Hesitancy of Arab Healthcare Workers towards COVID-19 Vaccination: A Large-Scale Multinational Study
Abstract
:1. Introduction
2. Methods
3. Results
3.1. Demographics
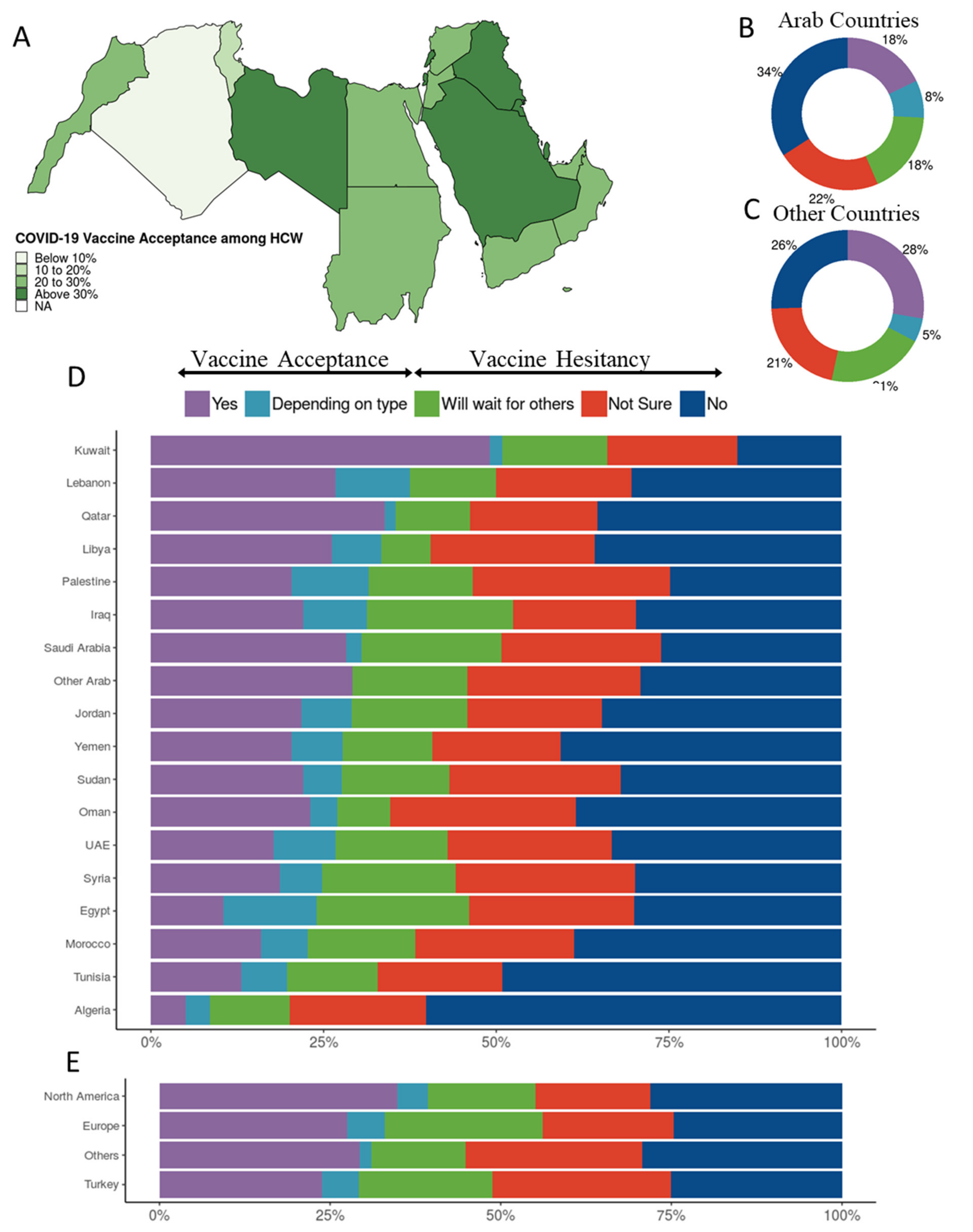
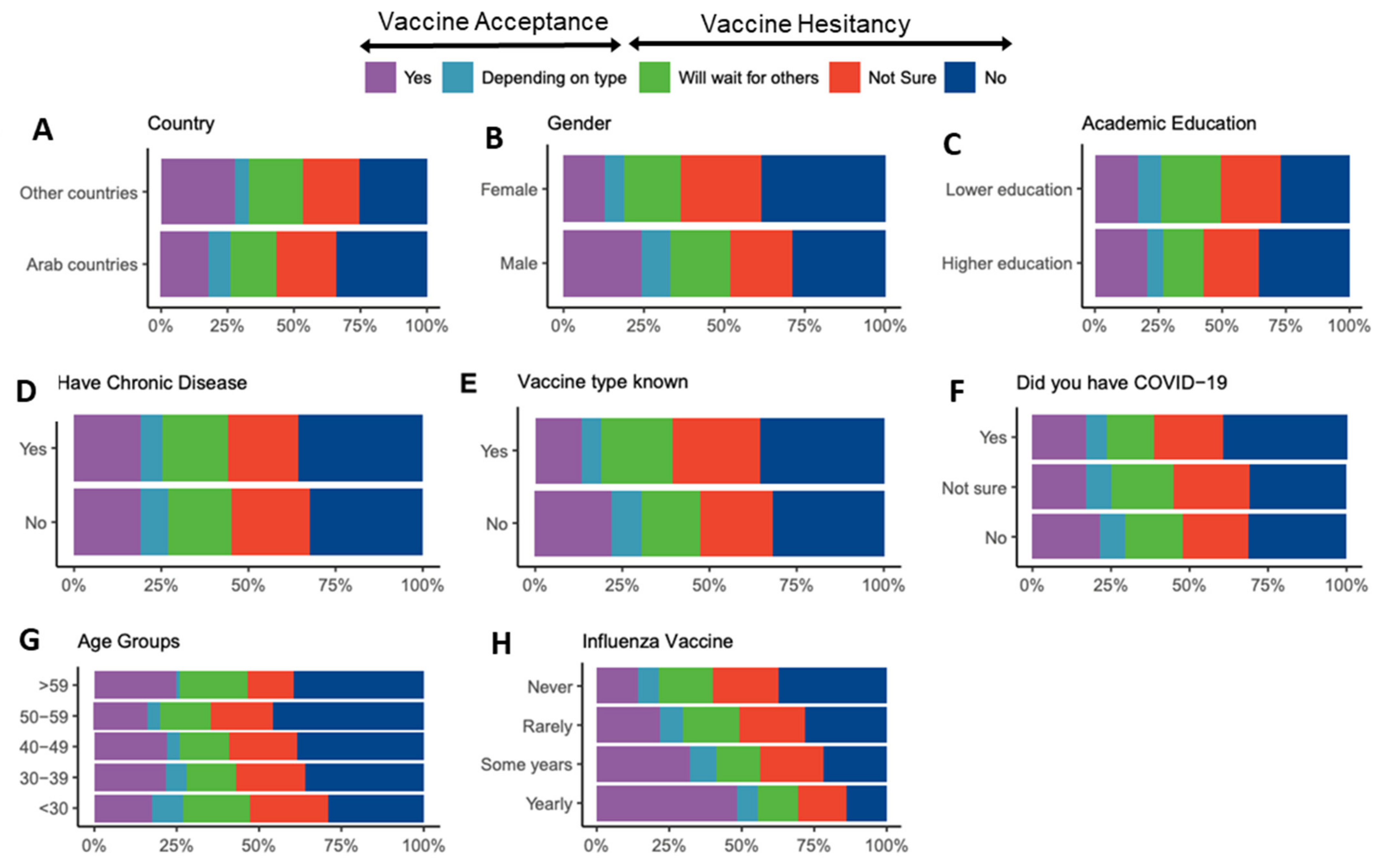
3.2. COVID-19 Vaccination Acceptance and Related Factors
3.3. Barriers to Acceptance
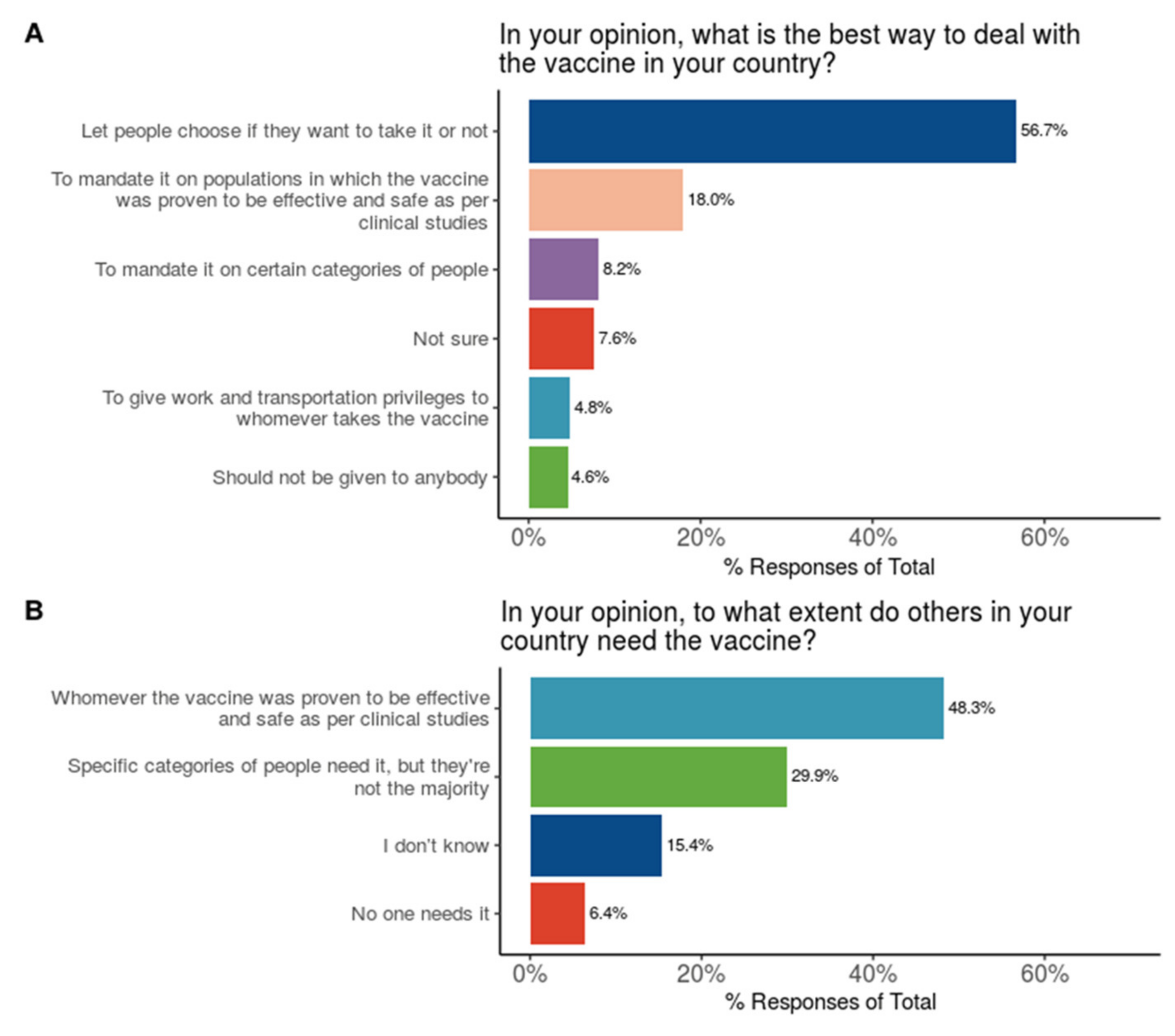
3.4. Stances of HCWs on Vaccination Policies and Need
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Shekhar, R.; Sheikh, A.; Upadhyay, S.; Singh, M.; Kottewar, S.; Mir, H.; Barrett, E.; Pal, S. COVID-19 Vaccine Acceptance among Health Care Workers in the United States. Vaccines 2021, 9, 119. [Google Scholar] [CrossRef] [PubMed]
- Gadoth, A.; Halbrook, M.; Martin-Blais, R.; Gray, A.; Tobin, N.H.; Ferbas, K.G.; Aldrovandi, G.M.; Rimoin, A.W. Cross-sectional Assessment of COVID-19 Vaccine Acceptance among Health Care Workers in Los Angeles. Ann. Intern. Med. 2021, 20–7580. [Google Scholar]
- Qattan, A.M.N.; Alshareef, N.; Alsharqi, O.; Al Rahahleh, N.; Chirwa, G.C.; Al-Hanawi, M.K. Acceptability of a COVID-19 Vaccine among Healthcare Workers in the Kingdom of Saudi Arabia. Front. Med. 2021, 8, 644300. [Google Scholar] [CrossRef]
- Mohamed-Hussein, A.A.; Makhlouf, H.; Abd El Aal, H.; Kholief, K.; Saad, M.M.; Abdellal, D.A. A national survey of potential acceptance of COVID-19 vaccines in healthcare workers in Egypt. medRxiv 2021, arXiv:10.1101/2021.01.11.21249324. [Google Scholar]
- Harapan, H.; Wagner, A.L.; Yufika, A.; Winardi, W.; Anwar, S.; Gan, A.K.; Setiawan, A.M.; Rajamoorthy, Y.; Sofyan, H.; Mudatsir, M. Acceptance of a COVID-19 Vaccine in Southeast Asia: A Cross-Sectional Study in Indonesia. Front. Public Health 2020, 8, 381. [Google Scholar] [CrossRef] [PubMed]
