Advancements in the Growth and Construction of Recombinant Lumpy Skin Disease Virus (LSDV) for Use as a Vaccine Vector
Abstract
:1. Introduction
2. Materials and Methods
2.1. Antibodies, Plasmids, Cell Lines and Reagents
2.2. Promoter Activity in LSDV
2.3. Generation of Recombinant LSDVGC5 Virus in BHK-21 Cells
2.4. Growth Curve of LSDVGC5 in BHK-21 Cells
2.5. Transgene Expression from MVAGC5 and LSDVGC5 in Non-Permissive Cells Stimulated with the pan-HDAC Inhibitor Sodium Butyrate
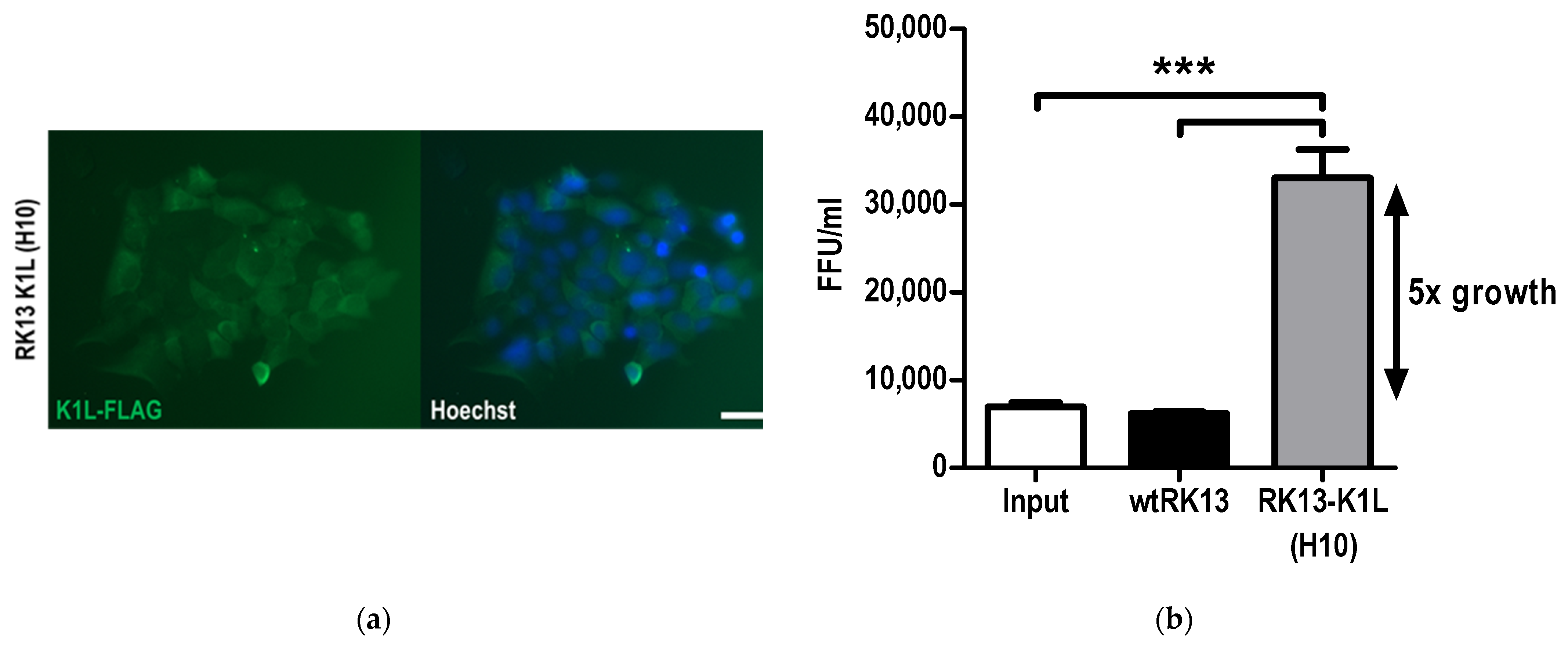
2.6. Generation of RK13 Cells with Stable Expression of VACV K1L
2.7. LSDVGC5 Growth in RK13 Cells
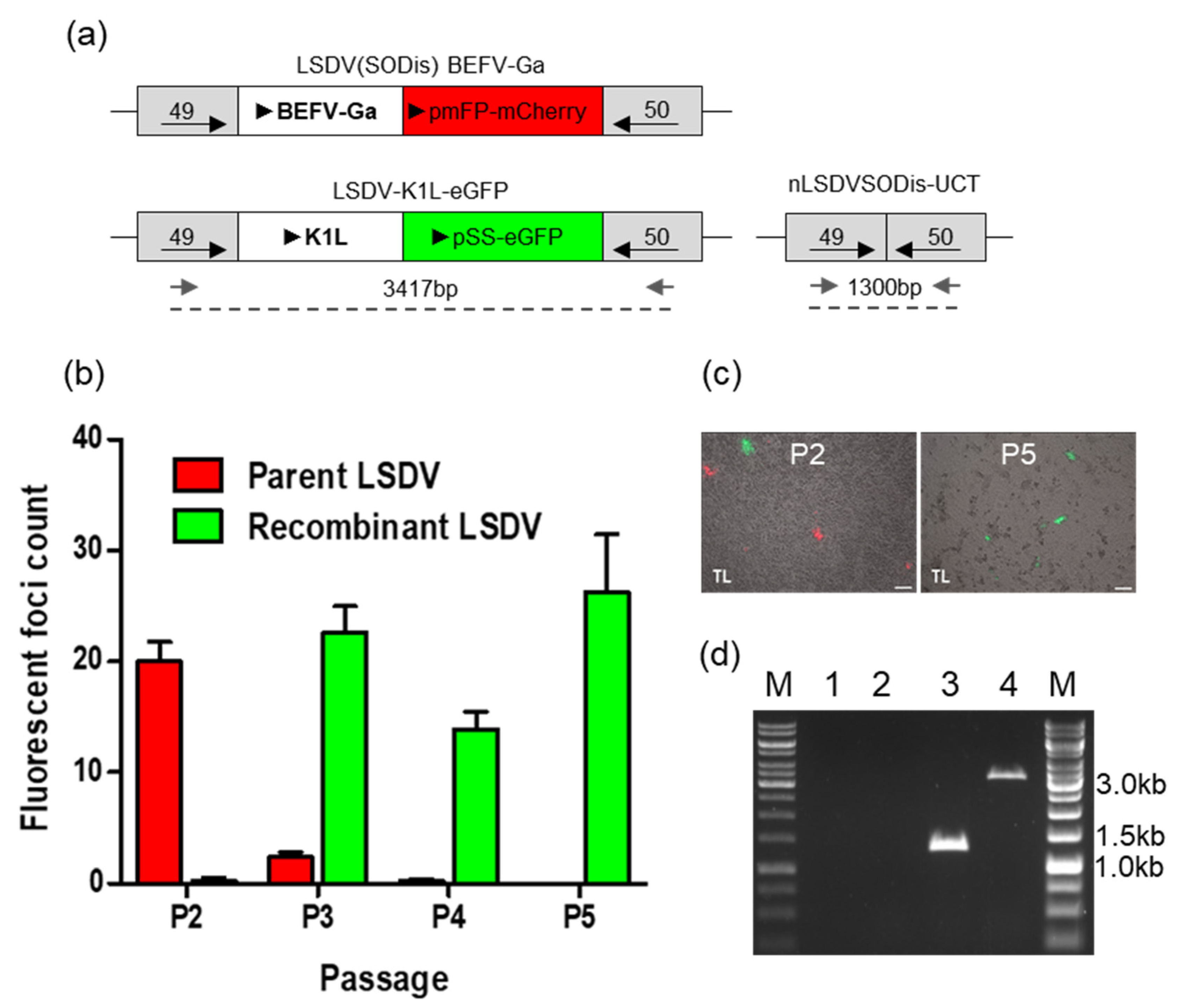
2.8. Generation of LSDV-K1L-eGFP in RK13 Cells
3. Results
3.1. Expression of Foreign Genes by LSDV from Different Promoters
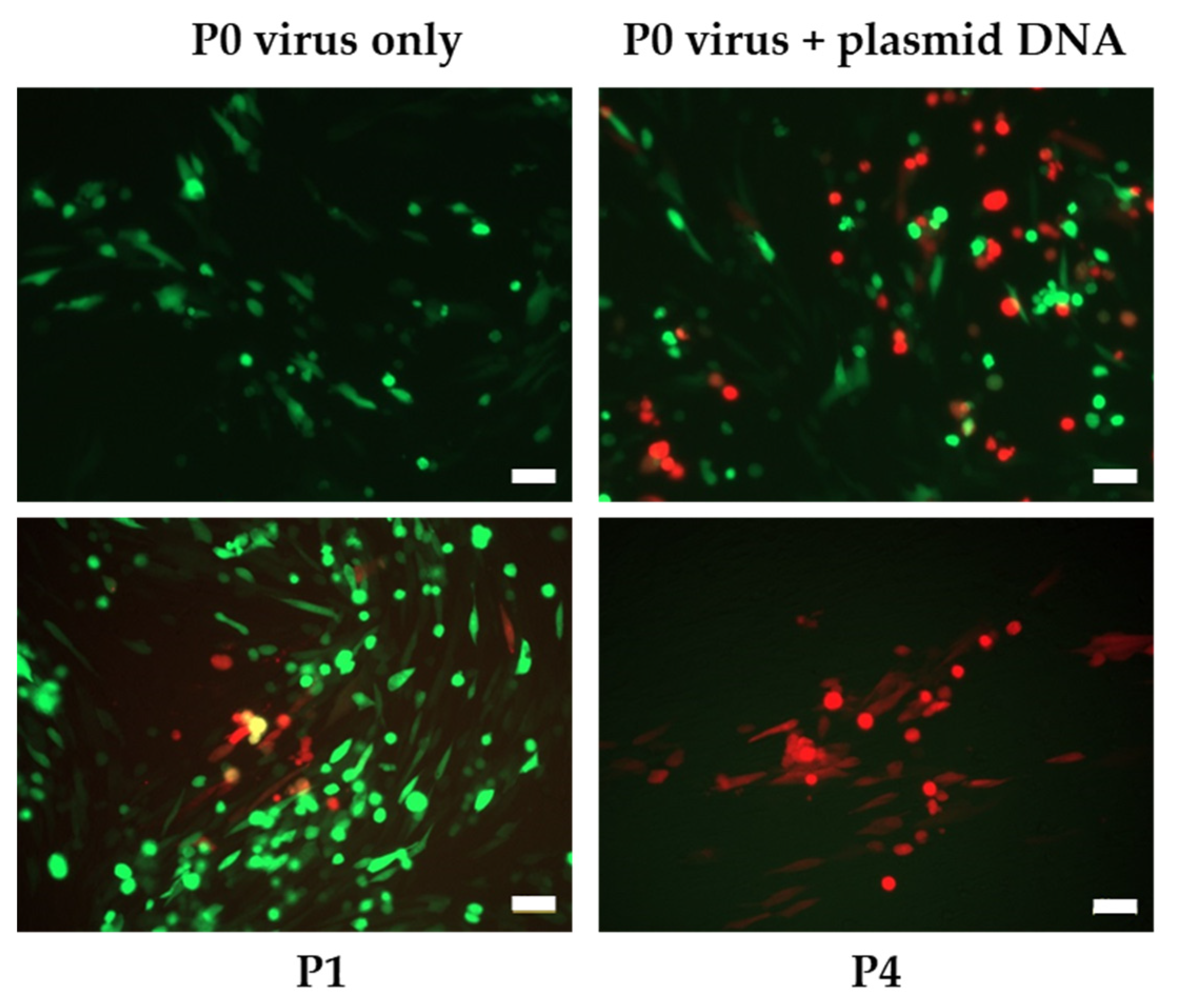
3.2. Construction of Recombinant LSDVGC5 in BHK-21 Cells
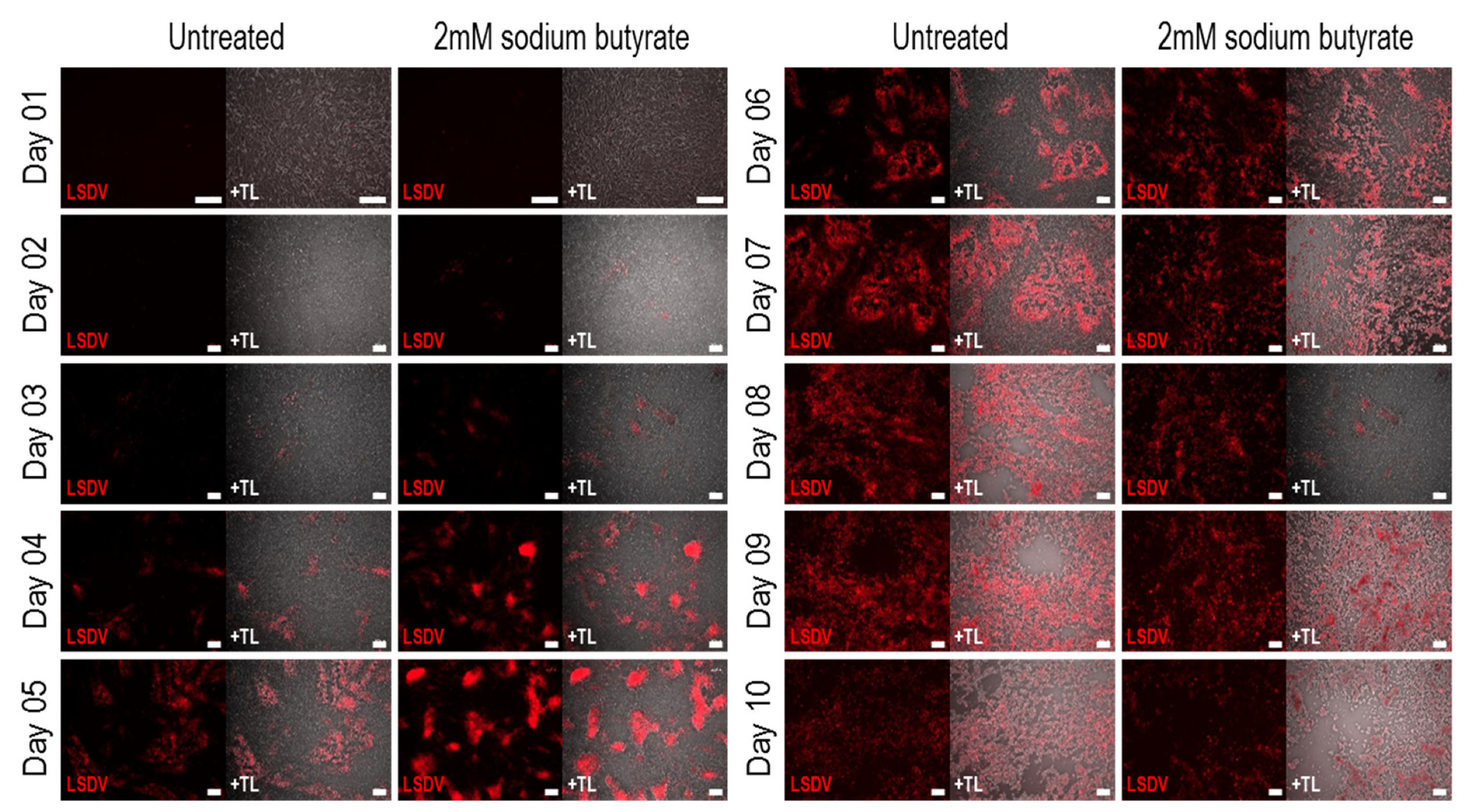
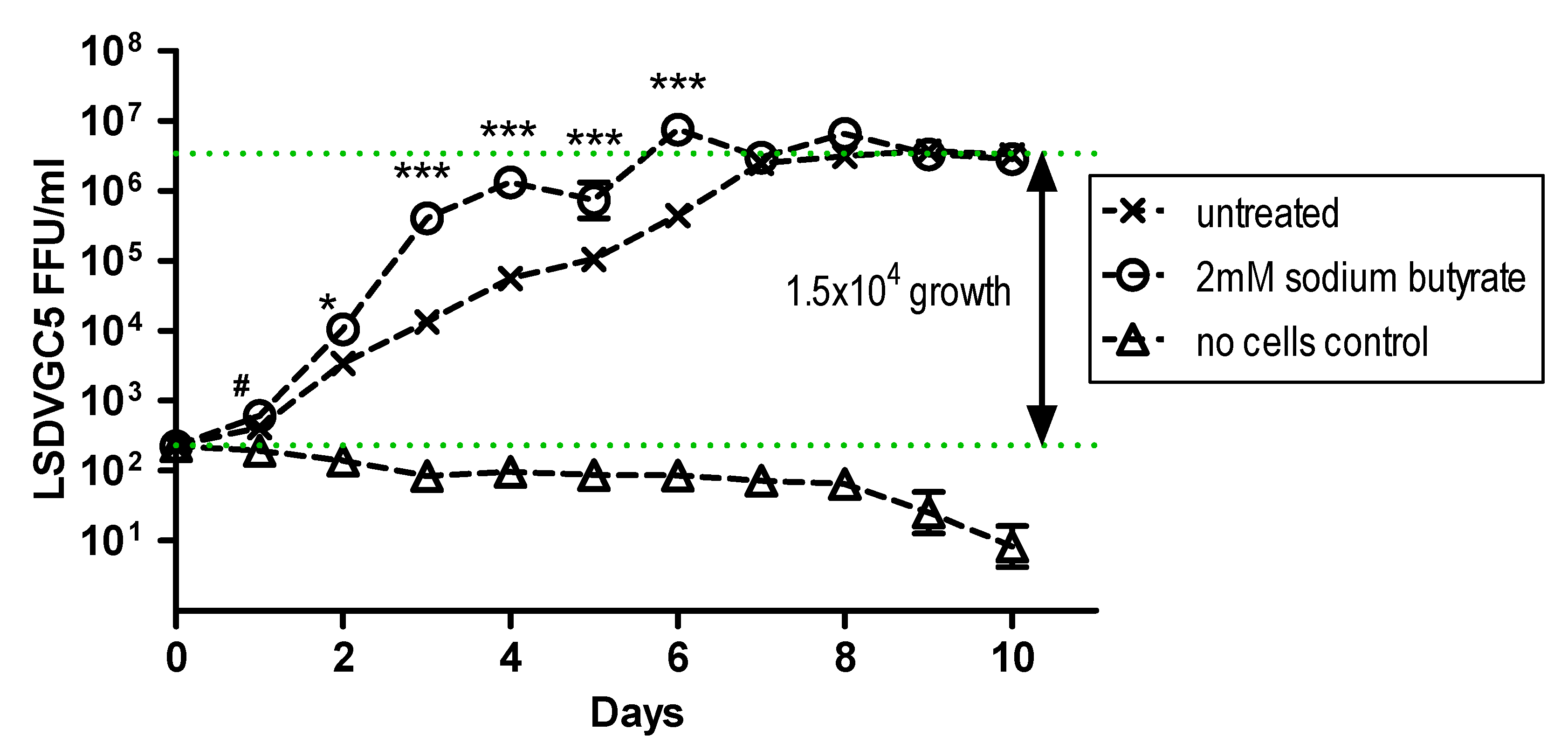
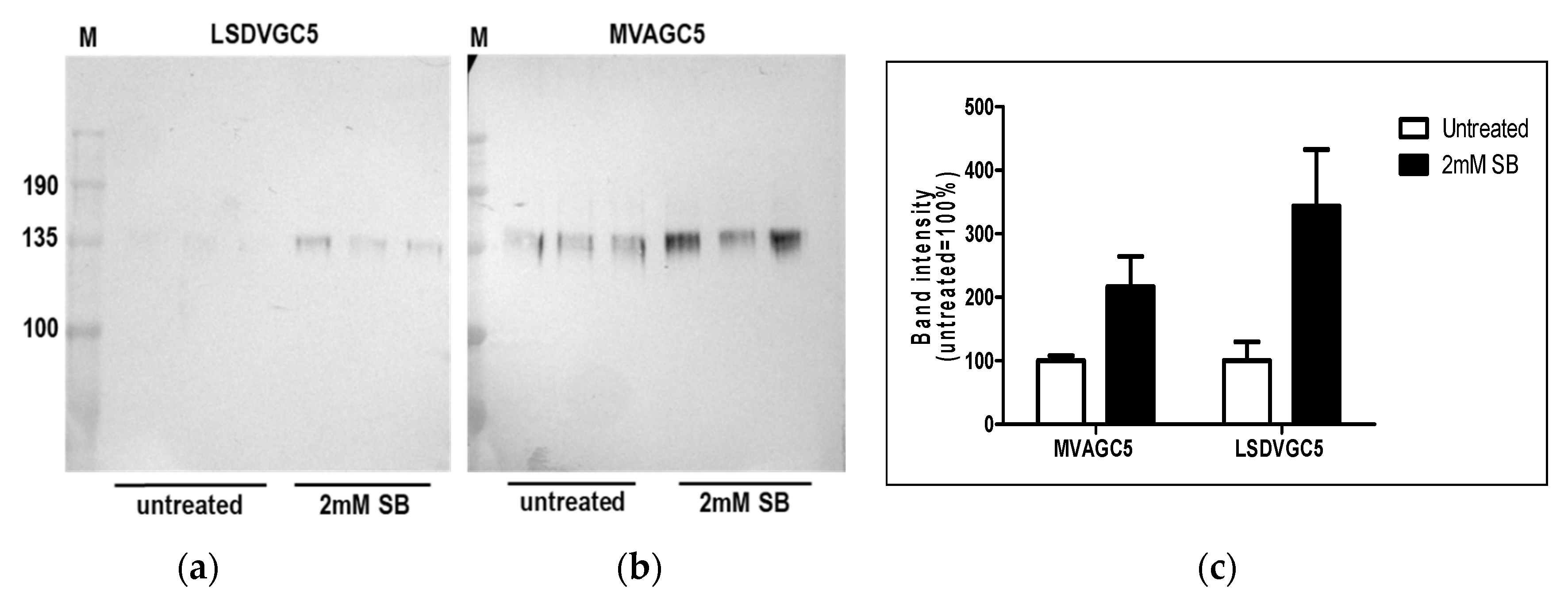
3.3. Evaluation of the Growth of LSDV and Expression of Foreign Genes from LSDV, in BHK Cells, in the Presence and Absence of Sodium Butyrate
3.4. The Use of VACV K1L to Improve Growth of LSDV and Select for Recombinant LSDV
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Tartaglia, J.; Pincus, S.; Paoletti, E. Poxvirus-based vectors as vaccine candidates. Crit Rev. Immunol. 1990, 10, 13–30. [Google Scholar] [PubMed]
- Sanchez-Sampedro, L.; Perdiguero, B.; Mejias-Perez, E.; Garcia-Arriaza, J.; Di Pilato, M.; Esteban, M. The evolution of poxvirus vaccines. Viruses 2015, 7, 1726–1803. [Google Scholar] [CrossRef] [Green Version]
- Taylor, J.; Tartaglia, J.; Riviere, M.; Duret, C.; Languet, B.; Chappuis, G.; Paoletti, E. Applications of canarypox (ALVAC) vectors in human and veterinary vaccination. Dev. Biol. Stand. 1994, 82, 131–135. [Google Scholar]
- Jarrett, O. Efficacy of recombinant feline leukemia virus vaccines. AIDS Res. Hum. Retrovir. 1996, 12, 435–436. [Google Scholar] [CrossRef]
- El-Hage, C.M.; Savage, C.J.; Minke, J.M.; Ficorilli, N.P.; Watson, J.; Gilkerson, J.R. Accelerated vaccination schedule provides protective levels of antibody and complete herd immunity to equine influenza. Equine Vet. J. 2013, 45, 235–239. [Google Scholar] [CrossRef]
