Attitude towards HPV Vaccination and the Intention to Get Vaccinated among Female University Students in Health Schools in Jordan
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Survey Items
2.3. Study Measures
2.4. Statistical Analysis
3. Results
3.1. Characteristics of the Study Participants
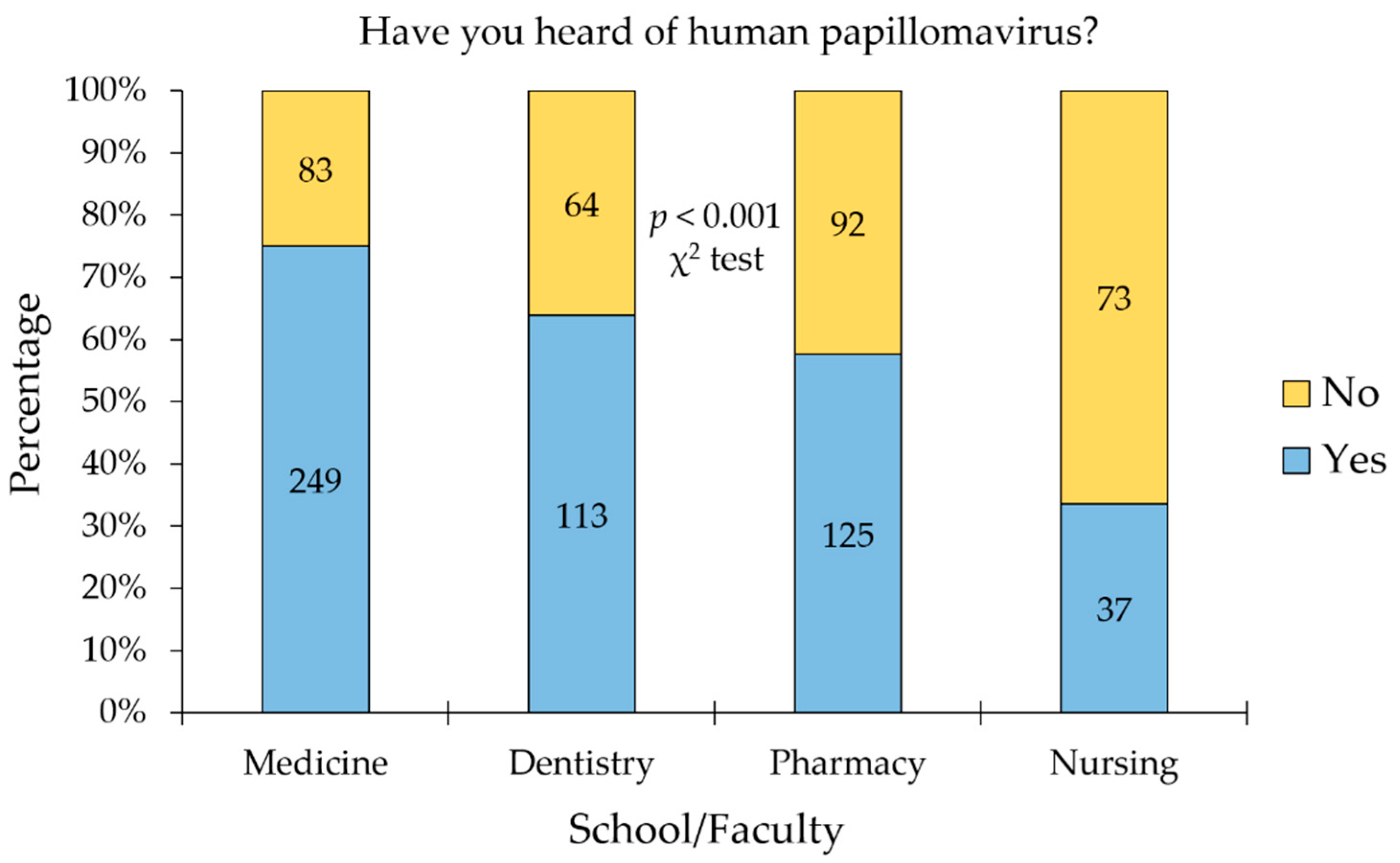
3.2. Prior Knowledge of HPV among the Study Participants
3.3. Overall Level of HPV Knowledge among the Students Who Have Heard of the Virus
3.4. History of HPV Vaccination and the Intentions to Get Vaccinated
3.5. Factors Associated with Unwillingness to Get the HPV Vaccination
3.6. Vaccine Conspiracy Beliefs Were Associated with a Lower Intent to Get HPV Vaccination
3.7. Sources of Knowledge Regarding HPV among the Study Sample
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Arbyn, M.; Weiderpass, E.; Bruni, L.; de Sanjosé, S.; Saraiya, M.; Ferlay, J.; Bray, F. Estimates of incidence and mortality of cervical cancer in 2018: A worldwide analysis. Lancet. Glob. Health 2020, 8, e191–e203. [Google Scholar] [CrossRef] [Green Version]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Zeng, Q.; Cai, W.; Ruan, W. Trends of cervical cancer at global, regional, and national level: Data from the Global Burden of Disease study 2019. BMC Public Health 2021, 21, 894. [Google Scholar] [CrossRef] [PubMed]
- Canfell, K.; Kim, J.J.; Brisson, M.; Keane, A.; Simms, K.T.; Caruana, M.; Burger, E.A.; Martin, D.; Nguyen, D.T.N.; Bénard, É.; et al. Mortality impact of achieving WHO cervical cancer elimination targets: A comparative modelling analysis in 78 low-income and lower-middle-income countries. Lancet 2020, 395, 591–603. [Google Scholar] [CrossRef] [Green Version]
- Burd, E.M. Human papillomavirus and cervical cancer. Clin. Microbiol. Rev. 2003, 16, 1–17. [Google Scholar] [CrossRef] [Green Version]
- Kombe Kombe, A.J.; Li, B.; Zahid, A.; Mengist, H.M.; Bounda, G.A.; Zhou, Y.; Jin, T. Epidemiology and Burden of Human Papillomavirus and Related Diseases, Molecular Pathogenesis, and Vaccine Evaluation. Front. Public Health 2020, 8, 552028. [Google Scholar] [CrossRef]
- Chesson, H.W.; Dunne, E.F.; Hariri, S.; Markowitz, L.E. The estimated lifetime probability of acquiring human papillomavirus in the United States. Sex. Transm. Dis. 2014, 41, 660–664. [Google Scholar] [CrossRef]
- Yanofsky, V.R.; Patel, R.V.; Goldenberg, G. Genital warts: A comprehensive review. J. Clin. Aesthet. Dermatol. 2012, 5, 25–36. [Google Scholar]
- Chan, C.K.; Aimagambetova, G.; Ukybassova, T.; Kongrtay, K.; Azizan, A. Human Papillomavirus Infection and Cervical Cancer: Epidemiology, Screening, and Vaccination—Review of Current Perspectives. J. Oncol. 2019, 2019, 3257939. [Google Scholar] [CrossRef]
