Sentiments Regarding COVID-19 Vaccination among Graduate Students in Singapore
Abstract
:1. Introduction
2. Methods
2.1. Materials and Procedure
- (1)
- COVID-19 infection status (Yes/No);
- (2)
- COVID-19 vaccination status (Complete/ Incomplete/ Scheduled/No);
- (3)
- COVID-19 Risk (Thesis research requires them to work in an environment that puts them at high-risk for COVID-19 infection)
- (4)
- Contraindication to COVID-19 vaccine (Pregnancy/Immunocompromised/Previous anaphylaxis or severe allergy reaction/ Breastfeeding/ Bleeding disorder/None of the above);
- (5)
- Willingness to be vaccinated (If you are given an opportunity to be vaccinated, will you choose to be vaccinated? Yes/No/Unsure);
- (6)
- Concerns for the COVID-19 vaccination (Response can cite multiple concerns):
- Safety Concerns
- Side Effects
- Vaccine Choice
- Unnecessary
- Youth (I’m young and healthy)
- Personal (allergy/pregnancy/Others). Only respondents who responded No or Unsure answered this question.
2.2. Statistical Analysis
3. Results
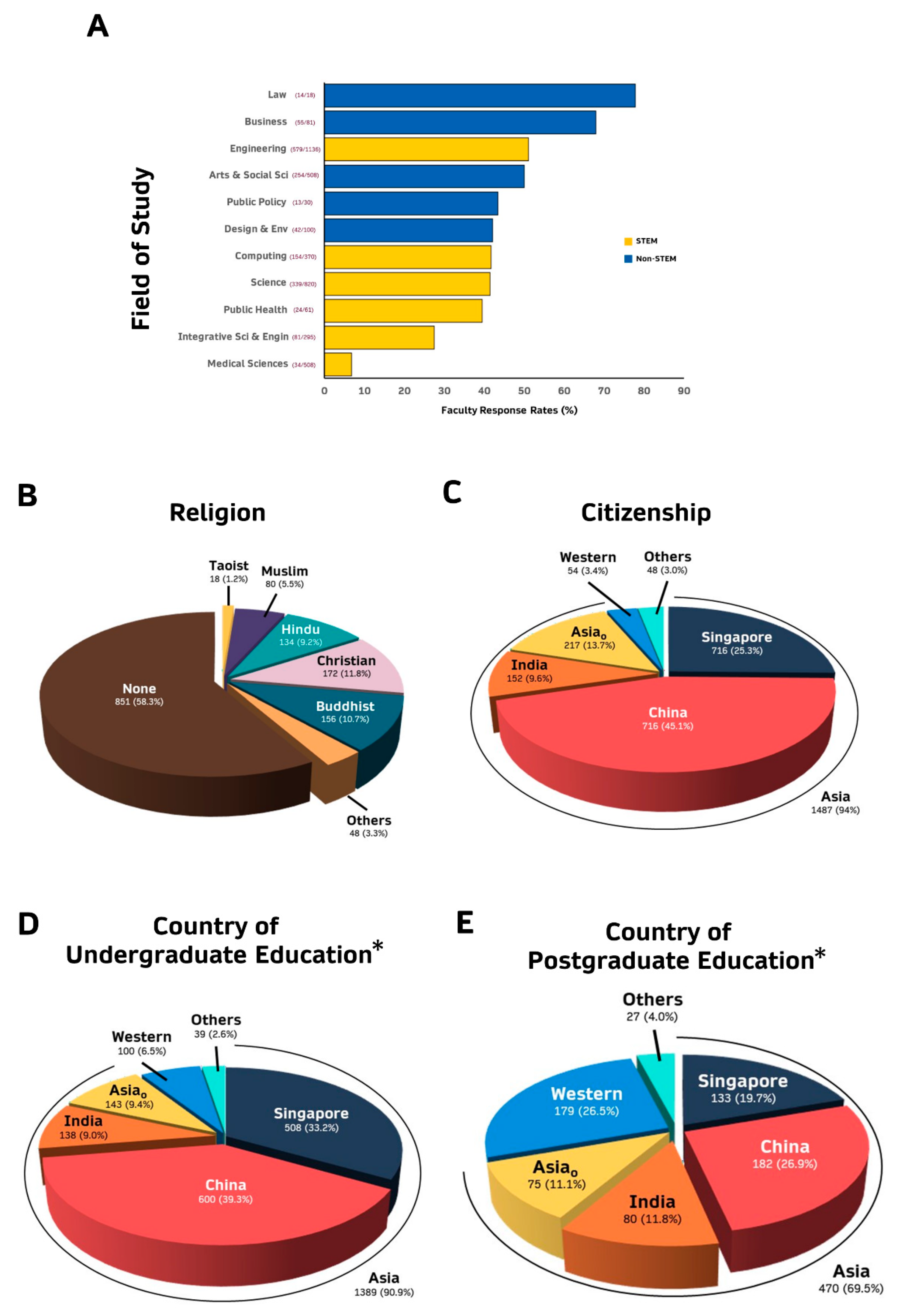
3.1. Majority of Respondents Are Asian PhD Graduate Students Pursuing STEM Fields