- Kim, J.H.; Excler, J.L.; Michael, N.L. Lessons from the RV144 Thai phase III HIV-1 vaccine trial and the search for correlates of protection. Annu. Rev. Med. 2015, 66, 423–437. [Google Scholar] [CrossRef] [Green Version]
- Churchyard, G.; Mlisana, K.; Karuna, S.; Williamson, A.L.; Williamson, C.; Morris, L.; Tomaras, G.D.; De Rosa, S.C.; Gilbert, P.B.; Gu, N.; et al. Sequential Immunization with gp140 boosts immune responses primed by modified vaccinia ankara or DNA in HIV-Uninfected South African participants. PLoS ONE 2016, 11, e0161753. [Google Scholar] [CrossRef] [Green Version]
- Gray, G.E.; Mayer, K.H.; Elizaga, M.L.; Bekker, L.G.; Allen, M.; Morris, L.; Montefiori, D.; De Rosa, S.C.; Sato, A.; Gu, N.; et al. Subtype C gp140 vaccine boosts immune responses primed by the South African AIDS vaccine initiative DNA-C2 and MVA-C HIV Vaccines after More than a 2-Year Gap. Clin. Vaccine Immunol. 2016, 23, 496–506. [Google Scholar] [CrossRef] [Green Version]
- Burgers, W.A.; Ginbot, Z.; Shen, Y.J.; Chege, G.K.; Soares, A.P.; Muller, T.L.; Bunjun, R.; Kiravu, A.; Munyanduki, H.; Douglass, N.; et al. The novel capripoxvirus vector lumpy skin disease virus efficiently boosts modified vaccinia Ankara human immunodeficiency virus responses in rhesus macaques. J. Gen. Virol. 2014, 95, 2267–2272. [Google Scholar] [CrossRef] [PubMed]
- Shen, Y.J.; Shephard, E.; Douglass, N.; Johnston, N.; Adams, C.; Williamson, C.; Williamson, A.L. A novel candidate HIV vaccine vector based on the replication deficient Capripoxvirus, Lumpy skin disease virus (LSDV). Virol. J. 2011, 8, 265. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Volkmann, A.; Williamson, A.L.; Weidenthaler, H.; Meyer, T.P.H.; Robertson, J.S.; Excler, J.L.; Condit, R.C.; Evans, E.; Smith, E.R.; Kim, D.; et al. The Brighton Collaboration standardized template for collection of key information for risk/benefit assessment of a Modified Vaccinia Ankara (MVA) vaccine platform. Vaccine 2021, 39, 3067–3080. [Google Scholar] [CrossRef]
