Assessment of an LSDV-Vectored Vaccine for Heterologous Prime-Boost Immunizations against HIV
Abstract
:1. Introduction
2. Materials and Methods
2.1. Antibodies, Cell Lines, Media, and Reagents
2.2. Design and Construction of DNA, MVA, and LSDV Vaccines Expressing Env and Gag
2.3. PCR Confirmation of the LSDV Recombinant
2.4. Live-Cell Staining Using Human Monoclonal Anti-Env Antibodies
2.5. VLP Isolation and Characterization
2.6. Rabbit Immunizations
2.7. Anti-Env Enzyme-Linked Immunosorbent Assays (ELISA) and HIV Neutralization Assays
2.8. Statistical Analysis
3. Results
3.1. Design and Construction of Vaccines
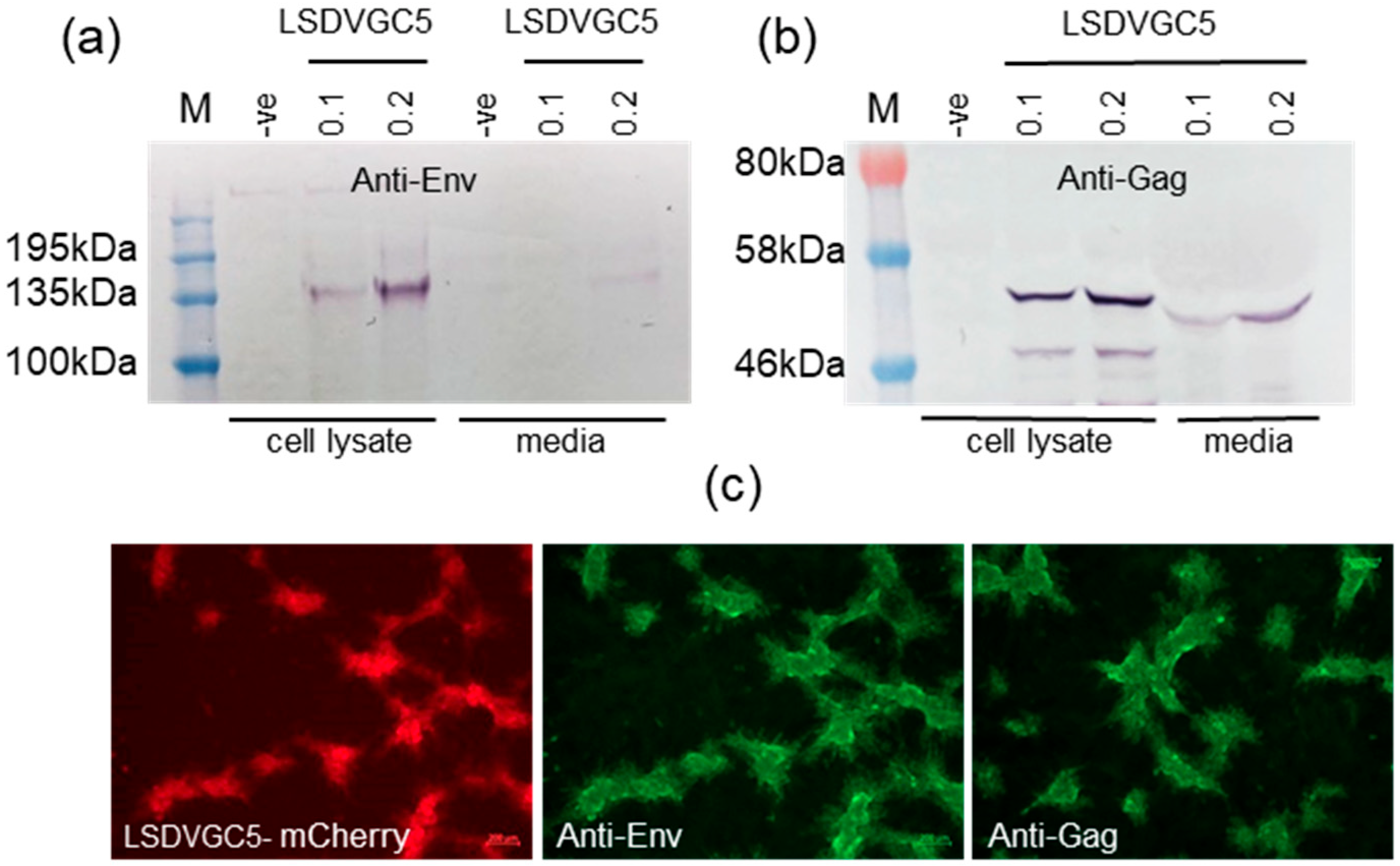
3.2. Expression of Env and Gag
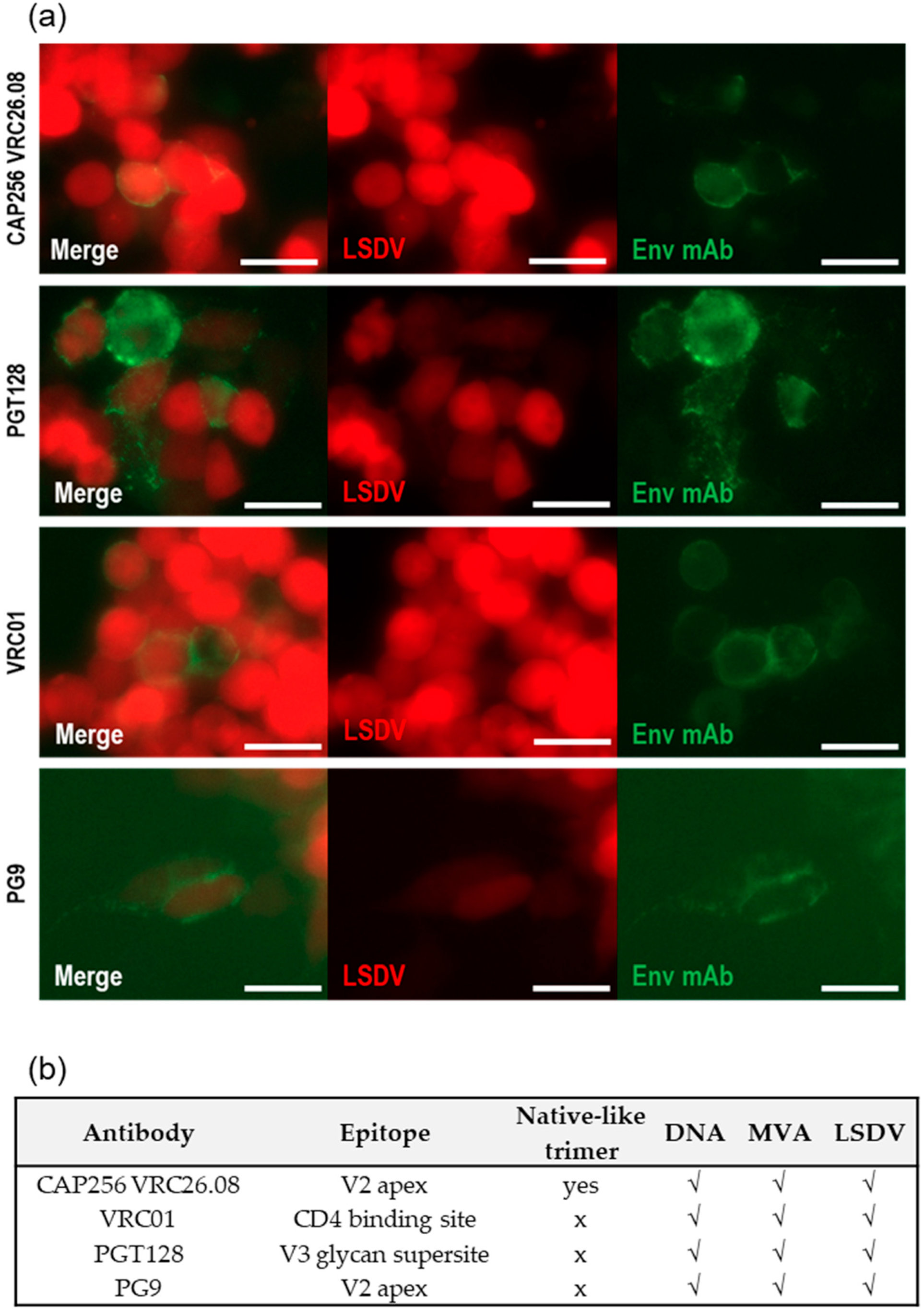
3.3. Quaternary Structure of Env Expressed In Vitro
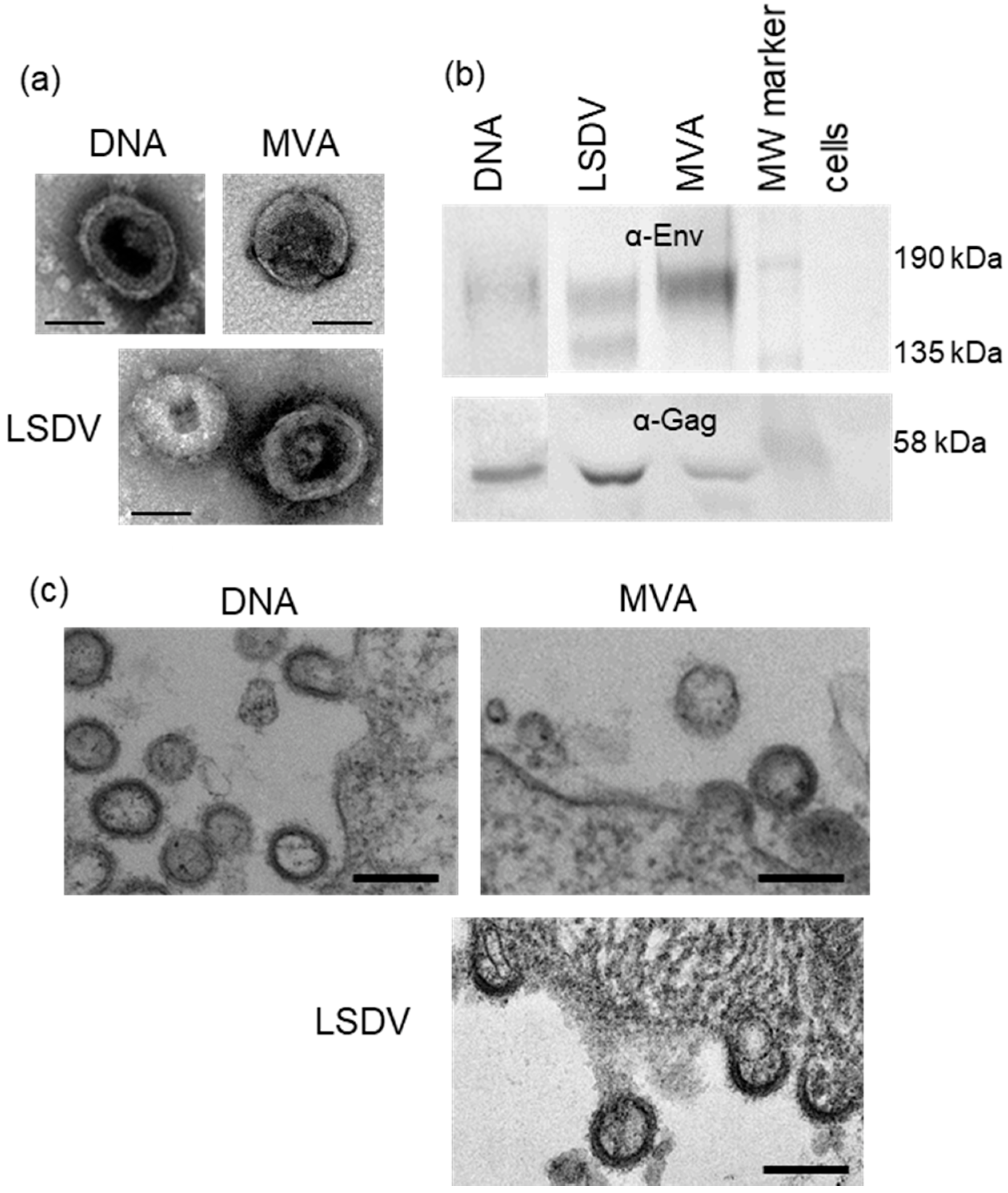
3.4. Confirmation of Virus-like Particle Formation
3.5. Heterologous Vaccination with DNA and Two Different Poxvirus Vectors
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Acknowledgments
Conflicts of Interest
References
- Lundstrom, K. Viral Vectors for COVID-19 Vaccine Development. Viruses 2021, 13, 317. [Google Scholar] [CrossRef] [PubMed]
- Sasso, E.; D’Alise, A.M.; Zambrano, N.; Scarselli, E.; Folgori, A.; Nicosia, A. New viral vectors for infectious diseases and cancer. Semin. Immunol. 2020, 50, 101430. [Google Scholar] [CrossRef]
- Mok, D.Z.L.; Chan, K.R. The Effects of Pre-Existing Antibodies on Live-Attenuated Viral Vaccines. Viruses 2020, 12, 520. [Google Scholar] [CrossRef]
- Buchbinder, S.P.; Mehrotra, D.V.; Duerr, A.; Fitzgerald, D.W.; Mogg, R.; Li, D.; Gilbert, P.B.; Lama, J.R.; Marmor, M.; Del Rio, C.; et al. Efficacy assessment of a cell-mediated immunity HIV-1 vaccine (the Step Study): A double-blind, randomised, placebo-controlled, test-of-concept trial. Lancet 2008, 372, 1881–1893. [Google Scholar] [CrossRef] [Green Version]
- Chang, J. Adenovirus Vectors: Excellent Tools for Vaccine Development. Immune Netw. 2021, 21, e6. [Google Scholar] [CrossRef] [PubMed]
- Beyrer, C. A pandemic anniversary: 40 years of HIV/AIDS. Lancet 2021, 397, 2142–2143. [Google Scholar] [CrossRef]
- Wen, Z.; Sun, C. A Zigzag but Upward Way to Develop an HIV-1 Vaccine. Vaccines 2020, 8, 511. [Google Scholar] [CrossRef] [PubMed]
- Stephenson, K.E.; Wagh, K.; Korber, B.; Barouch, D.H. Vaccines and Broadly Neutralizing Antibodies for HIV-1 Prevention. Annu. Rev. Immunol. 2020, 38, 673–703. [Google Scholar] [CrossRef] [PubMed]
- Jones, L.D.; Moody, M.A.; Thompson, A.B. Innovations in HIV-1 Vaccine Design. Clin. Ther. 2020, 42, 499–514. [Google Scholar] [CrossRef] [PubMed]