- Detoc, M.; Bruel, S.; Frappe, P.; Tardy, B.; Botelho-Nevers, E.; Gagneux-Brunon, A. Intention to participate in a COVID-19 vaccine clinical trial and to get vaccinated against COVID-19 in France during the pandemic. Vaccine 2020, 38, 7002–7006. [Google Scholar] [CrossRef] [PubMed]
- Kabamba Nzaji, M.; Kabamba Ngombe, L.; Ngoie Mwamba, G.; Banza Ndala, D.B.; Mbidi Miema, J.; Lungoyo, C.L.; Mwimba, B.L.; Bene, A.C.M.; Musenga, E.M. Acceptability of Vaccination Against COVID-19 among Healthcare Workers in the Democratic Republic of the Congo. Pragmatic Obs. Res. 2020, 11, 103–109. [Google Scholar] [CrossRef] [PubMed]
- Gagneux-Brunon, A.; Detoc, M.; Bruel, S.; Tardy, B.; Rozaire, O.; Frappe, P.; Botelho-Nevers, E. Intention to get vaccinations against COVID-19 in French healthcare workers during the first pandemic wave: A cross-sectional survey. J. Hosp. Infect. 2021, 108, 168–173. [Google Scholar] [CrossRef] [PubMed]
- Ledda, C.; Costantino, C.; Cuccia, M.; Maltezou, H.C.; Rapisarda, V. Attitudes of Healthcare Personnel towards Vaccinations before and during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health. 2021, 18, 2703. [Google Scholar] [CrossRef] [PubMed]
- Chew, N.W.; Cheong, C.; Kong, G.; Phua, K.; Ngiam, J.N.; Tan, B.Y.; Wang, B.; Hao, F.; Tan, W.; Han, X.; et al. An Asia-Pacific study on healthcare worker’s perception and willingness to receive COVID-19 vaccination. Int. J. Infect. Dis. 2021, 26, 1201. [Google Scholar]
- Yurttas, B.; Poyraz, B.C.; Sut, N.; Ozdede, A.; Oztas, M.; Uğurlu, S.; Tabak, F.; Hamuryudan, V.; Seyahi, E. Willingness to get the COVID-19 vaccine among patients with rheumatic diseases, healthcare workers and general population in Turkey: A web-based survey. Rheumatol. Int. 2021, 29, 1–10. [Google Scholar]