- Teigler, J.E.; Phogat, S.; Franchini, G.; Hirsch, V.M.; Michael, N.L.; Barouch, D.H. The canarypox virus vector ALVAC induces distinct cytokine responses compared to the vaccinia virus-based vectors MVA and NYVAC in rhesus monkeys. J. Virol. 2014, 88, 1809–1814. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Santra, S.; Sun, Y.; Parvani, J.G.; Philippon, V.; Wyand, M.S.; Manson, K.; Gomez-Yafal, A.; Mazzara, G.; Panicali, D.; Markham, P.D.; et al. Heterologous prime/boost immunization of rhesus monkeys by using diverse poxvirus vectors. J. Virol. 2007, 81, 8563–8570. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kitching, R.P. Vaccines for lumpy skin disease, sheep pox and goat pox. Dev. Biol. 2003, 114, 161–167. [Google Scholar]
- Haegeman, A.; De Leeuw, I.; Mostin, L.; Campe, W.V.; Aerts, L.; Venter, E.; Tuppurainen, E.; Saegerman, C.; De Clercq, K. Comparative evaluation of lumpy skin disease virus-based live attenuated vaccines. Vaccines 2021, 9, 473. [Google Scholar] [CrossRef] [PubMed]
- Hamdi, J.; Boumart, Z.; Daouam, S.; El Arkam, A.; Bamouh, Z.; Jazouli, M.; Tadlaoui, K.O.; Fihri, O.F.; Gavrilov, B.; El Harrak, M. Development and evaluation of an inactivated lumpy skin disease vaccine for cattle. Vet. Microbiol. 2020, 245, 108689. [Google Scholar] [CrossRef]
- Aspden, K.; van Dijk, A.A.; Bingham, J.; Cox, D.; Passmore, J.A.; Williamson, A.L. Immunogenicity of a recombinant lumpy skin disease virus (neethling vaccine strain) expressing the rabies virus glycoprotein in cattle. Vaccine 2002, 20, 2693–2701. [Google Scholar] [CrossRef]
- Wallace, D.B.; Mather, A.; Kara, P.D.; Naicker, L.; Mokoena, N.B.; Pretorius, A.; Nefefe, T.; Thema, N.; Babiuk, S. Protection of cattle elicited using a bivalent lumpy skin disease virus-vectored recombinant rift valley fever vaccine. Front. Vet. Sci. 2020, 7, 256. [Google Scholar] [CrossRef]
- Aspden, K.; Passmore, J.A.; Tiedt, F.; Williamson, A.L. Evaluation of lumpy skin disease virus, a capripoxvirus, as a replication-deficient vaccine vector. J. Gen. Virol. 2003, 84, 1985–1996. [Google Scholar] [CrossRef]
