stakeholders towards Human Papilloma Virus Infection and Vaccination in Mombasa and Tana-River Counties in Kenya: A Qualitative Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Area
2.2. Study Design and Sampling
2.3. Data Collection
2.4. Data Analysis
2.5. Techniques to Enhance Trustworthiness
2.6. Ethical Issues Pertaining Human Subjects
3. Results
3.1. Demographic Characteristics of Participants
3.2. Burden of Cervical Cancer
“...Yes, cervical cancer is a real problem in my community. We have had cases of several women who get diagnosed at very late stages and end up losing their life and practically we lost one of the community health volunteers to cervical cancer because it was diagnosed at a very late stage”.
“...Yeah it is, well of late we are getting cases because we have been encouraging people to do cervical cancer screening, and I think we got some few cases, so cervical cancer it is real in our community”.
“...Yes, it is rampant. So many people die with cervical cancer”.
“...It is a very serious problem, because, in the past, we did not understand the disease, but this time, we have seen women; it has become very challenging, because many are suffering from the disease. Before it is known, the mother loses her life, she dies“.
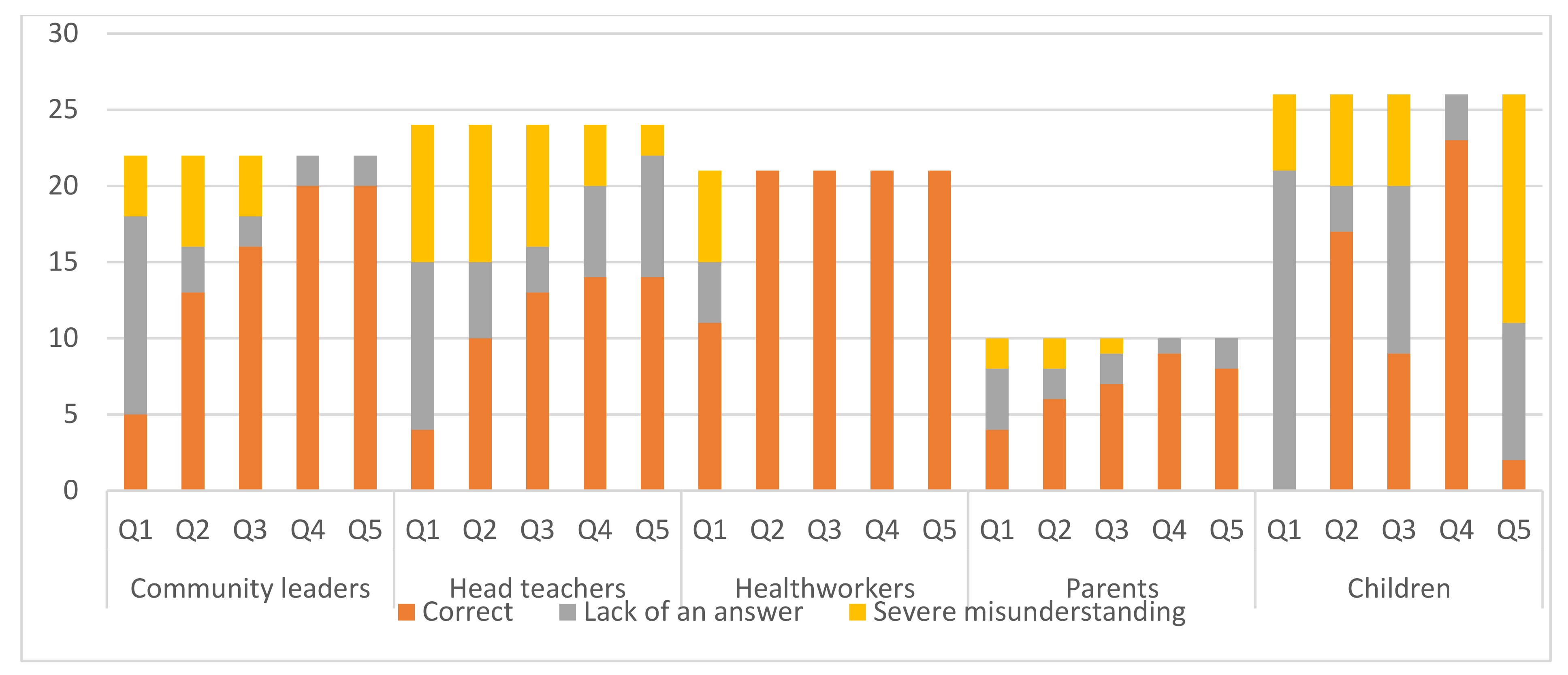
3.3. Knowledge on Cervical Cancer, HPV and HPV Vaccination
“…I don’t think it’s important at this point because I have never heard of a young child having the cervical cancer or something”.