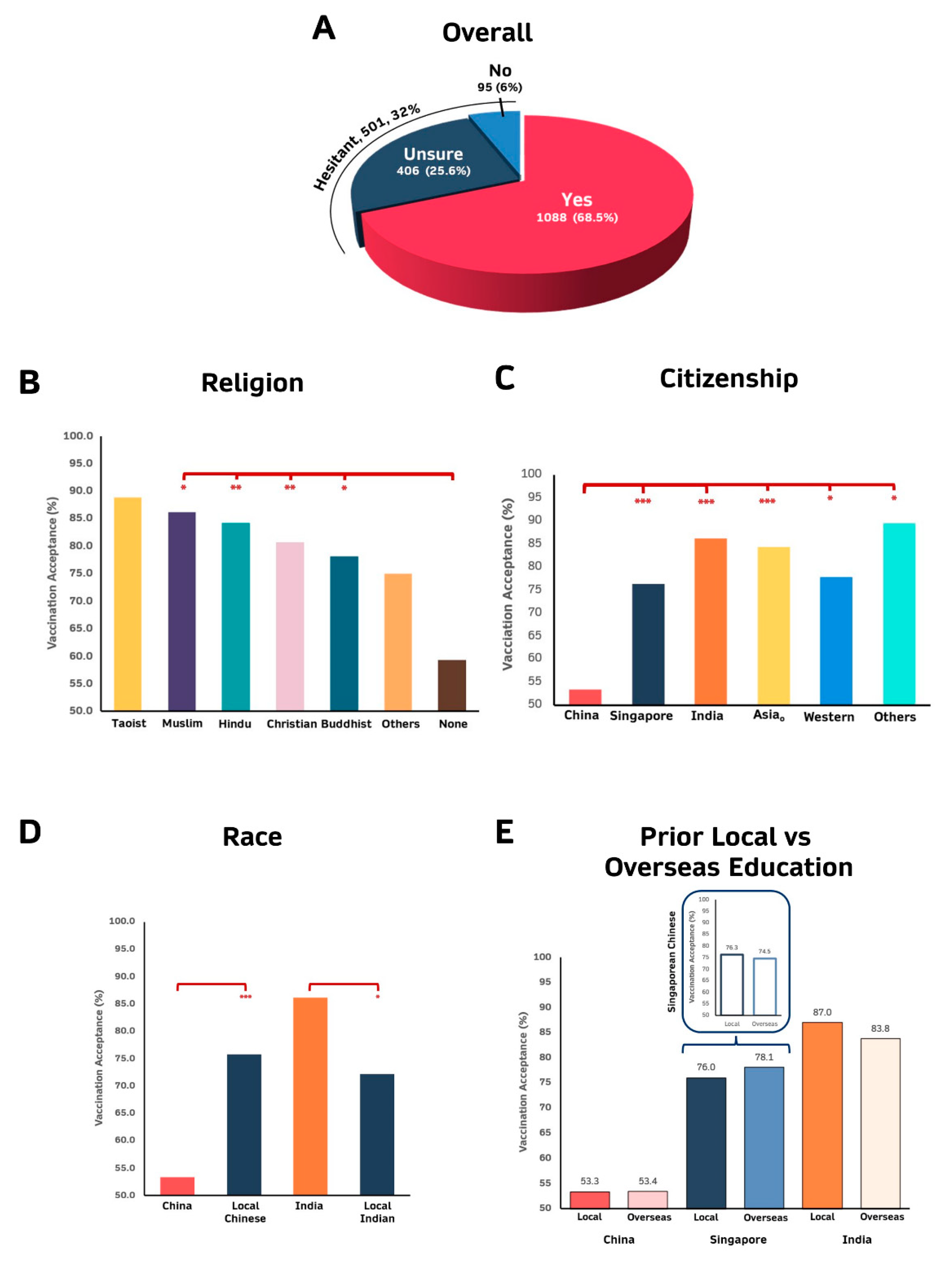
3.2. Non-Religious, Citizens of China and Graduate Students Pursuing Engineering, Law, Business and Design and Environment Are Less Willing to Be Vaccinated
3.3. Chinese Citizens without Prior Postgraduate Education Pursuing Business/Engineering Fields Are Predicted to Be Hesitant to Be Vaccinated
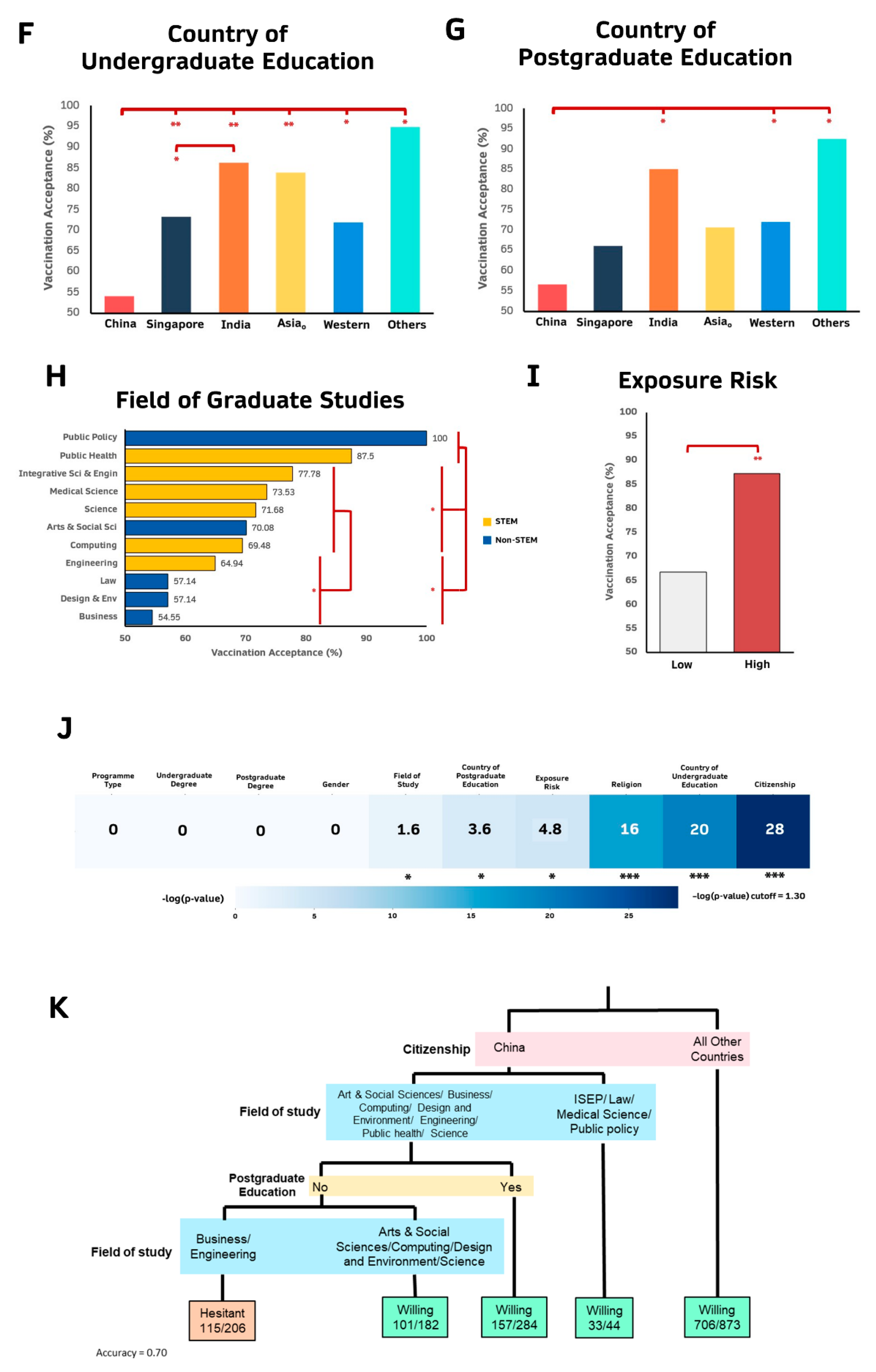
3.4. Safety Issues, Side Effects and Vaccine Choice Are the 3 Most Common Reasons for Vaccination Hesitancy
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 10 May 2021).