- Liu, F.; Zhang, H.; Liu, W. Construction of recombinant capripoxviruses as vaccine vectors for delivering foreign antigens: Methodology and application. Comp. Immunol. Microbiol. Infect. Dis. 2019, 65, 181–188. [Google Scholar] [CrossRef]
- Rhazi, H.; Safini, N.; Mikou, K.; Alhyane, M.; Lenk, M.; Tadlaoui, K.O.; Elharrak, M. Comparative sensitivity study of primary cells, vero, OA3.Ts and ESH-L cell lines to lumpy skin disease, sheeppox, and goatpox viruses detection and growth. J. Virol. Methods 2021, 293, 114164. [Google Scholar] [CrossRef]
- Fay, P.C.; Cook, C.G.; Wijesiriwardana, N.; Tore, G.; Comtet, L.; Carpentier, A.; Shih, B.; Freimanis, G.; Haga, I.R.; Beard, P.M. Madin-Darby bovine kidney (MDBK) cells are a suitable cell line for the propagation and study of the bovine poxvirus lumpy skin disease virus. J. Virol. Methods 2020, 285, 113943. [Google Scholar] [CrossRef] [PubMed]
- Munyanduki, H.; Omar, R.; Douglass, N.; Williamson, A.L. Removal of bovine viral diarrhea virus (BVDV) from lumpy skin disease virus (LSDV) vaccine stocks by passage on chorioallantoic membranes of fertilized hens’ eggs. J. Virol. Methods 2020, 275, 113752. [Google Scholar] [CrossRef] [PubMed]
- Soday, L.; Lu, Y.; Albarnaz, J.D.; Davies, C.T.R.; Antrobus, R.; Smith, G.L.; Weekes, M.P. Quantitative temporal proteomic analysis of vaccinia virus infection reveals regulation of histone deacetylases by an interferon antagonist. Cell Rep. 2019, 27, 1920–1933. [Google Scholar] [CrossRef] [Green Version]
- Lu, Y.; Stuart, J.H.; Talbot-Cooper, C.; Agrawal-Singh, S.; Huntly, B.; Smid, A.I.; Snowden, J.S.; Dupont, L.; Smith, G.L. Histone deacetylase 4 promotes type I interferon signaling, restricts DNA viruses, and is degraded via vaccinia virus protein C6. Proc. Natl. Acad. Sci. USA 2019, 116, 11997–12006. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meyer, H.; Sutter, G.; Mayr, A. Mapping of deletions in the genome of the highly attenuated vaccinia virus MVA and their influence on virulence. J. Gen. Virol. 1991, 72, 1031–1038. [Google Scholar] [CrossRef]
- Staib, C.; Drexler, I.; Ohlmann, M.; Wintersperger, S.; Erfle, V.; Sutter, G. Transient host range selection for genetic engineering of modified vaccinia virus Ankara. Biotechniques 2000, 28, 1137–1142, 1144–1146, 1148. [Google Scholar] [CrossRef]