- Raftopoulos, V.; Iordanou, S.; Katsapi, A.; Dedoukou, X.; Maltezou, H.C. A comparative online survey on the intention to get COVID-19 vaccine between Greek and Cypriot healthcare personnel: Is the country a predictor? Hum. Vaccines Immunother. 2021, 23, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Papagiannis, D.; Rachiotis, G.; Malli, F.; Papathanasiou, I.V.; Kotsiou, O.; Fradelos, E.C.; Giannakopoulos, K.; Gourgoulianis, K.I. Acceptability of COVID-19 Vaccination among Greek Health Professionals. Vaccines (Basel) 2021, 9, 200. [Google Scholar] [CrossRef] [PubMed]
- Qunaibi, E.A.; Helmy, M.; Basheti, I.; Sultan, I. A High Rate of COVID-19 Vaccine Hesitancy among Arabs: Results of a Large-scale Survey. medRxiv 2021, arXiv:10.1101/2021.03.09.21252764. [Google Scholar]
- Eysenbach, G. Improving the quality of Web surveys: The Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J. Med. Internet. Res. 2004, 6, e34. [Google Scholar] [CrossRef] [PubMed]
- Guidotti, E.; Ardia, D. COVID-19 Data Hub. J. Open Source Softw. 2020, 5, 2376. [Google Scholar] [CrossRef]
- Cyranoski, D. Arab nations first to approve Chinese COVID vaccine—despite lack of public data. Nature 2020, 588, 548. [Google Scholar] [CrossRef] [PubMed]



| Country | No | Not Sure | Will Wait for Others | Depending on Type | Yes | Total | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | ||
| Algeria | 287 | (60.2%) | 94 | (19.7%) | 55 | (11.5%) | 17 | (3.6%) | 24 | (5.0%) | 477 |
| Egypt | 376 | (30.1%) | 298 | (23.8%) | 276 | (22.1%) | 169 | (13.5%) | 131 | (10.5%) | 1250 |
| Europe | 98 | (24.7%) | 76 | (19.1%) | 92 | (23.2%) | 22 | (5.5%) | 109 | (27.5%) | 397 |
| Iraq | 42 | (29.8%) | 25 | (17.7%) | 30 | (21.3%) | 13 | (9.2%) | 31 | (22.0%) | 141 |
| Jordan | 379 | (34.7%) | 212 | (19.4%) | 184 | (16.8%) | 79 | (7.2%) | 238 | (21.8%) | 1092 |
