Role of Lipoproteins in the Pathophysiology of Breast Cancer
Abstract
:1. Introduction
1.1. Role of Obesity in Breast Cancer Development
1.2. Role of Adiposity in Obese Patients and Its Negative Effect on Prognosis
1.3. Importance of Cholesterol in Lipoprotein Synthesis
2. Clinical and Epidemiologic Studies of Breast Cancer Incidence in Association with Cholesterol Levels
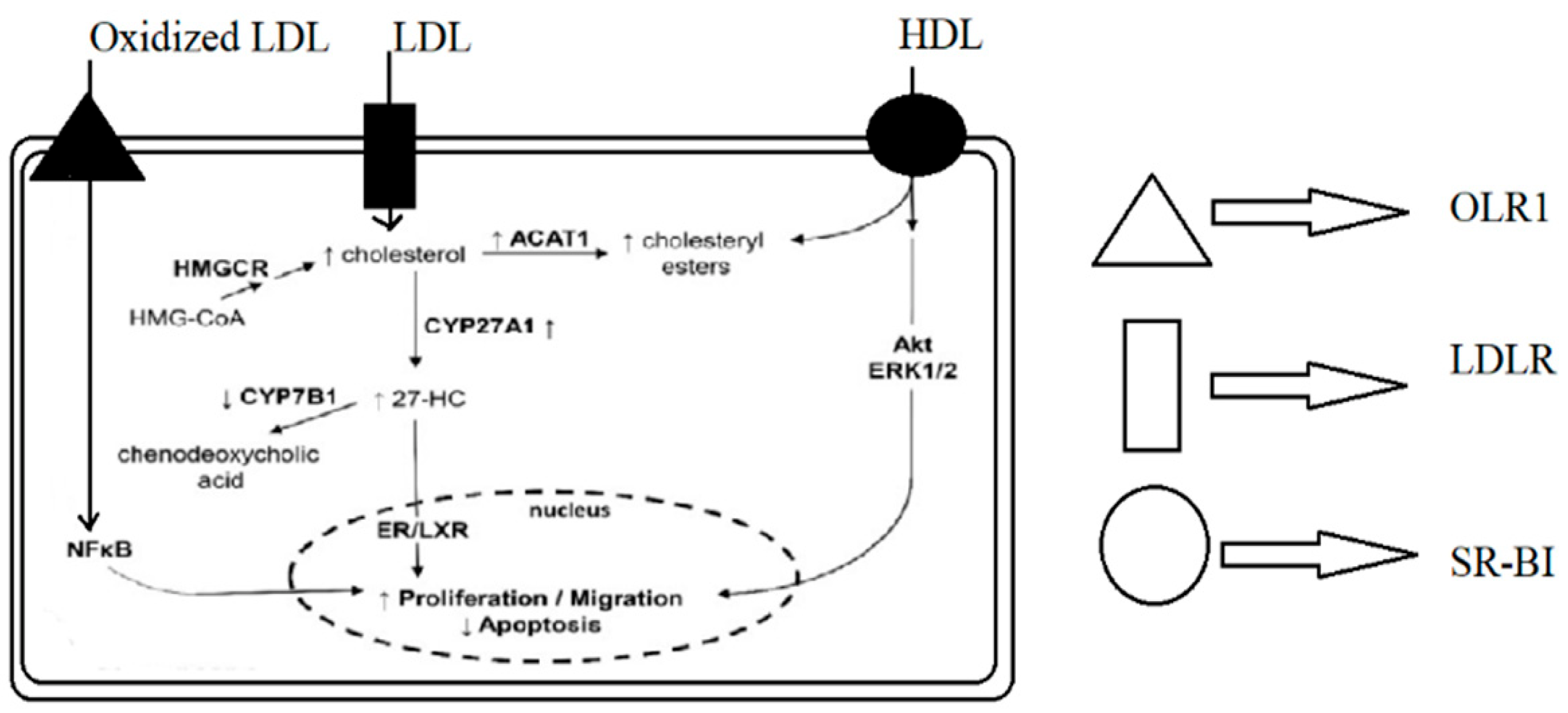
2.1. LDL and Breast Cancer
2.2. HDL and Breast Cancer
3. Clinical and Epidemiological Studies of the Roles of Lipoproteins in Various Malignancies
4. Cholesterol-Lowering Therapies for Breast Cancer
5. Future Possibilities of Targeting Lipid Metabolism to Reduce Breast Cancer Risk
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nelson, E.R.; Chang, C.Y.; McDonnell, D.P. Cholesterol and Breast Cancer Pathophysiology. Trends Endocrinol. Metab. 2014, 25, 649. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lehmann, B.D.; Bauer, J.A.; Chen, X.; Sanders, M.E.; Chakravarthy, A.B.; Shyr, Y.; Pietenpol, J.A. Identification of human triple-negative breast cancer subtypes and preclinical models for selection of targeted therapies. J. Clin. Investig. 2011, 121, 2750. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Elmore, S. Apoptosis: A Review of Programmed Cell Death. Toxicol. Pathol. 2007, 35, 495–516. [Google Scholar] [CrossRef] [PubMed]
- Freres, P.; Collignon, J.; Gennigens, C.; Scagnol, I.; Rorive, A.; Barbeaux, A.; Coucke, P.; Jerusalem, G. Le cancer du sein “triple négatif”. Rev. Med. Liege 2010, 65, 120–126. [Google Scholar]
- Bertucci, F.; Finetti, P.; Cervera, N.; Esterni, B.; Hermitte, F.; Viens, P.; Birnbaum, D. How Basal Are Triple-Negative Breast Cancers? Int. J. Cancer 2008, 123, 236–240. [Google Scholar] [CrossRef]
- Chikati, R.; Pandrangi, L.S.; Gundampati, R.; Vemuri, S.H.; Lakhanpal, M.; Singh, S.S.; Saxena, S.; Kuma, C.S. Molecular Studies on Evaluation of Phytol as Cytoskeleton Targeting Element in Cancer. Int. J. Sci. Eng. Res. 2018, 9, 1978–1992. [Google Scholar]
- Nielsen, T.O.; Hsu, F.D.; Jensen, K.; Cheang, M.; Karaca, G.; Hu, Z.; Hernandez-Boussard, T.; Livasy, C.; Cowan, D.; Dressler, L.; et al. Immunohistochemical and Clinical Characterization of the Basal-Like Subtype of Invasive Breast Carcinoma. Clin. Cancer Res. 2004, 10, 5367–5374. [Google Scholar] [CrossRef] [Green Version]
- Lakhanpal, M.; Singh, L.C.; Rahman, T.; Sharma, J.; Singh, M.M.; Kataki, A.C.; Verma, S.; Pandrangi, S.L.; Singh, Y.M.; Wajid, S.; et al. Study of single nucleotide polymorphisms of tumour necrosis factors and HSP genes in nasopharyngeal carcinoma in North East India. Tumor Biol. 2016, 37, 271–281. [Google Scholar] [CrossRef]
- Santos, C.R.; Schulze, A. Lipid metabolism in cancer. FEBS J. 2012, 279, 2610–2623. [Google Scholar] [CrossRef]
- Pandrangi, S.L.; Chalumuri, S.S.; Garimella, S. Emerging Therapeutic Efficacy of Alkaloids as Anticancer Agents. Ann. Rom. Soc. Cell Biol. 2022, 26, 64–74. [Google Scholar]
