Rotavirus as an Expression Platform of Domains of the SARS-CoV-2 Spike Protein
Abstract
:1. Introduction
2. Materials and Methods
2.1. Cell Culture
2.2. Plasmid Construction
2.3. Recombinant Viruses
2.4. Immunoblot Analysis
2.5. Immunoprecipitation Assay
2.6. CsCl Gradient Centrifugation
2.7. Genetic Stability of rSA11 Viruses
2.8. GenBank Accession Numbers
3. Results and Discussion
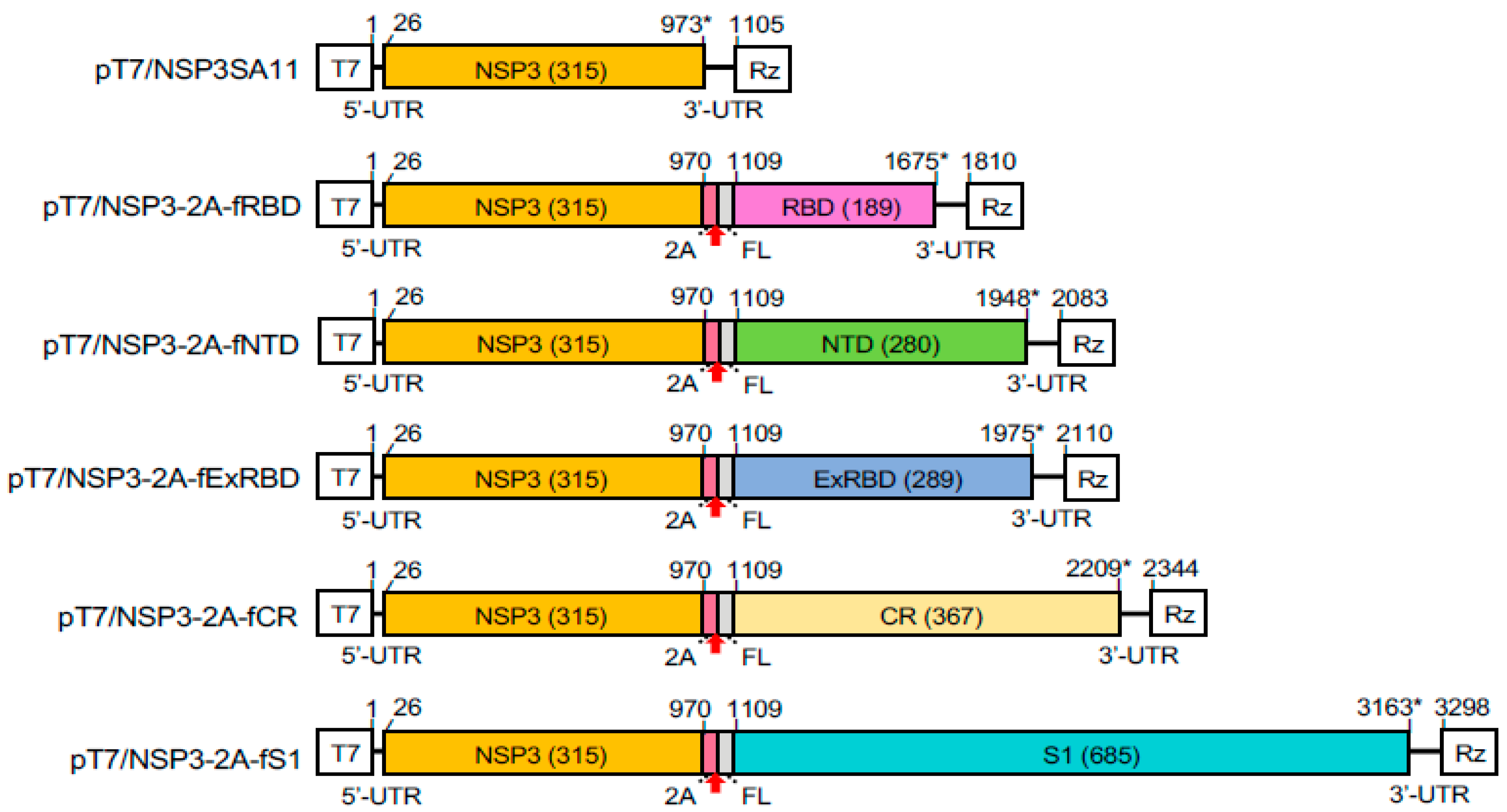
3.1. Modified Segment 7 (NSP3) Expression Vectors Containing SARS-CoV-2 S Sequences
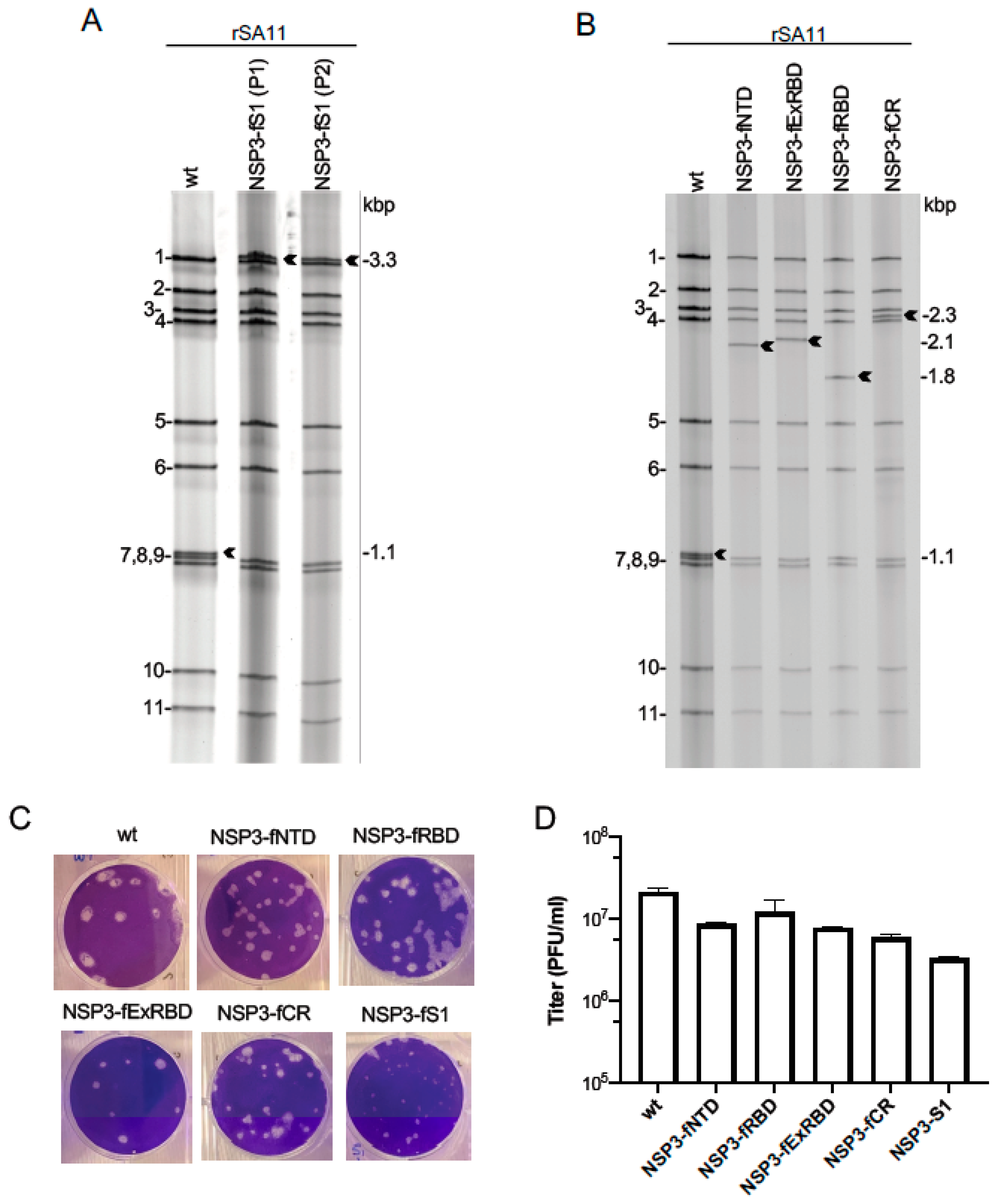
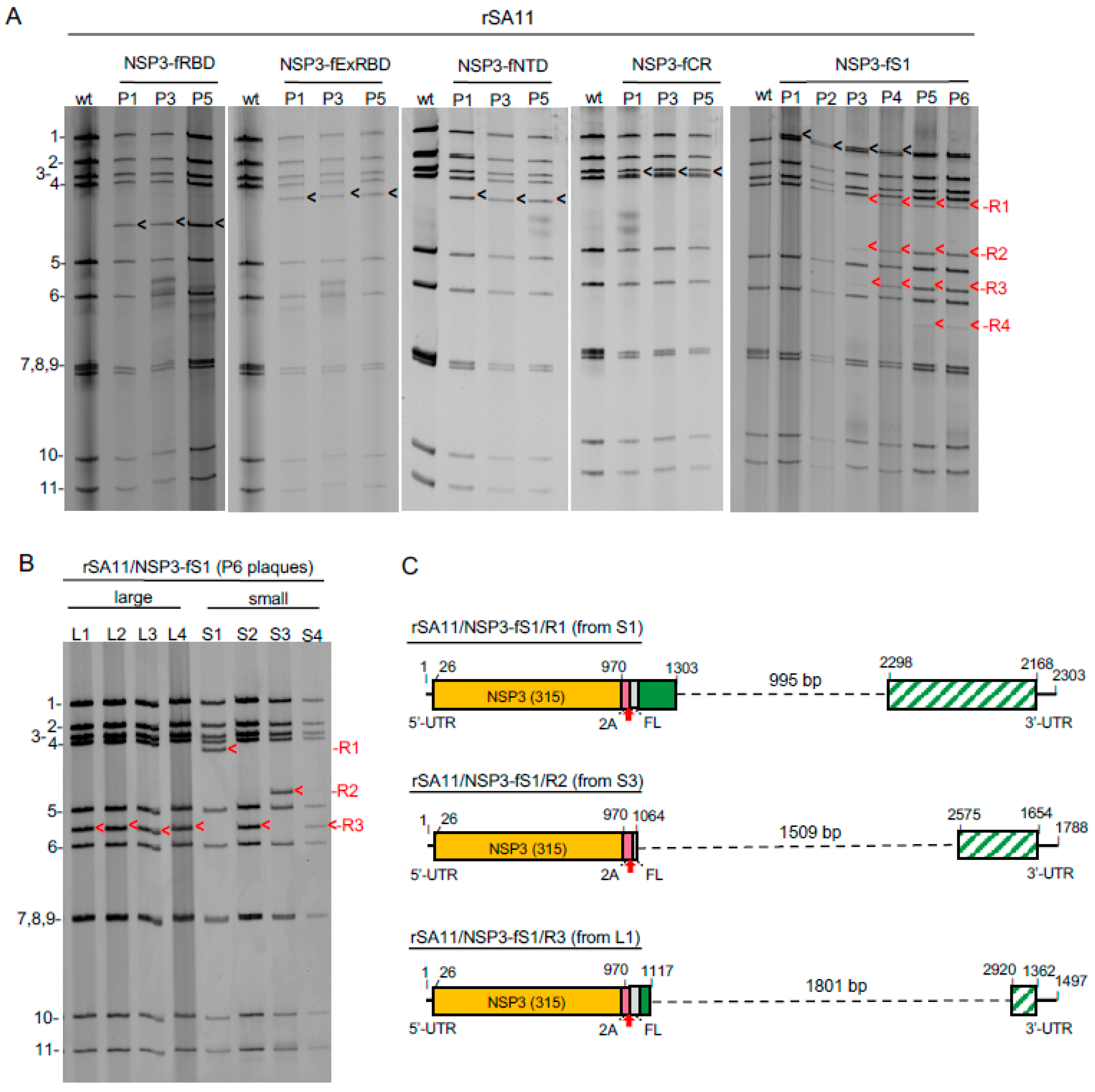
3.2. Recovery of rSA11 Rotaviruses with Segment 7 dsRNA Containing S Sequences
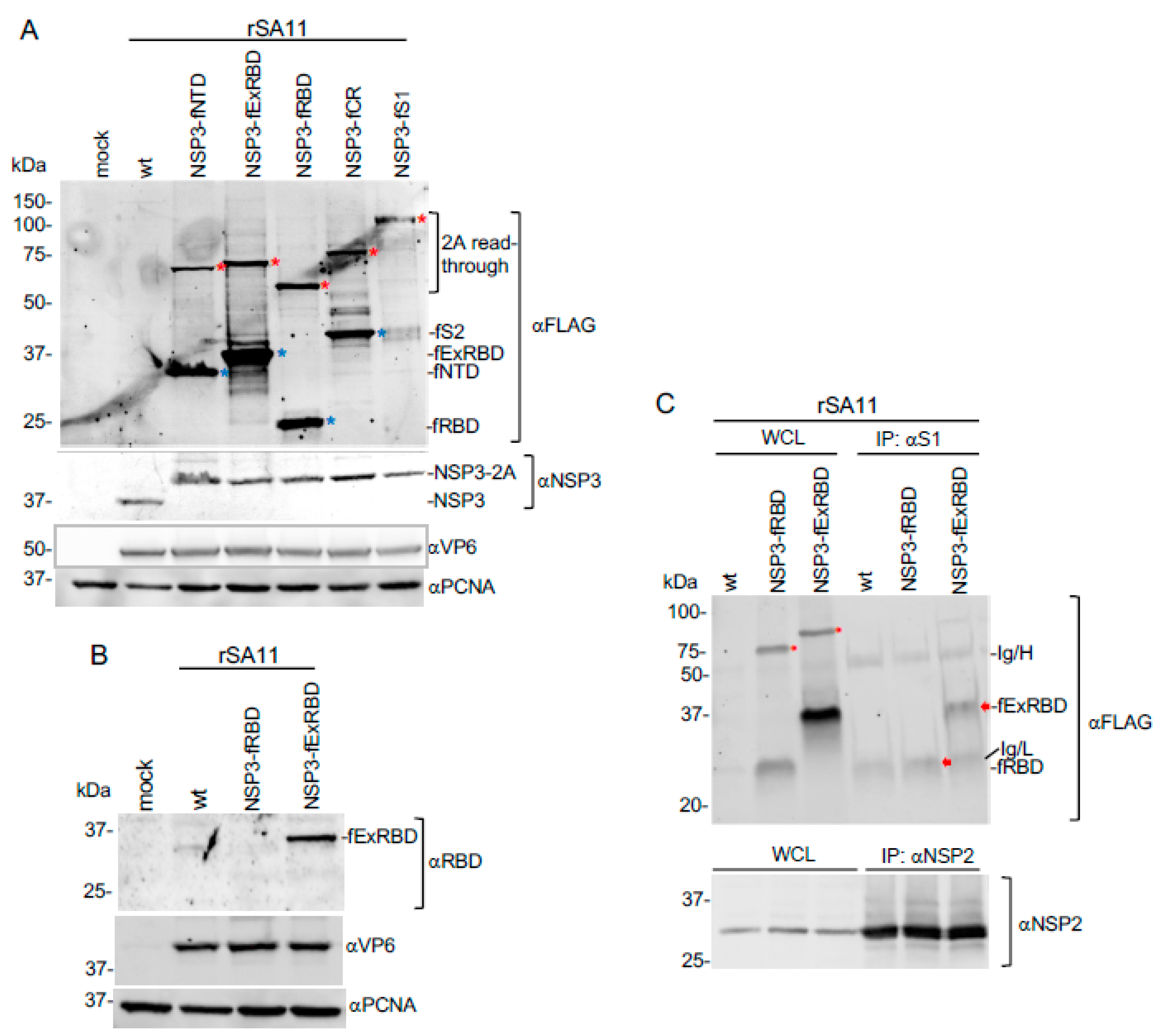
3.3. Expression of S Coding Sequences by rSA11 Rotaviruses
3.4. Expression of the ExRBD and RBD Products by rSA11s during Rotavirus Infection
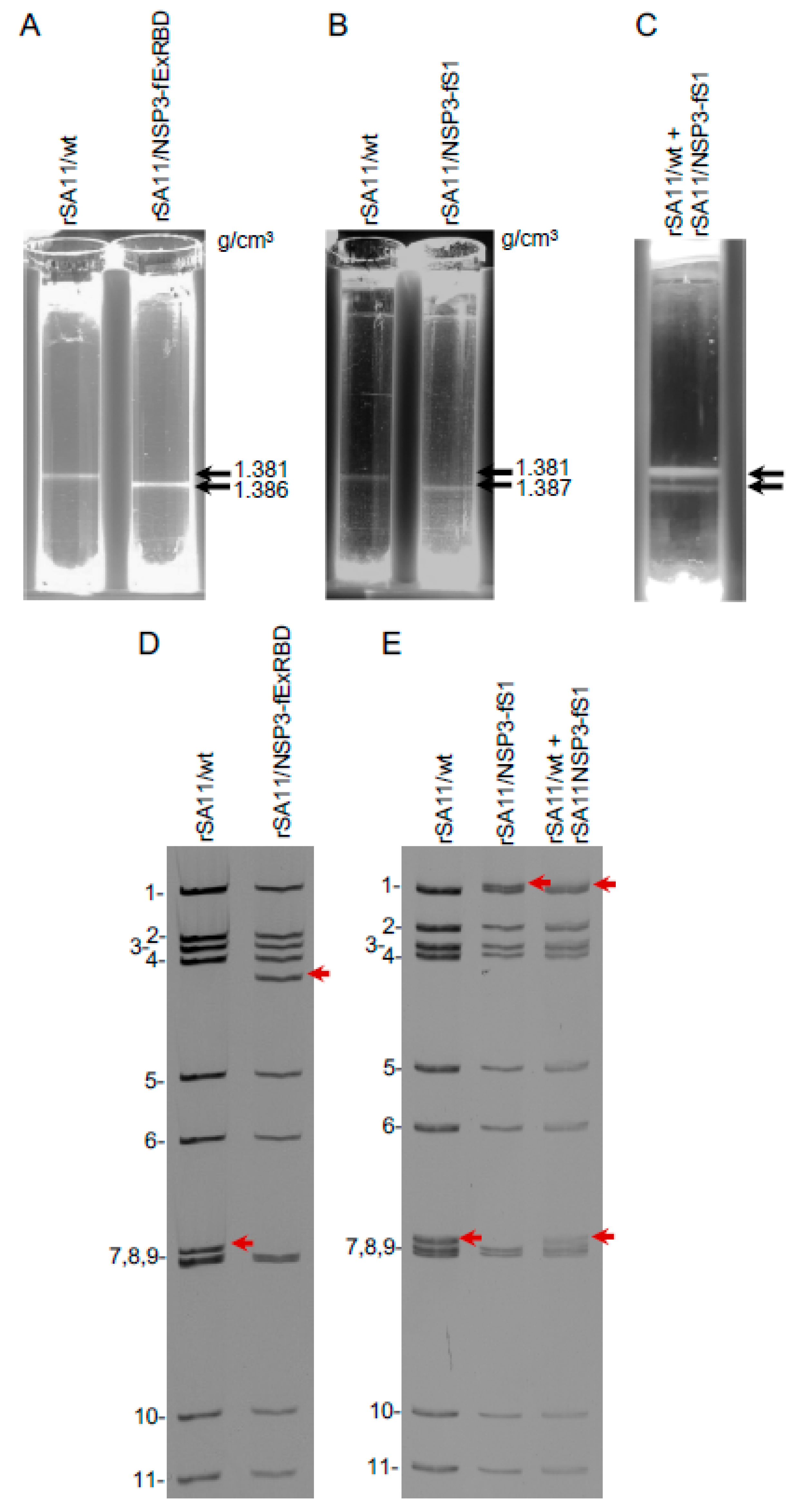
3.5. Density of rSA11 Virus Particles Containing S Sequences
3.6. Genetic Stability of rSA11 Rotaviruses Containing S Sequences
4. Summary
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dai, L.; Gao, G.F. Viral targets for vaccines against COVID-19. Nat. Rev. Immunol. 2021, 21, 73–82. [Google Scholar] [CrossRef]
- Kaur, S.P.; Gupta, V. COVID-19 Vaccine: A comprehensive status report. Virus Res. 2020, 288, 198114. [Google Scholar] [CrossRef]
- Ludvigsson, J.F. Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatr. 2020, 109, 1088–1095. [Google Scholar] [CrossRef]
- Pollán, M.; Pérez-Gómez, B.; Pastor-Barriuso, R.; Oteo, J.; Hernán, M.A.; Pérez-Olmeda, M.; Sanmartín, J.L.; Fernández-García, A.; Cruz, I.; Fernández de Larrea, N.; et al. Prevalence of SARS-CoV-2 in Spain (ENE-COVID): A nationwide, population-based seroepidemiological study. Lancet 2020, 396, 535–544. [Google Scholar] [CrossRef]
- Burke, R.M.; Tate, J.E.; Kirkwood, C.D.; Steele, A.D.; Parashar, U.D. Current and new rotavirus vaccines. Curr. Opin. Infect. Dis. 2019, 32, 435–444. [Google Scholar] [CrossRef] [PubMed]
- Burnett, E.; Parashar, U.D.; Tate, J.E. Real-world effectiveness of rotavirus vaccines, 2006–2019: A literature review and meta-analysis. Lancet Glob. Health 2020, 8, e1195–e1202. [Google Scholar] [CrossRef]
- Soares-Weiser, K.; Bergman, H.; Henschke, N.; Pitan, F.; Cunliffe, N. Vaccines for preventing rotavirus diarrhoea: Vaccines in use. Cochrane Database Syst. Rev. 2019, 3, CD008521. [Google Scholar] [PubMed]
- Folorunso, O.S.; Sebolai, O.M. Overview of the development, impacts, and challenges of live-attenuated oral rotavirus vaccines. Vaccines 2020, 8, 341. [Google Scholar] [CrossRef] [PubMed]