“…if she received this vaccine, even if she goes to get married, if she meets the man who is infected with the HPV virus, they do not get it. She will be safe”.
“…I can’t tell the prevention because I don’t know what is cervical cancer”.
“…Preventing will be by giving medicine, try to prevent it by giving medicine that will prevent it from happening”.
“…prevention mmmmmh mainly this disease we can prevent by your lifestyle maybe. The food you eat, that is your lifestyle”.
“…All I know is the one that is associated with HIV”.
“… acidic food actually, kind of thinking is a bit, delays it to the feelings of papilloma because once you eat this thing you feel some changes and then you relate it to papilloma”.
“…I have heard it is a terrible disease that is killing people”.
“…Yeah, you know I don’t have knowledge of health, otherwise I have heard about it”.
3.4. Attitudes and Views Regarding HPV Vaccination
“…they still need to be educated because the information they have is still low”.
“…am not quite sure if it can work, because I have heard many controversies about it. There have been uncertainties of whether it can actually work”.
“…it doesn’t relate to the boys or do they also have ovaries”.
“…it something that they cannot get because maybe they don’t have a uterus”.
“…they rejected and sent false messages that the vaccines are for family planning and it would affect their children in many ways”.
“…yes, some said they do not want to be injected. Others said, the vaccine spoils the womb of girls”.
“…so far I myself also, have fear of unknown. What if you’re taking it as a prevention then eventually you come into contact with cervical cancer as a result of you being vaccinated and then you get cervical cancer then what would be the repercussion of this vaccine, Is it 100 effective?”.
“…Yes. I have fear because, as a parent, I am at risk of getting the cancer, and my baby is also at risk of getting this cancer”.
“…Some said they were scared. Others when their turn to be injected came, they moved backwards”.
“…From the girls who have received the jabs and come for the follow-up vaccination we’ve not yet seen any side effect”.
“…in our community, culture, that is, is the biggest factor that has hindered. Because, they believe, the HPV vaccine, is to limit children, child bearing, that is, as in a child when she is older, they give her the vaccine so that, she does not have more children in the future”.
“…Religious reasons. Some have faith say that no medication to them should be administered right from birth, they should just live like that and only Jesus Christ would save them. Such faith becomes really a challenge to us”.
“…you know mostly the people who are living in this locality are Muslims, family planning is prohibited in the holy Quran that is their perception”.
“…They also say that you are being injected so that you join Illuminati”.
“…maybe after getting the first dose, maybe a parent was misled by someone maybe in the community that don’t repeat this”.
3.5. Practical Recommendations to Improve HPV Vaccination Compliance
“…the students were called and they were told to bring their parents and their parents were talked to and they were given consent forms to sign which there are others that refused.”
“…Before the COVID we had already arranged to go to certain schools so that we can give them there.”
“…the COVID pandemic drew us back again because when we were in top gear trying to do dissemination of information that’s when lockdowns came in, people are basically afraid to come to the hospitals”.
“…it would be good for the community to be sensitized so that they know the importance of the vaccine”.
“…the government make it compulsory for every child to receive this vaccination. So if after policy is in place it will be everybody abide by it to make sure that the child is given this vaccination”.