| Kuwait | 8 | (15.1%) | 10 | (18.9%) | 8 | (15.1%) | 1 | (1.9%) | 26 | (49.1%) | 53 |
| Lebanon | 17 | (30.4%) | 11 | (19.6%) | 7 | (12.5%) | 6 | (10.7%) | 15 | (26.8%) | 56 |
| Libya | 15 | (35.7%) | 10 | (23.8%) | 3 | (7.1%) | 3 | (7.1%) | 11 | (26.2%) | 42 |
| Morocco | 87 | (38.7%) | 52 | (23.1%) | 35 | (15.6%) | 15 | (6.7%) | 36 | (16.0%) | 225 |
| North America | 25 | (28.1%) | 15 | (16.9%) | 14 | (15.7%) | 4 | (4.5%) | 31 | (34.8%) | 89 |
| Oman | 10 | (38.5%) | 7 | (26.9%) | 2 | (7.7%) | 1 | (3.8%) | 6 | (23.1%) | 26 |
| Other Arab | 7 | (29.2%) | 6 | (25.0%) | 4 | (16.7%) | 0 | (0.0%) | 7 | (29.2%) | 24 |
| Others | 17 | (29.3%) | 15 | (25.9%) | 8 | (13.8%) | 1 | (1.7%) | 17 | (29.3%) | 58 |
| Palestine | 66 | (24.8%) | 76 | (28.6%) | 40 | (15.0%) | 30 | (11.3%) | 54 | (20.3%) | 266 |
| Qatar | 23 | (35.4%) | 12 | (18.5%) | 7 | (10.8%) | 1 | (1.5%) | 22 | (33.8%) | 65 |
| Saudi Arabia | 142 | (26.1%) | 126 | (23.2%) | 110 | (20.2%) | 12 | (2.2%) | 154 | (28.3%) | 544 |
| Sudan | 45 | (31.9%) | 35 | (24.8%) | 22 | (15.6%) | 8 | (5.7%) | 31 | (22.0%) | 141 |
| Syria | 103 | (29.9%) | 89 | (25.9%) | 67 | (19.5%) | 21 | (6.1%) | 64 | (18.6%) | 344 |
| Tunisia | 30 | (49.2%) | 11 | (18.0%) | 8 | (13.1%) | 4 | (6.6%) | 8 | (13.1%) | 61 |
| Turkey | 42 | (25.0%) | 44 | (26.2%) | 33 | (19.6%) | 9 | (5.4%) | 40 | (23.8%) | 168 |
| UAE | 45 | (33.3%) | 32 | (23.7%) | 22 | (16.3%) | 12 | (8.9%) | 24 | (17.8%) | 135 |
| Yemen | 22 | (40.7%) | 10 | (18.5%) | 7 | (13.0%) | 4 | (7.4%) | 11 | (20.4%) | 54 |
| Label | Levels | No | Not Sure | Will Wait for Others | Depending on Type | Yes | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | ||
| Age | <30 | 876 | (28.9%) | 720 | (23.7%) | 624 | (20.6%) | 290 | (9.6%) | 523 | (17.2%) |
| 30–39 | 595 | (36.1%) | 345 | (20.9%) | 249 | (15.1%) | 105 | (6.4%) | 355 | (21.5%) | |