- Lane, D.M.; Boatman, K.K.; McConathy, W.J. Serum lipids and apolipoproteins in women with breast masses. Breast Cancer Res. Treat. 1995, 34, 161–169. [Google Scholar] [CrossRef] [PubMed]
- Rambatla, P.K.; Pandrangi, S.L.; Rentala, S.; Sireesha, V. A Study on the Expression of CCL5, CXCR4 and Angiogenic Factors by Prostate Cancer Stem Cells. Ann. Rom. Soc. Cell Biol. 2021, 25, 1020–1028. [Google Scholar]
- Park, J.; Morley, T.S.; Kim, M.; Clegg, D.J.; Scherer, P.E. Tumour Progression and Recurrence. Nat. Rev. Endocrinol. 2014, 10, 455–465. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Luo, J.; Yang, H.; Song, B.L. Mechanisms and regulation of cholesterol homeostasis. Nat. Rev. Mol. Cell Biol. 2020, 1, 225–245. [Google Scholar] [CrossRef]
- Schüler-Toprak, S.; Weber, F.; Skrzypczak, M.; Ortmann, O.; Treeck, O. Expression of estrogen-related receptors in ovarian cancer and impact on survival. J. Cancer Res. Clin. Oncol. 2021, 147, 2555–2567. [Google Scholar] [CrossRef]
- Pike, M.C.; Spicer, D.V.; Dahmoush, L.; Press, M.F. Estrogens, progestogens, normal breast cell proliferation, and breast cancer risk. Epidemiol. Rev. 1993, 15, 17–30. [Google Scholar] [CrossRef]
- Lidegaard, O. 28 Reproductive Factors and Breast Cancer. Maturitas 2012, 71, S6–S7. [Google Scholar] [CrossRef]
- Vucenik, I.; Stains, J.P. Obesity and cancer risk: Evidence, mechanisms, and recommendations. Ann. N. Y. Acad. Sci. 2012, 1271, 37–43. [Google Scholar] [CrossRef]
- Myers, J. The Ecology of Modernism: American Environments and Avant-Garde Poetics. J. Mod. Lit. 2018, 41, 175–177. [Google Scholar]
- Zhao, H.; Zhou, L.; Shangguan, A.J.; Bulun, S.E. Aromatase Expression and Regulation in Breast and Endometrial Cancer. J. Mol. Endocrinol. 2016, 57, R19–R33. [Google Scholar] [CrossRef] [Green Version]
- Parekh, N.; Chandran, U.; Bandera, E.V. Obesity in cancer survival. Annu. Rev. Nutr. 2012, 32, 311–342. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ouchi, N.; Parker, J.L.; Lugus, J.J.; Walsh, K. Adipokines in inflammation and metabolic disease. Nat. Rev. Immunol. 2011, 11, 85–97. [Google Scholar] [CrossRef] [PubMed]
- Paz-Filho, G.; Lim, E.L.; Wong, M.L.; Licinio, J. Associations between adipokines and obesity-related cancer. Front. Biosci. 2011, 16, 1634–1650. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miana, V.V.; González, E.A.P. Adipose tissue stem cells in regenerative medicine. Ecancermedicalscience 2018, 12, 822. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kothari, C.; Diorio, C.; Durocher, F. The importance of breast adipose tissue in breast cancer. Int. J. Mol. Sci. 2020, 21, 5760. [Google Scholar] [CrossRef] [PubMed]
- Shi, L.; Tu, B.P. Acetyl-CoA and the regulation of metabolism: Mechanisms and consequences. Curr. Opin. Cell Biol. 2015, 33, 125–131. [Google Scholar] [CrossRef] [Green Version]
