Vaccines in Gastrointestinal Malignancies: From Prevention to Treatment
Abstract
1. Introduction
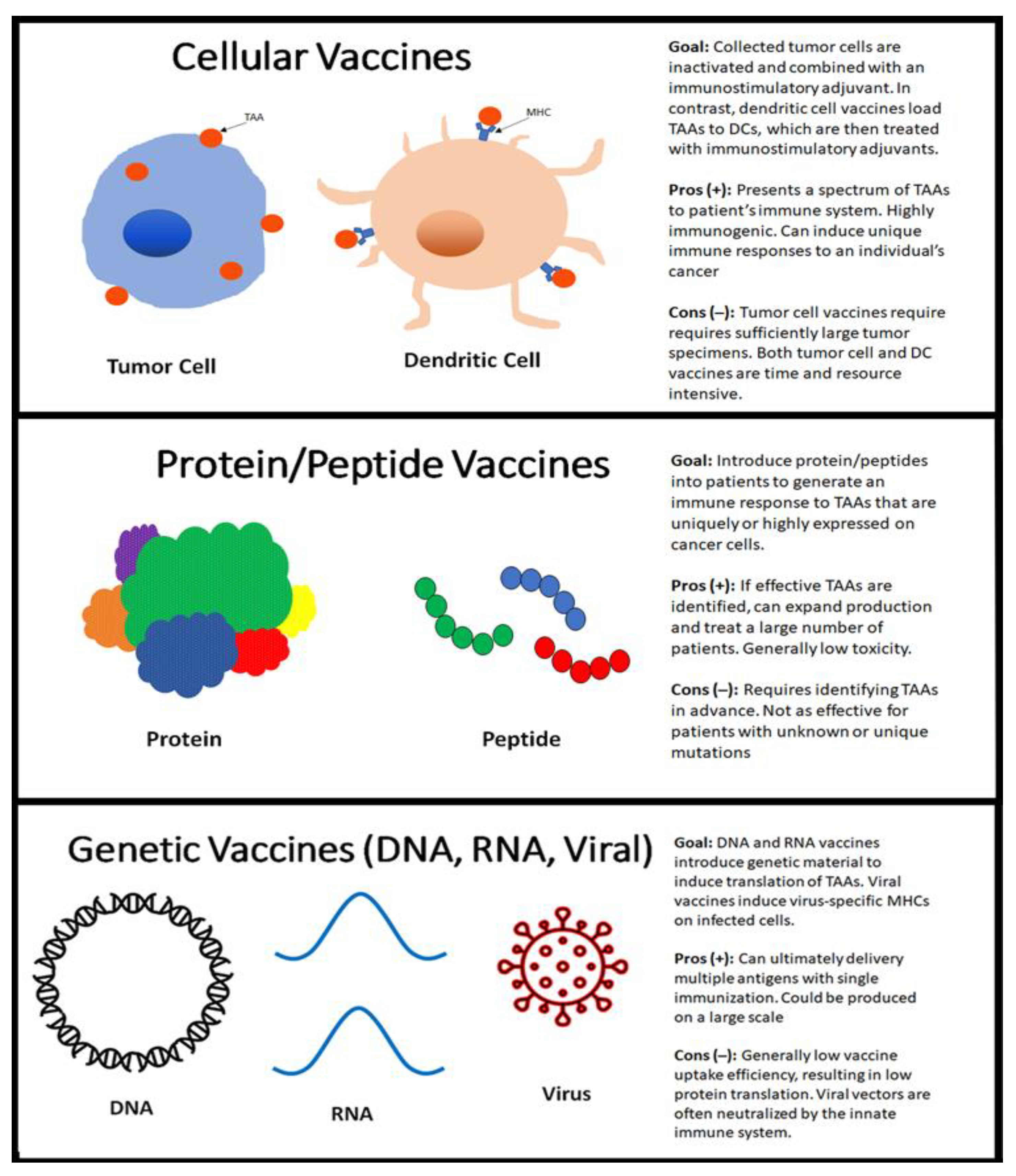
2. Role of Vaccines in Cancer
3. Types of Vaccines (Mechanisms)
4. Approved Vaccines
5. Vaccines in Gastrointestinal Malignancies
5.1. Colon Cancer
5.2. Gastric Cancer
5.3. Hepatocellular Carcinoma
5.4. Pancreatic Cancer
6. Vaccines in Prevention (HBV and HPV)
7. Challenges and Reasons for Inefficacy
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lollini, P.L.; Cavallo, F.; Nanni, P.; Forni, G. Vaccines for tumour prevention. Nat. Rev. Cancer 2006, 6, 204–216. [Google Scholar] [CrossRef]
- Hollingsworth, R.E.; Jansen, K. Turning the corner on therapeutic cancer vaccines. NPJ Vaccines 2019, 4, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Guo, C.; Manjili, M.H.; Subjeck, J.R.; Sarkar, D.; Fisher, P.B.; Wang, X.Y. Therapeutic cancer vaccines: Past, present, and future. Adv. Cancer Res. 2013, 119, 421–475. [Google Scholar] [CrossRef] [PubMed]
- Berger, M.; Kreutz, F.T.; Horst, J.L.; Baldi, A.C.; Koff, W.J. Phase I study with an autologous tumor cell vaccine for locally advanced or metastatic prostate cancer. J. Pharm. Pharm. Sci. 2007, 10, 144–152. [Google Scholar]
- Peters, L.C.; Brandhorst, J.S.; Hanna, M.G., Jr. Preparation of immunotherapeutic autologous tumor cell vaccines from solid tumors. Cancer Res. 1979, 39, 1353–1360. [Google Scholar]
- Sondak, V.K.; Sabel, M.S.; Mulé, J.J. Allogeneic and Autologous Melanoma Vaccines: Where Have We Been and Where Are We Going? Clin. Cancer Res. 2006, 12, 2337s–2341s. [Google Scholar] [CrossRef]
- Banchereau, J.; Briere, F.; Caux, C.; Davoust, J.; Lebecque, S.; Liu, Y.-J.; Pulendran, B.; Palucka, K. Immunobiology of Dendritic Cells. Annu. Rev. Immunol. 2000, 18, 767–811. [Google Scholar] [CrossRef] [PubMed]
- Kantoff, P.W.; Higano, C.S.; Shore, N.D.; Berger, E.R.; Small, E.J.; Penson, D.F.; Redfern, C.H.; Ferrari, A.C.; Dreicer, R.; Sims, R.B.; et al. Sipuleucel-T immunotherapy for castration-resistant prostate cancer. N. Engl. J. Med. 2010, 363, 411–422. [Google Scholar] [CrossRef]
- Gnjatic, S.; Ritter, E.; Büchler, M.W.; Giese, N.A.; Brors, B.; Frei, C.; Murray, A.; Halama, N.; Zörnig, I.; Chen, Y.-T.; et al. Seromic profiling of ovarian and pancreatic cancer. Proc. Natl. Acad. Sci. USA 2010, 107, 5088–5093. [Google Scholar] [CrossRef]
- Hofmann, O.; Caballero, O.L.; Stevenson, B.J.; Chen, Y.-T.; Cohen, T.; Chua, R.; Maher, C.A.; Panji, S.; Schaefer, U.; Kruger, A.; et al. Genome-wide analysis of cancer/testis gene expression. Proc. Natl. Acad. Sci. USA 2008, 105, 20422–20427. [Google Scholar] [CrossRef] [PubMed]
- Kufe, D.W. Mucins in cancer: Function, prognosis and therapy. Nat. Rev. Cancer 2009, 9, 874–885. [Google Scholar] [CrossRef]
- Tsang, K.Y.; Zaremba, S.; Nieroda, C.A.; Zhu, M.Z.; Hamilton, J.M.; Schlom, J. Generation of human cytotoxic T cells specific for human carcinoembryonic antigen epitopes from patients immunized with recombinant vaccinia-CEA vaccine. J. Natl. Cancer Inst. 1995, 87, 982–990. [Google Scholar] [CrossRef] [PubMed]
- Cho, H.-I.; Celis, E. Optimized Peptide Vaccines Eliciting Extensive CD8 T-Cell Responses with Therapeutic Antitumor Effects. Cancer Res. 2009, 69, 9012–9019. [Google Scholar] [CrossRef]
- Zom, G.G.; Khan, S.; Filippov, D.V.; Ossendorp, F. TLR ligand-peptide conjugate vaccines: Toward clinical application. Adv. Immunol. 2012, 114, 177–201. [Google Scholar] [CrossRef] [PubMed]
- Correale, P.; Nieroda, C.; Zaremba, S.; Zhu, M.; Schlom, J.; Tsang, K.Y.; Konstantin, W. In Vitro Generation of Human Cytotoxic T Lymphocytes Specific for Peptides Derived From Prostate-Specific Antigen. J. Natl. Cancer Inst. 1997, 89, 293–300. [Google Scholar] [CrossRef] [PubMed]