- Kimberly, C. Impact of COVID-19 on People’s Livelihoods, Their Health and Our Food Systems; World Health Organization: Geneva, Switzerland, 2020; pp. 4–7. [Google Scholar]
- Han, E.; Tan, M.M.J.; Turk, E.; Sridhar, D.; Leung, G.M.; Shibuya, K.; Asgari, N.; Oh, J.; García-Basteiro, A.L.; Hanefeld, J.; et al. Health Policy Lessons learnt from easing COVID-19 restrictions: An analysis of countries and regions in Asia Pacific and Europe. Lancet 2020, 396, 1525–1534. [Google Scholar] [CrossRef]
- Onyeaka, H.; Anumudu, C.K.; Al-Sharify, Z.T.; Egele-Godswill, E.; Mbaegbu, P. COVID-19 pandemic: A review of the global lockdown and its far-reaching effects. Sci. Prog. 2021, 104. [Google Scholar] [CrossRef]
- Chen, P.J.; Pusica, Y.; Sohaei, D.; Prassas, I.; Diamandis, E. An overview of mental health during the COVID-19 pandemic. Diagnosis 2021. [Google Scholar] [CrossRef]
- Authers, J. Covid, Liberty and Responsibility: Where’s the Line?-Bloomberg. Available online: https://www.bloomberg.com/opinion/articles/2021-05-09/covid-liberty-and-responsibility-where-s-the-line-kognfnb6 (accessed on 17 July 2021).
- Ball, P. The lightning-fast quest for COVID vaccines—and what it means for other diseases. Nature 2021, 589, 16–18. [Google Scholar] [CrossRef]
- Shen, M.; Zu, J.; Fairley, C.F.; Pagan, J.A.; An, L.; Du, Z.; Guo, Y.; Rong, L.; Xiao, Y.; Zhuang, G.; et al. Projected COVID-19 epidemic in the United States in the context of the effectiveness of a potential vaccine and implications for social distancing and face mask use. Vaccine 2021, 39, 2295–2302. [Google Scholar] [CrossRef]
- Miles, D.K.; Heald, A.H.; Stedman, M. How fast should social restrictions be eased in England as COVID-19 vaccinations are rolled out? Int. J. Clin. Pract. 2021, 75, e14191. [Google Scholar] [CrossRef] [PubMed]
- Aschwanden, C. The false promise of herd immunity for COVID-19. Nature 2020, 587, 26–28. [Google Scholar] [CrossRef] [PubMed]
- Coustasse, A.; Kimble, C.; Maxik, K. COVID-19 and Vaccine Hesitancy: A Challenge the United States Must Overcome. J. Ambul. Care Manag. 2021, 44, 71–75. [Google Scholar] [CrossRef]
- Kessels, R.; Luyten, J.; Tubeuf, S. Willingness to get vaccinated against COVID-19 and attitudes toward vaccination in general. Vaccine 2021, 39, 4716–4722. [Google Scholar] [CrossRef]
- Ball, P. Anti-vaccine movement could undermine efforts to end coronavirus pandemic, researchers warn. Nature 2020, 581, 251. [Google Scholar] [CrossRef]
- World Health Organization. Ten Threats to Global Health in 2019. Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 10 May 2021).