- Willis, K.L.; Langland, J.O.; Shisler, J.L. Viral double-stranded RNAs from vaccinia virus early or intermediate gene transcripts possess PKR activating function, resulting in NF-kappaB activation, when the K1 protein is absent or mutated. J. Biol. Chem. 2011, 286, 7765–7778. [Google Scholar] [CrossRef] [Green Version]
- Shisler, J.L.; Jin, X.L. The vaccinia virus K1L gene product inhibits host NF-kappaB activation by preventing IkappaBalpha degradation. J. Virol. 2004, 78, 3553–3560. [Google Scholar] [CrossRef] [Green Version]
- Bravo Cruz, A.G.; Han, A.; Roy, E.J.; Guzman, A.B.; Miller, R.J.; Driskell, E.A.; O’Brien, W.D., Jr.; Shisler, J.L. Deletion of the K1L gene results in a vaccinia virus that is less pathogenic due to muted innate immune responses, yet still elicits protective immunity. J. Virol. 2017, 91, e00542-17. [Google Scholar] [CrossRef] [Green Version]
- Sutter, G.; Ramsey-Ewing, A.; Rosales, R.; Moss, B. Stable expression of the vaccinia virus K1L gene in rabbit cells complements the host range defect of a vaccinia virus mutant. J. Virol. 1994, 68, 4109–4116. [Google Scholar] [CrossRef] [Green Version]
- Tulman, E.R.; Afonso, C.L.; Lu, Z.; Zsak, L.; Kutish, G.F.; Rock, D.L. Genome of lumpy skin disease virus. J. Virol. 2001, 75, 7122–7130. [Google Scholar] [CrossRef] [Green Version]
- Tanzer, F.L.; Shephard, E.G.; Palmer, K.E.; Burger, M.; Williamson, A.L.; Rybicki, E.P. The porcine circovirus type 1 capsid gene promoter improves antigen expression and immunogenicity in a HIV-1 plasmid vaccine. Virol. J. 2011, 8, 51. [Google Scholar] [CrossRef] [Green Version]
- Douglass, N.; Munyanduki, H.; Omar, R.; Gers, S.; Mutowembwa, P.; Heath, L.; Williamson, A.L. Influence of the Viral Superoxide Dismutase (SOD) Homologue on Lumpy Skin Disease Virus (LSDV) Growth, Histopathology and Pathogenicity. Vaccines 2020, 8, 664. [Google Scholar] [CrossRef] [PubMed]