- Jensen, K.E.; Schmiedel, S.; Norrild, B.; Frederiksen, K.; Iftner, T.; Kjaer, S.K. Parity as a cofactor for high-grade cervical disease among women with persistent human papillomavirus infection: A 13-year follow-up. Br. J. Cancer 2013, 108, 234–239. [Google Scholar] [CrossRef] [Green Version]
- Zhu, H.; Shen, Z.; Luo, H.; Zhang, W.; Zhu, X. Chlamydia Trachomatis Infection-Associated Risk of Cervical Cancer: A Meta-Analysis. Medicine 2016, 95, e3077. [Google Scholar] [CrossRef]
- Sugawara, Y.; Tsuji, I.; Mizoue, T.; Inoue, M.; Sawada, N.; Matsuo, K.; Ito, H.; Naito, M.; Nagata, C.; Kitamura, Y.; et al. Cigarette smoking and cervical cancer risk: An evaluation based on a systematic review and meta-analysis among Japanese women. Jpn. J. Clin. Oncol. 2019, 49, 77–86. [Google Scholar] [CrossRef]
- Braaten, K.P.; Laufer, M.R. Human Papillomavirus (HPV), HPV-Related Disease, and the HPV Vaccine. Rev. Obstet. Gynecol. 2008, 1, 2–10. [Google Scholar]
- Boda, D.; Docea, A.O.; Calina, D.; Ilie, M.A.; Caruntu, C.; Zurac, S.; Neagu, M.; Constantin, C.; Branisteanu, D.E.; Voiculescu, V.; et al. Human papilloma virus: Apprehending the link with carcinogenesis and unveiling new research avenues (Review). Int. J. Oncol. 2018, 52, 637–655. [Google Scholar] [CrossRef] [Green Version]
- Lawson, J.S.; Glenn, W.K. Evidence for a causal role by human papillomaviruses in prostate cancer—A systematic review. Infect. Agents Cancer 2020, 15, 41. [Google Scholar] [CrossRef]
- De Martel, C.; Georges, D.; Bray, F.; Ferlay, J.; Clifford, G.M. Global burden of cancer attributable to infections in 2018: A worldwide incidence analysis. Lancet Glob. Health 2020, 8, e180–e190. [Google Scholar] [CrossRef] [Green Version]
- Dadar, M.; Chakraborty, S.; Dhama, K.; Prasad, M.; Khandia, R.; Hassan, S.; Munjal, A.; Tiwari, R.; Karthik, K.; Kumar, D.; et al. Advances in Designing and Developing Vaccines, Drugs and Therapeutic Approaches to Counter Human Papilloma Virus. Front. Immunol. 2018, 9, 2478. [Google Scholar] [CrossRef]
- Safaeian, M.; Solomon, D.; Castle, P.E. Cervical cancer prevention-cervical screening: Science in evolution. Obs. Gynecol. Clin. N. Am. 2007, 34, 739–760. [Google Scholar] [CrossRef] [Green Version]
- Watson, M.; Benard, V.; King, J.; Crawford, A.; Saraiya, M. National assessment of HPV and Pap tests: Changes in cervical cancer screening, National Health Interview Survey. Prev. Med. 2017, 100, 243–247. [Google Scholar] [CrossRef]
- Fokom Domgue, J.; Valea, F.A. Is It Relevant to Keep Advocating Visual Inspection of the Cervix with Acetic Acid for Primary Cervical Cancer Screening in Limited-Resource Settings? J. Glob. Oncol. 2018, 4, 1–5. [Google Scholar] [CrossRef]