- Rivoltini, L.; Castelli, C.; Carrabba, M.; Mazzaferro, V.M.; Pilla, L.; Huber, V.; Coppa, J.; Gallino, G.; Scheibenbogen, C.; Squarcina, P.; et al. Human Tumor-Derived Heat Shock Protein 96 Mediates In Vitro Activation and In Vivo Expansion of Melanoma- and Colon Carcinoma-Specific T Cells. J. Immunol. 2003, 171, 3467–3474. [Google Scholar] [CrossRef]
- Schwartzentruber, D.J.; Lawson, D.H.; Richards, J.M.; Conry, R.M.; Miller, D.M.; Treisman, J.; Gailani, F.; Riley, L.; Conlon, K.; Pockaj, B.; et al. gp100 peptide vaccine and interleukin-2 in patients with advanced melanoma. N. Engl. J. Med. 2011, 364, 2119–2127. [Google Scholar] [CrossRef]
- Aurisicchio, L.; Ciliberto, G. Genetic cancer vaccines: Current status and perspectives. Expert Opin. Biol. Ther. 2012, 12, 1043–1058. [Google Scholar] [CrossRef] [PubMed]
- Pan, R.-Y.; Chung, W.-H.; Chu, M.-T.; Chen, S.-J.; Chen, H.-C.; Zheng, L.; Hung, S.-I. Recent Development and Clinical Application of Cancer Vaccine: Targeting Neoantigens. J. Immunol. Res. 2018, 2018, 1–9. [Google Scholar] [CrossRef]
- Orlandi, F.; Guevara-Patino, J.A.; Merghoub, T.; Wolchok, J.D.; Houghton, A.N.; Gregor, P.D. Combination of epitope-optimized DNA vaccination and passive infusion of monoclonal antibody against HER2/neu leads to breast tumor regression in mice. Vaccine 2011, 29, 3646–3654. [Google Scholar] [CrossRef]
- Kariko, K.; Weissman, D. Naturally occurring nucleoside modifications suppress the immunostimulatory activity of RNA: Implication for therapeutic RNA development. Curr. Opin. Drug Discov. Devel. 2007, 10, 523–532. [Google Scholar]
- antoff, P.W.; Schuetz, T.J.; Blumenstein, B.A.; Glode, L.M.; Bilhartz, D.L.; Wyand, M.; Manson, K.; Panicali, D.L.; Laus, R.; Schlom, J.; et al. Overall survival analysis of a phase II randomized controlled trial of a Poxviral-based PSA-targeted immunotherapy in metastatic castration-resistant prostate cancer. J. Clin. Oncol. 2010, 28, 1099–1105. [Google Scholar] [CrossRef]
- Kardani, K.; Bolhassani, A.; Shahbazi, S. Prime-boost vaccine strategy against viral infections: Mechanisms and benefits. Vaccine 2016, 34, 413–423. [Google Scholar] [CrossRef]
- Morales, A.; Eidinger, D.; Bruce, A. Intracavitary Bacillus Calmette-guerin in the Treatment of Superficial Bladder Tumors. J. Urol. 1976, 116, 180–182. [Google Scholar] [CrossRef]
- Lamm, D.L.; Blumenstein, B.A.; Crawford, E.D.; Montie, J.E.; Scardino, P.; Grossman, H.B.; Stanisic, T.H.; Smith, J.A.; Sullivan, J.; Sarosdy, M.F.; et al. A Randomized Trial of Intravesical Doxorubicin and Immunotherapy with Bacille Calmette–Guérin for Transitional-Cell Carcinoma of the Bladder. N. Engl. J. Med. 1991, 325, 1205–1209. [Google Scholar] [CrossRef] [PubMed]
- Lamm, D.L.; Blumenstein, B.A.; Crissman, J.D.; Montie, J.E.; Gottesman, J.E.; Lowe, B.A.; Sarosdy, M.F.; Bohl, R.D.; Grossman, H.B.; Beck, T.M.; et al. Maintenance bacillus calmette-guerin immunotherapy for recurrent ta, t1 and carcinoma in situ transitional cell carcinoma of the bladder: A randomized southwest oncology group study. J. Urol. 2000, 163, 1124–1129. [Google Scholar] [CrossRef]
- Higano, C.S.; Schellhammer, P.F.; Small, E.J.; Burch, P.A.; Nemunaitis, J.; Yuh, L.; Provost, N.; Frohlich, M.W. Integrated data from 2 randomized, double-blind, placebo-controlled, phase 3 trials of active cellular immunotherapy with sipuleucel-T in advanced prostate cancer. Cancer 2009, 115, 3670–3679. [Google Scholar] [CrossRef] [PubMed]