“…We will also like to involve the politicians, the spiritual leaders because they are the people who influence most of the peoples’ decisions, so if we involve them at least to create a positive impact when it comes to the vaccination and also if the ministry of education works together with the ministry of health to ensure that each and every girl gets the jab; at least no girl is left behind”.
4. Discussion
4.1. Summary of Major Findings
4.2. Integration with Prior Work, Implications, Transferability and Contribution to the Field
4.3. Implications
4.4. Limitation
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Arbyn, M.; Xu, L.; Simoens, C.; Martin-Hirsch, P.P.L. Prophylactic vaccination against human papillomaviruses to prevent cervical cancer and its precursors. Cochrane Database Syst. Rev. 2018, 5, CD009069. [Google Scholar] [CrossRef] [PubMed]
- WHO. Human Papillomavirus (HPV) and Cervical Cancer. Available online: https://www.who.int/news-room/fact-sheets/detail/human-papillomavirus-(hpv)-and-cervical-cancer#:~:text=Cervical%20cancer%20is%20caused%20by,%2C%20vagina%2C%20penis%20and%20oropharynx (accessed on 14 July 2020).
- Bruni, L.A.G.; Serrano, B.; Mena, M.; Gómez, D.; Muñoz, J.; Bosch, F.X.; de Sanjosé, S. ICO/IARC Information centre on HPV and cancer (HPV information centre). In Human Papillomavirus and Related Diseases in Africa. Summary Report; Institut Català d’Oncologia: Barcelona, Spain, 2019. [Google Scholar]
- Ogembo, R.K.; Gona, P.N.; Seymour, A.J.; Park, H.S.-M.; Bain, P.A.; Maranda, L.; Ogembo, J.G. Prevalence of human papillomavirus genotypes among African women with normal cervical cytology and neoplasia: A systematic review and meta-analysis. PLoS ONE 2015, 10, e0122488. [Google Scholar] [CrossRef]
- Adams, M.; Jasani, B.; Fiander, A. Prophylactic HPV vaccination for women over 18 years of age. Vaccine 2009, 27, 3391–3394. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. Comprehensive Cervical Cancer Control: A Guide to Essential Practice; World Health Organization: Geneva, Switzerland, 2014; ISBN 978-92415489532014. [Google Scholar]
- Stanley, M. HPV vaccination in boys and men. Hum. Vaccin. Immunother. 2014, 10, 2109–2111. [Google Scholar] [CrossRef] [PubMed]
- Datta, S.; Pink, J.; Medley, G.F.; Petrou, S.; Staniszewska, S.; Underwood, M.; Sonnenberg, P.; Keeling, M.J. Assessing the cost-effectiveness of HPV vaccination strategies for adolescent girls and boys in the UK. BMC Infect. Dis. 2019, 19, 552. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jedy-Agba, E.; Joko, W.Y.; Liu, B.; Buziba, N.G.; Borok, M.; Korir, A.; Masamba, L.; Manraj, S.S.; Finesse, A.; Wabinga, H.; et al. Trends in cervical cancer incidence in Sub-Saharan Africa. Br. J. Cancer 2020, 123, 148–154. [Google Scholar] [CrossRef]
- Hopkins, T.G.; Wood, N. Female human papillomavirus (HPV) vaccination: Global uptake and the impact of attitudes. Vaccine 2013, 31, 1673–1679. [Google Scholar] [CrossRef]
- Patel, H.; Wilson, E.; Vizzotti, C.; Parston, G.; Prestt, J.; Darzi, A. Argentina’s successful implementation of a national human papillomavirus vaccination program. Health Aff. 2016, 35, 301–308. [Google Scholar] [CrossRef]
- Patel, C.; Brotherton, J.M.; Pillsbury, A.; Jayasinghe, S.; Donovan, B.; Macartney, K.; Marshall, H. The impact of 10 years of human papillomavirus (HPV) vaccination in Australia: What additional disease burden will a nonavalent vaccine prevent? Eur. Surveill. 2018, 23, 1700737. [Google Scholar] [CrossRef]