- Mathews, M.; Hou, M. The COVID-19 Pandemic in Singapore, One Year on: Population Attitudes and Sentiments April 2021 IPS Working Papers No. 40; Ingram Publisher Services: La Vergne, TN, USA, 2021. [Google Scholar]
- Clemente-Suárez, V.J.; Hormeño-Holgado, A.; Jiménez, M.; Benitez-Agudelo, J.C.; Navarro-Jiménez, E.; Perez-Palencia, N.; Maestre-Serrano, R.; Laborde-Cárdenas, C.C.; Tornero-Aguilera, J.F. Dynamics of Population Immunity Due to the Herd Effect in the COVID-19 Pandemic. Vaccines 2020, 8, 236. [Google Scholar] [CrossRef] [PubMed]
- Kadkhoda, K. Herd Immunity to COVID-19. Am. J. Clin. Pathol. 2021, 155, 471–472. [Google Scholar] [CrossRef] [PubMed]
- Edwards, B.; Biddle, N.; Gray, M.; Sollis, K. COVID-19 vaccine hesitancy and resistance: Correlates in a nationally representative longitudinal survey of the Australian population. PLoS ONE 2021, 16, e0248892. [Google Scholar] [CrossRef]
- Chew, N.W.S.; Cheong, C.; Kong, G.; Phua, K.; Ngiam, J.N.; Tan, B.Y.Q.; Wang, B.; Hao, F.; Tan, W.; Han, X.; et al. An Asia-Pacific study on healthcare workers’ perceptions of, and willingness to receive, the COVID-19 vaccination. Int. J. Infect. Dis. 2021, 106, 52–60. [Google Scholar] [CrossRef]
- Lazarus, J.V.; Ratzan, S.C.; Palayew, A.; Gostin, L.O.; Larson, H.J.; Rabin, K.; Kimball, S.; El-Mohandes, A. A global survey of potential acceptance of a COVID-19 vaccine. Nat. Med. 2021, 27, 225–228. [Google Scholar] [CrossRef]
- Dodd, R.H.; Pickles, K.; Nickel, B.; Cvejic, E.; Ayre, J.; Batcup, C.; Bonner, C.; Copp, T.; Cornell, S.; Dakin, T.; et al. Concerns and motivations about COVID-19 vaccination. Lancet Infect. Dis. 2021, 21, 161–163. [Google Scholar] [CrossRef]
- Dodd, R.H.; Cvejic, E.; Bonner, C.; Pickles, K.; McCaffery, K.J.; Ayre, J.; Batcup, C.; Copp, T.; Cornell, S.; Dakin, T.; et al. Willingness to vaccinate against COVID-19 in Australia. Lancet Infect. Dis. 2021, 21, 318–319. [Google Scholar] [CrossRef]
- World Population Review. Singapore Population 2021 (Demographics, Maps, Graphs). Available online: https://worldpopulationreview.com/countries/singapore-population (accessed on 18 July 2021).
- Ministry of Health of Singapore. COVID-19 Situation Report. Available online: https://covidsitrep.moh.gov.sg/ (accessed on 15 August 2021).
- Choo, Y.T. First COVID-19 vaccine shots to be given to NCID healthcare workers on Wednesday. The Straits Times, 30 December 2020. [Google Scholar]
- Lai, L. S’pore residents can now choose which COVID-19 vaccine to take; Moderna jabs given at 11 centres. The Straits Times, 13 April 2021. [Google Scholar]
- Bai, W.; Cai, H.; Liu, S.; Liu, H.; Qi, H.; Chen, X.; Liu, R.; Cheung, T.; Su, Z.; Ng, C.H.; et al. Attitudes toward COVID-19 vaccines in Chinese college students. Int. J. Biol. Sci. 2021, 17, 1469–1475. [Google Scholar] [CrossRef]
- Barello, S.; Nania, T.; Dellafiore, F.; Graffigna, G.; Caruso, R. Vaccine hesitancy among university students in Italy during the COVID-19 pandemic. Eur. J. Epidemiol. 2020, 35, 781–783. [Google Scholar] [CrossRef]
- Tavolacci, M.P.; Dechelotte, P.; Ladner, J. COVID-19 Vaccine Acceptance, Hesitancy, and Resistancy among University Students in France. Vaccines 2021, 9, 654. [Google Scholar] [CrossRef] [PubMed]
- Harapan, H.; Wagner, A.L.; Yufika, A.; Winardi, W.; Anwar, S.; Gan, A.K.; Setiawan, A.M.; Rajamoorthy, Y.; Sofyan, H.; Mudatsir, M. Acceptance of a COVID-19 Vaccine in Southeast Asia: A Cross-Sectional Study in Indonesia. Front. Public Health 2020, 8, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Therneau, T.; Atkinson, B.; Ripley, B.; Ripley, M.B. rpart: Recursive Partitioning and Regression Trees. R Packag. Version 4.1-10. 2015. Available online: https://stat.ethz.ch/R-manual/R-devel/library/rpart/html/rpart.html (accessed on 23 August 2021).