- Small, E.J.; Schellhammer, P.F.; Higano, C.S.; Redfern, C.H.; Nemunaitis, J.J.; Valone, F.H.; Verjee, S.S.; Jones, L.A.; Hershberg, R.M. Placebo-Controlled Phase III Trial of Immunologic Therapy with Sipuleucel-T (APC8015) in Patients with Metastatic, Asymptomatic Hormone Refractory Prostate Cancer. J. Clin. Oncol. 2006, 24, 3089–3094. [Google Scholar] [CrossRef]
- Andtbacka, R.H.; Kaufman, H.L.; Collichio, F.; Amatruda, T.; Senzer, N.; Chesney, J.; Delman, K.A.; Spitler, L.E.; Puzanov, I.; Agarwala, S.S.; et al. Talimogene Laherparepvec Improves Durable Response Rate in Patients with Advanced Melanoma. J. Clin. Oncol. 2015, 33, 2780–2788. [Google Scholar] [CrossRef]
- Finn, O.J. The dawn of vaccines for cancer prevention. Nat. Rev. Immunol. 2018, 18, 183–194. [Google Scholar] [CrossRef] [PubMed]
- Wagner, S.; Mullins, C.S.; Linnebacher, M. Colorectal cancer vaccines: Tumor-associated antigens vs neoantigens. World J. Gastroenterol. 2018, 24, 5418–5432. [Google Scholar] [CrossRef]
- Lesterhuis, W.J.; De Vries, I.J.M.; Schuurhuis, D.H.; Boullart, A.C.I.; Jacobs, J.F.M.; De Boer, A.J.; Scharenborg, N.M.; Brouwer, H.M.H.; Van De Rakt, M.W.M.M.; Figdor, C.G.; et al. Vaccination of colorectal cancer patients with CEA-loaded dendritic cells: Antigen-specific T cell responses in DTH skin tests. Ann. Oncol. 2006, 17, 974–980. [Google Scholar] [CrossRef]
- Kavanagh, B.; Ko, A.; Venook, A.; Margolin, K.; Zeh, H.; Lotze, M.; Schillinger, B.; Liu, W.; Lu, Y.; Mitsky, P.; et al. Vaccination of metastatic colorectal cancer patients with matured dendritic cells loaded with multiple major histocompatibility complex class I peptides. J. Immunother. 2007, 30, 762–772. [Google Scholar] [CrossRef]
- Kawamura, J.; Sugiura, F.; Sukegawa, Y.; Yoshioka, Y.; Hida, J.I.; Hazama, S.; Okuno, K. Multicenter, phase II clinical trial of peptide vaccination with oral chemotherapy following curative resection for stage III colorectal cancer. Oncol. Lett. 2018, 15, 4241–4247. [Google Scholar] [CrossRef] [PubMed]
- Toubaji, A.; Achtar, M.; Provenzano, M.; Herrin, V.E.; Behrens, R.; Hamilton, M.; Bernstein, S.; Venzon, D.; Gause, B.; Marincola, F.; et al. Pilot study of mutant ras peptide-based vaccine as an adjuvant treatment in pancreatic and colorectal cancers. Cancer Immunol. Immunother. 2008, 57, 1413–1420. [Google Scholar] [CrossRef] [PubMed]
- Harris, J.E.; Ryan, L.; Hoover, H.C., Jr.; Stuart, R.K.; Oken, M.M.; Benson, A.B., 3rd; Mansour, E.; Haller, D.G.; Manola, J.; Hanna, M.G., Jr. Adjuvant active specific immunotherapy for stage II and III colon cancer with an autologous tumor cell vaccine: Eastern Cooperative Oncology Group Study E5283. J. Clin. Oncol. 2000, 18, 148–157. [Google Scholar] [CrossRef] [PubMed]
- Hazama, S.; Nakamura, Y.; Takenouchi, H.; Suzuki, N.; Tsunedomi, R.; Inoue, Y.; Tokuhisa, Y.; Iizuka, N.; Yoshino, S.; Takeda, K.; et al. A phase I study of combination vaccine treatment of five therapeutic epitope-peptides for metastatic colorectal cancer; safety, immunological response, and clinical outcome. J. Transl. Med. 2014, 12, 63. [Google Scholar] [CrossRef]
- Sato, Y.; Maeda, Y.; Shomura, H.; Sasatomi, T.; Takahashi, M.; Une, Y.; Kondo, M.; Shinohara, T.; Hida, N.; Katagiri, K.; et al. A phase I trial of cytotoxic T-lymphocyte precursor-oriented peptide vaccines for colorectal carcinoma patients. Br. J. Cancer 2004, 90, 1334–1342. [Google Scholar] [CrossRef]
- Rahma, O.E.; Hamilton, J.M.; Wojtowicz, M.; Dakheel, O.; Bernstein, S.; Liewehr, D.J.; Steinberg, S.M.; Khleif, S.N. The immunological and clinical effects of mutated ras peptide vaccine in combination with IL-2, GM-CSF, or both in patients with solid tumors. J. Transl. Med. 2014, 12, 55. [Google Scholar] [CrossRef] [PubMed]