- Burton, S.; Spicer, L.M.; Charles, T.P.; Gangadhara, S.; Reddy, P.B.J.; Styles, T.M.; Velu, V.; Kasturi, S.P.; Legere, T.; Hunter, E.; et al. Clade C HIV-1 Envelope Vaccination Regimens Differ in Their Ability To Elicit Antibodies with Moderate Neutralization Breadth against Genetically Diverse Tier 2 HIV-1 Envelope Variants. J. Virol. 2019, 93. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Palli, R.; Seaton, K.E.; Piepenbrink, M.S.; Hural, J.; Goepfert, P.A.; Laher, F.; Buchbinder, S.P.; Churchyard, G.; Gray, G.E.; Robinson, H.L.; et al. Impact of vaccine type on HIV-1 vaccine elicited antibody durability and B cell gene signature. Sci. Rep. 2020, 10, 13031. [Google Scholar] [CrossRef] [PubMed]
- Eslamizar, L.; Petrovas, C.; Leggat, D.J.; Furr, K.; Lifton, M.L.; Levine, G.; Ma, S.; Fletez-Brant, C.; Hoyland, W.; Prabhakaran, M.; et al. Recombinant MVA-prime elicits neutralizing antibody responses by inducing antigen-specific B cells in the germinal center. NPJ Vaccines 2021, 6, 15. [Google Scholar] [CrossRef]
- Offerman, K.; Deffur, A.; Carulei, O.; Wilkinson, R.; Douglass, N.; Williamson, A.L. Six host-range restricted poxviruses from three genera induce distinct gene expression profiles in an in vivo mouse model. BMC Genom. 2015, 16, 510. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paoletti, E. Poxvirus recombinant vaccines. Ann. N. Y. Acad. Sci. 1990, 590, 309–325. [Google Scholar] [CrossRef] [PubMed]
- Kitching, R.P. Capripoxviruses; Academic Press: Cambridge, MA, USA, 2008; pp. 427–432. [Google Scholar]
- Hamdi, J.; Bamouh, Z.; Jazouli, M.; Boumart, Z.; Tadlaoui, K.O.; Fihri, O.F.; El Harrak, M. Experimental evaluation of the cross-protection between Sheeppox and bovine Lumpy skin vaccines. Sci. Rep. 2020, 10, 8888. [Google Scholar] [CrossRef]
- Baxby, D. A comparison of the antigens present on the surface of virus released artificially from chick cells infected with vaccinia virus, and cowpox virus and its white pock mutant. J. Hyg. (Lond.) 1972, 70, 353–365. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gilchuk, I.; Gilchuk, P.; Sapparapu, G.; Lampley, R.; Singh, V.; Kose, N.; Blum, D.L.; Hughes, L.J.; Satheshkumar, P.S.; Townsend, M.B.; et al. Cross-Neutralizing and Protective Human Antibody Specificities to Poxvirus Infections. Cell 2016, 167, 684–694.e9. [Google Scholar] [CrossRef] [Green Version]
- Gomez, C.E.; Perdiguero, B.; Garcia-Arriaza, J.; Esteban, M. Poxvirus vectors as HIV/AIDS vaccines in humans. Hum. Vaccin. Immunother. 2012, 8, 1192–1207. [Google Scholar] [CrossRef] [Green Version]
- Carulei, O.; Douglass, N.; Williamson, A.L. Comparative analysis of avian poxvirus genomes, including a novel poxvirus from lesser flamingos (Phoenicopterus minor), highlights the lack of conservation of the central region. BMC Genom. 2017, 18, 947. [Google Scholar] [CrossRef]
- Tulman, E.R.; Afonso, C.L.; Lu, Z.; Zsak, L.; Kutish, G.F.; Rock, D.L. The genome of canarypox virus. J. Virol. 2004, 78, 353–366. [Google Scholar] [CrossRef] [Green Version]