- van Diepen, M.T.; Chapman, R.; Douglass, N.; Galant, S.; Moore, P.L.; Margolin, E.; Ximba, P.; Morris, L.; Rybicki, E.P.; Williamson, A.L. Prime-boost immunizations with DNA, modified vaccinia virus ankara, and protein-based vaccines elicit robust HIV-1 Tier 2 neutralizing antibodies against the CAP256 superinfecting virus. J. Virol. 2019, 93, e02155-18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chakrabarti, S.; Sisler, J.R.; Moss, B. Compact, synthetic, vaccinia virus early/late promoter for protein expression. Biotechniques 1997, 23, 1094–1097. [Google Scholar] [CrossRef]
- Di Pilato, M.; Mejias-Perez, E.; Gomez, C.E.; Perdiguero, B.; Sorzano, C.O.; Esteban, M. New vaccinia virus promoter as a potential candidate for future vaccines. J. Gen. Virol. 2013, 94, 2771–2776. [Google Scholar] [CrossRef] [Green Version]
- Omar, R. Comparison of the Two Lumpy Skin Disease Virus Vaccines, Neethling and Herbivac, and Construction of a Recombinant Herbivac-Rift Valley Fever Virus Vaccine. Master’s dgree, University of Cape Town, Cape Town, South Africa, 2015. [Google Scholar]
- Kumar, S.; Boyle, D.B. A poxvirus bidirectional promoter element with early/late and late functions. Virology 1990, 179, 151–158. [Google Scholar] [CrossRef]
- Cochran, M.A.; Puckett, C.; Moss, B. In vitro mutagenesis of the promoter region for a vaccinia virus gene: Evidence for tandem early and late regulatory signals. J. Virol. 1985, 54, 30–37. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wyatt, L.S.; Shors, S.T.; Murphy, B.R.; Moss, B. Development of a replication-deficient recombinant vaccinia virus vaccine effective against parainfluenza virus 3 infection in an animal model. Vaccine 1996, 14, 1451–1458. [Google Scholar] [CrossRef]
- Alharbi, N.K. Poxviral promoters for improving the immunogenicity of MVA delivered vaccines. Hum. Vaccin Immunother 2019, 15, 203–209. [Google Scholar] [CrossRef] [Green Version]
- Moss, B. Reflections on the early development of poxvirus vectors. Vaccine 2013, 31, 4220–4222. [Google Scholar] [CrossRef] [Green Version]
- Okeke, M.I.; Okoli, A.S.; Diaz, D.; Offor, C.; Oludotun, T.G.; Tryland, M.; Bohn, T.; Moens, U. Hazard characterization of modified vaccinia virus ankara vector: What are the knowledge gaps? Viruses 2017, 9, 318. [Google Scholar] [CrossRef] [Green Version]