- Higashihara, Y.; Kato, J.; Nagahara, A.; Izumi, K.; Konishi, M.; Kodani, T.; Serizawa, N.; Osada, T.; Watanabe, S. Phase I clinical trial of peptide vaccination with URLC10 and VEGFR1 epitope peptides in patients with advanced gastric cancer. Int. J. Oncol. 2014, 44, 662–668. [Google Scholar] [CrossRef] [PubMed]
- Ogasawara, M. Dendritic cell vaccine-based immunotherapy in combination with salvage chemotherapy for patients with advanced or relapsed gastric cancer. Ann. Oncol. 2018, 29, v21. [Google Scholar] [CrossRef]
- Ajani, J.A.; Hecht, J.R.; Ho, L.; Baker, J.; Oortgiesen, M.; Eduljee, A.; Michaeli, D. An open-label, multinational, multicenter study of G17DT vaccination combined with cisplatin and 5-fluorouracil in patients with untreated, advanced gastric or gastroesophageal cancer: The GC4 study. Cancer 2006, 106, 1908–1916. [Google Scholar] [CrossRef]
- Fujiwara, Y.; Sugimura, K.; Miyata, H.; Omori, T.; Nakano, H.; Mochizuki, C.; Shimizu, K.; Saito, H. A pilot study of post-operative adjuvant vaccine for advanced gastric cancer Adjuvant cancer vaccine for gastric can-cer. Yonago Acta Med. 2017, 60, 101–105. [Google Scholar] [CrossRef]
- Butterfield, L.H.; Ribas, A.; Meng, W.S.; Dissette, V.B.; Amarnani, S.; Vu, H.T.; Seja, E.; Todd, K.; Glaspy, J.A.; McBride, W.H.; et al. T cell responses to HLA-A*0201 immunodominant peptides derived from alpha-fetoprotein in patients with hepa-tocellular cancer. Clin. Cancer Res. 2003, 9, 5902–5908. [Google Scholar]
- Butterfield, L.H.; Ribas, A.; Dissette, V.B.; Lee, Y.; Yang, J.Q.; De La Rocha, P.; Duran, S.D.; Hernandez, J.; Seja, E.; Potter, D.M.; et al. A Phase I/II Trial Testing Immunization of Hepatocellular Carcinoma Patients with Dendritic Cells Pulsed with Four α-Fetoprotein Peptides. Clin. Cancer Res. 2006, 12, 2817–2825. [Google Scholar] [CrossRef] [PubMed]
- Nakagawa, H.; Mizukoshi, E.; Kobayashi, E.; Tamai, T.; Hamana, H.; Ozawa, T.; Kishi, H.; Kitahara, M.; Yamashita, T.; Arai, K.; et al. Association Between High-Avidity T-Cell Receptors, Induced by α-Fetoprotein−Derived Peptides, and Anti-Tumor Effects in Patients with Hepatocellular Carcinoma. Gastroenterology 2017, 152, 1395–1406.e10. [Google Scholar] [CrossRef] [PubMed]
- Abdul-Latif, M.; Townsend, K.; Dearman, C.; Shiu, K.-K.; Khan, K. Immunotherapy in gastrointestinal cancer: The current scenario and future perspectives. Cancer Treat. Rev. 2020, 88, 102030. [Google Scholar] [CrossRef] [PubMed]
- Rizell, M.; Eilard, M.S.; Andersson, M.; Andersson, B.; Karlsson-Parra, A.; Suenaert, P. Phase 1 Trial with the Cell-Based Immune Primer Ilixadencel, Alone, and Combined with Sorafenib, in Advanced Hepatocellular Carcinoma. Front. Oncol. 2019, 9, 19. [Google Scholar] [CrossRef] [PubMed]
- Greten, T.F.; Forner, A.; Korangy, F.; N’Kontchou, G.; Barget, N.; Ayuso, C.; Ormandy, L.A.; Manns, M.P.; Beaugrand, M.; Bruix, J. A phase II open label trial evaluating safety and efficacy of a telomerase peptide vaccination in patients with advanced hepatocellular carcinoma. BMC Cancer 2010, 10, 209. [Google Scholar] [CrossRef]
- Sawada, Y.; Yoshikawa, T.; Nobuoka, D.; Shirakawa, H.; Kuronuma, T.; Motomura, Y.; Mizuno, S.; Ishii, H.; Nakachi, K.; Konishi, M.; et al. Phase I Trial of a Glypican-3–Derived Peptide Vaccine for Advanced Hepatocellular Carcinoma: Immunologic Evidence and Potential for Improving Overall Survival. Clin. Cancer Res. 2012, 18, 3686–3696. [Google Scholar] [CrossRef]
- Sawada, Y.; Yoshikawa, T.; Ofuji, K.; Yoshimura, M.; Tsuchiya, N.; Takahashi, M. Phase II study of the GPC3-derived peptide vaccine as an adjuvant therapy for hepatocellular carcinoma patients. Oncoimmunology 2016, 5, e1129483. [Google Scholar] [CrossRef] [PubMed]