- Mackenzie, J.S.; Jeggo, M. The One Health Approach-Why Is It So Important? Trop Med. Infect. Dis. 2019, 4, 88. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Volkmann, A.; Williamson, A.L.; Weidenthaler, H.; Meyer, T.P.H.; Robertson, J.S.; Excler, J.L.; Condit, R.C.; Evans, E.; Smith, E.R.; Kim, D.; et al. The Brighton Collaboration standardized template for collection of key information for risk/benefit assessment of a Modified Vaccinia Ankara (MVA) vaccine platform. Vaccine 2021, 39, 3067–3080. [Google Scholar] [CrossRef] [PubMed]
- Gray, G.E.; Mayer, K.H.; Elizaga, M.L.; Bekker, L.G.; Allen, M.; Morris, L.; Montefiori, D.; De Rosa, S.C.; Sato, A.; Gu, N.; et al. Subtype C gp140 Vaccine Boosts Immune Responses Primed by the South African AIDS Vaccine Initiative DNA-C2 and MVA-C HIV Vaccines after More than a 2-Year Gap. Clin. Vaccine Immunol. 2016, 23, 496–506. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heger, E.; Schuetz, A.; Vasan, S. HIV Vaccine Efficacy Trials: RV144 and Beyond. Adv. Exp. Med. Biol. 2018, 1075, 3–30. [Google Scholar] [CrossRef]
- Levy, Y.; Lacabaratz, C.; Ellefsen-Lavoie, K.; Stohr, W.; Lelievre, J.D.; Bart, P.A.; Launay, O.; Weber, J.; Salzberger, B.; Wiedemann, A.; et al. Optimal priming of poxvirus vector (NYVAC)-based HIV vaccine regimens for T cell responses requires three DNA injections. Results of the randomized multicentre EV03/ANRS VAC20 Phase I/II Trial. PLoS Pathog. 2020, 16, e1008522. [Google Scholar] [CrossRef]
- Tuppurainen, E.S.M.; Venter, E.H.; Shisler, J.L.; Gari, G.; Mekonnen, G.A.; Juleff, N.; Lyons, N.A.; De Clercq, K.; Upton, C.; Bowden, T.R.; et al. Review: Capripoxvirus Diseases: Current Status and Opportunities for Control. Transbound Emerg. Dis. 2017, 64, 729–745. [Google Scholar] [CrossRef]
- Burgers, W.A.; Ginbot, Z.; Shen, Y.J.; Chege, G.K.; Soares, A.P.; Muller, T.L.; Bunjun, R.; Kiravu, A.; Munyanduki, H.; Douglass, N.; et al. The novel capripoxvirus vector lumpy skin disease virus efficiently boosts modified vaccinia Ankara human immunodeficiency virus responses in rhesus macaques. J. Gen. Virol. 2014, 95, 2267–2272. [Google Scholar] [CrossRef] [PubMed]
- Shen, Y.J.; Shephard, E.; Douglass, N.; Johnston, N.; Adams, C.; Williamson, C.; Williamson, A.L. A novel candidate HIV vaccine vector based on the replication deficient Capripoxvirus, Lumpy skin disease virus (LSDV). Virol. J. 2011, 8, 265. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aspden, K.; Passmore, J.A.; Tiedt, F.; Williamson, A.L. Evaluation of lumpy skin disease virus, a capripoxvirus, as a replication-deficient vaccine vector. J. Gen. Virol. 2003, 84, 1985–1996. [Google Scholar] [CrossRef] [PubMed]
- Sanders, R.W.; Moore, J.P. Native-like Env trimers as a platform for HIV-1 vaccine design. Immunol. Rev. 2017, 275, 161–182. [Google Scholar] [CrossRef] [Green Version]