- Pinschewer, D.D. Virally vectored vaccine delivery: Medical needs, mechanisms, advantages and challenges. Swiss Med. Wkly. 2017, 147, w14465. [Google Scholar] [CrossRef] [Green Version]
- Prow, N.A.; Jimenez Martinez, R.; Hayball, J.D.; Howley, P.M.; Suhrbier, A. Poxvirus-based vector systems and the potential for multi-valent and multi-pathogen vaccines. Expert Rev. Vaccines 2018, 17, 925–934. [Google Scholar] [CrossRef] [PubMed]
- Offerman, K.; Deffur, A.; Carulei, O.; Wilkinson, R.; Douglass, N.; Williamson, A.L. Six host-range restricted poxviruses from three genera induce distinct gene expression profiles in an in vivo mouse model. BMC Genomics 2015, 16, 510. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yates, N.L.; Liao, H.X.; Fong, Y.; deCamp, A.; Vandergrift, N.A.; Williams, W.T.; Alam, S.M.; Ferrari, G.; Yang, Z.Y.; Seaton, K.E.; et al. Vaccine-induced Env V1-V2 IgG3 correlates with lower HIV-1 infection risk and declines soon after vaccination. Sci Transl. Med. 2014, 6, 228ra239. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cottingham, M.G.; Carroll, M.W. Recombinant MVA vaccines: Dispelling the myths. Vaccine 2013, 31, 4247–4251. [Google Scholar] [CrossRef]
- Burgers, W.A.; Shephard, E.; Monroe, J.E.; Greenhalgh, T.; Binder, A.; Hurter, E.; Van Harmelen, J.H.; Williamson, C.; Williamson, A.L. Construction, characterization, and immunogenicity of a multigene modified vaccinia Ankara (MVA) vaccine based on HIV type 1 subtype C. AIDS Res. Hum. Retrovir. 2008, 24, 195–206. [Google Scholar] [CrossRef]
- Di Pilato, M.; Sanchez-Sampedro, L.; Mejias-Perez, E.; Sorzano, C.O.S.; Esteban, M. Modification of promoter spacer length in vaccinia virus as a strategy to control the antigen expression. J. Gen. Virol. 2015, 96, 2360–2371. [Google Scholar] [CrossRef]
- Noyce, R.S.; Lederman, S.; Evans, D.H. Construction of an infectious horsepox virus vaccine from chemically synthesized DNA fragments. PLoS ONE 2018, 13, e0188453. [Google Scholar] [CrossRef] [PubMed]
- Gowripalan, A.; Smith, S.; Stefanovic, T.; Tscharke, D.C. Rapid poxvirus engineering using CRISPR/Cas9 as a selection tool. Commun. Biol. 2020, 3, 643. [Google Scholar] [CrossRef] [PubMed]