- Banks, D.L. Exploratory Data Analysis: Multivariate Approaches (Nonparametric Regression). Int. Encycl. Soc. Behav. Sci. 2001, 5164–5169. [Google Scholar] [CrossRef]
- Ihaka, R.; Gentleman, R. R: A Language for Data Analysis and Graphics. J. Comput. Graph. Stat. 1996, 5, 299. [Google Scholar] [CrossRef]
- Statista. Singapore: Resident Population by Ethnic Group 2020|Statista. Available online: https://www.statista.com/statistics/622748/singapore-resident-population-by-ethnic-group/ (accessed on 23 August 2021).
- Morgan, J. Classification and Regression Tree Analysis; Boston University: Boston, MA, USA, 2014. [Google Scholar]
- Statista. Singapore: COVID-19 Vaccination Willingness 2021|Statista. Available online: https://www.statista.com/statistics/1200507/singapore-vaccination-willingness-against-covid-19/#statisticContainer (accessed on 23 August 2021).
- Lucia, V.C.; Kelekar, A.; Afonso, N.M. COVID-19 vaccine hesitancy among medical students. J. Public Health 2020, 43, 1–5. [Google Scholar] [CrossRef]
- Jain, J.; Saurabh, S.; Kumar, P.; Verma, M.K.; Goel, A.D.; Gupta, M.K.; Bhardwaj, P.; Raghav, P.R. COVID-19 vaccine hesitancy among medical students in India. Epidemiol. Infect. 2021, 149, e132. [Google Scholar] [CrossRef]
- Mant, M.; Aslemand, A.; Prine, A.; Holland, A.J. University students’ perspectives, planned uptake, and hesitancy regarding the COVID-19 vaccine: A multi-methods study. PLoS ONE 2021, 16, e0255447. [Google Scholar] [CrossRef] [PubMed]
- Burge, R. The Young and Secular Are Least Vaccinated, Not Evangelicals. Available online: https://religionunplugged.com/news/2021/8/3/the-young-and-secular-are-least-vaccinated-not-evangelicals (accessed on 15 August 2021).
- VaxDashboard Singapore COVID-19 Vaccination Info. Available online: https://vaxdashboard.com (accessed on 1 September 2021).
- Ministry of Health. MOH|COVID-19 Vaccination. Available online: https://www.moh.gov.sg/covid-19/vaccination (accessed on 13 August 2021).
- Pazos, R.S.A. Tracking Singapore’s COVID-19 Vaccination Progress|The Straits Times. Available online: https://www.straitstimes.com/multimedia/graphics/2021/06/singapore-covid-vaccination-tracker/index.html?shell (accessed on 2 September 2021).
- Question Pro. Snowball Sampling: Definition, Method, Advantages and Disadvantages|Question Pro. Available online: https://www.questionpro.com/blog/snowball-sampling/ (accessed on 15 September 2021).
- Sharma, G. Pros and cons of different sampling techniques. Int. J. Appl. Res. 2017, 3, 749–752. [Google Scholar]
- Robinson, N. Advantages & Disadvantages of Snowball Sampling. Available online: https://classroom.synonym.com/advantages-disadvantages-snowball-sampling-8444993.html (accessed on 15 September 2021).