- Cubie, H.A.; Campbell, C. Cervical cancer screening—The challenges of complete pathways of care in low-income countries: Focus on Malawi. Womens Health 2020, 16, 1745506520914804. [Google Scholar] [CrossRef] [PubMed]
- Catarino, R.; Petignat, P.; Dongui, G.; Vassilakos, P. Cervical cancer screening in developing countries at a crossroad: Emerging technologies and policy choices. World J. Clin. Oncol. 2015, 6, 281–290. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Comprehensive Cervical Cancer Control: A Guide to Essential Practice. Available online: https://www.who.int/reproductivehealth/publications/cancers/cervical-cancer-guide/en/ (accessed on 27 October 2021).
- Cheng, L.; Wang, Y.; Du, J. Human Papillomavirus Vaccines: An Updated Review. Vaccines 2020, 8, 391. [Google Scholar] [CrossRef] [PubMed]
- Schiller, J.; Lowy, D. Explanations for the high potency of HPV prophylactic vaccines. Vaccine 2018, 36, 4768–4773. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Pan, W.; Jin, L.; Huang, W.; Li, Y.; Wu, D.; Gao, C.; Ma, D.; Liao, S. Human papillomavirus vaccine against cervical cancer: Opportunity and challenge. Cancer Lett. 2020, 471, 88–102. [Google Scholar] [CrossRef] [PubMed]
- Meites, E.; Szilagyi, P.G.; Chesson, H.W.; Unger, E.R.; Romero, J.R.; Markowitz, L.E. Human Papillomavirus Vaccination for Adults: Updated Recommendations of the Advisory Committee on Immunization Practices. MMWR Morb. Mortal. Wkly. Rep. 2019, 68, 698–702. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, J.J.; Simms, K.T.; Killen, J.; Smith, M.A.; Burger, E.A.; Sy, S.; Regan, C.; Canfell, K. Human papillomavirus vaccination for adults aged 30 to 45 years in the United States: A cost-effectiveness analysis. PLoS Med. 2021, 18, e1003534. [Google Scholar] [CrossRef] [PubMed]
- Garbuglia, A.R.; Lapa, D.; Sias, C.; Capobianchi, M.R.; Del Porto, P. The Use of Both Therapeutic and Prophylactic Vaccines in the Therapy of Papillomavirus Disease. Front. Immunol. 2020, 11, 188. [Google Scholar] [CrossRef] [Green Version]
- Di Donato, V.; Caruso, G.; Petrillo, M.; Kontopantelis, E.; Palaia, I.; Perniola, G.; Plotti, F.; Angioli, R.; Muzii, L.; Benedetti Panici, P.; et al. Adjuvant HPV Vaccination to Prevent Recurrent Cervical Dysplasia after Surgical Treatment: A Meta-Analysis. Vaccines 2021, 9, 410. [Google Scholar] [CrossRef]
- Petrillo, M.; Dessole, M.; Tinacci, E.; Saderi, L.; Muresu, N.; Capobianco, G.; Cossu, A.; Dessole, S.; Sotgiu, G.; Piana, A. Efficacy of HPV Vaccination in Women Receiving LEEP for Cervical Dysplasia: A Single Institution’s Experience. Vaccines 2020, 8, 45. [Google Scholar] [CrossRef] [Green Version]
- The HPV Information Centre. Jordan: Human Papillomavirus and Related Cancers, Fact Sheet 2021. Available online: https://hpvcentre.net/statistics/reports/JOR_FS.pdf (accessed on 7 November 2021).