- Miyazawa, M.; Katsuda, M.; Maguchi, H.; Katanuma, A.; Ishii, H.; Ozaka, M.; Yamao, K.; Imaoka, H.; Kawai, M.; Hirono, S.; et al. Phase II clinical trial using novel peptide cocktail vaccine as a postoperative adjuvant treatment for surgically resected pancreatic cancer patients. Int. J. Cancer 2017, 140, 973–982. [Google Scholar] [CrossRef]
- Weitzenfeld, P.; Bournazos, S.; Ravetch, J.V. Antibodies targeting sialyl Lewis A mediate tumor clearance through distinct effector pathways. J. Clin. Investig. 2019, 129, 3952–3962. [Google Scholar] [CrossRef] [PubMed]
- Ward, J.P.; Gubin, M.M.; Schreiber, R.D. The Role of Neoantigens in Naturally Occurring and Therapeutically Induced Immune Responses to Cancer. Adv. Immunol. 2016, 130, 25–74. [Google Scholar] [CrossRef] [PubMed]
- Bassani-Sternberg, M.; Digklia, A.; Huber, F.; Wagner, D.; Sempoux, C.; Stevenson, B.J.; Thierry, A.-C.; Michaux, J.; Pak, H.; Racle, J.; et al. A Phase Ib Study of the Combination of Personalized Autologous Dendritic Cell Vaccine, Aspirin, and Standard of Care Adjuvant Chemotherapy Followed by Nivolumab for Resected Pancreatic Adenocarcinoma—A Proof of Antigen Discovery Feasibility in Three Patients. Front. Immunol. 2019, 10, 1832. [Google Scholar] [CrossRef]
- Pan, L.; Shang, N.; Shangguan, J.; Figini, M.; Xing, W.; Wang, B.; Sun, C.; Yang, J.; Zhang, Y.; Hu, S.; et al. Magnetic resonance imaging monitoring therapeutic response to dendritic cell vaccine in murine orthotopic pancreatic cancer models. Am. J. Cancer Res. 2019, 9, 562–573. [Google Scholar]
- Rong, Y.; Qin, X.; Jin, D.; Lou, W.; Wu, L.; Wang, D.; Wu, W.; Ni, X.; Mao, Z.; Kuang, T.; et al. A phase I pilot trial of MUC1-peptide-pulsed dendritic cells in the treatment of advanced pancreatic cancer. Clin. Exp. Med. 2011, 12, 173–180. [Google Scholar] [CrossRef]
- Mehrotra, S.; Britten, C.D.; Chin, S.; Garrett-Mayer, E.; Cloud, C.A.; Li, M.; Scurti, G.; Salem, M.; Nelson, M.H.; Thomas, M.B.; et al. Vaccination with poly(IC:LC) and peptide-pulsed autologous dendritic cells in patients with pancreatic cancer. J. Hematol. Oncol. 2017, 10, 1–13. [Google Scholar] [CrossRef]
- de Martel, C.; Ferlay, J.; Franceschi, S.; Vignat, J.; Bray, F.; Forman, D.; Plummer, M. Global burden of cancers attributable to infections in 2008: A review and synthetic analysis. Lancet Oncol. 2012, 13, 607–615. [Google Scholar] [CrossRef]
- Kim, M.N.; Han, K.-H.; Ahn, S.H. Prevention of Hepatocellular Carcinoma: Beyond Hepatitis B Vaccination. Semin. Oncol. 2015, 42, 316–328. [Google Scholar] [CrossRef] [PubMed]
- Chang, M.H.; You, S.-L.; Chen, C.-J.; Liu, C.-J.; Lai, M.-W.; Wu, T.-C.; Wu, S.-F.; Lee, C.-M.; Yang, S.-S.; Chu, H.-C.; et al. Long-term Effects of Hepatitis B Immunization of Infants in Preventing Liver Cancer. Gastroenterology 2016, 151, 472–480.e1. [Google Scholar] [CrossRef] [PubMed]
- Hurez, V.; Padrón, Á.S.; Svatek, R.S.; Curiel, T.J. Considerations for successful cancer immunotherapy in aged hosts. Clin. Exp. Immunol. 2016, 187, 53–63. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Zhao, J.; Zhang, L.; Wei, F.; Lian, Y.; Wu, Y.; Gong, Z.; Zhang, S.; Zhou, J.; Cao, K.; et al. Role of tumor microenvironment in tumorigenesis. J. Cancer 2017, 8, 761–773. [Google Scholar] [CrossRef] [PubMed]
- Hegde, P.S.; Chen, D.S. Top 10 Challenges in Cancer Immunotherapy. Immunity 2020, 52, 17–35. [Google Scholar] [CrossRef] [PubMed]
- Parkhurst, M.R.; Yang, J.C.; Langan, R.C.; Dudley, M.E.; Nathan, D.-A.N.; Feldman, S.A.; Davis, J.L.; Morgan, R.A.; Merino, M.J.; Sherry, R.M.; et al. T Cells Targeting Carcinoembryonic Antigen Can Mediate Regression of Metastatic Colorectal Cancer but Induce Severe Transient Colitis. Mol. Ther. 2011, 19, 620–626. [Google Scholar] [CrossRef]