- Brotherton, J.M.L. Impact of HPV vaccination: Achievements and future challenges. Papillomavirus Res. 2019, 7, 138–140. [Google Scholar] [CrossRef]
- Brisson, M.; Kim, J.J.; Canfell, K.; Drolet, M.; Gingras, G.; Burger, E.A.; Martin, D.; Simms, K.T.; Bénard, É.; Boily, M.-C.; et al. Impact of HPV vaccination and cervical screening on cervical cancer elimination: A comparative modelling analysis in 78 low-income and lower-middle-income countries. Lancet 2020, 395, 575–590. [Google Scholar] [CrossRef] [Green Version]
- Gallagher, K.E.; LaMontagne, D.S.; Watson-Jones, D. Status of HPV vaccine introduction and barriers to country uptake. Vaccine 2018, 36, 4761–4767. [Google Scholar] [CrossRef]
- Jindal, H.A.; Kaur, A.; Murugan, S. Human papilloma virus vaccine for low and middle income countries: A step too soon? Hum. Vaccin Immunother. 2017, 13, 2723–2725. [Google Scholar] [CrossRef]
- Gallagher, K.E.; Howard, N.; Kabakama, S.; Mounier-Jack, S.; Burchett, H.E.D.; LaMontagne, D.S.; Watson-Jones, D. Human papillomavirus (HPV) vaccine coverage achievements in low and middle-income countries 2007–2016. Papillomavirus Res. 2017, 4, 72–78. [Google Scholar] [CrossRef] [PubMed]
- LaMontagne, D.S.; Bloem, P.J.N.; Brotherton, J.M.L.; Gallagher, K.E.; Badiane, O.; Ndiaye, C. Progress in HPV vaccination in low- and lower-middle-income countries. Int. J. Gynecol. Obstet. 2017, 138, 7–14. [Google Scholar] [CrossRef] [Green Version]
- Téguété, I.; Dolo, A.; Sangare, K.; Sissoko, A.; Rochas, M.; Beseme, S.; Tounkara, K.; Yekta, S.; De Groot, A.S.; Koita, O.A. Prevalence of HPV 16 and 18 and attitudes toward HPV vaccination trials in patients with cervical cancer in Mali. PLoS ONE 2017, 12, e0172661. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- The Global Cancer Observatory. Kenya. Available online: https://gco.iarc.fr/today/data/factsheets/populations/404-kenya-fact-sheets.pdf (accessed on 14 July 2020).
- Bruni, L.A.G.; Serrano, B.; Mena, M.; Gómez, D.; Muñoz, J.; Bosch, F.X.; de Sanjosé, S.; ICO/IARC Information Centre on HPV and Cancer (HPV Information Centre). Human Papillomavirus and Related Diseases in Kenya. Summary Report. 2019. Available online: https://hpvcentre.net/statistics/reports/KEN.pdf (accessed on 14 July 2020).
- Njuguna, D.W.; Mahrouseh, N.; Onisoyonivosekume, D.; Varga, O. National policies to prevent and manage cervical cancer in East African countries: A policy mapping analysis. Cancers 2020, 12, 1520. [Google Scholar] [CrossRef]
- De Vuyst, H.; Alemany, L.; Lacey, C.; Chibwesha, C.J.; Sahasrabuddhe, V.; Banura, C.; Denny, L.; Parham, G.P. The burden of human papillomavirus infections and related diseases in Sub-Saharan Africa. Vaccine 2013, 31 (Suppl. 5), F32–F46. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, X.; Zeng, Q.; Cai, W.; Ruan, W. Trends of cervical cancer at global, regional, and national level: Data from the Global Burden of Disease study 2019. BMC Public Health 2021, 21, 894. [Google Scholar] [CrossRef] [PubMed]
- Nawrat, A.; Study Reveals Impressive Success of Widespread HPV Vaccination. Pharmaceutical Technology. 27 June 2019. Available online: https://www.pharmaceutical-technology.com/news/success-of-hpv-vaccination-high-income-countries/ (accessed on 14 July 2020).