- Williamson, A.L.; Rybicki, E.P. Justification for the inclusion of Gag in HIV vaccine candidates. Expert Rev. Vaccines 2016, 15, 585–598. [Google Scholar] [CrossRef]
- Chapman, R.; Jongwe, T.I.; Douglass, N.; Chege, G.; Williamson, A.L. Heterologous prime-boost vaccination with DNA and MVA vaccines, expressing HIV-1 subtype C mosaic Gag virus-like particles, is highly immunogenic in mice. PLoS ONE 2017, 12, e0173352. [Google Scholar] [CrossRef]
- Chapman, R.; van Diepen, M.; Galant, S.; Kruse, E.; Margolin, E.; Ximba, P.; Hermanus, T.; Moore, P.; Douglass, N.; Williamson, A.L.; et al. Immunogenicity of HIV-1 Vaccines Expressing Chimeric Envelope Glycoproteins on the Surface of Pr55 Gag Virus-Like Particles. Vaccines 2020, 8, 54. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Douglass, N.; van Diepen, M.T.; Chapman, R.; Galant, S.; Margolin, E.; Ximba, P.; Hermanus, T.; Moore, P.L.; Williamson, A.L. Modifications to the HIV-1 SAAVI MVA-C vaccine improve in vitro expression and in vivo immunogenicity. Vaccine 2021, 39, 463–468. [Google Scholar] [CrossRef] [PubMed]
- van Diepen, M.T.; Chapman, R.; Douglass, N.; Galant, S.; Moore, P.L.; Margolin, E.; Ximba, P.; Morris, L.; Rybicki, E.P.; Williamson, A.L. Prime-Boost Immunizations with DNA, Modified Vaccinia Virus Ankara, and Protein-Based Vaccines Elicit Robust HIV-1 Tier 2 Neutralizing Antibodies against the CAP256 Superinfecting Virus. J. Virol. 2019, 93. [Google Scholar] [CrossRef] [Green Version]
- van Diepen, M.T.; Chapman, R.; Moore, P.L.; Margolin, E.; Hermanus, T.; Morris, L.; Ximba, P.; Rybicki, E.P.; Williamson, A.L. The adjuvant AlhydroGel elicits higher antibody titres than AddaVax when combined with HIV-1 subtype C gp140 from CAP256. PLoS ONE 2018, 13, e0208310. [Google Scholar] [CrossRef] [Green Version]
- Doria-Rose, N.A.; Schramm, C.A.; Gorman, J.; Moore, P.L.; Bhiman, J.N.; DeKosky, B.J.; Ernandes, M.J.; Georgiev, I.S.; Kim, H.J.; Pancera, M.; et al. Developmental pathway for potent V1V2-directed HIV-neutralizing antibodies. Nature 2014, 509, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Bhiman, J.N.; Anthony, C.; Doria-Rose, N.A.; Karimanzira, O.; Schramm, C.A.; Khoza, T.; Kitchin, D.; Botha, G.; Gorman, J.; Garrett, N.J.; et al. Viral variants that initiate and drive maturation of V1V2-directed HIV-1 broadly neutralizing antibodies. Nat. Med. 2015, 21, 1332–1336. [Google Scholar] [CrossRef]
- Andrabi, R.; Voss, J.E.; Liang, C.H.; Briney, B.; McCoy, L.E.; Wu, C.Y.; Wong, C.H.; Poignard, P.; Burton, D.R. Identification of Common Features in Prototype Broadly Neutralizing Antibodies to HIV Envelope V2 Apex to Facilitate Vaccine Design. Immunity 2015, 43, 959–973. [Google Scholar] [CrossRef]
- Gorman, J.; Soto, C.; Yang, M.M.; Davenport, T.M.; Guttman, M.; Bailer, R.T.; Chambers, M.; Chuang, G.Y.; DeKosky, B.J.; Doria-Rose, N.A.; et al. Structures of HIV-1 Env V1V2 with broadly neutralizing antibodies reveal commonalities that enable vaccine design. Nat. Struct. Mol. Biol. 2016, 23, 81–90. [Google Scholar] [CrossRef]