| 40–49 | 266 | (38.4%) | 142 | (20.5%) | 106 | (15.3%) | 26 | (3.8%) | 152 | (22.0%) | |
| 50–59 | 120 | (46.0%) | 49 | (18.8%) | 40 | (15.3%) | 10 | (3.8%) | 42 | (16.1%) | |
| >59 | 29 | (39.7%) | 10 | (13.7%) | 15 | (20.5%) | 1 | (1.4%) | 18 | (24.7%) | |
| Chronic Diseases | No | 1600 | (32.6%) | 1104 | (22.5%) | 883 | (18.0%) | 384 | (7.8%) | 937 | (19.1%) |
| Yes | 286 | (35.8%) | 162 | (20.3%) | 151 | (18.9%) | 48 | (6.0%) | 153 | (19.1%) | |
| Country | Arab countries | 1704 | (34.1%) | 1116 | (22.3%) | 887 | (17.8%) | 396 | (7.9%) | 893 | (17.9%) |
| Other countries | 182 | (25.6%) | 150 | (21.1%) | 147 | (20.6%) | 36 | (5.1%) | 197 | (27.7%) | |
| Academic Education | Higher education | 1388 | (35.8%) | 835 | (21.5%) | 607 | (15.7%) | 260 | (6.7%) | 785 | (20.3%) |
| Lower education | 498 | (27.2%) | 431 | (23.5%) | 427 | (23.3%) | 172 | (9.4%) | 305 | (16.6%) | |
| Had Covid | No | 809 | (31.4%) | 535 | (20.7%) | 481 | (18.7%) | 202 | (7.8%) | 552 | (21.4%) |
| Not sure | 578 | (31.1%) | 451 | (24.3%) | 362 | (19.5%) | 148 | (8.0%) | 320 | (17.2%) | |
| Yes | 499 | (39.3%) | 280 | (22.0%) | 191 | (15.0%) | 82 | (6.5%) | 218 | (17.2%) | |
| Job | HCW | 1886 | (33.0%) | 1266 | (22.2%) | 1034 | (18.1%) | 432 | (7.6%) | 1090 | (19.1%) |
| Gender | Male | 911 | (28.7%) | 623 | (19.6%) | 588 | (18.5%) | 285 | (9.0%) | 764 | (24.1%) |
| Female | 975 | (38.4%) | 643 | (25.3%) | 446 | (17.6%) | 147 | (5.8%) | 326 | (12.8%) | |
| Influenza Vaccine | Yearly | 45 | (14.0%) | 53 | (16.5%) | 45 | (14.0%) | 23 | (7.2%) | 155 | (48.3%) |
| Some years | 149 | (21.9%) | 148 | (21.7%) | 105 | (15.4%) | 61 | (9.0%) | 218 | (32.0%) | |
| Rarely | 201 | (28.2%) | 160 | (22.5%) | 141 | (19.8%) | 57 | (8.0%) | 153 | (21.5%) | |
| Never | 1491 | (37.3%) | 905 | (22.7%) | 743 | (18.6%) | 291 | (7.3%) | 564 | (14.1%) | |