- Sipp, D.; Frazer, I.H.; Rasko, J.E.J. No Vacillation on HPV vaccination. Cell 2018, 172, 1163–1167. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Government of Kenya. Government to Roll Out HPV Vaccine to Prevent Cervical Cancer Next Month. 2019. Available online: https://www.health.go.ke/government-to-roll-out-hpv-vaccine-to-prevent-cervical-cancer-next-month-nairobi-kenya-wednesday-october-2-2019/ (accessed on 18 August 2020).
- World Health Organisation. Major Milestone Reached as 100 Countries Have Introduced HPV Vaccine into National Schedule. 2019. Available online: https://www.who.int/news/item/31-10-2019-major-milestone-reached-as-100-countries-have-introduced-hpv-vaccine-into-national-schedule (accessed on 14 July 2020).
- Global Alliance for Vaccines and Immunizations. Kenya Introduces Cervical Cancer Vaccine Nationally. Available online: https://www.gavi.org/news/media-room/kenya-introduces-cervical-cancer-vaccine-nationally (accessed on 30 June 2021).
- Schiller, J.T.; Castellsagué, X.; Garland, S.M. A review of clinical trials of human papillomavirus prophylactic vaccines. Vaccine 2012, 30 (Suppl. 5), F123–F138. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garland, S.M.; Steben, M.; Sings, H.L.; James, M.; Lu, S.; Railkar, R.; Barr, E.; Haupt, R.M.; Joura, E.A. Natural history of genital warts: Analysis of the placebo arm of 2 randomized phase III trials of a quadrivalent human papillomavirus (types 6, 11, 16, and 18) vaccine. J. Infect. Dis. 2009, 199, 805–814. [Google Scholar] [CrossRef]
- Bastani, R.; Glenn, B.A.; Tsui, J.; Chang, L.C.; Marchand, E.J.; Taylor, V.M.; Singhal, R. Understanding suboptimal human papillomavirus vaccine uptake among ethnic minority girls. Cancer Epidemiol. Biomark. Prev. 2011, 20, 1463. [Google Scholar] [CrossRef] [Green Version]
- Loke, A.Y.; Kwan, M.L.; Wong, Y.-T.; Wong, A.K.Y. The uptake of human papillomavirus vaccination and its associated factors among adolescents: A systematic review. J. Prim. Care Community Health 2017, 8, 349–362. [Google Scholar] [CrossRef]
- Nabirye, J.; Okwi, L.A.; Nuwematsiko, R.; Kiwanuka, G.; Muneza, F.; Kamya, C.; Babirye, J.N. Health system factors influencing uptake of Human Papilloma Virus (HPV) vaccine among adolescent girls 9–15 years in Mbale District, Uganda. BMC Public Health 2020, 20, 171. [Google Scholar] [CrossRef] [Green Version]
- Anderson, E.L. Recommended solutions to the barriers to immunization in children and adults. Mo. Med. 2014, 111, 344–348. [Google Scholar]
- Masika, M.M.; Ogembo, J.G.; Chabeda, S.V.; Wamai, R.G.; Mugo, N. Knowledge on HPV vaccine and cervical cancer facilitates vaccine acceptability among school teachers in Kitui county, Kenya. PLoS ONE 2015, 10, e0135563. [Google Scholar] [CrossRef] [PubMed]
- Mburu, A.; Itsura, P.; Mabeya, H.; Kaaria, A.; Brown, D.R. Knowledge of cervical cancer and acceptability of prevention strategies among human papillomavirus-vaccinated and human papillomavirus-unvaccinated adolescent women in Eldoret, Kenya. BioRes. Open Access 2019, 8, 139–145. [Google Scholar] [CrossRef] [Green Version]
- Deignan, C.; Swartz, A.; Cooper, S.; Colvin, C.J. Stakeholders’ understandings of human papillomavirus (HPV) vaccination in Sub-Saharan Africa: A rapid qualitative systematic review. Vaccines 2021, 9, 496. [Google Scholar] [CrossRef] [PubMed]
- Kimmel, S.R. Practical implementation of HPV vaccines in clinical practice. J. Fam. Pract. 2006, 55, S18–S22. [Google Scholar]
- Becker-Dreps, S.; Otieno, W.A.; Brewer, N.T.; Agot, K.; Smith, J.S. HPV vaccine acceptability among Kenyan women. Vaccine 2010, 28, 4864–4867. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mabeya, H.; Odunga, J.; Broeck, D.V. Mothers of adolescent girls and Human Papilloma Virus (HPV) vaccination in Western Kenya. Pan. Afr. Med. J. 2021, 38, 126. [Google Scholar] [CrossRef]
- Turiho, A.K.; Okello, E.S.; Muhwezi, W.W.; Katahoire, A.R. Perceptions of human papillomavirus vaccination of adolescent schoolgirls in western Uganda and their implications for acceptability of HPV vaccination: A qualitative study. BMC Res. Notes 2017, 10, 431. [Google Scholar] [CrossRef]
- Kenya National Bureau of Statistics. Gross County Product. Available online: https://www.knbs.or.ke/?wpdmpro=gross-county-product-2019 (accessed on 19 August 2021).