- Gao, Z.; Daquinag, A.C.; Su, F.; Snyder, B.; Kolonin, M.G. PDGFRA/PDGFRβ signaling balance modulates progenitor cell differentiation into white and beige adipocytes. Development 2018, 145, dev155861. [Google Scholar] [CrossRef] [Green Version]
- Wankhade, U.D.; Shen, M.; Yadav, H.; Thakali, K.M. Novel Browning Agents, Mechanisms, and Therapeutic Potentials of Brown Adipose Tissue. BioMed Res. Int. 2016, 2016, 2365609. [Google Scholar] [CrossRef] [Green Version]
- Sakakura, T.; Sakagami, Y.; Nishizuka, Y. Dual origin of mesenchymal tissues participating in mouse mammary gland embryogenesis. Dev. Biol. 1982, 91, 202–207. [Google Scholar] [CrossRef]
- Kumar, G.R.; Chikati, R.; Pandrangi, S.L.; Kandapal, M.; Sonkar, K.; Gupta, N.; Mulakayala, C.; Jagannadham, M.V.; Kumar, C.S.; Saxena, S.; et al. Molecular docking and dynamics simulations of A.niger RNase from Aspergillus niger ATCC26550: For potential prevention of human cancer. J. Mol. Model. 2013, 19, 613–621. [Google Scholar] [CrossRef]
- Patel, K.K.; Kashfi, K. Lipoproteins and cancer: The role of HDL-C, LDL-C, and cholesterol-lowering drugs. Biochem. Pharmacol. 2022, 196, 114654. [Google Scholar] [CrossRef] [PubMed]
- Pandrangi, S.L.; Chittineedi, P.; Chikati, R.; Lingareddy, J.R. Role of dietary iron revisited: In metabolism, ferroptosis and pathophysiology of cancer. Am. J. Cancer Res. 2022, 12, 974–985. [Google Scholar] [PubMed]
- Nakano, T.; Inoue, I.; Murakoshi, T. A newly integrated model for intestinal cholesterol absorption and efflux reappraises how plant sterol intake reduces circulating cholesterol levels. Nutrients 2019, 11, 310. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Torres-Romero, J.C.; Lara-Riegos, J.C.; Parra, E.A.E.; Sánchez, V.F.; Arana-Argáez, V.E.; Uc-Colli, S.; Peña-Rico, M.Á.; Ramírez-Camacho, M.A.; Regalado, M.D.P.; Alvarez-Sánchez, M.E. Lipoproteomics: Methodologies and Analysis of Lipoprotein-Associated Proteins along with the Drug Intervention; IntechOpen: London, UK, 2020. [Google Scholar] [CrossRef]
- Malla, R.R.; Pandrangi, S.; Kumari, S.; Gavara, M.M.; Badana, A.K. Exosomal tetraspanins as regulators of cancer progression and metastasis and novel diagnostic markers. Asia Pac. J. Clin. Oncol. 2018, 14, 383–391. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Freeman, M.W.; Walford, G.A. Lipoprotein Metabolism and the Treatment of Lipid Disorders. Endocrinol. Adult Pediatr. 2016, 1–2, 715–736. [Google Scholar]
- Dallinga-Thie, G.M.; Franssen, R.; Mooij, H.L.; Visser, M.E.; Hassing, H.C.; Peelman, F.; Kastelein, J.J.P.; Péterfy, M.; Nieuwdorp, M. The metabolism of triglyceride-rich lipoproteins revisited: New players, new insight. Atherosclerosis 2010, 211, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Cedó, L.; Reddy, S.T.; Mato, E.; Blanco-Vaca, F.; Escolà-Gil, J.C. HDL and LDL: Potential new players in breast cancer development. J. Clin. Med. 2019, 8, 853. [Google Scholar] [CrossRef] [Green Version]