- Rahma, O.; Samir, N. Therapeutic vaccines for gastrointestinal cancers. Gastroenterol. Hepatol. 2011, 7, 517. [Google Scholar]
- Mogensen, M.B.; Rossing, M.; Østrup, O.; Larsen, P.N.; Engel, P.H.; Jørgensen, L. N Genomic alterations accompanying tumour evolution in colorectal cancer: Tracking the differences between prima-ry tumours and synchronous liver metastases by whole-exome sequencing. BMC Cancer 2018, 18, 752. [Google Scholar] [CrossRef]
- Jacobs, J.J.L.; Snackey, C.; Geldof, A.A.; Characiejus, D.; Van Moorselaar, R.J.; Otter, W.D. Inefficacy of therapeutic cancer vaccines and proposed improvements. Casus of prostate cancer. Anticancer. Res. 2014, 34, 2689–2700. [Google Scholar]
- Jou, J.; Harrington, K.J.; Zocca, M.-B.; Ehrnrooth, E.; Cohen, E.E. The Changing Landscape of Therapeutic Cancer Vaccines—Novel Platforms and Neoantigen Identification. Clin. Cancer Res. 2021, 27, 689–703. [Google Scholar] [CrossRef]
- Safety and Efficacy Study for MG-7-DC Vaccine in Gastric Cancer Treatment. Available online: https://clinicaltrials.gov/ct2/show/NCT04567069 (accessed on 12 June 2021).
- Nivolumab, Ipilimumab and OTSGC-A24 Therapeutic Peptide Vaccine in Gastric Cancer—A Combination Immunotherapy Phase Ib Study (da VINci). Available online: https://clinicaltrials.gov/ct2/show/NCT03784040 (accessed on 12 June 2021).
- A Study of IMU-131(HER-Vaxx) and Chemotherapy Compared to Chemotherapy Only in Patients with HER2 Positive Advanced Gastric Cancer. Available online: https://clinicaltrials.gov/ct2/show/NCT02795988 (accessed on 12 June 2021).
- DC Vaccine in Colorectal Cancer. Available online: https://clinicaltrials.gov/ct2/show/NCT03730948 (accessed on 12 June 2021).
- Intratumoral Influenza Vaccine for Early Colorectal Cancer. Available online: https://clinicaltrials.gov/ct2/show/NCT04591379 (accessed on 12 June 2021).
- Vaccination with Autologous Dendritic Cells Loaded with Autologous Tumour Homogenate after Curative Resection for Stage IV Colorectal Cancer (COREVAX-1). Available online: https://clinicaltrials.gov/ct2/show/NCT02919644 (accessed on 12 June 2021).
- GVAX for Colorectal Cancer. Available online: https://clinicaltrials.gov/ct2/show/NCT01952730 (accessed on 12 June 2021).
- A Trial of Perioperative CV301 Vaccination in Combination with Nivolumab and Systemic Chemotherapy for Metastatic CRC. Available online: https://clinicaltrials.gov/ct2/show/NCT03547999 (accessed on 12 June 2021).
- Phase 1b Study to Evaluate ATP128, with or without BI 754091, in Patients with Stage IV Colorectal Cancer (KISIMA-01). Available online: https://clinicaltrials.gov/ct2/show/NCT04046445 (accessed on 12 June 2021).
- Trial of PalloV-CC in Colon Cancer. Available online: https://clinicaltrials.gov/ct2/show/NCT03827967 (accessed on 12 June 2021).
- DNAJB1-PRKACA Fusion Kinase Peptide Vaccine Combined with Nivolumab and Ipilimumab for Patients with Fi-brolamellar Hepatocellular Carcinoma. Available online: https://clinicaltrials.gov/ct2/show/NCT04248569 (accessed on 12 June 2021).
- "Cocktail" Therapy for Hepatitis B Related Hepatocellular Carcinoma. Available online: https://clinicaltrials.gov/ct2/show/NCT04317248 (accessed on 12 June 2021).
- GNOS-PV02 Personalized Neoantigen Vaccine, INO-9012 and Pembrolizumab in Subjects with Advanced HCC. Available online: https://clinicaltrials.gov/ct2/show/NCT04251117 (accessed on 12 June 2021).
- Neoantigen Peptide Vaccine Strategy in Pancreatic Cancer Patients Following Surgical Resection and Adjuvant Chemothera-py. Available online: https://clinicaltrials.gov/ct2/show/NCT03956056 (accessed on 12 June 2021).