- National Drought Management Authority. Drought Early Warning Bulletin. Available online: https://reliefweb.int/sites/reliefweb.int/files/resources/Tana%20River%20May%202021.pdf (accessed on 7 August 2021).
- Bosire, J.; Celliers, L.; Groeneveld, J.; Paula, J.; Schleyer, M.H. Regional State of the Coast Report—Western Indian Ocean. 2015. Available online: https://wedocs.unep.org/handle/20.500.11822/9700. (accessed on 20 August 2021).
- O’Brien, B.C.; Harris, I.B.; Beckman, T.J.; Reed, D.A.; Cook, D.A. Standards for reporting qualitative research: A synthesis of recommendations. Acad. Med. 2014, 89, 1245–1251. [Google Scholar] [CrossRef] [PubMed]
- McHugh, M.L. Interrater reliability: The kappa statistic. Biochem. Med. 2012, 22, 276–282. [Google Scholar] [CrossRef]
- Yamaguchi, M.; Sekine, M.; Hanley, S.J.B.; Kudo, R.; Hara, M.; Adachi, S.; Ueda, Y.; Miyagi, E.; Enomoto, T. Risk factors for HPV infection and high-grade cervical disease in sexually active Japanese women. Sci. Rep. 2021, 11, 2898. [Google Scholar] [CrossRef] [PubMed]
- Cunningham, M.S.; Skrastins, E.; Fitzpatrick, R.; Jindal, P.; Oneko, O.; Yeates, K.; Booth, C.M.; Carpenter, J.; Aronson, K.J. Cervical cancer screening and HPV vaccine acceptability among rural and urban women in Kilimanjaro Region, Tanzania. BMJ Open 2015, 5, e005828. [Google Scholar] [CrossRef] [Green Version]
- Wigle, J.; Coast, E.; Watson-Jones, D. Human papillomavirus (HPV) vaccine implementation in low and middle-income countries (LMICs): Health system experiences and prospects. Vaccine 2013, 31, 3811–3817. [Google Scholar] [CrossRef] [Green Version]
- Ogembo, J.G.; Manga, S.; Nulah, K.; Foglabenchi, L.H.; Perlman, S.; Wamai, R.G.; Welty, T.; Welty, E.; Tih, P. Achieving high uptake of human papillomavirus vaccine in Cameroon: Lessons learned in overcoming challenges. Vaccine 2014, 32, 4399–4403. [Google Scholar] [CrossRef]
- Cordoba-Sanchez, V.; Tovar-Aguirre, O.L.; Franco, S.; Arias Ortiz, N.E.; Louie, K.; Sanchez, G.I.; Garces-Palacio, I.C. Perception about barriers and facilitators of the school-based HPV vaccine program of Manizales, Colombia: A qualitative study in school-enrolled girls and their parents. Prev. Med. Rep. 2019, 16, 100977. [Google Scholar] [CrossRef]
- Bednarczyk, R.A. Addressing HPV vaccine myths: Practical information for healthcare providers. Hum. Vaccin. Immunother. 2019, 15, 1628–1638. [Google Scholar] [CrossRef]
- Otieno, N.A.; Malik, F.A.; Nganga, S.W.; Wairimu, W.N.; Ouma, D.O.; Bigogo, G.M.; Chaves, S.S.; Verani, J.R.; Widdowson, M.-A.; Wilson, A.D.; et al. Decision-making process for introduction of maternal vaccines in Kenya, 2017–2018. Implement. Sci. 2021, 16, 39. [Google Scholar] [CrossRef]
- Bigaard, J.; Franceschi, S. Vaccination against HPV: Boosting coverage and tackling misinformation. Mol. Oncol. 2021, 15, 770–778. [Google Scholar] [CrossRef]