- Wyatt, L.S.; Carroll, M.W.; Czerny, C.P.; Merchlinsky, M.; Sisler, J.R.; Moss, B. Marker rescue of the host range restriction defects of modified vaccinia virus Ankara. Virology 1998, 251, 334–342. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Promoter | Sequence | Size | Ref |
|---|---|---|---|
| pSS | AAAATTGAAATTTTATTTTTTTTTTTTGGAATATAAATA | 39 bp | [36] |
| pLEO | TTTTATTTTTTTTTTTTGGAATATAAATATCCGGTAAAATTGAAAAAATATACACTAATTAGCGTCTCGTTTCAGACGCTAG | 82 bp | [37] |
| pmFP | AGAAAAATATCCTAAAATTGAATTGTAATTATCGATAATAA | 41 bp | [38,39] |
| p7.5 | TCCAAACCCACCCGCTTTTTATAGTAAGTTTTTCACCCATAAATAATAAATACAATAATTAATTTCTCGTAAAAGTAGAAAATATA TTCTAATTTATTGCACGG | 104 bp | [40] |
| pmH5 | AAAAATTGAAAATAAATACAAAGGTTCTTGAGGGTTGTGTTAAATTGAAAGCGAGAAATAATCATAAATAA | 71 bp | [41] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
van Diepen, M.; Chapman, R.; Douglass, N.; Whittle, L.; Chineka, N.; Galant, S.; Cotchobos, C.; Suzuki, A.; Williamson, A.-L. Advancements in the Growth and Construction of Recombinant Lumpy Skin Disease Virus (LSDV) for Use as a Vaccine Vector. Vaccines 2021, 9, 1131. https://doi.org/10.3390/vaccines9101131
van Diepen M, Chapman R, Douglass N, Whittle L, Chineka N, Galant S, Cotchobos C, Suzuki A, Williamson A-L. Advancements in the Growth and Construction of Recombinant Lumpy Skin Disease Virus (LSDV) for Use as a Vaccine Vector. Vaccines. 2021; 9(10):1131. https://doi.org/10.3390/vaccines9101131
Chicago/Turabian Stylevan Diepen, Michiel, Rosamund Chapman, Nicola Douglass, Leah Whittle, Nicole Chineka, Shireen Galant, Christian Cotchobos, Akiko Suzuki, and Anna-Lise Williamson. 2021. "Advancements in the Growth and Construction of Recombinant Lumpy Skin Disease Virus (LSDV) for Use as a Vaccine Vector" Vaccines 9, no. 10: 1131. https://doi.org/10.3390/vaccines9101131
APA Stylevan Diepen, M., Chapman, R., Douglass, N., Whittle, L., Chineka, N., Galant, S., Cotchobos, C., Suzuki, A., & Williamson, A.-L. (2021). Advancements in the Growth and Construction of Recombinant Lumpy Skin Disease Virus (LSDV) for Use as a Vaccine Vector. Vaccines, 9(10), 1131. https://doi.org/10.3390/vaccines9101131