- McCormick, S.P.A. Lipoprotein(a): Biology and Clinical Importance. Clin. Biochem. Rev. 2004, 25, 69–80. [Google Scholar]
- dos Santos, C.R.; Fonseca, I.; Dias, S.; de Almeida, J.C.M. Plasma level of LDL-cholesterol at diagnosis is a predictor factor of, breast tumor progression. BMC Cancer 2014, 14, 132. [Google Scholar]
- Rader, D.J. Molecular regulation of HDL metabolism and function: Implications for novel therapies. J. Clin. Investig. 2006, 116, 3090–3100. [Google Scholar] [CrossRef] [Green Version]
- His, M.; Zelek, L.; Deschasaux, M.; Pouchieu, C.; Kesse-Guyot, E.; Hercberg, S.; Galan, P.; Latino-Martel, P.; Blacher, J.; Touvier, M. Prospective associations between serum biomarkers of lipid metabolism and overall, breast and prostate cancer risk. Eur. J. Epidemiol. 2014, 29, 119–132. [Google Scholar] [CrossRef] [PubMed]
- Lakhanpal, M.; Yadav, D.S.; Devi, T.R.; Singh, L.C.; Singh, K.J.; Latha, S.P.; Chauhan, P.S.; Verma, Y.; Zomavia, E.; Sharma, J.; et al. Association of interleukin-1β-511 C/T polymorphism with tobacco-associated cancer in northeast India: A study on oral and gastric cancer. Cancer Genet. 2014, 207, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Iyengar, N.M.; Brown, K.A.; Zhou, X.K.; Gucalp, A.; Subbaramaiah, K.; Giri, D.D.; Zahid, H.; Bhardwaj, P.; Wendel, N.K.; Falcone, D.J.; et al. Metabolic Obesity, Adipose Inflammation and Elevated Breast Aromatase in Women with Normal Body Mass Index. Cancer Prev. Res. 2017, 10, 235. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pandrangi, S.L.; Bagadi, S.A.R.; Sinha, N.K.; Kumar, M.; Dada, R.; Lakhanpal, M.; Soni, A.; Malvia, S.; Simon, S.; Chintamani, C.; et al. Establishment and characterization of two primary breast cancer cell lines from young Indian breast cancer patients: Mutation analysis. Cancer Cell Int. 2014, 14, 14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blackburn, G.L.; Wang, K.A. Dietary fat reduction and breast cancer outcome: Results from the Women’s Intervention Nutrition Study (WINS). Am. J. Clin. Nutr. 2007, 86, s878–s881. [Google Scholar] [CrossRef] [Green Version]
- Wakeling, A.E.; Newboult, E.; Peters, S.W. Effects of antioestrogens on the proliferation of MCF-7 human breast cancer cells. J. Mol. Endocrinol. 1989, 2, 225–234. [Google Scholar] [CrossRef]
- Pandrangi, S.L.; Chittineedi, P.; Chalumuri, S.S.; Meena, A.S.; Mosquera, J.A.N.; Llaguno, S.N.S.; Pamuru, R.R.; Mohiddin, G.J.; Mohammad, A. Role of Intracellular Iron in Switching Apoptosis to Ferroptosis to Target Therapy-Resistant Cancer Stem Cells. Molecules 2022, 27, 3011. [Google Scholar] [CrossRef]
- Mebratu, Y.; Tesfaigzi, Y. How ERK1/2 activation controls cell proliferation and cell death is subcellular localization the answer? Cell Cycle 2009, 8, 1168–1175. [Google Scholar] [CrossRef]