- Grandahl, M.; Nevéus, T.; Dalianis, T.; Larsson, M.; Tydén, T.; Stenhammar, C. ‘I also want to be vaccinated!’—Adolescent boys’ awareness and thoughts, perceived benefits, information sources, and intention to be vaccinated against Human papillomavirus (HPV). Hum. Vaccin Immunother. 2019, 15, 1794–1802. [Google Scholar] [CrossRef] [PubMed]
- Otieno, N.A.; Otiato, F.; Nyawanda, B.; Adero, M.; Wairimu, W.N.; Ouma, D.; Atito, R.; Wilson, A.; Gonzalez-Casanova, I.; Malik, F.A.; et al. Drivers and barriers of vaccine acceptance among pregnant women in Kenya. Hum. Vaccin Immunother. 2020, 16, 2429–2437. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yoon, D.; Lee, J.-H.; Lee, H.; Shin, J.-Y. Association between human papillomavirus vaccination and serious adverse events in South Korean adolescent girls: Nationwide cohort study. BMJ 2021, 372, m4931. [Google Scholar] [CrossRef] [PubMed]
- Zimet, G.D.; Rosberger, Z.; Fisher, W.A.; Perez, S.; Stupiansky, N.W. Beliefs, behaviors and HPV vaccine: Correcting the myths and the misinformation. Prev. Med. 2013, 57, 414–418. [Google Scholar] [CrossRef] [Green Version]
- Masterson, L.; Lechner, M. HPV vaccination in boys—Will the UK join the fight? Nat. Rev. Clin. Oncol. 2016, 13, 721–722. [Google Scholar] [CrossRef]
- Lindley, M.C.; Jeyarajah, J.; Yankey, D.; Curtis, C.R.; Markowitz, L.E.; Stokley, S. Comparing human papillomavirus vaccine knowledge and intentions among parents of boys and girls. Hum. Vaccin Immunother. 2016, 12, 1519–1527. [Google Scholar] [CrossRef] [Green Version]
- Prue, G.; Grimes, D.; Baker, P.; Lawler, M. Access to HPV vaccination for boys in the United Kingdom. Med. Access Point Care 2018, 2, 2399202618799691. [Google Scholar] [CrossRef]
- Elfström, K.M.; Lazzarato, F.; Franceschi, S.; Dillner, J.; Baussano, I. Human papillomavirus vaccination of boys and extended catch-up vaccination: Effects on the resilience of programs. J. Infect. Dis. 2015, 213, 199–205. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vamos, C.A.; McDermott, R.J.; Daley, E.M. The HPV Vaccine: Framing the arguments FOR and AGAINST mandatory vaccination of all middle school girls. J. Sch. Health 2008, 78, 302–309. [Google Scholar] [CrossRef] [PubMed]
- Katz, I.T.; Nkala, B.; Dietrich, J.; Wallace, M.; Bekker, L.-G.; Pollenz, K.; Bogart, L.M.; Wright, A.A.; Tsai, A.C.; Bangsberg, D.R.; et al. A qualitative analysis of factors influencing HPV vaccine uptake in Soweto, South Africa among adolescents and their caregivers. PLoS ONE 2013, 8, e72094. [Google Scholar] [CrossRef] [Green Version]
- Walker, K.K.; Head, K.J.; Owens, H.; Zimet, G.D. A qualitative study exploring the relationship between mothers’ vaccine hesitancy and health beliefs with COVID-19 vaccination intention and prevention during the early pandemic months. Hum. Vaccines Immunother. 2021, 17, 3355–3364. [Google Scholar] [CrossRef]