- Ali, A.; Kazi, A.M.; Cortese, M.M.; Fleming, J.A.; Moon, S.; Parashar, U.D.; Jiang, B.; McNeal, M.M.; Steele, D.; Bhutta, Z.; et al. Impact of withholding breastfeeding at the time of vaccination on the immunogenicity of oral rotavirus vaccine—A randomized trial. PLoS ONE 2015, 10, e0127622, Erratum in 2015, 10, e0145568. [Google Scholar]
- Liu, G.F.; Hille, D.; Kaplan, S.S.; Goveia, M.G. Postdose 3 G1 serum neutralizing antibody as correlate of protection for pentavalent rotavirus vaccine. Hum. Vaccines Immunother. 2017, 13, 2357–2363. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Angel, J.; Steele, A.D.; Franco, M.A. Correlates of protection for rotavirus vaccines: Possible alternative trial endpoints, opportunities, and challenges. Hum. Vaccines Immunother. 2014, 10, 3659–3671. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leshem, E.; Tate, J.E.; Steiner, C.A.; Curns, A.T.; Lopman, B.A.; Parashar, U.D. Acute gastroenteritis hospitalizations among US children following implementation of the rotavirus vaccine. JAMA 2015, 313, 2282–2284, Erratum in 2015, 314, 188. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clark, A.; Black, R.; Tate, J.; Roose, A.; Kotloff, K.; Lam, D.; Blackwelder, W.; Parashar, U.; Lanata, C.; Kang, G.; et al. Estimating global, regional and national rotavirus deaths in children aged < 5 years: Current approaches, new analyses and proposed improvements. PLoS ONE 2017, 12, e0183392. [Google Scholar]
- Kanai, Y.; Kawagishi, T.; Nouda, R.; Onishi, M.; Pannacha, P.; Nurdin, J.A.; Nomura, K.; Matsuura, Y.; Kobayashi, T. Development of stable rotavirus reporter expression systems. J. Virol. 2018, 93, e01774-18. [Google Scholar] [CrossRef] [Green Version]
- Kanai, Y.; Komoto, S.; Kawagishi, T.; Nouda, R.; Nagasawa, N.; Onishi, M.; Matsuura, Y.; Taniguchi, K.; Kobayashi, T. Entirely plasmid-based reverse genetics system for rotaviruses. Proc. Natl. Acad. Sci. USA 2017, 114, 2349–2354. [Google Scholar] [CrossRef] [Green Version]
- Kanai, Y.; Kobayashi, T. Rotavirus reverse genetics systems: Development and application. Virus Res. 2021, 10, 198296. [Google Scholar] [CrossRef] [PubMed]
- Komoto, S.; Fukuda, S.; Ide, T.; Ito, N.; Sugiyama, M.; Yoshikawa, T.; Murata, T.; Taniguchi, K. Generation of recombinant rotaviruses expressing fluorescent proteins by using an optimized reverse genetics system. J. Virol. 2018, 92, e00588-18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Komoto, S.; Fukuda, S.; Kugita, M.; Hatazawa, R.; Koyama, C.; Katayama, K.; Murata, T.; Taniguchi, K. Generation of infectious recombinant human rotaviruses from just 11 cloned cDNAs encoding the rotavirus genome. J. Virol. 2019, 93, e02207-18. [Google Scholar] [CrossRef] [Green Version]