- Chege, G.K.; Adams, C.H.; Keyser, A.T.; Bekker, V.; Morris, L.; Villinger, F.J.; Williamson, A.L.; Chapman, R.E. Infection of Chinese Rhesus Monkeys with a Subtype C SHIV Resulted in Attenuated In Vivo Viral Replication Despite Successful Animal-to-Animal Serial Passages. Viruses 2021, 13, 397. [Google Scholar] [CrossRef] [PubMed]
- Rademeyer, C.; Korber, B.; Seaman, M.S.; Giorgi, E.E.; Thebus, R.; Robles, A.; Sheward, D.J.; Wagh, K.; Garrity, J.; Carey, B.R.; et al. Features of Recently Transmitted HIV-1 Clade C Viruses that Impact Antibody Recognition: Implications for Active and Passive Immunization. PLoS Pathog. 2016, 12, e1005742. [Google Scholar] [CrossRef] [PubMed]
- Douglass, N.; Munyanduki, H.; Omar, R.; Gers, S.; Mutowembwa, P.; Heath, L.; Williamson, A.L. Influence of the Viral Superoxide Dismutase (SOD) Homologue on Lumpy Skin Disease Virus (LSDV) Growth, Histopathology and Pathogenicity. Vaccines 2020, 8, 664. [Google Scholar] [CrossRef]
- Moore, P.L.; Sheward, D.; Nonyane, M.; Ranchobe, N.; Hermanus, T.; Gray, E.S.; Abdool Karim, S.S.; Williamson, C.; Morris, L. Multiple pathways of escape from HIV broadly cross-neutralizing V2-dependent antibodies. J. Virol. 2013, 87, 4882–4894. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fischer, W.; Perkins, S.; Theiler, J.; Bhattacharya, T.; Yusim, K.; Funkhouser, R.; Kuiken, C.; Haynes, B.; Letvin, N.L.; Walker, B.D.; et al. Polyvalent vaccines for optimal coverage of potential T-cell epitopes in global HIV-1 variants. Nat. Med. 2007, 13, 100–106. [Google Scholar] [CrossRef]
- Tanzer, F.L.; Shephard, E.G.; Palmer, K.E.; Burger, M.; Williamson, A.L.; Rybicki, E.P. The porcine circovirus type 1 capsid gene promoter improves antigen expression and immunogenicity in a HIV-1 plasmid vaccine. Virol. J. 2011, 8, 51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Douglass, N.; Omar, R.; Munyanduki, H.; Suzuki, A.; de Moor, W.; Mutowembwa, P.; Pretorius, A.; Nefefe, T.; Schalkwyk, A.v.; Kara, P.; et al. The Development of Dual Vaccines against Lumpy Skin Disease (LSD) and Bovine Ephemeral Fever (BEF). Vaccines 2021, 9, 1215. [Google Scholar] [CrossRef]
- Omar, R. Comparison of the two lumpy skin disease virus vaccines, Neethling and Herbivac, and construction of a recombinant Herbivac-Rift Valley fever virus vaccine. Master’s Thesis, University of Cape Town, Cape Town, South Africa, 2015. [Google Scholar]
- van Diepen, M.; Chapman, R.; Douglass, N.; Whittle, L.; Chineka, N.; Galant, S.; Cotchobos, C.; Suzuki, A.; Williamson, A.L. Advancements in the Growth and Construction of Recombinant Lumpy Skin Disease Virus (LSDV) for Use as a Vaccine Vector. Vaccines 2021, 9, 1131. [Google Scholar] [CrossRef]