- Sharkas, G.; Arqoub, K.; Khader, Y.; Nimri, O.; Shroukh, W.; Jadallah, H.; Saheb, T. Trends in the Incidence of Cervical Cancer in Jordan, 2000–2013. J. Oncol. 2017, 2017, 6827384. [Google Scholar] [CrossRef] [Green Version]
- Mahafzah, A.M.; Al-Ramahi, M.Q.; Asa’d, A.M.; El-Khateeb, M.S. Prevalence of sexually transmitted infections among sexually active Jordanian females. Sex. Transm. Dis. 2008, 35, 607–610. [Google Scholar] [CrossRef]
- Abu-Lubad, M.A.; Jarajreh, D.a.A.; Helaly, G.F.; Alzoubi, H.M.; Haddadin, W.J.; Dabobash, M.D.; Albataineh, E.M.; Aqel, A.A.; Alnawaiseh, N.A. Human papillomavirus as an independent risk factor of invasive cervical and endometrial carcinomas in Jordan. J. Infect. Public Health 2020, 13, 613–618. [Google Scholar] [CrossRef]
- Obeidat, B.; Matalka, I.; Mohtaseb, A.; Jaradat, S.; Hayajneh, W.; Khasawneh, R.; Haddad, H.; Obeidat, F. Prevalence and distribution of high-risk human papillomavirus genotypes in cervical carcinoma, low-grade, and high-grade squamous intraepithelial lesions in Jordanian women. Eur. J. Gynaecol. Oncol. 2013, 34, 257–260. [Google Scholar]
- Maraqa, B.; Lataifeh, I.; Otay, L.; Badran, O.; Qutaiba Nouri, Y.; Issam, I.; Al Hussaini, M. Prevalence of Abnormal Pap Smears: A Descriptive Study from a Cancer Center in a Low-Prevalence Community. Asian Pac. J. Cancer Prev. 2017, 18, 3117–3121. [Google Scholar] [CrossRef]
- Abu Qatouseh, L.; Sabri, I.; Alkhatib, I.; Atwa, E.; Arafat, T. Detection of High-Risk Human Papillomavirus Genotypes 16 and 18 in Head and Neck Squamous Cell Carcinomas in Jordan. Asian Pac. J. Cancer Prev. 2017, 18, 1337–1341. [Google Scholar] [CrossRef]
- Khasawneh, A.I.; Himsawi, N.; Abu-Raideh, J.; Salameh, M.; Abdullah, N.; Khasawneh, R.; Saleh, T. Prevalence of human papillomavirus associated with head and neck squamous cell carcinoma in Jordanian patients. Open Microbiol. J. 2020, 14, 57–64. [Google Scholar] [CrossRef]
- Sallam, M.; Dababseh, D.; Yaseen, A.; Al-Haidar, A.; Ettarras, H.; Jaafreh, D.; Hasan, H.; Al-Salahat, K.; Al-Fraihat, E.; Hassona, Y.; et al. Lack of knowledge regarding HPV and its relation to oropharyngeal cancer among medical students. Cancer Rep. 2021, e1517. [Google Scholar] [CrossRef]
- Sallam, M.; Al-Fraihat, E.; Dababseh, D.; Yaseen, A.; Taim, D.; Zabadi, S.; Hamdan, A.A.; Hassona, Y.; Mahafzah, A.; Şahin, G. Dental students’ awareness and attitudes toward HPV-related oral cancer: A cross sectional study at the University of Jordan. BMC Oral Health 2019, 19, 171. [Google Scholar] [CrossRef] [Green Version]
- Lataifeh, I.; Al Chalabi, H.; Faleh, N.; Yousef, L.; Al Jallad, M.; Asfour, Y. A survey of knowledge and awareness of Jordanian female university students of human papillomavirus infection and its vaccine. Eur. J. Gynaecol. Oncol. 2016, 37, 796–799. [Google Scholar]
- Alsous, M.M.; Ali, A.; Al-Azzam, S.; Karasneh, R.; Amawi, H. Knowledge about cervical cancer and awareness about human papillomavirus vaccination among medical students in Jordan. PeerJ 2021, 9, e11611. [Google Scholar] [CrossRef] [PubMed]
- Lataifeh, I.; Obeidat, N.; Al-Mehaisen, L.; Khriesat, W.; Tadros, R.; Khader, Y.; Al-Sukhun, S. A survey of Jordanian obstetricians and gynecologists’ knowledge and attitudes toward human papillomavirus infection and vaccination. Eur. J. Gynaecol. Oncol. 2014, 35, 429–432. [Google Scholar] [PubMed]