- Philip, A.A.; Patton, J.T. Expression of separate heterologous proteins from the rotavirus NSP3 genome segment using a translational 2A stop-restart element. J. Virol 2020, 94, e00959-20. [Google Scholar] [CrossRef]
- Philip, A.A.; Herrin, B.E.; Garcia, M.L.; Abad, A.T.; Katen, S.P.; Patton, J.T. Collection of recombinant rotaviruses expressing fluorescent reporter proteins. Microbio. Resour. Announc. 2019, 8, e00523-19. [Google Scholar] [CrossRef] [Green Version]
- Philip, A.A.; Perry, J.L.; Eaton, H.E.; Shmulevitz, M.; Hyser, J.M.; Patton, J.T. Generation of recombinant rotavirus expressing NSP3-UnaG fusion protein by a simplified reverse genetics system. J. Virol. 2019, 93, e01616-19. [Google Scholar] [CrossRef]
- Sánchez-Tacuba, L.; Feng, N.; Meade, N.J.; Mellits, K.H.; Jaïs, P.H.; Yasukawa, L.L.; Resch, T.K.; Jiang, B.; López, S.; Ding, S.; et al. An optimized reverse genetics system suitable for efficient recovery of simian, human, and murine-like rotaviruses. J. Virol. 2020, 94, e01294-20. [Google Scholar] [CrossRef]
- Crawford, S.E.; Ramani, S.; Tate, J.E.; Parashar, U.D.; Svensson, L.; Hagbom, M.; Franco, M.A.; Greenberg, H.B.; O’Ryan, M.; Kang, G.; et al. Rotavirus infection. Nat. Rev. Dis. Primers 2017, 3, 17083. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Trask, S.D.; McDonald, S.M.; Patton, J.T. Structural insights into the coupling of virion assembly and rotavirus replication. Nat. Rev. Microbiol. 2012, 10, 165–177. [Google Scholar] [CrossRef] [Green Version]
- Eaton, H.E.; Kobayashi, T.; Dermody, T.S.; Johnston, R.N.; Jais, P.H.; Shmulevitz, M. African swine fever virus NP868R capping enzyme promotes reovirus rescue during reverse genetics by promoting reovirus protein expression, virion assembly, and RNA incorporation into infectious virions. J. Virol. 2017, 91, e02416-16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Criglar, J.M.; Crawford, S.E.; Zhao, B.; Smith, H.G.; Stossi, F.; Estes, M.K. A genetically engineered rotavirus NSP2 phosphorylation mutant impaired in viroplasm formation and replication shows an early interaction between vNSP2 and cellular lipid droplets. J. Virol. 2020, 94, e00972-20. [Google Scholar] [CrossRef]