- Arbyn, M.; Gultekin, M.; Morice, P.; Nieminen, P.; Cruickshank, M.; Poortmans, P.; Kelly, D.; Poljak, M.; Bergeron, C.; Ritchie, D.; et al. The European response to the WHO call to eliminate cervical cancer as a public health problem. Int. J. Cancer 2021, 148, 277–284. [Google Scholar] [CrossRef] [PubMed]
- Daniels, V.; Saxena, K.; Roberts, C.; Kothari, S.; Corman, S.; Yao, L.; Niccolai, L. Impact of reduced human papillomavirus vaccination coverage rates due to COVID-19 in the United States: A model based analysis. Vaccine 2021, 39, 2731–2735. [Google Scholar] [CrossRef]
| Absence of Actual Side Effects | Birth Control Misconceptions | Fear of the Unknown | |
|---|---|---|---|
| Parents | 6% (6/10) | 45% (10/10) | 49% (7/10) |
| Health workers | 16% (10/21) | 51% (7/21 | 34% (7/21) |
| Head teachers | 22% (20/23) | 64% (14/23) | 14% (5/23) |
| Community leaders | 8% (20/22) | 64% (16/22) | 28% (11/22) |
| Children | 59% (10/26) | 28% (3/26) | 13% (1/26) |
| Tana-River County | 13% (35/50) | 74% (26/50) | 13% (6/50) |
| Mombasa County | 14% (41/52) | 50% (32/52) | 36% (27/52) |
| Neutral | Opposing | Supportive | |
|---|---|---|---|
| Children | 14% (5/36) | 19% (7/36) | 78% (28/36) |
| Community leaders | 27% (6/22) | 23% (5/22) | 82% (18/22) |
| Community members | 21% (14/67) | 79% (53/67) | 39% (26/67) |
| Healthcare workers | 26% (10/38) | 39% (15/38) | 82% (31/38) |
| Media | 0% | 17% (2/12) | 67% (8/12) |
| Parents’ opinions | 12% (8/66) | 71% (47/66) | 52% (34/66) |
| Teachers | 13% (3/23) | 4% (1/23) | 83% (19/23) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Njuguna, D.W.; Mahrouseh, N.; Isowamwen, O.V.; Varga, O. Knowledge, Attitude and Practice of Main Stakeholders towards Human Papilloma Virus Infection and Vaccination in Mombasa and Tana-River Counties in Kenya: A Qualitative Study. Vaccines 2021, 9, 1099. https://doi.org/10.3390/vaccines9101099
Njuguna DW, Mahrouseh N, Isowamwen OV, Varga O. Knowledge, Attitude and Practice of Main Stakeholders towards Human Papilloma Virus Infection and Vaccination in Mombasa and Tana-River Counties in Kenya: A Qualitative Study. Vaccines. 2021; 9(10):1099. https://doi.org/10.3390/vaccines9101099
Chicago/Turabian StyleNjuguna, Diana Wangeshi, Nour Mahrouseh, Osarugue Victory Isowamwen, and Orsolya Varga. 2021. "Knowledge, Attitude and Practice of Main Stakeholders towards Human Papilloma Virus Infection and Vaccination in Mombasa and Tana-River Counties in Kenya: A Qualitative Study" Vaccines 9, no. 10: 1099. https://doi.org/10.3390/vaccines9101099
APA StyleNjuguna, D. W., Mahrouseh, N., Isowamwen, O. V., & Varga, O. (2021). Knowledge, Attitude and Practice of Main Stakeholders towards Human Papilloma Virus Infection and Vaccination in Mombasa and Tana-River Counties in Kenya: A Qualitative Study. Vaccines, 9(10), 1099. https://doi.org/10.3390/vaccines9101099