- Dabla-Norris, E.; Khan, H.; Lima, F.; Sollaci, A. IMF Working Paper: Who Doesn’t Want to Be Vaccinated? Determinants of Vaccine Hesitancy During COVID-19; International Monetary Fund: Washington, DC, USA, 2021. [Google Scholar]
- ABC News. What’s Fueling COVID-19 Vaccine Hesitancy in Young Adults—ABC News. Available online: https://abcnews.go.com/Health/young-adults-remain-hesitant-covid-19-vaccine/story?id=78828317 (accessed on 8 August 2021).
- Burke, P.F.; Masters, D.; Massey, G. Enablers and barriers to COVID-19 vaccine uptake: An international study of perceptions and intentions. Vaccine 2021, 39, 5116–5128. [Google Scholar] [CrossRef]
- Ministry of Health of Singapore. Past Updates on COVID-19 Local Situation. Available online: https://www.moh.gov.sg/covid-19/past-updates (accessed on 15 August 2021).
- Riley, S.; Wang, H.; Eales, O.; Haw, D.; Walters, C.E.; Ainslie, K.E.C.; Atchison, C.; Fronterre, C.; Diggle, P.J.; Page, A.J.; et al. REACT-1 round 12 report: Resurgence of SARS-CoV-2 infections in England associated with increased frequency of the Delta variant. medRxiv 2021. [Google Scholar] [CrossRef]
- Sheikh, A.; McMenamin, J.; Taylor, B.; Robertson, C.; Protection Health Scotland; EAVE Collaborators I. SARS-CoV-2 Delta VOC in Scotland: Demographics, risk of hospital admission, and vaccine effectiveness. Lancet 2021, 397, 2461–2462. [Google Scholar] [CrossRef]
- Machingaidze, S.; Wiysonge, C.S. Understanding COVID-19 vaccine hesitancy. Nat. Med. 2021, 27, 1–2. [Google Scholar] [CrossRef]
- Verger, P.; Scronias, D.; Dauby, N.; Adedzi, K.A.; Gobert, C.; Bergeat, M.; Gagneur, A.; Dubé, E. Attitudes of healthcare workers towards COVID-19 vaccination: A survey in France and French-speaking parts of Belgium and Canada, 2020. Eurosurveillance 2021, 26, 2002047. [Google Scholar] [CrossRef]
- Dong, D.; Xu, R.H.; Wong, E.L.Y.I.; Hung, C.T.; Feng, D.; Feng, Z.; Yeoh, E.; Wong, S.Y. Shan Public preference for COVID-19 vaccines in China: A discrete choice experiment. Health Expect. 2020, 23, 1543–1578. [Google Scholar] [CrossRef] [PubMed]
- Bell, S.; Clarke, R.; Mounier-Jack, S.; Walker, J.L.; Paterson, P. Parents’ and guardians’ views on the acceptability of a future COVID-19 vaccine: A multi-methods study in England. Vaccine 2020, 38, 7789–7798. [Google Scholar] [CrossRef]
- Yin, F.; Wu, Z.; Xia, X.; Ji, M.; Wang, Y.; Hu, Z. Unfolding the Determinants of COVID-19 Vaccine Acceptance in China. J. Med. Internet Res. 2021, 23, e26089. [Google Scholar] [CrossRef] [PubMed]
- Leng, A.; Maitland, E.; Wang, S.; Nicholas, S.; Liu, R.; Wang, J. Individual preferences for COVID-19 vaccination in China. Vaccine 2021, 39, 247–254. [Google Scholar] [CrossRef] [PubMed]
- Toh, T. First Shipment of Moderna’s COVID-19 Vaccine Arrives in Singapore Ahead of Schedule, Transport News & Top Stories-The Straits Times. Available online: https://www.straitstimes.com/singapore/transport/first-shipment-of-modernas-covid-19-vaccine-arrives-in-singapore-on-feb-17 (accessed on 16 August 2021).
- Goh, T. Moderna COVID-19 Vaccine to Start Being Administered at Four New Vaccination Centres, Health News & Top Stories-The Straits Times. Available online: https://www.straitstimes.com/singapore/health/moderna-covid-19-vaccine-to-start-being-administered-at-four-new-vaccination (accessed on 16 August 2021).