- Navarro, A.; Trask, S.D.; Patton, J.T. Generation of genetically stable recombinant rotaviruses containing novel genome rearrangements and heterologous sequences by reverse genetics. J. Virol. 2013, 87, 6211–6220. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chang-Graham, A.L.; Perry, J.L.; Strtak, A.C.; Ramachandran, N.K.; Criglar, J.M.; Philip, A.A.; Patton, J.T.; Estes, M.K.; Hyser, J.M. Rotavirus calcium dysregulation manifests as dynamic calcium signaling in the cytoplasm and endoplasmic reticulum. Sci. Rep. 2019, 9, 10822. [Google Scholar] [CrossRef] [Green Version]
- Komoto, S.; Kanai, Y.; Fukuda, S.; Kugita, M.; Kawagishi, T.; Ito, N.; Sugiyama, M.; Matsuura, Y.; Kobayashi, T.; Taniguchi, K. Reverse genetics system demonstrates that rotavirus nonstructural protein NSP6 is not essential for viral replication in cell culture. J. Virol. 2017, 91, e00695-17. [Google Scholar] [CrossRef] [Green Version]
- Papa, G.; Venditti, L.; Arnoldi, F.; Schraner, E.M.; Potgieter, C.; Borodavka, A.; Eichwald, C.; Burrone, O.R. Recombinant rotaviruses rescued by reverse genetics reveal the role of NSP5 hyperphosphorylation in the assembly of viral factories. J. Virol. 2019, 94, e01110–e01119. [Google Scholar] [CrossRef] [Green Version]
- Gratia, M.; Sarot, E.; Vende, P.; Charpilienne, A.; Baron, C.H.; Duarte, M.; Pyronnet, S.; Poncet, D. Rotavirus NSP3 is a translational surrogate of the poly(A)-binding protein-poly(A) complex. J. Virol. 2015, 89, 8773–8782. [Google Scholar] [CrossRef] [Green Version]
- Piron, M.; Delaunay, T.; Grosclaude, J.; Poncet, D. Identification of the RNA-binding, dimerization, and eIF4GI-binding domains of rotavirus nonstructural protein NSP3. J. Virol. 1999, 73, 5411–5421. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Duan, L.; Zheng, Q.; Zhang, H.; Niu, Y.; Lou, Y.; Wang, H. The SARS-CoV-2 spike glycoprotein biosynthesis, structure, function, and antigenicity: Implications for the design of spike-based vaccine immunogens. Front. Immunol. 2020, 11, 576622. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Yang, C.; Xu, X.F.; Xu, W.; Liu, S.W. Structural and functional properties of SARS-CoV-2 spike protein: Potential antivirus drug development for COVID-19. Acta Pharmacol. Sin. 2020, 41, 1141–1149. [Google Scholar] [CrossRef] [PubMed]
- Medina-Enríquez, M.M.; Lopez-León, S.; Carlos-Escalante, J.A.; Aponte-Torres, Z.; Cuapio, A.; Wegman-Ostrosky, T. ACE2, the molecular doorway to SARS-CoV-2. Cell Biosci. 2020, 10, 148. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, M.; Kleine-Weber, H.; Schroeder, S.; Krüger, N.; Herrler, T.; Erichsen, S.; Schiergens, T.S.; Herrler, G.; Wu, N.H.; Nitsche, A.; et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell 2020, 181, 271–280.e8. [Google Scholar] [CrossRef]