- Clinical Trial on Personalized Neoantigen Vaccine for Pancreatic Tumor. Available online: https://clinicaltrials.gov/ct2/show/NCT03558945 (accessed on 12 June 2021).
- A Trial of Boost Vaccinations of Pancreatic Tumor Cell Vaccine. Available online: https://clinicaltrials.gov/ct2/show/NCT01088789 (accessed on 12 June 2021).
- Neoadjuvant/Adjuvant GVAX Pancreas Vaccine (with CY) with or without Nivolumab and Urelumab Trial for Surgically Resectable Pancreatic Cancer. Available online: https://clinicaltrials.gov/ct2/show/NCT02451982 (accessed on 12 June 2021).
- GVAX Pancreas Vaccine (with CY) in Combination with Nivolumab and SBRT for Patients with Borderline Resectable Pan-creatic Cancer. Available online: https://clinicaltrials.gov/ct2/show/NCT03161379 (accessed on 12 June 2021).
- Study of Personalized Tumor Vaccines (PCVs) and a PD-L1 Blocker in Patients with Pancreatic Cancer That Can be Treated with Surgery. Available online: https://www.clinicaltrials.gov/ct2/show/NCT04161755 (accessed on 12 June 2021).
- Study of CRS-207, Nivolumab, and Ipilimumab with or without GVAX Pancreas Vaccine (with Cy) in Patients with Pancre-atic Cancer. Available online: https://www.clinicaltrials.gov/ct2/show/NCT03190265 (accessed on 12 June 2021).
- DC Vaccine in Pancreatic Cancer. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6694698/ (accessed on 12 June 2021).
- Epacadostat, Pembrolizumab, and CRS-207, with or without CY/GVAX Pancreas in Patients with Metastatic Pancreas Cancer. Available online: https://clinicaltrials.gov/ct2/show/NCT03006302 (accessed on 12 June 2021).
- Personalized Vaccine with SOC Chemo Followed by Nivo in Pancreatic Cancer. Available online: https://clinicaltrials.gov/ct2/show/NCT04627246 (accessed on 12 June 2021).
- Trial of Neoadjuvant and Adjuvant Nivolumab and BMS-813160 with or without GVAX for Locally Advanced Pancreatic Ductal Adenocarcinomas. Available online: https://clinicaltrials.gov/ct2/show/NCT03767582 (accessed on 12 June 2021).
- Maintenance Therapy with OSE2101 Vaccine Alone or in Combination with Nivolumab, or FOLFIRI after Induction Thera-py with FOLFIRINOX in Patients with Locally Advanced or Metastatic Pancreatic Ductal Adenocarcinoma (TEDOPAM). Available online: https://clinicaltrials.gov/ct2/show/NCT03806309 (accessed on 12 June 2021).
| Author (Date)—Study Name | Treatment Regimen | Total Patients | Patient Population | ORR/CR | mRFS (Months) HR, p-Value | mOS (Months) HR, p-Value |
|---|---|---|---|---|---|---|
| Lamm et al., (1991), SWOG 8507 [25] | Intravesicular BCG vs. intravesicular doxorubicin | 262 | Ta, T1, in situ transitional cell carcinoma of bladder | NR/70% | 22.4 vs. 10.4 | NR |
| NR/34% | NR, p = 0.015 | |||||
| Lamm et al., (2000), SWOG 8507 [26] | Maintenance intravesicular BCG vs. placebo | 384 | Ta, T1, in situ transitional cell carcinoma of bladder | NR | 76.8 vs. 35.7 | NR |
| NR, p < 0.0001 | ||||||
| Small et al., (2006), IMPACT [28] | Sipuleucel-T vs. placebo | 512 | Metastatic hormone-refractory prostate cancer | NR | 11.7 vs. 10.0 | 25.9 vs. 21.4 |
| NR, p = 0.052 | NR, p = 0.01 | |||||
| Andtbacka et al., (2015) [29] | Talimogene laherparepvec vs. GM-CSF | 436 | Unresectable stage IIIB/C and stage IV melanoma | 26%/10.8% | NR | 23.3 vs. 18.9 |
| 5.7%/<1% | HR 0.79, p = 0.51 |
| GI Malignancy | Trial Name | Intervention/Study Arms |
|---|---|---|
| Gastric Cancer | Safety and Efficacy Study for MG-7-DC Vaccine in Gastric Cancer Treatment [70] | DC vaccine DC vaccine + CTL DC vaccine + Sintilimab Injection (PD-1 monoclonal ab) |
| Nivolumab, Ipilimumab, and OTSGC-A24 Therapeutic Peptide Vaccine in Gastric Cancer—a Combination Immunotherapy Phase Ib Study [71] | OTSGC-A24 + nivolumab OTSGC-A24 + nivolumab + ipilimumab | |
| A Study of IMU-131(HER-Vaxx) and Chemotherapy Compared to Chemotherapy Only in Patients With HER2 Positive Advanced Gastric Cancer [72] | IMU-131 + Cisplatin + 5-FU or Capecitabine IMU-131 + Cisplatin + 5-FU or Capecitabine or Oxaliplatin and Capecitabine Cisplatin + 5-FU or Capecitabine or Oxaliplatin and Capecitabine | |
| Colorectal Cancer | DC Vaccine in Colorectal Cancer [73] | DC vaccine |
| Intratumoral Influenza Vaccine for Early Colorectal Cancer [74] | Influenza Vaccine | |