- Aslam, N.; Nadeem, K.; Noreen, R.J.A.C. Upregulation of scavenger receptor B1 is required for steroidogenic and non-steroidogenic cholesterol metabolism in prostate cancer. Abeloff’s Clin. Oncol. 5/E 2015, 8, 938–944. [Google Scholar]
- Hoekstra, M.; Sorci-Thomas, M. Rediscovering scavenger receptor type BI: Surprising new roles for the HDL receptor. Curr. Opin. Lipidol. 2017, 28, 255–260. [Google Scholar] [CrossRef]
- Goldstein, J.L.; Brown, M.S. Regulation of the mevalonate pathway. Nature 1990, 343, 425–430. [Google Scholar] [CrossRef] [PubMed]
- Sakellakis, M.; Akinosoglou, K.; Kostaki, A.; Spyropoulou, D.; Koutras, A. Statins and risk of breast cancer recurrence. Breast Cancer Targets Ther. 2016, 8, 199–205. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pandrangi, S.L.; Chikati, R.; Chauhan, P.S.; Kumar, C.S.; Banarji, A.; Saxena, S. Effects of ellipticine on ALDH1A1-expressing breast cancer stem cells-An in vitro and in silico study. Tumor Biol. 2014, 35, 723–737. [Google Scholar] [CrossRef] [PubMed]
- Bonovas, S.; Filioussi, K.; Tsavaris, N.; Sitaras, N.M. Use of statins and breast cancer: A meta-analysis of seven randomized clinical trials and nine observational studies. J. Clin. Oncol. 2005, 23, 8606–8612. [Google Scholar] [CrossRef] [PubMed]
- Anothaisintawee, T.; Udomsubpayakul, U.; McEvoy, M.; Lerdsitthichai, P.; Attia, J.; Thakkinstian, A. Effect of lipophilic and hydrophilic statins on breast cancer risk in thai women: A cross-sectional study. J. Cancer 2016, 7, 1163–1168. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Karp, I.; Behlouli, H.; LeLorier, J.; Pilote, L. Statins and Cancer Risk. Am. J. Med. 2008, 121, 302–309. [Google Scholar] [CrossRef]
- Gulati, R.; Naik Ramavath, M.; Metta, V.S.M.K.; Latha Pandrangi, S. Exploring the CRISPR/Cas9 System in Targeting Drug Resistant Cancer Stem Cells. Ann. Rom. Soc. Cell Biol. 2021, 25, 1583–6258. [Google Scholar]
- Cedó, L.; Blanco-Vaca, F.; Escolà-Gil, J.C. Antiatherogenic potential of ezetimibe in sitosterolemia: Beyond plant sterols lowering. Atherosclerosis 2017, 260, 94–96. [Google Scholar] [CrossRef]
- Pelton, K.; Coticchia, C.M.; Curatolo, A.S.; Schaffner, C.P.; Zurakowski, D.; Solomon, K.R.; Moses, M.A. Hypercholesterolemia induces angiogenesis and accelerates growth of breast tumors in vivo. Am. J. Pathol. 2014, 184, 2099–2110. [Google Scholar] [CrossRef] [Green Version]
- Lauridsen, B.K.; Stender, S.; Frikke-Schmidt, R.; Nordestgaard, B.G.; Tybjærg-Hansen, A. Using genetics to explore whether the cholesterol-lowering drug ezetimibe may cause an increased risk of cancer. Int. J. Epidemiol. 2017, 46, 1777–1785. [Google Scholar] [CrossRef]
- Abdelwahed, K.S.; Siddique, A.B.; Mohyeldin, M.M.; Qusa, M.H.; Goda, A.A.; Singh, S.S.; Ayoub, N.M.; King, J.A.; Jois, S.D.; El Sayed, K.A. Pseurotin A as a novel suppressor of hormone dependent breast cancer progression and recurrence by inhibiting PCSK9 secretion and interaction with LDL receptor. Pharmacol. Res. 2020, 158, 104847. [Google Scholar] [CrossRef] [PubMed]