- Brouwer, P.J.M.; Caniels, T.G.; van der Straten, K.; Snitselaar, J.L.; Aldon, Y.; Bangaru, S.; Torres, J.L.; Okba, N.M.A.; Claireaux, M.; Kerster, G.; et al. Potent neutralizing antibodies from COVID-19 patients define multiple targets of vulnerability. Science 2020, 369, 643–650. [Google Scholar] [CrossRef]
- Graham, C.; Seow, J.; Huettner, I.; Khan, H.; Kouphou, N.; Acors, S.; Winstone, H.; Pickering, S.; Pedro Galao, R.; Jose Lista, M.; et al. Impact of the B.1.1.7 variant on neutralizing monoclonal antibodies recognizing diverse epitopes on SARS-CoV-2 Spike. bioRxiv 2021. [Google Scholar] [CrossRef]
- Liu, L.; Wang, P.; Nair, M.S.; Yu, J.; Rapp, M.; Wang, Q.; Luo, Y.; Chan, J.F.; Sahi, V.; Figueroa, A.; et al. Potent neutralizing antibodies against multiple epitopes on SARS-CoV-2 spike. Nature 2020, 584, 450–456. [Google Scholar] [CrossRef]
- Rogers, T.F.; Zhao, F.; Huang, D.; Beutler, N.; Burns, A.; He, W.T.; Limbo, O.; Smith, C.; Song, G.; Woehl, J.; et al. Isolation of potent SARS-CoV-2 neutralizing antibodies and protection from disease in a small animal model. Science 2020, 369, 956–963. [Google Scholar] [CrossRef]
- Suryadevara, N.; Shrihari, S.; Gilchuk, P.; VanBlargan, L.A.; Binshtein, E.; Zost, S.J.; Nargi, R.S.; Sutton, R.E.; Winkler, E.S.; Chen, E.C.; et al. Neutralizing and protective human monoclonal antibodies recognizing the N-terminal domain of the SARS-CoV-2 spike protein. Cell 2021. [Google Scholar] [CrossRef]
- Wu, Y.; Wang, F.; Shen, C.; Peng, W.; Li, D.; Zhao, C.; Li, Z.; Li, S.; Bi, Y.; Yang, Y.; et al. A noncompeting pair of human neutralizing antibodies block COVID-19 virus binding to its receptor ACE2. Science 2020, 368, 1274–1278. [Google Scholar] [CrossRef] [PubMed]
- Xiaojie, S.; Yu, L.; Lei, Y.; Guang, Y.; Min, Q. Neutralizing antibodies targeting SARS-CoV-2 spike protein. Stem Cell Res. 2021, 50, 102125. [Google Scholar] [CrossRef] [PubMed]
- Zost, S.J.; Gilchuk, P.; Chen, R.E.; Case, J.B.; Reidy, J.X.; Trivette, A.; Nargi, R.S.; Sutton, R.E.; Suryadevara, N.; Chen, E.C.; et al. Rapid isolation and profiling of a diverse panel of human monoclonal antibodies targeting the SARS-CoV-2 spike protein. Nat. Med. 2020, 26, 1422–1427. [Google Scholar] [CrossRef] [PubMed]
- Arnold, M.; Patton, J.T.; McDonald, S.M. Culturing, storage, and quantification of rotaviruses. Curr. Protoc. Microbiol. 2009, 15, Unit 15C.3. [Google Scholar] [CrossRef]
- Philip, A.A.; Dai, J.; Katen, S.P.; Patton, J.T. Simplified reverse genetics method to recover recombinant rotaviruses expressing reporter proteins. J. Vis. Exp. 2020, 158, e61039. [Google Scholar] [CrossRef]