| Vaccine type unknown | No | 1228 | (31.8%) | 800 | (20.7%) | 656 | (17.0%) | 326 | (8.5%) | 847 | (22.0%) |
| Yes | 658 | (35.5%) | 466 | (25.2%) | 378 | (20.4%) | 106 | (5.7%) | 243 | (13.1%) | |
| Variable | Levels | Acceptance (%) | Hesitancy (%) | Univariable OR (CI) | Multivariable OR (CI) |
|---|---|---|---|---|---|
| Age | <30 | 813 (26.8) | 2220 (73.2) | − | − |
| 30–39 | 460 (27.9) | 1189 (72.1) | 0.95 (0.83–1.08) | 1.21 (1.03–1.42) | |
| 40–49 | 178 (25.7) | 514 (74.3) | 1.06 (0.88–1.28) | 1.41 (1.14–1.75) | |
| 50–59 | 52 (19.9) | 209 (80.1) | 1.47 (1.08–2.03) | 1.92 (1.37–2.73) | |
| >59 | 19 (26.0) | 54 (74.0) | 1.04 (0.62–1.81) | 1.62 (0.93–2.94) | |
| Chronic Diseases | No | 1321 (26.9) | 3587 (73.1) | − | − |
| Yes | 201 (25.1) | 599 (74.9) | 1.10 (0.93-1.31) | 1.01 (0.84–1.22) | |
| Country | Arab countries | 1289 (25.8) | 3707 (74.2) | − | − |
| Other countries | 233 (32.7) | 479 (67.3) | 0.71 (0.60–0.85) | 0.87 (0.73-1.05) | |
| Academic Education | Higher education | 1045 (27.0) | 2830 (73.0) | − | − |
| Lower education | 477 (26.0) | 1356 (74.0) | 1.05 (0.93–1.19) | 0.97 (0.84–1.14) | |
| Had Covid | No | 754 (29.2) | 1825 (70.8) | − | − |
| Not sure | 468 (25.2) | 1391 (74.8) | 1.23 (1.07-1.41) | 1.25 (1.08–1.44) | |
| Yes | 300 (23.6) | 970 (76.4) | 1.34 (1.15–1.56) | 1.34 (1.14-1.58) | |
| Gender | Male | 1049 (33.1) | 2122 (66.9) | − | − |
| Female | 473 (18.6) | 2064 (81.4) | 2.16 (1.91–2.44) | 2.04 (1.79–2.32) | |
| Vaccine Type Unknown | No | 1173 (30.4) | 2684 (69.6) | − | − |
| Yes | 349 (18.9) | 1502 (81.1) | 1.88 (1.64–2.16) | 1.69 (1.47–1.96) | |
| Influenza Vaccine | Yearly | 178 (55.5) | 143 (44.5) | − | − |
| Some years | 279 (41.0) | 402 (59.0) | 1.79 (1.37–2.35) | 1.70 (1.29–2.24) | |