- Dror, A.A.; Daoud, A.; Morozov, N.G.; Layous, E.; Eisenbach, N.; Mizrachi, M.; Rayan, D.; Bader, A.; Francis, S.; Kaykov, E.; et al. Vaccine hesitancy due to vaccine country of origin, vaccine technology, and certification. Eur. J. Epidemiol. 2021, 36, 1–6. [Google Scholar] [CrossRef]
- Lin, Y.; Hu, Z.; Zhao, Q.; Alias, H.; Danaee, M.; Wong, L.P. Understanding COVID-19 vaccine demand and hesitancy: A nationwide online survey in China. PLoS Negl. Trop. Dis. 2020, 14, e0008961. [Google Scholar] [CrossRef]
- O’Brien, E.; Che, C.; Leigh, K.; Hong, J.; Chrysoloras, N. When It Comes to a Travel Restart All Vaccines Are Not Equal-Bloomberg. Available online: https://www.bloomberg.com/news/articles/2021-04-25/vaccine-travel-rules-widen-the-rift-between-china-and-the-west (accessed on 9 August 2021).
- Davidson, H. China to Only Allow Foreign Visitors Who Have Had Chinese-Made Vaccine|China|The Guardian. Available online: https://www.theguardian.com/world/2021/mar/17/china-to-allow-foreign-visitors-who-have-had-chinese-made-vaccine (accessed on 8 August 2021).
- The Straits Times. COVID-19 Vaccine Travel Rules Widen the Rift between China and the West, East Asia News & Top Stories-The Straits Times. Available online: https://www.straitstimes.com/asia/east-asia/covid-19-vaccine-travel-rules-widen-the-rift-between-china-and-the-west (accessed on 8 August 2021).
- Deng, C. Traveling to China Just Got Easier—If You Take a Chinese COVID-19 Vaccine-WSJ. Available online: https://www.wsj.com/articles/china-to-allow-more-foreigners-inif-theyve-had-a-chinese-covid-vaccine-11615900150 (accessed on 8 August 2021).
- Wikipedia COVID-19 Vaccination in Singapore. Available online: https://en.wikipedia.org/wiki/COVID-19_vaccination_in_Singapore (accessed on 10 August 2021).
- Rostkowska, O.M.; Peters, A.; Montvidas, J.; Magdas, T.M.; Rensen, L.; Zgliczyński, W.S.; Durlik, M.; Pelzer, B.W. Attitudes and knowledge of European medical students and early graduates about vaccination and self-reported vaccination coverage—multinational cross-sectional survey. Int. J. Environ. Res. Public Health 2021, 18, 3595. [Google Scholar] [CrossRef] [PubMed]
- Roccetti, M.; Marfia, G.; Salomoni, P.; Prandi, C.; Zagari, R.M.; Kengni, F.L.G.; Montagnani, M. Attitudes of Crohn’s Disease Patients: Infodemiology Case Study and Sentiment Analysis of Facebook and Twitter Posts. JMIR Public Health Surveill. 2017, 3, e7004. [Google Scholar] [CrossRef] [PubMed]
- Milano, M.; Zucco, C.; Cannataro, M. COVID-19 Community Temporal Visualizer: A new methodology for the network-based analysis and visualization of COVID-19 data. Netw. Model. Anal. Health Inform. Bioinforma. 2021, 10, 46. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lim, L.J.; Lim, A.J.W.; Fong, K.K.; Lee, C.G. Sentiments Regarding COVID-19 Vaccination among Graduate Students in Singapore. Vaccines 2021, 9, 1141. https://doi.org/10.3390/vaccines9101141
Lim LJ, Lim AJW, Fong KK, Lee CG. Sentiments Regarding COVID-19 Vaccination among Graduate Students in Singapore. Vaccines. 2021; 9(10):1141. https://doi.org/10.3390/vaccines9101141
Chicago/Turabian StyleLim, Lee Jin, Ashley J. W. Lim, Kevin K. Fong, and Caroline G. Lee. 2021. "Sentiments Regarding COVID-19 Vaccination among Graduate Students in Singapore" Vaccines 9, no. 10: 1141. https://doi.org/10.3390/vaccines9101141
APA StyleLim, L. J., Lim, A. J. W., Fong, K. K., & Lee, C. G. (2021). Sentiments Regarding COVID-19 Vaccination among Graduate Students in Singapore. Vaccines, 9(10), 1141. https://doi.org/10.3390/vaccines9101141