- Arnold, M.M.; Brownback, C.S.; Taraporewala, Z.F.; Patton, J.T. Rotavirus variant replicates efficiently although encoding an aberrant NSP3 that fails to induce nuclear localization of poly(A)-binding protein. J. Gen. Virol. 2012, 93 Pt 7, 1483–1494. [Google Scholar] [CrossRef] [Green Version]
- Matthijnssens, J.; Ciarlet, M.; McDonald, S.M.; Attoui, H.; Bányai, K.; Brister, J.R.; Buesa, J.; Esona, M.D.; Estes, M.K.; Gentsch, J.R.; et al. Uniformity of rotavirus strain nomenclature proposed by the Rotavirus Classification Working Group (RCWG). Arch. Virol. 2011, 156, 1397–1413. [Google Scholar] [CrossRef] [Green Version]
- Desselberger, U. What are the limits of the packaging capacity for genomic RNA in the cores of rotaviruses and of other members of the Reoviridae? Virus Res. 2020, 276, 197822. [Google Scholar] [CrossRef]
- Sockolosky, J.T.; Tiffany, M.R.; Szoka, F.C. Engineering neonatal Fc receptor-mediated recycling and transcytosis in recombinant proteins by short terminal peptide extensions. Proc. Natl. Acad. Sci. USA 2012, 109, 16095–16100. [Google Scholar] [CrossRef] [Green Version]
- Okba, N.M.A.; Widjaja, I.; van Dieren, B.; Aebischer, A.; van Amerongen, G.; de Waal, L.; Stittelaar, K.J.; Schipper, D.; Martina, B.; van den Brand, J.M.A.; et al. Particulate multivalent presentation of the receptor binding domain induces protective immune responses against MERS-CoV. Emerg. Microbes Infect. 2020, 9, 1080–1091. [Google Scholar] [CrossRef] [PubMed]
- Guest, J.D.; Wang, R.; Elkholy, K.H.; Chagas, A.; Chao, K.L.; Cleveland, T.E., IV; Kim, Y.C.; Keck, Z.Y.; Marin, A.; Yunus, A.S.; et al. Design of a native-like secreted form of the hepatitis C virus E1E2 heterodimer. Proc. Natl. Acad. Sci. USA 2021, 118, e2015149118. [Google Scholar] [CrossRef] [PubMed]
- Argentinian AntiCovid Consortium. Structural and functional comparison of SARS-CoV-2-spike receptor binding domain produced in Pichia pastoris and mammalian cells. Sci. Rep. 2020, 10, 21779. [Google Scholar] [CrossRef] [PubMed]
- Wen, B.; Deng, Y.; Guan, J.; Yan, W.; Wang, Y.; Tan, W.; Gao, J. Signal peptide replacements enhance expression and secretion of hepatitis C virus envelope glycoproteins. Acta Biochim. Biophys. Sin. 2011, 43, 96–102. [Google Scholar] [CrossRef] [Green Version]
- Characterisation of protease activity during SARS-CoV-2 infection identifies novel viral cleavage sites and cellular targets for drug repurposing. Available online: https://livrepository.liverpool.ac.uk/3106341/ (accessed on 20 April 2021).