- Liu, F.; Zhang, H.; Liu, W. Construction of recombinant capripoxviruses as vaccine vectors for delivering foreign antigens: Methodology and application. Comp. Immunol. Microbiol. Infect. Dis. 2019, 65, 181–188. [Google Scholar] [CrossRef]
- Chea, L.S.; Amara, R.R. Immunogenicity and efficacy of DNA/MVA HIV vaccines in rhesus macaque models. Expert Rev. Vaccines 2017, 16, 973–985. [Google Scholar] [CrossRef] [PubMed]
- Burgers, W.A.; Shephard, E.; Monroe, J.E.; Greenhalgh, T.; Binder, A.; Hurter, E.; Van Harmelen, J.H.; Williamson, C.; Williamson, A.L. Construction, characterization, and immunogenicity of a multigene modified vaccinia Ankara (MVA) vaccine based on HIV type 1 subtype C. AIDS Res. Hum. Retrovir. 2008, 24, 195–206. [Google Scholar] [CrossRef]
- Barouch, D.H.; Liu, J.; Li, H.; Maxfield, L.F.; Abbink, P.; Lynch, D.M.; Iampietro, M.J.; SanMiguel, A.; Seaman, M.S.; Ferrari, G.; et al. Vaccine protection against acquisition of neutralization-resistant SIV challenges in rhesus monkeys. Nature 2012, 482, 89–93. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Julien, J.P.; Lee, J.H.; Ozorowski, G.; Hua, Y.; Torrents de la Pena, A.; de Taeye, S.W.; Nieusma, T.; Cupo, A.; Yasmeen, A.; Golabek, M.; et al. Design and structure of two HIV-1 clade C SOSIP.664 trimers that increase the arsenal of native-like Env immunogens. Proc. Natl. Acad. Sci. USA 2015, 112, 11947–11952. [Google Scholar] [CrossRef] [Green Version]
- Dubrovskaya, V.; Guenaga, J.; de Val, N.; Wilson, R.; Feng, Y.; Movsesyan, A.; Karlsson Hedestam, G.B.; Ward, A.B.; Wyatt, R.T. Targeted N-glycan deletion at the receptor-binding site retains HIV Env NFL trimer integrity and accelerates the elicited antibody response. PLoS Pathog. 2017, 13, e1006614. [Google Scholar] [CrossRef] [PubMed]
- Guenaga, J.; Dubrovskaya, V.; de Val, N.; Sharma, S.K.; Carrette, B.; Ward, A.B.; Wyatt, R.T. Structure-Guided Redesign Increases the Propensity of HIV Env To Generate Highly Stable Soluble Trimers. J. Virol. 2015, 90, 2806–2817. [Google Scholar] [CrossRef] [Green Version]
- Guenaga, J.; Garces, F.; de Val, N.; Stanfield, R.L.; Dubrovskaya, V.; Higgins, B.; Carrette, B.; Ward, A.B.; Wilson, I.A.; Wyatt, R.T. Glycine Substitution at Helix-to-Coil Transitions Facilitates the Structural Determination of a Stabilized Subtype C HIV Envelope Glycoprotein. Immunity 2017, 46, 792–803.e3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martinez-Murillo, P.; Tran, K.; Guenaga, J.; Lindgren, G.; Adori, M.; Feng, Y.; Phad, G.E.; Vazquez Bernat, N.; Bale, S.; Ingale, J.; et al. Particulate Array of Well-Ordered HIV Clade C Env Trimers Elicits Neutralizing Antibodies that Display a Unique V2 Cap Approach. Immunity 2017, 46, 804–817.e7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ringe, R.P.; Ozorowski, G.; Yasmeen, A.; Cupo, A.; Cruz Portillo, V.M.; Pugach, P.; Golabek, M.; Rantalainen, K.; Holden, L.G.; Cottrell, C.A.; et al. Improving the Expression and Purification of Soluble, Recombinant Native-Like HIV-1 Envelope Glycoprotein Trimers by Targeted Sequence Changes. J. Virol. 2017, 91. [Google Scholar] [CrossRef] [Green Version]