- Waller, J.; Ostini, R.; Marlow, L.A.; McCaffery, K.; Zimet, G. Validation of a measure of knowledge about human papillomavirus (HPV) using item response theory and classical test theory. Prev. Med. 2013, 56, 35–40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shapiro, G.K.; Holding, A.; Perez, S.; Amsel, R.; Rosberger, Z. Validation of the vaccine conspiracy beliefs scale. Papillomavirus Res. 2016, 2, 167–172. [Google Scholar] [CrossRef] [Green Version]
- Thomas, T.; Dalmida, S.; Higgins, M. The Student Human Papillomavirus Survey: Nurse-Led Instrument Development and Psychometric Testing to Increase Human Papillomavirus Vaccine Series Completion in Young Adults. J. Nurs. Meas. 2016, 24, 226–244. [Google Scholar] [CrossRef] [Green Version]
- Kellogg, C.; Shu, J.; Arroyo, A.; Dinh, N.T.; Wade, N.; Sanchez, E.; Equils, O. A significant portion of college students are not aware of HPV disease and HPV vaccine recommendations. Hum. Vaccines Immunother. 2019, 15, 1760–1766. [Google Scholar] [CrossRef]
- CheckMarket. CheckMarket: Sample Size Calculator. Available online: https://www.checkmarket.com/ (accessed on 27 October 2021).
- Bal-Yılmaz, H.; Koniak-Griffin, D. Knowledge, Behaviors, and Attitudes about Human Papilloma Virus among Nursing Students in Izmir, Turkey. J. Cancer Educ. Off. J. Am. Assoc. Cancer Educ. 2018, 33, 814–820. [Google Scholar] [CrossRef]
- Villanueva, S.; Mosteiro-Miguéns, D.G.; Domínguez-Martís, E.M.; López-Ares, D.; Novío, S. Knowledge, Attitudes, and Intentions towards Human Papillomavirus Vaccination among Nursing Students in Spain. Int. J. Environ. Res. Public Health 2019, 16, 4507. [Google Scholar] [CrossRef] [Green Version]
- Shetty, S.; Shetty, V.; Badiger, S.; Shetty, A.K. An exploratory study of undergraduate healthcare student perspectives regarding human papillomavirus and vaccine intent in India. Women’s Health 2021, 17, 17455065211055304. [Google Scholar] [CrossRef]
- Hussain, A.N.; Alkhenizan, A.; McWalter, P.; Qazi, N.; Alshmassi, A.; Farooqi, S.; Abdulkarim, A. Attitudes and perceptions towards HPV vaccination among young women in Saudi Arabia. J. Fam. Community Med. 2016, 23, 145–150. [Google Scholar] [CrossRef] [Green Version]
- Alsous, M.M.; Ali, A.A.; Al-Azzam, S.I.; Abdel Jalil, M.H.; Al-Obaidi, H.J.; Al-Abbadi, E.I.; Hussain, Z.K.; Jirjees, F.J. Knowledge and awareness about human papillomavirus infection and its vaccination among women in Arab communities. Sci. Rep. 2021, 11, 786. [Google Scholar] [CrossRef]
- Dany, M.; Chidiac, A.; Nassar, A.H. Human papillomavirus vaccination: Assessing knowledge, attitudes, and intentions of college female students in Lebanon, a developing country. Vaccine 2015, 33, 1001–1007. [Google Scholar] [CrossRef]
- Makwe, C.C.; Anorlu, R.I.; Odeyemi, K.A. Human papillomavirus (HPV) infection and vaccines: Knowledge, attitude and perception among female students at the University of Lagos, Lagos, Nigeria. J. Epidemiol. Glob. Health 2012, 2, 199–206. [Google Scholar] [CrossRef] [Green Version]
- Farsi, N.J.; Baharoon, A.H.; Jiffri, A.E.; Marzouki, H.Z.; Merdad, M.A.; Merdad, L.A. Human papillomavirus knowledge and vaccine acceptability among male medical students in Saudi Arabia. Hum. Vaccines Immunother. 2021, 17, 1968–1974. [Google Scholar] [CrossRef]