- Boson, B.; Legros, V.; Zhou, B.; Siret, E.; Mathieu, C.; Cosset, F.L.; Lavillette, D.; Denolly, S. The SARS-CoV-2 envelope and membrane proteins modulate maturation and retention of the spike protein, allowing assembly of virus-like particles. J. Biol. Chem. 2020, 296, 100111. [Google Scholar] [CrossRef]
- Roulston, C.; Luke, G.A.; de Felipe, P.; Ruan, L.; Cope, J.; Nicholson, J.; Sukhodub, A.; Tilsner, J.; Ryan, M.D. ‘2A-like’ signal sequences mediating translational recoding: A novel form of dual protein targeting. Traffic 2016, 17, 923–939. [Google Scholar] [CrossRef] [Green Version]
- Luke, G.; Escuin, H.; De Felipe, P.; Ryan, M. 2A to the fore—Research, technology and applications. Biotechnol. Genet. Eng. Rev. 2010, 26, 223–260. [Google Scholar] [CrossRef]
- Liu, Z.; Chen, O.; Wall, J.; Zheng, M.; Zhou, Y.; Wang, L.; Vaseghi, H.R.; Qian, L.; Liu, J. Systematic comparison of 2A peptides for cloning multi-genes in a polycistronic vector. Sci. Rep. 2017, 7, 2193. [Google Scholar] [CrossRef]
- Sharma, P.; Yan, F.; Doronina, V.A.; Escuin-Ordinas, H.; Ryan, M.D.; Brown, J.D. 2A peptides provide distinct solutions to driving stop-carry on translational recoding. Nucleic Acids Res. 2012, 40, 3143–3151. [Google Scholar] [CrossRef] [Green Version]
- Shaimardanova, A.A.; Kitaeva, K.V.; Abdrakhmanova, I.I.; Chernov, V.M.; Rutland, C.S.; Rizvanov, A.A.; Chulpanova, D.S.; Solovyeva, V.V. Production and application of multicistronic constructs for various human disease therapies. Pharmaceutics 2019, 11, 580. [Google Scholar] [CrossRef] [Green Version]
- Huo, J.; Zhao, Y.; Ren, J.; Zhou, D.; Duyvesteyn, H.M.E.; Ginn, H.M.; Carrique, L.; Malinauskas, T.; Ruza, R.R.; Shah, P.N.M.; et al. Neutralization of SARS-CoV-2 by Destruction of the Prefusion Spike. Cell Host Microbe 2020, 28, 497. [Google Scholar] [CrossRef] [PubMed]
- McIntyre, M.; Rosenbaum, V.; Rappold, W.; Desselberger, M.; Wood, D.; Desselberger, U. Biophysical characterization of rotavirus particles containing rearranged genomes. J. Gen. Virol. 1987, 68 Pt 11, 2961–2966. [Google Scholar] [CrossRef]


| Primer | Sequence |
|---|---|
| Vector_For | TGACCATTTTGATACATGTTGAACAATCAAATACAG |
| Vector_Rev | GCTAGCCTTGTCATCGTCATCCT |
| NTD_For | GATGACAAGGCTAGCTGTGTTAATCTTACAACCAGAACTCAATTACCCC |
| NTD_Rev | GTATCAAAATGGTCAGTCAAGTGCACAGTCTACAGCATC |
| ExRBD_For | GATGACAAGGCTAGCGGAATCTATCAAACTTCTAACTTTAGAGTCCAACCA |
| ExRBD_Rev | GTATCAAAATGGTCATGTTATAACACTGACACCACCAAAAGAACA |
| RBD_For | GATGACAAGGCTAGCTTGTGCCCTTTTGGTGAAGTTT |
| RBD_Rev | GTATCAAAATGGTCAAGTTGCTGGTGCATGTAGAAGT |