- Ringe, R.P.; Yasmeen, A.; Ozorowski, G.; Go, E.P.; Pritchard, L.K.; Guttman, M.; Ketas, T.A.; Cottrell, C.A.; Wilson, I.A.; Sanders, R.W.; et al. Influences on the Design and Purification of Soluble, Recombinant Native-Like HIV-1 Envelope Glycoprotein Trimers. J. Virol. 2015, 89, 12189–12210. [Google Scholar] [CrossRef] [Green Version]
- Yates, N.L.; Liao, H.X.; Fong, Y.; deCamp, A.; Vandergrift, N.A.; Williams, W.T.; Alam, S.M.; Ferrari, G.; Yang, Z.Y.; Seaton, K.E.; et al. Vaccine-induced Env V1-V2 IgG3 correlates with lower HIV-1 infection risk and declines soon after vaccination. Sci. Transl. Med. 2014, 6, 228ra239. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xiao, P.; Zhao, J.; Patterson, L.J.; Brocca-Cofano, E.; Venzon, D.; Kozlowski, P.A.; Hidajat, R.; Demberg, T.; Robert-Guroff, M. Multiple vaccine-elicited nonneutralizing antienvelope antibody activities contribute to protective efficacy by reducing both acute and chronic viremia following simian/human immunodeficiency virus SHIV89.6P challenge in rhesus macaques. J. Virol. 2010, 84, 7161–7173. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wines, B.D.; Billings, H.; McLean, M.R.; Kent, S.J.; Hogarth, P.M. Antibody Functional Assays as Measures of Fc Receptor-Mediated Immunity to HIV—New Technologies and their Impact on the HIV Vaccine Field. Curr. HIV Res. 2017, 15, 202–215. [Google Scholar] [CrossRef] [Green Version]
- Veillette, M.; Richard, J.; Pazgier, M.; Lewis, G.K.; Parsons, M.S.; Finzi, A. Role of HIV-1 Envelope Glycoproteins Conformation and Accessory Proteins on ADCC Responses. Curr. HIV Res. 2016, 14, 9–23. [Google Scholar] [CrossRef] [PubMed]
- Alter, G.; Barouch, D. Immune Correlate-Guided HIV Vaccine Design. Cell Host Microbe 2018, 24, 25–33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Montefiori, D.C.; Roederer, M.; Morris, L.; Seaman, M.S. Neutralization tiers of HIV-1. Curr. Opin. HIV AIDS 2018, 13, 128–136. [Google Scholar] [CrossRef]
- Ruprecht, R.M.; Marasini, B.; Thippeshappa, R. Mucosal Antibodies: Defending Epithelial Barriers against HIV-1 Invasion. Vaccines 2019, 7, 194. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Burton, S.L.; Kilgore, K.M.; Smith, S.A.; Reddy, S.; Hunter, E.; Robinson, H.L.; Silvestri, G.; Amara, R.R.; Derdeyn, C.A. Breakthrough of SIV strain smE660 challenge in SIV strain mac239-vaccinated rhesus macaques despite potent autologous neutralizing antibody responses. Proc. Natl. Acad. Sci. USA 2015, 112, 10780–10785. [Google Scholar] [CrossRef] [Green Version]