- Browne, M.; Thomson, P.; Rockloff, M.J.; Pennycook, G. Going against the Herd: Psychological and Cultural Factors Underlying the ‘Vaccination Confidence Gap’. PLoS ONE 2015, 10, e0132562. [Google Scholar] [CrossRef] [Green Version]
- Albanghali, M.A.; Othman, B.A. A Cross-Sectional Study on the Knowledge of Sexually Transmitted Diseases among Young Adults Living in Albaha, Saudi Arabia. Int. J. Environ. Res. Public Health 2020, 17, 1872. [Google Scholar] [CrossRef] [Green Version]
- Ferrer, H.B.; Trotter, C.; Hickman, M.; Audrey, S. Barriers and facilitators to HPV vaccination of young women in high-income countries: A qualitative systematic review and evidence synthesis. BMC Public Health 2014, 14, 700. [Google Scholar] [CrossRef] [Green Version]
- Khatiwada, M.; Kartasasmita, C.; Mediani, H.S.; Delprat, C.; Van Hal, G.; Dochez, C. Knowledge, Attitude and Acceptability of the Human Papilloma Virus Vaccine and Vaccination among University Students in Indonesia. Front. Public Health 2021, 9, 607. [Google Scholar] [CrossRef]
- Badgujar, V.B.; Ahmad Fadzil, F.S.; Balbir Singh, H.K.; Sami, F.; Badgujar, S.; Ansari, M.T. Knowledge, understanding, attitude, perception and views on HPV infection and vaccination among health care students and professionals in Malaysia. Hum. Vaccines Immunother. 2019, 15, 156–162. [Google Scholar] [CrossRef] [Green Version]
- Rajiah, K.; Maharajan, M.K.; Chin, N.S.; Num, K.S.F. Awareness and acceptance of human papillomavirus vaccination among health sciences students in Malaysia. Virusdisease 2015, 26, 297–303. [Google Scholar] [CrossRef] [Green Version]
- Muhamad, N.A.; Buang, S.N.; Jaafar, S.; Jais, R.; Tan, P.S.; Mustapha, N.; Lodz, N.A.; Aris, T.; Sulaiman, L.H.; Murad, S. Achieving high uptake of human papillomavirus vaccination in Malaysia through school-based vaccination programme. BMC Public Health 2018, 18, 1402. [Google Scholar] [CrossRef] [PubMed]
- Farsi, N.J.; Al Sharif, S.; Al Qathmi, M.; Merdad, M.; Marzouki, H.; Merdad, L. Knowledge of Human Papillomavirus (HPV) and Oropharyngeal Cancer and Acceptability of the HPV Vaccine among Dental Students. Asian Pac. J. Cancer Prev. 2020, 21, 3595–3603. [Google Scholar] [CrossRef] [PubMed]
- Patel, D.A.; Zochowski, M.; Peterman, S.; Dempsey, A.F.; Ernst, S.; Dalton, V.K. Human papillomavirus vaccine intent and uptake among female college students. J. Am. Coll. Health 2012, 60, 151–161. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, Y.; Di, N.; Tao, X. Knowledge, practice and attitude towards HPV vaccination among college students in Beijing, China. Hum. Vaccines Immunother. 2020, 16, 116–123. [Google Scholar] [CrossRef]
- You, D.; Han, L.; Li, L.; Hu, J.; Zimet, G.D.; Alias, H.; Danaee, M.; Cai, L.; Zeng, F.; Wong, L.P. Human Papillomavirus (HPV) Vaccine Uptake and the Willingness to Receive the HPV Vaccination among Female College Students in China: A Multicenter Study. Vaccines 2020, 8, 31. [Google Scholar] [CrossRef] [Green Version]
- Yin, G.; Zhang, Y.; Chen, C.; Ren, H.; Guo, B.; Zhang, M. Have you ever heard of Human Papillomavirus (HPV) vaccine? The awareness of HPV vaccine for college students in China based on meta-analysis. Hum. Vaccines Immunother. 2021, 17, 2736–2747. [Google Scholar] [CrossRef]
- Trucchi, C.; Amicizia, D.; Tafuri, S.; Sticchi, L.; Durando, P.; Costantino, C.; Varlese, F.; Silverio, B.D.; Bagnasco, A.M.; Ansaldi, F.; et al. Assessment of Knowledge, Attitudes, and Propensity towards HPV Vaccine of Young Adult Students in Italy. Vaccines 2020, 8, 74. [Google Scholar] [CrossRef] [Green Version]