| CR_For | GATGACAAGGCTAGCTCTATTGCCATACCCACAAATTTTACTATTAGTGT |
| CR_Rev | GTATCAAAATGGTCAAGTTGTGAAGTTCTTTTCTTGTGCAGG |
| S1_For | GATGACAAGGCTAGCGTGTTTGTTTTTCTTGTTTTATTGCCACTAGTCT |
| S1_Rev | GTATCAAAATGGTCAACGTGCCCGCCG |
| Virus Strain | Genome Segment 7 | |||||||
|---|---|---|---|---|---|---|---|---|
| RNA (bp) | Protein Product | NCBI Accession # | ||||||
| Abbreviated Name | Formal Name * | Genome Size/Increase Over wt (bp) | Uncleaved (aa) | 2A Cleaved (aa) | Uncleaved (kDa) | 2A Cleaved (kDa) | ||
| rSA11/wt | RVA/Simian-lab/USA/SA11wt/2019/G3P[2] | 18,559/0 | 1105 | 315 | nd | 36.4 | nd | LC178572 |
| rSA11/NSP3-fNTD | RVA/Simian-lab/USA/SA11(NSP3-P2A-CoV2:fNTD)/2020/G3P[2] | 19,537/978 | 2083 | 641 | 336 + 305 | 73.2 | 38.5 + 34.8 | MW059024 |
| rSA11/NSP3-fRBD | RVA/Simian-lab/USA/SA11(NSP3-P2A-CoV2:fRBD)/2020/G3P[2] | 19,264/705 | 1810 | 550 | 336 + 214 | 62.7 | 38.5 + 24.3 | MT655947 |
| rSA11/NSP3-fExRBD | RVA/Simian-lab/USA/SA11(NSP3-P2A-CoV2:fExRBD)/2020/G3P[2] | 19,564/1005 | 2110 | 650 | 336 + 314 | 74.7 | 38.5 + 35.2 | MT655946 |
| rSA11/NSP3-fCR | RVA/Simian-lab/USA/SA11(NSP3-P2A-CoV2:fCR)/2020/G3P[2] | 19,798/1239 | 2344 | 728 | 336 + 392 | 81.4 | 38.5 + 42.9 | MW059025 |
| rSA11/NSP3-fS1 | RVA/Simian-lab/USA/SA11(NSP3-P2A-CoV2:fS1)/2020/G3P[2] | 20,752/2193 | 3298 | 1046 | 336 + 710 | 118.1 | 38.5 + 79.6 | MW059026 |
| rSA11/NSP3-fS1/R1 | RVA/Simian-lab/USA/SA11(NSP3-P2A-CoV2:fS1/R1)/2020/G3P[2] | 19,757/1198 | 2303 | 431 | 336 + 95 | 49.6 | 38.5 + 11.1 | MW353715 |
| rSA11/NSP3-fS1/R2 | RVA/Simian-lab/USA/SA11(NSP3-P2A-CoV2:fS1/R2)/2020/G3P[2] | 19,333/683 | 1788 | 367 | 336 + 31 | 42.1 | 38.5 + 3.7 | MW353716 |
| rSA11/NSP3-fS1/R3 | RVA/Simian-lab/USA/SA11(NSP3-P2A-CoV2:fS1R3)/2020/G3P[2] | 18,951/392 | 1497 | 410 | 336 + 74 | 47.2 | 38.5 + 8.8 | MW353717 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Philip, A.A.; Patton, J.T. Rotavirus as an Expression Platform of Domains of the SARS-CoV-2 Spike Protein. Vaccines 2021, 9, 449. https://doi.org/10.3390/vaccines9050449
Philip AA, Patton JT. Rotavirus as an Expression Platform of Domains of the SARS-CoV-2 Spike Protein. Vaccines. 2021; 9(5):449. https://doi.org/10.3390/vaccines9050449
Chicago/Turabian StylePhilip, Asha Ann, and John Thomas Patton. 2021. "Rotavirus as an Expression Platform of Domains of the SARS-CoV-2 Spike Protein" Vaccines 9, no. 5: 449. https://doi.org/10.3390/vaccines9050449
APA StylePhilip, A. A., & Patton, J. T. (2021). Rotavirus as an Expression Platform of Domains of the SARS-CoV-2 Spike Protein. Vaccines, 9(5), 449. https://doi.org/10.3390/vaccines9050449