- Corey, L.; Gilbert, P.B.; Juraska, M.; Montefiori, D.C.; Morris, L.; Karuna, S.T.; Edupuganti, S.; Mgodi, N.M.; deCamp, A.C.; Rudnicki, E.; et al. Two Randomized Trials of Neutralizing Antibodies to Prevent HIV-1 Acquisition. N. Engl. J. Med. 2021, 384, 1003–1014. [Google Scholar] [CrossRef]
- Garcia-Arriaza, J.; Perdiguero, B.; Heeney, J.; Seaman, M.; Montefiori, D.C.; Labranche, C.; Yates, N.L.; Shen, X.; Tomaras, G.D.; Ferrari, G.; et al. Head-to-Head Comparison of Poxvirus NYVAC and ALVAC Vectors Expressing Identical HIV-1 Clade C Immunogens in Prime-Boost Combination with Env Protein in Nonhuman Primates. J. Virol. 2015, 89, 8525–8539. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fouts, T.R.; Bagley, K.; Prado, I.J.; Bobb, K.L.; Schwartz, J.A.; Xu, R.; Zagursky, R.J.; Egan, M.A.; Eldridge, J.H.; LaBranche, C.C.; et al. Balance of cellular and humoral immunity determines the level of protection by HIV vaccines in rhesus macaque models of HIV infection. Proc. Natl. Acad. Sci. USA 2015, 112, E992–E999. [Google Scholar] [CrossRef] [Green Version]
- Hamdi, J.; Boumart, Z.; Daouam, S.; El Arkam, A.; Bamouh, Z.; Jazouli, M.; Tadlaoui, K.O.; Fihri, O.F.; Gavrilov, B.; El Harrak, M. Development and Evaluation of an Inactivated Lumpy Skin Disease Vaccine for Cattle. Vet. Microbiol. 2020, 245, 108689. [Google Scholar] [CrossRef] [PubMed]
- Hamdi, J.; Munyanduki, H.; Omari Tadlaoui, K.; El Harrak, M.; Fassi Fihri, O. Capripoxvirus Infections in Ruminants: A Review. Microorganisms 2021, 9, 902. [Google Scholar] [CrossRef] [PubMed]
- Wallace, D.B.; Mather, A.; Kara, P.D.; Naicker, L.; Mokoena, N.B.; Pretorius, A.; Nefefe, T.; Thema, N.; Babiuk, S. Protection of Cattle Elicited Using a Bivalent Lumpy Skin Disease Virus-Vectored Recombinant Rift Valley Fever Vaccine. Front. Vet. Sci. 2020, 7, 256. [Google Scholar] [CrossRef] [PubMed]



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chapman, R.; van Diepen, M.; Douglass, N.; Galant, S.; Jaffer, M.; Margolin, E.; Ximba, P.; Hermanus, T.; Moore, P.L.; Williamson, A.-L. Assessment of an LSDV-Vectored Vaccine for Heterologous Prime-Boost Immunizations against HIV. Vaccines 2021, 9, 1281. https://doi.org/10.3390/vaccines9111281
Chapman R, van Diepen M, Douglass N, Galant S, Jaffer M, Margolin E, Ximba P, Hermanus T, Moore PL, Williamson A-L. Assessment of an LSDV-Vectored Vaccine for Heterologous Prime-Boost Immunizations against HIV. Vaccines. 2021; 9(11):1281. https://doi.org/10.3390/vaccines9111281
Chicago/Turabian StyleChapman, Ros, Michiel van Diepen, Nicola Douglass, Shireen Galant, Mohamed Jaffer, Emmanuel Margolin, Phindile Ximba, Tandile Hermanus, Penny L. Moore, and Anna-Lise Williamson. 2021. "Assessment of an LSDV-Vectored Vaccine for Heterologous Prime-Boost Immunizations against HIV" Vaccines 9, no. 11: 1281. https://doi.org/10.3390/vaccines9111281