| Vaccination With Autologous Dendritic Cells Loaded With Autologous Tumour Homogenate After Curative Resection for Stage IV Colorectal Cancer [75] | Autologous dendritic cells loaded with autologous tumour homogenate + Interleukin-2 (IL2) | |
| GVAX for Colorectal Cancer [76] | GVAX | |
| A Trial of Perioperative CV301 Vaccination in Combination With Nivolumab and Systemic Chemotherapy for Metastatic CRC [77] | mFOLFOX6 + nivolumab nivolumab + MVA-BN-CV301 + FPV-CV301 | |
| Phase 1b Study to Evaluate ATP128, With or Without BI 754091, in Patients With Stage IV Colorectal Cancer [78] | ATP128 + BI 754091 | |
| Trial of PalloV-CC in Colon Cancer [79] | PalloV-CC | |
| HCC | DNAJB1-PRKACA Fusion Kinase Peptide Vaccine Combined With Nivolumab and Ipilimumab for Patients With Fibrolamellar Hepatocellular Carcinoma [80] | DNAJB1-PRKACA peptide vaccine + Nivolumab + Ipilimumab |
| “Cocktail” Therapy for Hepatitis B Related Hepatocellular Carcinoma [81] | MSDCV with radical surgery therapy Radical surgery therapy MSDCV with TACE therapy TACE Therapy MSDCV with Sorafenib or Lenvatinib Sorafenib or Lenvatinib | |
| GNOS-PV02 Personalized Neoantigen Vaccine, INO-9012, and Pembrolizumab in Subjects With Advanced HCC [82] | GNOS-PV02 + INO-9012 + Pembrolizumab | |
| Pancreatic Cancer | Neoantigen Peptide Vaccine Strategy in Pancreatic Cancer Patients Following Surgical Resection and Adjuvant Chemotherapy ([83]) | Neoantigen Peptide Vaccine + poly IC:LC |
| Clinical Trial on Personalized Neoantigen Vaccine For Pancreatic Cancer ([84]) | Personalized neoantigen vaccine | |
| A Trial of Boost Vaccionations of Pancreatic Tumor Cell Vaccine ([85]) | Neo vaccine Neo vaccine + single dose cyclophosphamide Neo vaccine + metronomic cyclophosphamide | |
| Neoadjuvant/Adjuvant GVAX Pancreas Vaccine (With CY) With or Without Nivolumab and Urelumab Trial for Surgically Resectable Pancreatic Cancer ([86]) | Cyclophosphamide + GVAX Cyclophosphamide + GVAX + nivolumab Cyclophosphamide + GVAX + nivoulumab + Urelumab | |
| GVAX Pancreas Vaccine (With CY) in Combination With Nivolumab and SBRT for Patients With Borderline Resectable Pancreatic Cancer ([87]) | Cyclophosphamide + nivolumab + GVAX + SBRT | |
| Study of Personalized Tumor Vaccines (PCVs) and a PD-L1 Blocker in Patients With Pancreatic Cancer That Can be Treated With Surgery ([88]) | Atezolizumab + RO7198457 + mFOLFIRINOX | |
| Study of CRS-207, Nivolumab, and Ipilimumab With or Without GVAX Pancreas Vaccine (With Cy) in Patients With Pancreatic Cancer ([89]) | Cyclophosphamide + Nivolumab + Ipilimumab + GVAX + CRS-207 Nivolumab + Ipilimumab + CRS-207 | |
| DC Vaccine in Pancreatic Cancer ([90]) | DC vaccine | |
| Epacadostat, Pembrolizumab, and CRS-207, With or Without CY/GVAX Pancreas in Patients With Metastatic Pancreas Cancer ([91]) | Epacadostat + Pembrolizumab + CRS-207 + Cyclophosphamide + GVAX Epacadostat + Pembrolizumab + CRS-207 | |
| Personalized Vaccine With SOC Chemo Followed by Nivo in Pancreatic Cancer ([92]) | PEP-DC vaccine + nivolumab + gemcitabine/capecitabine | |
| Trial of Neoadjuvant and Adjuvant Nivolumab and BMS-813160 With or Without GVAX for Locally Advanced Pancreatic Ductal Adenocarcinomas.([93]) | SBRT + Nivolumab + CCR2/CCR5 dual antagonist + GVAX SBRT + Nivolumab + CCR2/CCR5 dual antagonist | |
| Maintenance Therapy With OSE2101 Vaccine Alone or in Combination With Nivolumab, or FOLFIRI After Induction Therapy With FOLFIRINOX in Patients With Locally Advanced or Metastatic Pancreatic Ductal Adenocarcinoma (TEDOPAM) ([94]) | FOLFIRI OSE2101 vaccine OSE2101 vaccine + Nivolumab |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chudasama, R.; Phung, Q.; Hsu, A.; Almhanna, K. Vaccines in Gastrointestinal Malignancies: From Prevention to Treatment. Vaccines 2021, 9, 647. https://doi.org/10.3390/vaccines9060647
Chudasama R, Phung Q, Hsu A, Almhanna K. Vaccines in Gastrointestinal Malignancies: From Prevention to Treatment. Vaccines. 2021; 9(6):647. https://doi.org/10.3390/vaccines9060647
Chicago/Turabian StyleChudasama, Rani, Quan Phung, Andrew Hsu, and Khaldoun Almhanna. 2021. "Vaccines in Gastrointestinal Malignancies: From Prevention to Treatment" Vaccines 9, no. 6: 647. https://doi.org/10.3390/vaccines9060647
APA StyleChudasama, R., Phung, Q., Hsu, A., & Almhanna, K. (2021). Vaccines in Gastrointestinal Malignancies: From Prevention to Treatment. Vaccines, 9(6), 647. https://doi.org/10.3390/vaccines9060647