| Rarely | 210 (29.5) | 502 (70.5) | 2.98 (2.27–3.91) | 2.87 (2.17–3.81) | |
| Never | 855 (21.4) | 3139 (78.6) | 4.57 (3.62–5.77) | 4.30 (3.37–5.49) |
| Barriers | HCW | Not HCW | X2 Statistic | p-Value | ||
| n | (%) | n | (%) | |||
| Afraid of unknown side effects | 3313 | (58.0%) | 18,922 | (62.0%) | 20.31 | <0.0001 |
| Not enough time to test vaccine safety | 3252 | (57.0%) | 16,920 | (55.5%) | 9.74 | 0.0018 |
| Vaccine production was rushed | 2505 | (43.9%) | 14,193 | (46.5%) | 7.99 | 0.0047 |
| Do not trust the healthcare policies | 2133 | (37.4%) | 12,018 | (39.4%) | 4.63 | 0.031 |
| Insufficient numbers of studies | 1693 | (29.7%) | 8208 | (26.9%) | 23.58 | <0.0001 |
| No value for new strains | 1569 | (27.5%) | 6475 | (21.2%) | 120.27 | <0.0001 |
| Do not trust company/studies | 1541 | (27.0%) | 10,427 | (34.2%) | 99.31 | <0.0001 |
| No published studies on vaccine | 1175 | (20.6%) | 5911 | (19.4%) | 6.61 | 0.010 |
| Pandemic is exaggerated to benefit pharma | 1119 | (19.6%) | 7868 | (25.8%) | 89.01 | <0.0001 |
| Most infected people recover | 979 | (17.2%) | 7036 | (23.1%) | 88.7 | <0.0001 |
| Vaccine immunity is short | 976 | (17.1%) | 3637 | (11.9%) | 124.47 | <0.0001 |
| Vaccines irreversibly alter DNA | 928 | (16.3%) | 6985 | (22.9%) | 114.28 | <0.0001 |
| Afraid of SE mentioned in studies | 847 | (14.8%) | 5695 | (18.7%) | 42.19 | <0.0001 |
| Coronavirus/vaccine are a conspiracy | 700 | (12.3%) | 5972 | (19.6%) | 160.99 | <0.0001 |
| Vaccine can cause COVID19 | 695 | (12.2%) | 5939 | (19.5%) | 160.83 | <0.0001 |
| I had/have COVID | 681 | (11.9%) | 2875 | (9.4%) | 38.01 | <0.0001 |
| Vaccine may cause death | 630 | (11.0%) | 4257 | (14.0%) | 31.15 | <0.0001 |
| Vaccines were not tested in Arabs | 543 | (9.5%) | 2209 | (7.2%) | 38.84 | <0.0001 |