- Wirawan, G.B.S.; Mahardani, P.; Cahyani, M.R.K.; Laksmi, N.; Januraga, P.P. Conspiracy beliefs and trust as determinants of COVID-19 vaccine acceptance in Bali, Indonesia: Cross-sectional study. Pers. Individ. Differ. 2021, 180, 110995. [Google Scholar] [CrossRef]
- Tomljenovic, H.; Bubic, A.; Erceg, N. It just doesn’t feel right—The relevance of emotions and intuition for parental vaccine conspiracy beliefs and vaccination uptake. Psychol. Health 2020, 35, 538–554. [Google Scholar] [CrossRef]
- Andrade, G. COVID-19 vaccine hesitancy, conspiracist beliefs, paranoid ideation and perceived ethnic discrimination in a sample of University students in Venezuela. Vaccine 2021, 39, 6837–6842. [Google Scholar] [CrossRef]
- Sallam, M.; Dababseh, D.; Eid, H.; Hasan, H.; Taim, D.; Al-Mahzoum, K.; Al-Haidar, A.; Yaseen, A.; Ababneh, N.A.; Assaf, A.; et al. Low COVID-19 Vaccine Acceptance Is Correlated with Conspiracy Beliefs among University Students in Jordan. Int. J. Environ. Res. Public Health 2021, 18, 2407. [Google Scholar] [CrossRef]
- Mavundza, E.J.; Iwu-Jaja, C.J.; Wiyeh, A.B.; Gausi, B.; Abdullahi, L.H.; Halle-Ekane, G.; Wiysonge, C.S. A Systematic Review of Interventions to Improve HPV Vaccination Coverage. Vaccines 2021, 9, 687. [Google Scholar] [CrossRef]
- Barnard, M.; Cole, A.C.; Ward, L.; Gravlee, E.; Cole, M.L.; Compretta, C. Interventions to increase uptake of the human papillomavirus vaccine in unvaccinated college students: A systematic literature review. Prev. Med. Rep. 2019, 14, 100884. [Google Scholar] [CrossRef]
- Massey, P.M.; Kearney, M.D.; Hauer, M.K.; Selvan, P.; Koku, E.; Leader, A.E. Dimensions of Misinformation about the HPV Vaccine on Instagram: Content and Network Analysis of Social Media Characteristics. J. Med. Internet Res. 2020, 22, e21451. [Google Scholar] [CrossRef]
- Ekram, S.; Debiec, K.E.; Pumper, M.A.; Moreno, M.A. Content and Commentary: HPV Vaccine and YouTube. J. Pediatr. Adolesc. Gynecol. 2019, 32, 153–157. [Google Scholar] [CrossRef]
- Sallam, M.; Dababseh, D.; Yaseen, A.; Al-Haidar, A.; Taim, D.; Eid, H.; Ababneh, N.A.; Bakri, F.G.; Mahafzah, A. COVID-19 misinformation: Mere harmless delusions or much more? A knowledge and attitude cross-sectional study among the general public residing in Jordan. PLoS ONE 2020, 15, e0243264. [Google Scholar] [CrossRef]
- Sallam, M.; Dababseh, D.; Eid, H.; Al-Mahzoum, K.; Al-Haidar, A.; Taim, D.; Yaseen, A.; Ababneh, N.A.; Bakri, F.G.; Mahafzah, A. High Rates of COVID-19 Vaccine Hesitancy and Its Association with Conspiracy Beliefs: A Study in Jordan and Kuwait among Other Arab Countries. Vaccines 2021, 9, 42. [Google Scholar] [CrossRef]
- Sallam, M.; Dababseh, D.; Yaseen, A.; Al-Haidar, A.; Ababneh, N.A.; Bakri, F.G.; Mahafzah, A. Conspiracy Beliefs Are Associated with Lower Knowledge and Higher Anxiety Levels Regarding COVID-19 among Students at the University of Jordan. Int. J. Environ. Res. Public Health 2020, 17, 4915. [Google Scholar] [CrossRef]



| Variable | Category | School/Faculty | |||
|---|---|---|---|---|---|
| Medicine | Dentistry | Pharmacy | Nursing | ||
| n 2 (%) | n (%) | n (%) | n (%) | ||
| Age | Less than 20 years | 124 (37.35) | 76 (42.94) | 25 (11.52) | 42 (38.18) |