- Mahboobnia, K.; Pirro, M.; Marini, E.; Grignani, F.; Bezsonov, E.E.; Jamialahmadi, T.; Sahebkar, A. PCSK9 and cancer: Rethinking the link. Biomed. Pharmacother. 2021, 140, 111758. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.E.; Han, S.Y.; Wolfson, B.; Zhou, Q. The Role of Endothelial Lipase in Lipid Metabolism, Inflammation, and Cancer. Histol. Histopathol. 2018, 33, 1. [Google Scholar] [PubMed]
- Kersten, S. ANGPTL3 as therapeutic target. Curr. Opin. Lipidol. 2021, 32, 335. [Google Scholar] [CrossRef] [PubMed]

| Lipoprotein Type | Density (g/mL) | Major Lipids | Major Apoproteins | Properties |
|---|---|---|---|---|
| Chylomicrons | <0.930 | Triglycerides | Apo B-48, Apo C, Apo E, Apo A-I, A-II, A-IV | Lowest protein-to lipid ratio; comprising about 90% of the lipid content [14] |
| Very low-density Lipoprotein | 0.930–1.006 | Triglycerides | Apo B-100, Apo C, Apo-E | Has high cholesterol content when compared with chylomicrons. Major triglyceride carrier [36]. |
| Intermediate low-density Lipoprotein | 1.006–1.019 | Triglycerides Cholesterol | Apo B-100, Apo C, Apo-E | Triglyceride scavenger [37]. |
| Low-density Lipoprotein | 1.019–1.063 | Cholesterol | Apo B-100 | Smaller, denser, readily oxidized molecules and are associated with great atherogenicity [38]. |
| High-density Lipoprotein | 1.063–1.210 | Cholesterol Phospholipids | Apo A-I, Apo A-II, Apo C, Apo-E | Inhibits oxidation, coagulation, activation of endothelium, platelet aggregation, and inflammation [31]. |
| Lipoprotein (a) | 1.055–1.085 | Cholesterol | Apo B-100, Apo (a) | High affitinity towards arterial wall and exihibits thrombogenic properties [39]. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pandrangi, S.L.; Chittineedi, P.; Chikati, R.; Mosquera, J.A.N.; Llaguno, S.N.S.; Mohiddin, G.J.; Lanka, S.; Chalumuri, S.S.; Maddu, N. Role of Lipoproteins in the Pathophysiology of Breast Cancer. Membranes 2022, 12, 532. https://doi.org/10.3390/membranes12050532
Pandrangi SL, Chittineedi P, Chikati R, Mosquera JAN, Llaguno SNS, Mohiddin GJ, Lanka S, Chalumuri SS, Maddu N. Role of Lipoproteins in the Pathophysiology of Breast Cancer. Membranes. 2022; 12(5):532. https://doi.org/10.3390/membranes12050532
Chicago/Turabian StylePandrangi, Santhi Latha, Prasanthi Chittineedi, Rajasekhar Chikati, Juan Alejandro Neira Mosquera, Sungey Naynee Sánchez Llaguno, Gooty Jaffer Mohiddin, Suseela Lanka, Sphoorthi Shree Chalumuri, and Narendra Maddu. 2022. "Role of Lipoproteins in the Pathophysiology of Breast Cancer" Membranes 12, no. 5: 532. https://doi.org/10.3390/membranes12050532
APA StylePandrangi, S. L., Chittineedi, P., Chikati, R., Mosquera, J. A. N., Llaguno, S. N. S., Mohiddin, G. J., Lanka, S., Chalumuri, S. S., & Maddu, N. (2022). Role of Lipoproteins in the Pathophysiology of Breast Cancer. Membranes, 12(5), 532. https://doi.org/10.3390/membranes12050532