| Infection rate decreasing | 426 | (7.5%) | 3056 | (10.0%) | 32.87 | <0.0001 |
| Do not believe in vaccines in general | 419 | (7.3%) | 4186 | (13.7%) | 168.53 | <0.0001 |
| Most vaccinated people had SE | 416 | (7.3%) | 2608 | (8.5%) | 8.39 | 0.0038 |
| Most people already had COVID | 373 | (6.5%) | 1898 | (6.2%) | 1.29 | 0.26 |
| Vaccines contain aluminum | 326 | (5.7%) | 2896 | (9.5%) | 80.31 | <0.0001 |
| May get COVID19 after vaccine | 267 | (4.7%) | 1370 | (4.5%) | 0.68 | 0.41 |
| I do not like needles | 220 | (3.9%) | 1750 | (5.7%) | 30.91 | <0.0001 |
| I am not eligible (pregnant or <16 old) | 147 | (2.6%) | 965 | (3.2%) | 4.89 | 0.027 |
| I have a chronic disease | 136 | (2.4%) | 1266 | (4.1%) | 38.39 | 0 |
| I have allergies to foods/drugs | 132 | (2.3%) | 716 | (2.3%) | 0 | 0.99 |
| I do not think I will get COVID19 | 86 | (1.5%) | 674 | (2.2%) | 10.76 | 0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Qunaibi, E.; Basheti, I.; Soudy, M.; Sultan, I. Hesitancy of Arab Healthcare Workers towards COVID-19 Vaccination: A Large-Scale Multinational Study. Vaccines 2021, 9, 446. https://doi.org/10.3390/vaccines9050446
Qunaibi E, Basheti I, Soudy M, Sultan I. Hesitancy of Arab Healthcare Workers towards COVID-19 Vaccination: A Large-Scale Multinational Study. Vaccines. 2021; 9(5):446. https://doi.org/10.3390/vaccines9050446
Chicago/Turabian StyleQunaibi, Eyad, Iman Basheti, Mohamed Soudy, and Iyad Sultan. 2021. "Hesitancy of Arab Healthcare Workers towards COVID-19 Vaccination: A Large-Scale Multinational Study" Vaccines 9, no. 5: 446. https://doi.org/10.3390/vaccines9050446
APA StyleQunaibi, E., Basheti, I., Soudy, M., & Sultan, I. (2021). Hesitancy of Arab Healthcare Workers towards COVID-19 Vaccination: A Large-Scale Multinational Study. Vaccines, 9(5), 446. https://doi.org/10.3390/vaccines9050446