| 20–22 years | 174 (52.41) | 83 (46.89) | 134 (61.75) | 59 (53.64) | |
| More than 22 years | 34 (10.24) | 18 (10.17) | 58 (26.73) | 9 (8.18) | |
| Nationality | Jordanian | 197 (59.34) | 106 (59.89) | 177 (81.57) | 107 (97.27) |
| Kuwaiti | 103 (31.02) | 53 (29.94) | 22 (10.14) | 0 | |
| Palestinian | 10 (3.01) | 11 (6.21) | 4 (1.84) | 3 (2.73) | |
| Iraqi | 15 (4.52) | 3 (1.69) | 6 (2.76) | 0 | |
| Syrian | 2 (0.60) | 2 (1.13) | 5 (2.30) | 0 | |
| Other (Arab) | 5 (1.51) | 2 (1.13) | 3 (1.38) | 0 | |
| University | Public | 332 (100.00) | 177 (100.00) | 182 (83.87) | 109 (99.09) |
| Private | 0 | 0 | 35 (16.13) | 1 (0.91) | |
| Monthly income of household | Less than or equal to 1000 JOD 1 | 87 (26.20) | 66 (37.29) | 129 (59.45) | 85 (77.27) |
| More than 1000 JOD | 245 (73.80) | 111 (62.71) | 88 (40.55) | 25 (22.73) | |
| HPV Knowledge Item | Response | School/Faculty | p Value 2 | |||
|---|---|---|---|---|---|---|
| Medicine | Dentistry | Pharmacy | Nursing | |||
| n 1 (%) | n (%) | n (%) | n (%) | |||
| HPV infections are rare * | Correct | 157 (63.05) | 82 (72.57) | 59 (47.20) | 15 (40.54) | <0.001 |
| Incorrect | 92 (36.95) | 31 (27.43) | 66 (52.80) | 22 (59.46) | ||
| HPV is sexually transmitted | Correct | 228 (91.57) | 98 (86.73) | 106 (84.80) | 34 (91.89) | 0.186 |
| Incorrect | 21 (8.43) | 15 (13.27) | 19 (15.20) | 3 (8.11) | ||
| Genital warts are caused by HPV | Correct | 220 (88.35) | 92 (81.42) | 102 (81.60) | 34 (91.89) | 0.116 |
| Incorrect | 29 (11.65) | 21 (18.58) | 23 (18.40) | 3 (8.11) | ||
| HPV can cause cervical cancer | Correct | 238 (95.58) | 106 (93.81) | 120 (96.00) | 35 (94.59) | 0.857 |
| Incorrect | 11 (4.42) | 7 (6.19) | 5 (4.00) | 2 (5.41) | ||
| Men cannot get HPV * | Correct | 209 (83.94) | 86 (76.11) | 104 (83.20) | 29 (78.38) | 0.301 |
| Incorrect | 40 (16.06) | 27 (23.89) | 21 (16.80) | 8 (21.62) | ||
| Individuals can be infected by HPV for years without knowing | Correct | 233 (93.57) | 97 (85.84) | 113 (90.40) | 30 (81.08) | 0.027 |
| Incorrect | 16 (6.43) | 16 (14.16) | 12 (9.60) | 7 (18.92) | ||
| HPV can be cured by antibiotics * | Correct | 207 (83.13) | 83 (73.45) | 102 (81.60) | 26 (70.27) | 0.076 |
| Incorrect | 42 (16.87) | 30 (26.55) | 23 (18.40) | 11 (29.73) | ||
| Are you aware of the availability of HPV vaccines? | Yes | 154 (61.85) | 41 (36.28) | 49 (39.20) | 11 (29.73) | <0.001 |
| No | 95 (38.15) | 72 (63.72) | 76 (60.80) | 26 (70.27) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sallam, M.; Al-Mahzoum, K.; Eid, H.; Assaf, A.M.; Abdaljaleel, M.; Al-Abbadi, M.; Mahafzah, A. Attitude towards HPV Vaccination and the Intention to Get Vaccinated among Female University Students in Health Schools in Jordan. Vaccines 2021, 9, 1432. https://doi.org/10.3390/vaccines9121432
Sallam M, Al-Mahzoum K, Eid H, Assaf AM, Abdaljaleel M, Al-Abbadi M, Mahafzah A. Attitude towards HPV Vaccination and the Intention to Get Vaccinated among Female University Students in Health Schools in Jordan. Vaccines. 2021; 9(12):1432. https://doi.org/10.3390/vaccines9121432
Chicago/Turabian StyleSallam, Malik, Kholoud Al-Mahzoum, Huda Eid, Areej M. Assaf, Maram Abdaljaleel, Mousa Al-Abbadi, and Azmi Mahafzah. 2021. "Attitude towards HPV Vaccination and the Intention to Get Vaccinated among Female University Students in Health Schools in Jordan" Vaccines 9, no. 12: 1432. https://doi.org/10.3390/vaccines9121432








